Clinical Outcome of Fully Digital Workflow for Single-Implant-Supported Crowns: A Retrospective Clinical Study
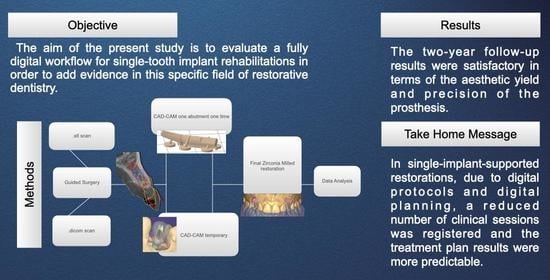
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subject Population
- Patients over 18 years of age;
- Good general health conditions according to the American Society of Anesthesiology scale (ASA 1 or ASA 2) [15];
- Patients requiring single-implant-supported reconstructions.
- General contraindications to oral surgery;
- Periodontally compromised patients (probing pocket depth ≥ 5 mm, bleeding on probing, and plaque index ≥ 25%);
- Patients requiring bone augmentation procedures.
2.3. Surgical and Prosthetic Workflow
2.4. Outcome
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bennardo, F.; Barone, S.; Vocaturo, C.; Nucci, L.; Antonelli, A.; Giudice, A. Usefulness of Magnetic Mallet in Oral Surgery and Implantology: A Systematic Review. J. Pers. Med. 2022, 12, 108. [Google Scholar] [CrossRef] [PubMed]
- Salomão, G.V.D.S.; Chun, E.P.; Panegaci, R.D.S.; Santos, F.T. Analysis of Digital Workflow in Implantology. Case Rep. Dent. 2021, 1–7. [Google Scholar] [CrossRef]
- De Angelis, P.; Gasparini, G.; Rella, E.; De Angelis, S.; Grippaudo, C.; D’Addona, A.; Manicone, P.F. Patient Satisfaction with Implant-Supported Monolithic and Partially Veneered Zirconia Restorations. BioMed Res. Int. 2021, 2021, 6692939. [Google Scholar] [CrossRef]
- De Angelis, P.; Manicone, P.F.; De De Angelis, S.; Grippaudo, C.; Gasparini, G.; Liguori, M.G.; Camodeca, F.; Piccirillo, G.B.; DeSantis, V.; D’Amato, G.; et al. Patient and Operator Centered Outcomes in Implant Dentistry: Comparison between Fully Digital and Conventional Workflow for Single Crown and Three-Unit Fixed-Bridge. Materials 2020, 13, 2781. [Google Scholar] [CrossRef]
- Stanley, M.; Paz, A.G.; Miguel, I.; Coachman, C. Fully digital workflow, integrating dental scan, smile design and CAD-CAM: Case report. BMC Oral Health 2018, 18, 1–8. [Google Scholar] [CrossRef]
- Mangano, F.; Margiani, B.; Admakin, O. A Novel Full-Digital Protocol (SCAN-PLAN-MAKE-DONE®) for the Design and Fabrication of Implant-Supported Monolithic Translucent Zirconia Crowns Cemented on Customized Hybrid Abutments: A Retrospective Clinical Study on 25 Patients. Int. J. Environ. Res. Public Health 2019, 16, 317. [Google Scholar] [CrossRef] [Green Version]
- Mangano, F.; Veronesi, G. Digital versus Analog Procedures for the Prosthetic Restoration of Single Implants: A Randomized Controlled Trial with 1 Year of Follow-Up. BioMed Res. Int. 2018, 2018, 5325032. [Google Scholar] [CrossRef] [Green Version]
- Gallardo, Y.R.; Bohner, L.; Tortamano, P.; Pigozzo, M.N.; Laganá, D.C.; Sesma, N. Patient outcomes and procedure working time for digital versus conventional impressions: A systematic review. J. Prosthet. Dent. 2018, 119, 214–219. [Google Scholar] [CrossRef]
- Christensen, G.J. Impressions Are Changing. J. Am. Dent. Assoc. 2009, 140, 1301–1304. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Abbasi, M.S.; Haider, S.; Ahmed, N.; Habib, S.R.; Altamash, S.; Zafar, M.S.; Alam, M.K. Fit Accuracy of Removable Partial Denture Frameworks Fabricated with CAD/CAM, Rapid Prototyping, and Conventional Techniques: A Systematic Review. BioMed Res. Int. 2021, 2021, 3194433. [Google Scholar] [CrossRef]
- Canullo, L.; Di Domenico, A.; Marinotti, F.; Menini, M.; Pesce, P. Soft Tissue Contour Impression with Analogic or Digital Work Flow: A Case Report. Int. J. Environ. Res. Public Health 2018, 15, 2623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joda, T.; Zarone, F.; Ferrari, M. The complete digital workflow in fixed prosthodontics: A systematic review. BMC Oral Health 2017, 17, 124. [Google Scholar] [CrossRef] [PubMed]
- Ferrini, F.; Sannino, G.; Chiola, C.; Capparé, P.; Gastaldi, G.; Gherlone, E.F. Influence of Intra-Oral Scanner (I.O.S.) on The Marginal Accuracy of CAD/CAM Single Crowns. Int. J. Environ. Res. Public Health 2019, 16, 544. [Google Scholar] [CrossRef] [Green Version]
- Park, J.-S.; Lim, Y.-J.; Kim, B.; Kim, M.-J.; Kwon, H.-B. Clinical Evaluation of Time Efficiency and Fit Accuracy of Lithium Disilicate Single Crowns between Conventional and Digital Impression. Materials 2020, 13, 5467. [Google Scholar] [CrossRef]
- Doyle, D.J.; Goyal, A.; Garmon, E.H. American Society of Anesthesiologists Classification. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Canullo, L.; Colombo, M.; Menini, M.; Sorge, P.; Pesce, P. Trueness of Intraoral Scanners Considering Operator Experience and Three Different Implant Scenarios: A Preliminary Report. Int. J. Prosthodont. 2021, 34, 250–253. [Google Scholar] [CrossRef] [PubMed]
- Fürhauser, R.; Mailath-Pokorny, G.; Haas, R.; Busenlechner, D.; Watzek, G.; Pommer, B. Immediate Restoration of Immediate Implants in the Esthetic Zone of the Maxilla Via the Copy-Abutment Technique: 5-Year Follow-Up of Pink Esthetic Scores. Clin. Implant Dent. Relat. Res. 2016, 19, 28–37. [Google Scholar] [CrossRef]
- Dolcini, G.A.; Colombo, M.; Mangano, C. From Guided Surgery to Final Prosthesis with a Fully Digital Procedure: A Prospective Clinical Study on 15 Partially Edentulous Patients. Int. J. Dent. 2016, 2016, 7358423. [Google Scholar] [CrossRef] [Green Version]
- Flugge, T.; Derksen, W.; Te Poel, J.; Hassan, B.; Nelson, K.; Wismeijer, D. Registration of cone beam computed tomography data and intraoral surface scans—A prerequisite for guided implant surgery with CAD/CAM drilling guides. Clin. Oral Implant. Res. 2017, 28, 1113–1118. [Google Scholar] [CrossRef]
- Scherer, M.D. Presurgical Implant-Site Assessment and Restoratively Driven Digital Planning. Dent. Clin. N. Am. 2014, 58, 561–595. [Google Scholar] [CrossRef]
- El Kholy, K.; Lazarin, R.; Janner, S.F.M.; Faerber, K.; Buser, R.; Buser, D. Influence of surgical guide support and implant site location on accuracy of static Computer-Assisted Implant Surgery. Clin. Oral Implant. Res. 2019, 30, 1067–1075. [Google Scholar] [CrossRef]
- Nickenig, H.-J.; Eitner, S.; Rothamel, D.; Wichmann, M.; Zöller, J.E. Possibilities and limitations of implant placement by virtual planning data and surgical guide templates. Int. J. Comput. Dent. 2012, 15, 9–21. [Google Scholar] [PubMed]
- El Kholy, K.; Ebenezer, S.; Wittneben, J.; Lazarin, R.; Rousson, D.; Buser, D. Influence of implant macrodesign and insertion connection technology on the accuracy of static computer-assisted implant surgery. Clin. Implant Dent. Relat. Res. 2019, 21, 1073–1079. [Google Scholar] [CrossRef]
- Stimmelmayr, M.; Güth, J.-F.; Erdelt, K.; Happe, A.; Schlee, M.; Beuer, F. Clinical study evaluating the discrepancy of two different impression techniques of four implants in an edentulous jaw. Clin. Oral Investig. 2012, 17, 1929–1935. [Google Scholar] [CrossRef]
- Favero, R.; Volpato, A.; De Francesco, M.; Di Fiore, A.; Guazzo, R.; Favero, L. Accuracy of 3D digital modeling of dental arches. Dent. Press J. Orthod. 2019, 24, 038e1–037e7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mangano, F.G.; Admakin, O.; Bonacina, M.; Lerner, H.; Rutkunas, V.; Mangano, C. Trueness of 12 intraoral scanners in the full-arch implant impression: A comparative in vitro study. BMC Oral Health 2020, 20, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J. Fit of CAD/CAM Implant Frameworks: A Comprehensive Review. J. Oral Implant. 2014, 40, 758–766. [Google Scholar] [CrossRef]
- Klongbunjit, D.; Aunmeungtong, W.; Khongkhunthian, P. Implant-abutment screw removal torque values between customized titanium abutment, straight titanium abutment, and hybrid zirconia abutment after a million cyclic loading: An in vitro comparative study. Int. J. Implant Dent. 2021, 7, 98. [Google Scholar] [CrossRef]
- Ren, X.; Son, K.; Lee, K.-B. Accuracy of Proximal and Occlusal Contacts of Single Implant Crowns Fabricated Using Different Digital Scan Methods: An In Vitro Study. Materials 2021, 14, 2843. [Google Scholar] [CrossRef]
- Hanif, A.; Qureshi, S.; Sheikh, Z.; Rashid, H. Complications in implant dentistry. Eur. J. Dent. 2017, 11, 135–140. [Google Scholar] [CrossRef] [Green Version]
- Colombo, M.; Mangano, C.; Mijiritsky, E.; Krebs, M.; Hauschild, U.; Fortin, T. Clinical applications and effectiveness of guided implant surgery: A critical review based on randomized controlled trials. BMC Oral Health 2017, 17, 150. [Google Scholar] [CrossRef] [PubMed]
- Bishti, S.; Tuna, T.; Rittich, A.; Wolfart, S. Patient-reported outcome measures (PROMs) of implant-supported reconstructions using digital workflows: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2021, 32, 318–335. [Google Scholar] [CrossRef]
- Siqueira, R.; Chen, Z.; Galli, M.; Saleh, I.; Wang, H.; Chan, H. Does a fully digital workflow improve the accuracy of computer-assisted implant surgery in partially edentulous patients? A systematic review of clinical trials. Clin. Implant Dent. Relat. Res. 2020, 22, 660–671. [Google Scholar] [CrossRef]
- Hasanzade, M.; Aminikhah, M.; Afrashtehfar, K.I.; Alikhasi, M. Marginal and internal adaptation of single crowns and fixed dental prostheses by using digital and conventional workflows: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 126, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Russo, L.L.; Caradonna, G.; Biancardino, M.; De Lillo, A.; Troiano, G.; Guida, L. Digital versus conventional workflow for the fabrication of multiunit fixed prostheses: A systematic review and meta-analysis of vertical marginal fit in controlled in vitro studies. J. Prosthet. Dent. 2019, 122, 435–440. [Google Scholar] [CrossRef]
- Raffone, C.; Gianfreda, F.; Bollero, P.; Pompeo, M.G.; Miele, G.; Canullo, L. Chairside virtual patient protocol. Part 1: Free vs Guided face scan protocol. J. Dent. 2021, 116, 103881. [Google Scholar] [CrossRef]
- Raffone, C.; Gianfreda, F.; Pompeo, M.G.; Antonacci, D.; Bollero, P.; Canullo, L. Chairside virtual patient protocol. Part 2: Management of multiple face scans and alignment predictability. J. Dent. 2022, 122, 104123. [Google Scholar] [CrossRef]








| Patients | Age (y) | Sex (M/F) | Site | Incisors | Canine | Premolar | Molar |
|---|---|---|---|---|---|---|---|
| 19 | Mean: 47.7 SD: 13.6 | 6/19 | Mandible: 4 Maxilla: 15 | 12 | 2 | 5 | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gianfreda, F.; Pesce, P.; Marcano, E.; Pistilli, V.; Bollero, P.; Canullo, L. Clinical Outcome of Fully Digital Workflow for Single-Implant-Supported Crowns: A Retrospective Clinical Study. Dent. J. 2022, 10, 139. https://doi.org/10.3390/dj10080139
Gianfreda F, Pesce P, Marcano E, Pistilli V, Bollero P, Canullo L. Clinical Outcome of Fully Digital Workflow for Single-Implant-Supported Crowns: A Retrospective Clinical Study. Dentistry Journal. 2022; 10(8):139. https://doi.org/10.3390/dj10080139
Chicago/Turabian StyleGianfreda, Francesco, Paolo Pesce, Erich Marcano, Valeria Pistilli, Patrizio Bollero, and Luigi Canullo. 2022. "Clinical Outcome of Fully Digital Workflow for Single-Implant-Supported Crowns: A Retrospective Clinical Study" Dentistry Journal 10, no. 8: 139. https://doi.org/10.3390/dj10080139
APA StyleGianfreda, F., Pesce, P., Marcano, E., Pistilli, V., Bollero, P., & Canullo, L. (2022). Clinical Outcome of Fully Digital Workflow for Single-Implant-Supported Crowns: A Retrospective Clinical Study. Dentistry Journal, 10(8), 139. https://doi.org/10.3390/dj10080139