Oral Function and the Oral Microbiome in the Elderly in the Kyotango Area
Abstract
:1. Introduction
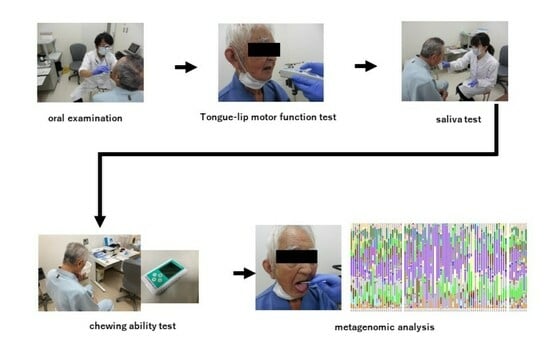
2. Materials and Methods
2.1. Evaluation of General Condition
2.2. Chewing Ability Test
2.3. Tongue–Lip Motor Function Test
2.4. Saliva Test
2.5. Plaque 16S rDNA Analysis
2.6. Sequence Data Processing
2.7. Statistical Analysis and Data Visualization
3. Results
3.1. Elderly Subjects
3.2. Oral Function of Elderly Subjects
3.3. Saliva Volume and Diversity of the Oral Microbiome
3.4. Diversity of the Oral Microbiome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Watanabe, Y.; Okada, K.; Kondo, M.; Matsushita, T.; Nakazawa, S.; Yamazaki, Y. Oral health for achieving longevity. Geriatr. Gerontol. Int. 2020, 20, 526–538. [Google Scholar] [CrossRef] [PubMed]
- Nomura, Y.; Kakuta, E.; Okada, A.; Otsuka, R.; Shimada, M.; Tomizawa, Y.; Taguchi, C.; Arikawa, K.; Daikoku, H.; Sato, T.; et al. Effects of self-assessed chewing ability, tooth loss and serum albumin on mortality in 80-year-old individuals: A 20-year follow-up study. BMC Oral Health 2020, 20, 122. [Google Scholar]
- Ansai, T.; Takata, Y.; Soh, I.; Awano, S.; Yoshida, A.; Sonoki, K.; Hamasaki, T.; Torisu, T.; Sogame, A.; Shimada, N.; et al. Relationship between tooth loss and mortality in 80-year-old Japanese community-dwelling subjects. BMC Public Health 2010, 10, 386. [Google Scholar]
- Hashimoto, M.; Yamanaka, K.; Shimosato, T.; Ozawa, A.; Takigawa, T.; Hidaka, S.; Sakai, T.; Noguchi, T. Oral condition and health status of elderly 8020 achievers in Aichi Prefecture. Bull. Tokyo Dent. Coll. 2006, 47, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Minakuchi, S.; Tsuga, K.; Ikebe, K.; Ueda, T.; Tamura, F.; Nagao, K.; Furuya, J.; Matsuo, K.; Yamamoto, K.; Kanazawa, M.; et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology 2018, 35, 317–324. [Google Scholar] [CrossRef]
- Iwasaki, M.; Motokawa, K.; Watanabe, Y.; Shirobe, M.; Ohara, Y.; Edahiro, A.; Kawai, H.; Fujiwara, Y.; Kim, H.; Ihara, K.; et al. Oral hypofunction and malnutrition among community-dwelling older adults: Evidence from the Otassha study. Gerodontology 2022, 39, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Shimazaki, Y.; Nonoyama, T.; Tsushita, K.; Arai, H.; Matsushita, K.; Uchibori, N. Oral Hypofunction and Its Association with Frailty in Community-Dwelling Older People. Geriatr. Gerontol. Int. 2020, 20, 917–926. [Google Scholar]
- Nakamura, M.; Hamada, T.; Tanaka, A.; Nishi, K.; Kume, K.; Goto, Y.; Beppu, M.; Hijioka, H.; Higashi, Y.; Tabata, H.; et al. Association of Oral Hypofunction with Frailty, Sarcopenia, and Mild Cognitive Impairment: A Cross-Sectional Study of Community-Dwelling Japanese Older Adults. J. Clin. Med. 2021, 10, 1626. [Google Scholar] [CrossRef]
- Azarpazhooh, A.; Leake, J.L. Systematic review of the association between respiratory diseases and oral health. J. Periodontol. 2006, 77, 1465–1482. [Google Scholar] [CrossRef]
- Yamamura, K.; Baba, Y.; Nakagawa, S.; Mima, K.; Miyake, K.; Nakamura, K.; Sawayama, H.; Kinoshita, K.; Ishimoto, T.; Iwatsuki, M.; et al. Human microbiome Fusobacterium nucleatum in esophageal cancer tissue is associated with prognosis. Clin. Cancer Res. 2016, 22, 5574–5581. [Google Scholar] [CrossRef]
- Flynn, K.J.; Baxter, N.T.; Schloss, P.D. Metabolic and community synergy of oral bacteria in colorectal cancer. mSphere 2016, 1, e00102-16. [Google Scholar]
- Scannapieco, F.A.; Cantos, A. Oral inflammation and infection, and chronic medical diseases: Implications for the elderly. Periodontology 2016, 72, 153–175. [Google Scholar]
- Aida, J.; Kondo, K.; Yamamoto, T.; Hirai, H.; Nakade, M.; Osaka, K.; Sheiham, A.; Tsakos, G.; Watt, R.G. Oral health and cancer, cardiovascular, and respiratory mortality of Japanese. J. Dent. Res. 2011, 90, 1129–1135. [Google Scholar] [PubMed]
- Tuominen, H.; Rautava, J. Oral microbiota and cancer development. Pathobiology 2021, 88, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Kong, C.; Yang, Y.; Cai, S.; Li, X.; Cai, G.; Ma, Y. Human oral microbiome dysbiosis as a novel noninvasive biomarker in detection of colorectal cancer. Theranostics 2020, 10, 11595–11606. [Google Scholar] [CrossRef] [PubMed]
- Qi, Y.; Zang, S.Q.; Wei, J.; Yu, H.C.; Yang, Z.; Wu, H.M.; Kang, Y.; Tao, H.; Yang, M.F.; Jin, L.; et al. High-throughput sequencing provides insights into oral microbiota dysbiosis in association with inflammatory bowel disease. Genomics 2021, 113, 664–676. [Google Scholar]
- Mohammed, H.; Varoni, E.M.; Cochis, A.; Cordaro, M.; Gallenzi, P.; Patini, R.; Staderini, E.; Lajolo, C.; Rimondini, L.; Rocchetti, V. Oral dysbiosis in pancreatic cancer and liver cirrhosis: A review of the literature. Biomedicines 2018, 6, 115. [Google Scholar] [CrossRef]
- Naito, Y.; Takagi, T.; Inoue, R.; Kashiwagi, S.; Mizushima, K.; Tsuchiya, S.; Itoh, Y.; Okuda, K.; Tsujimoto, Y.; Adachi, A.; et al. Gut microbiota differences in elderly subjects between rural city Kyotango and urban city Kyoto: An age-gender-matched study. Clin. Biochem. Nutr. 2019, 65, 125–131. [Google Scholar] [CrossRef]
- Zhou, Y.; Gao, H.; Mihindukulasuriya, K.A.; La Rosa, P.S.; Wylie, K.M.; Vishnivetskaya, T.; Podar, M.; Warner, B.; Tarr, P.I.; Nelson, D.E.; et al. Biogeography of the ecosystems of the healthy human body. Genome Biol. 2013, 14, R1. [Google Scholar] [CrossRef]
- Yamanaka, K.; Nakagaki, H.; Morita, I.; Suzaki, H.; Hashimoto, M.; Sakai, T. Comparison of the health condition between the 8020 achievers and the 8020 non-achievers. Int. Dent. J. 2008, 58, 146–150. [Google Scholar] [CrossRef]
- Yamamoto, T.; Kondo, K.; Misawa, J.; Hirai, H.; Nakade, M.; Aida, J.; Kondo, N.; Kawachi, I.; Hirata, Y. Dental status and incident falls among older Japanese: A prospectivecohort study. BMJ Open 2012, 2, e001262. [Google Scholar] [CrossRef] [PubMed]
- Tamura, B.K.; Bell, C.L.; Masaki, K.H.; Amella, E.J. Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: A systematic review of the literature. J. Am. Med. Dir. Assoc. 2013, 14, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Inomata, C.; Ikebe, K.; Kagawa, R.; Okubo, H.; Sasaki, S.; Okada, T.; Takeshita, H.; Tada, S.; Matsuda, K.; Kurushima, Y.; et al. Significance of occlusal force for dietary fibre and vitamin intakes in independently living 70-year-old Japanese: From SONIC Study. J. Dent. 2014, 42, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Seraj, Z.; Al-Najjar, D.; Akl, M.; Aladle, N.; Altijani, Y.; Zaki, A.; Al Kawas, S. The effect of number of teeth and chewing ability on cognitive function of elderly in UAE: A pilot study. Int. J. Dent. 2017, 2017, 5732748. [Google Scholar]
- Hasegawa, Y.; Sakuramoto-Sadakane, A.; Nagai, K.; Tamaoka, J.; Oshitani, M.; Ono, T.; Sawada, T.; Shinmura, K.; Kishimoto, H. Does oral hypofunction promote social withdrawal in the older adults? A longitudinal survey of elderly subjects in rural Japan. Int. J. Environ. Res. Public Health 2020, 17, 8904. [Google Scholar] [CrossRef]
- Dusek, M.; Simmons, J.; Buschang, P.H.; al-Hashimi, I. Masticatory function in patients with xerostomia. Gerodontology 1996, 13, 3–8. [Google Scholar] [PubMed]
- Li, L.; Finnegan, M.B.; Özkan, S.; Kim, Y.; Lillehoj, P.B.; Ho, C.M.; Lux, R.; Mito, R.; Loewy, Z.; Shi, W. In vitro study of biofilm formation and effectiveness of antimicrobial treatment on various dental material surfaces. Mol. Oral Microbiol. 2010, 25, 384–390. [Google Scholar]
- Busscher, H.J.; Rinastiti, M.; Siswomihardjo, W.; van der Mei, H.C. Biofilm formation on dental restorative and implant materials. J. Dent. Res. 2010, 89, 657–665. [Google Scholar]
- Kreth, J.; Merritt, J.; Pfeifer, C.S.; Khajotia, S.; Ferracane, J.L. Interaction between the oral microbiome and dental composite biomaterials: Where we are and where we should go. J. Dent. Res. 2020, 99, 1140–1149. [Google Scholar] [CrossRef]
- Hatanaka, Y.; Furuya, J.; Sato, Y.; Uchida, Y.; Shichita, T.; Kitagawa, N.; Osawa, T. Associations between Oral Hypofunction Tests, Age, and Sex. Int. J. Environ. Res. Public Health 2021, 18, 10256. [Google Scholar] [CrossRef]
- Onuki, W.; Magara, J.; Tsujimura, T.; Ito, K.; Sakai, H.; Kulvanich, S.; Nakajima, Y.; Saka, N.; Inoue, M. Survey of oral hypofunction in older outpatients at a dental hospital. J. Oral Rehabil. 2021, 48, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Archambault, L.; Koshy-Chenthittayilm, S.; Thompson, A.; Dongari-Bagtzoglou, A.; Laubenbacher, R.; Mendes, P. Understanding Lactobacillus paracasei and Streptococcus oralis Biofilm Interactions through Agent-Based Modeling. mSphere 2021, 6, e0087521. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, J.; Tanaka, M. Influence of type of prosthesis on oral environment and the number of missing teeth in elderly persons. Int. J. Dent. 2010, 2010, 584134. [Google Scholar] [CrossRef]
- Montenegro, L.A.S.; Silva, E.; Farias, I.P.; de Araújo, E.C.; de Pontes, J.C.; Raymundo, M.L.; de Sousa, S.A.; Almeida, L.F.D.; Cavalcanti, Y.W. Biochemical and microbiological analysis of the saliva of institutionalized elderly: With edentulism, use of dentures and presence of biofilm. J. Clin. Exp. Dent. 2020, 12, e632–e637. [Google Scholar] [CrossRef] [PubMed]
- Buranarom, N.; Komin, O.; Matangkasombut, O. Hyposalivation, oral health, and Candida colonization in independent dentate elders. PLoS ONE 2020, 15, e0242832. [Google Scholar] [CrossRef] [PubMed]
- Shirasugi, M.; Nakagawa, M.; Nishioka, K.; Yamamoto, T.; Nakaya, T.; Kanamura, N. Relationship between periodontal disease and butyric acid produced by periodontopathic bacteria. Inflamm. Regen. 2018, 38, 23. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Wang, Y.; Zhao, X.; Liu, C.; Wang, B.; Zhou, J. Mechanistic basis and preliminary practice of butyric acid and butyrate sodium to mitigate gut inflammatory diseases: A comprehensive review. Nutr. Res. 2021, 95, 1–18. [Google Scholar] [CrossRef]
- Wu, G.D.; Chen, J.; Hoffmann, C.; Bittinger, K.; Chen, Y.Y.; Keilbaugh, S.A.; Bewtra, M.; Knights, D.; Walters, W.A.; Knight, R.; et al. Linking long-term dietary pattern with gut microbial enterptypes. Science 2011, 334, 105–108. [Google Scholar]
- Saito, S.; Aoki, Y.; Tamahara, T.; Goto, M.; Matsui, H.; Kawashima, J.; Danjoh, I.; Hozawa, A.; Kuriyama, S.; Suzuki, Y.; et al. Oral microbiome analysis in prospective genome cohort studies of the Tohoku medical megabank project. Front. Cell. Infect. Microbiol. 2021, 29, 604596. [Google Scholar]
- Curtis, M.A.; Diaz, P.I.; Van Dyke, T.E. The role of the microbiota in periodontal disease. Periodontology 2000 2020, 83, 14–25. [Google Scholar] [CrossRef]
- Parashar, A.; Parashar, S.; Zingade, A.; Gupta, S.; Sanikop, S. Interspecies communication in oral biofilm: An ocean of information. Int. Oral Sci. 2015, 12, 37–42. [Google Scholar]
- Ptasiewicz, M.; Grywalska, E.; Mertowska, P.; Korona-Głowniak, I.; Poniewierska-Baran, A.; Niedźwiedzka-Rystwej, P.; Chałas, R. Armed to the teeth-the oral mucosa immunity system and microbiota. Int. J. Mol. Sci. 2022, 23, 882. [Google Scholar] [PubMed]







| Number of Subjects | Kyotango 78 | Kyoto 26 | ||
|---|---|---|---|---|
| Age | Male | Female | Male | Female |
| 100– | 1 | 0 | ||
| 99–90 | 6 | 0 | ||
| 89–80 | 34 | 37 | ||
| 39–30 | 5 | 6 | ||
| 29–20 | 8 | 7 | ||
| Total | 41 | 37 | 13 | 13 |
| Hypertension (%) | 48.7 (38/78) | 0 | ||
| Hypercholesterolemia (%) | 33.3 (26/78) | 0 | ||
| Diabetes mellitus (%) | 3.8 (3/78) | 0 | ||
| Cardiovascular disease (%) | 6.4 (5/78) | 0 | ||
| Medication (%) | 24.3 (19/78) | 0 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, Y.; Yamamoto, T.; Miyamoto, N.; Kinoshita, K.; Nishikawa, S.; Adachi, T.; Takizawa, S.; Inoue, R.; Matoba, S.; Kanamura, N. Oral Function and the Oral Microbiome in the Elderly in the Kyotango Area. Dent. J. 2024, 12, 16. https://doi.org/10.3390/dj12010016
Yamamoto Y, Yamamoto T, Miyamoto N, Kinoshita K, Nishikawa S, Adachi T, Takizawa S, Inoue R, Matoba S, Kanamura N. Oral Function and the Oral Microbiome in the Elderly in the Kyotango Area. Dentistry Journal. 2024; 12(1):16. https://doi.org/10.3390/dj12010016
Chicago/Turabian StyleYamamoto, Yoshiaki, Toshiro Yamamoto, Nao Miyamoto, Kohei Kinoshita, Satomi Nishikawa, Tetsuya Adachi, Shigeta Takizawa, Ryo Inoue, Satoaki Matoba, and Narisato Kanamura. 2024. "Oral Function and the Oral Microbiome in the Elderly in the Kyotango Area" Dentistry Journal 12, no. 1: 16. https://doi.org/10.3390/dj12010016
APA StyleYamamoto, Y., Yamamoto, T., Miyamoto, N., Kinoshita, K., Nishikawa, S., Adachi, T., Takizawa, S., Inoue, R., Matoba, S., & Kanamura, N. (2024). Oral Function and the Oral Microbiome in the Elderly in the Kyotango Area. Dentistry Journal, 12(1), 16. https://doi.org/10.3390/dj12010016