‘I Would Rather Be Having My Leg Cut off Than a Little Needle’: A Supplementary Qualitative Analysis of Dentally Anxious Children’s Experiences of Needle Fear
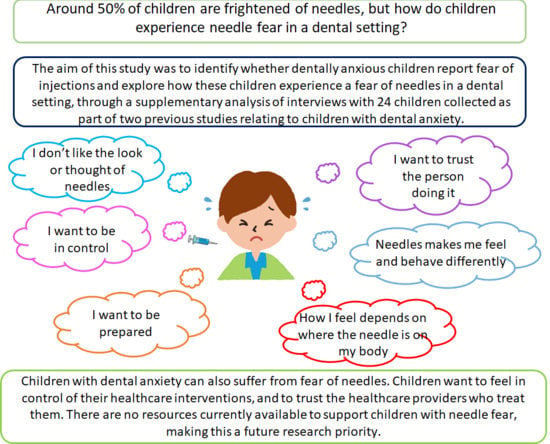
Abstract
:1. Introduction
2. Materials and Methods
2.1. Secondary Analysis
2.2. Sampling Selection
2.3. Analysis
3. Results
3.1. Demographics
3.2. Analysis
3.2.1. Feelings about Needles
‘I would rather be having my leg cut off than a little needle.’(14M, DenAnx)
‘For me just because it’s the, it’s not the teeth coming out that I’ve got to get over it’s the injection bit.’(15F, DecAid)
Interviewer: So are you alright with injections in your arm then?
‘Yeah, because I’ve had 5 already.’(13F, DenAnx)
‘Once I’ve done the first one, I can’t really say I won’t do the next.’(14F, DenAnx)
3.2.2. Nature of Fear
3.2.3. Appearance of the Needle
‘Like a normal injection but a bit bigger.’(10F, DenAnx)
‘I had a picture like a big needle.’(11F, DenAnx)
‘I could see like all like pointy and sharp things that made me pretty scared.’(14M, DenAnx)
‘It’s the point on the needle you seen first.’(15F, DecAid)
3.2.4. Feel of the Needle
‘It stings really badly like 10,000 bees stinging you inside your mouth.’(14M, DenAnx)
‘It is going to really really hurt.’(10F, DenAnx)
‘I liked it. I could not feel that part of my face. But I liked it.’(14F, DenAnx)
3.2.5. Relevance of Area of the Body
‘Interviewer: Is it just injections inside your mouth?
Participant: Any injections. Like at school or anything.’(14F, DenAnx)
‘Why can’t they put it in my arm, and why does it have to go in my mouth.’(11F, DenAnx)
‘I would rather have one in my mouth than in my arms.’(14M, DenAnx)
‘Participant: I am not having a needle stuck in my vein.’
Interviewer: Would you be alright having a needle in your mouth?
‘Participant: Yeah. I’ve had it before so I know what it is like.’(15F, DenAnx)
3.2.6. Context of Fear
‘The second time I was more panicky because I knew what I was expecting, and I didn’t want to have it done again.’(14F, DenAnx)
‘They were like it’s the biggest needle you’ll ever see so.’(14F, DenAnx)
‘They’d go like the needle really hurts and stuff.’(10F, DecAid)
3.2.7. Consequences of Fear
‘I sort of nearly fainted.’(14F, DecAid)
‘And like she once tried to like give me a needle but I didn’t want it. So I like moved her arm.’(14F, DecAid)
‘They had to like bring people to hold me down and stuff.’(14M, DenAnx)
‘But before I came to the appointment I was very distressed. Just sort of, you know, knowing that I was going to have to have an injection, it was going to have to happen. Erm beforehand it did make me very, I don’t know the word, just distressed.’(15F, DecAid)
‘People just get sick of me because I’m taking ages because I don’t want it.’(11F, DenAnx)
3.2.8. Controlling the Process
3.2.9. Awareness and Information
‘Now I know when the needle is going to be going in and stuff like that. And that is the thing.’(15M, DecAid)
‘What was good also was that they didn’t tell me when they were going to do the injection. So in my first injection the first time I just felt stinging, And then I said are you doing the injection, and they were like err no. And then I was sort of calmer because I didn’t know they were doing it.’(14F, DenAnx)
‘To see like what size it was and what was going on in my mouth.’(10F, DenAnx)
‘If they went round the side of my mouth that’s alright because you can see the full thing when they just go over my head.’(15F, DecAid)
3.2.10. Preparation
‘I was expecting like just 1 and then I had 4 so.’(14F, DecAid)
Interviewer: ‘Would you like the dentist to say we are going to do an injection?’
Participant: ‘Yeah’.(11F, DenAnx)
‘I’ve been able to prepare myself, I’ve been able to have the gas and air.’(15F, DecAid)
3.2.11. Trust
‘When I had my needle I said when I put my hand up can you stop, he said yeah, and then when I put my hand up they didn’t, they went on.’(11F, DenAnx)
‘After that I didn’t trust anybody.’(11F, DenAnx)
‘We got this crap one, she was, she was like proper evil.’(14F, DecAid)
‘I have to have someone in the room with me, but not holding my hand or anything.’(15F, DenAnx)
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- McLenon, J.; Rogers, M.A.M. The fear of needles: A systematic review and meta-analysis. J. Adv. Nurs. 2018, 75, 30–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kose, S.; Mandiracioglu, A. Fear of blood/injection in healthy and unhealthy adults admitted to a teaching hospital. Int. J. Clin. Pract. 2007, 61, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Noyes, R.J.; Hartz, A.J.; Doebbeling, C.C.; Malis, R.W.; Happel, R.L.; Werner, L.A.; Yagla, S.J. Illness Fears in the General Population. Psychosom. Med. 2000, 62, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Potasman, Y.N.; Alona, P.A.Z.; Edmond, S.; Israel, P. Fear of Injections in Young Adults: Prevalence and Associations. Am. J. Trop. Med. Hyg. 2003, 68, 341–344. [Google Scholar]
- Sokolowski, C.J.; Giovannitti, J.A., Jr.; Boynes, S.G. Needle phobia: Etiology, adverse consequences, and patient management. Dent. Clin. N. Am. 2010, 54, 731–744. [Google Scholar] [CrossRef] [PubMed]
- Kleinknecht, R.; Lenz, J. Blood/injury fear, fainting and avoidance of medically-related situations: A family correspondence study. Behav. Res. Ther. 1989, 27, 537–547. [Google Scholar] [CrossRef]
- Berge, K.G.; Agdal, M.L.; Vika, M.; Skeie, M.S. High fear of intra-oral injections: Prevalence and relationship to dental fear and dental avoidance among 10- to 16-yr-old children. Eur. J. Oral Sci. 2016, 124, 572–579. [Google Scholar] [CrossRef]
- Siddiqui, T.; Wali, A.; Abdullah, H.; Khan, F.; Tanvir, R.; Siddiqui, M. Evaluation of fear of injections and its association with avoidance of dental treatment. J. Restor. Dent. 2016, 4, 81. [Google Scholar]
- Domoto, P.; Weinstein, P.; Melnick, S.; Ohmura, M.; Uehida, H.; Ohmachi, K.; Shimono, T. Results of a dental fear survey in Japan: Implications for dental public health in Asia. Community Dent. Oral Epidemiol. 1988, 16, 199–201. [Google Scholar] [CrossRef]
- Milgrom, P.; Mancl, L.; King, B.; Weinstein, P. Origins of childhood dental fear. Behav. Res. Ther. 1995, 33, 313–319. [Google Scholar] [CrossRef]
- Wright, S.; Yelland, M.; Heathcote, K.; Ng, S.; Wright, G. Fear of needles—Nature and prevalence in general practice. Aust. Fam. Physician 2009, 38, 172–176. [Google Scholar] [PubMed]
- James, A.C.; James, G.; Cowdrey, F.A.; Soler, A.; Choke, A. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst. Rev. 2015, CD004690. [Google Scholar] [CrossRef] [PubMed]
- Heaton, J. Reworking Qualitative Data; SAGE Publications: London, UK, 2004. [Google Scholar]
- Stewart, D.; Kamins, M. Secondaary Research; Sage Publications: London, UK, 1998. [Google Scholar]
- Porritt, J.; Rodd, H.; Morgan, A.; Williams, C.; Gupta, E.; Kirby, J.; Cresswell, C.; Newton, T.; Stevens, K.; Baker, S.; et al. Development and testing of a Cognitive Behavioural Therapy resource for children’s dental anxiety. JDR Clin. Transl. Res. 2017, 2, 23–37. [Google Scholar] [CrossRef]
- Hulin, J.; Baker, S.R.; Marshman, Z.; Albadri, S.; Rodd, H.D. Development of a decision aid for children faced with the decision to undergo dental treatment with sedation or general anaesthesia. Int. J. Paediatr. Dent. 2017, 27, 344–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ritchie, J.; Lewis, J. Qualitative Research Practice; Sage Publications: London, UK, 2003. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Heft, M.W.; Meng, X.; Bradley, M.M.; Lang, P.J. Gender differences in reported dental fear and fear of dental pain—Heft 2007 Community Dentistry and Oral Epidemiology—Wiley Online Library. Community Dent. Oral Epidemiol. 2007, 35, 421–428. [Google Scholar] [CrossRef]
- Milgrom, P.; Vignehsa, H.; Weinstein, P. Adolescent dental fear and control: Prevalence and theoretical implications. Behav. Res. Ther. 1992, 30, 367–373. [Google Scholar] [CrossRef]
- Porritt, J.; Marshman, Z.; Rodd, H.D. Understanding children’s dental anxiety and psychological approaches to its reduction. Int. J. Paediatr. Dent. 2012, 22, 397–405. [Google Scholar] [CrossRef]
- Zak, P.J.; Kurzban, R.; Matzner, W.T. Oxytocin is associated with human trustworthiness. Horm. Behav. 2005, 48, 522–527. [Google Scholar] [CrossRef]
- Tops, M.; van Peer, J.M.; Korf, J.; Wijers, A.A.; Tucker, D.M. Anxiety, cortisol, and attachment predict plasma oxytocin. Psychophysiology 2007, 44, 444–449. [Google Scholar] [CrossRef]
- Uvnas-Moberg, K. Oxytocin may mediate the benefits of positive social interaction and emotions. Psychoneuroendocrinology 1998, 23, 819–835. [Google Scholar] [CrossRef]
- Karlsson, K.; Rydstrom, I.; Nystrom, M.; Enskar, K.; Dalheim Englund, A.C. Consequences of Needle-Related Medical Procedures: A Hermeneutic Study with Young Children (3–7 Years). J. Pediatr. Nurs. 2016, 31, e109–e118. [Google Scholar] [CrossRef] [PubMed]
- Kortesluoma, R.L.; Nikkonen, M.; Serlo, W. You just have to make the pain go away—Children’s experiences of pain management. Pain Manag. Nurs. 2008, 9, 143–149.e5. [Google Scholar] [CrossRef] [PubMed]
- Polkki, T.; Pietila, A.M.; Rissanen, L. Pain in children: Qualitative research of Finnish school-aged children’s experiences of pain in hospital. Int. J. Nurs. Pract. 1999, 5, 21–28. [Google Scholar] [CrossRef]
- Salmela, M.; Aronen, E.T.; Salantera, S. The experience of hospital-related fears of 4- to 6-year-old children. Child Care Health Dev. 2011, 37, 719–726. [Google Scholar] [CrossRef]
- Taddio, A.; Ipp, M.; Thivakaran, S.; Jamal, A.; Parikh, C.; Smart, S.; Katz, J. Survey of the prevalence of immunization non-compliance due to needle fears in children and adults. Vaccine 2012, 30, 4807–4812. [Google Scholar] [CrossRef] [Green Version]
- Szabo, V.; Strang, V.R. Secondary analysis of qualitative data. Adv. Nurs. Sci. 1997, 20, 66–74. [Google Scholar] [CrossRef]
- Morse, J.M. Qualitative Methods: The State of the Art. Qual. Health Res. 1999, 9, 393–406. [Google Scholar] [CrossRef]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef]
- Gardner, H.; Randall, D. The effects of the presence or absence of parents on interviews with children. Nurse Res. 2012, 19, 6–10. [Google Scholar] [CrossRef]

| Pseudonym | Sex (M/F) | Age at Interview | Original Study |
|---|---|---|---|
| Chloe | F | 11 | Dental anxiety |
| Samantha | F | 15 | Dental anxiety |
| Danielle | F | 11 | Dental anxiety |
| Amelia | F | 14 | Dental anxiety |
| Joe | M | 12 | Dental anxiety |
| Lucy | F | 13 | Dental anxiety |
| Olivia | F | 14 | Dental anxiety |
| Sophie | F | 12 | Dental anxiety |
| Katy | F | 10 | Dental anxiety |
| Ella | F | 14 | Dental anxiety |
| Claire | F | 14 | Dental anxiety |
| Michael | M | 14 | Dental anxiety |
| WK | F | 14 | Decision aid |
| WJL | F | 15 | Decision aid |
| GL | F | 15 | Decision aid |
| MA | F | 13 | Decision aid |
| LJ | F | 12 | Decision aid |
| VL | F | 14 | Decision aid |
| WA | M | 15 | Decision aid |
| SC | F | 13 | Decision aid |
| LD | F | 10 | Decision aid |
| LK | F | 15 | Decision aid |
| Themes | Subthemes |
|---|---|
| Feelings about needles | |
| Nature of fear | Appearance of the needle |
| Feel of the needle | |
| Relevance of area of the body | |
| Context of fear | Origin of fear |
| Social influences | |
| Impacts of fear | Physical |
| Behavioural | |
| Emotional | |
| Controlling the process | Information and awareness |
| Preparation | |
| Trust |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noble, F.; Kettle, J.; Hulin, J.; Morgan, A.; Rodd, H.; Marshman, Z. ‘I Would Rather Be Having My Leg Cut off Than a Little Needle’: A Supplementary Qualitative Analysis of Dentally Anxious Children’s Experiences of Needle Fear. Dent. J. 2020, 8, 50. https://doi.org/10.3390/dj8020050
Noble F, Kettle J, Hulin J, Morgan A, Rodd H, Marshman Z. ‘I Would Rather Be Having My Leg Cut off Than a Little Needle’: A Supplementary Qualitative Analysis of Dentally Anxious Children’s Experiences of Needle Fear. Dentistry Journal. 2020; 8(2):50. https://doi.org/10.3390/dj8020050
Chicago/Turabian StyleNoble, Fiona, Jennifer Kettle, Joe Hulin, Annie Morgan, Helen Rodd, and Zoe Marshman. 2020. "‘I Would Rather Be Having My Leg Cut off Than a Little Needle’: A Supplementary Qualitative Analysis of Dentally Anxious Children’s Experiences of Needle Fear" Dentistry Journal 8, no. 2: 50. https://doi.org/10.3390/dj8020050
APA StyleNoble, F., Kettle, J., Hulin, J., Morgan, A., Rodd, H., & Marshman, Z. (2020). ‘I Would Rather Be Having My Leg Cut off Than a Little Needle’: A Supplementary Qualitative Analysis of Dentally Anxious Children’s Experiences of Needle Fear. Dentistry Journal, 8(2), 50. https://doi.org/10.3390/dj8020050