Cervical Cancer Prevention in Racially Disparate Rural Populations
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population and Ethical Statement
2.2. Pap, HPV Testing and Colposcopic Examination
2.3. Follow-Up Treatment and Care
2.4. Hematoxylin and Eosin Staining of Tissue Biopsies
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics and Ethical Statement
3.2. HPV, Pap testing and Colposcopic Outcomes
3.3. Follow-Ups and Interventions
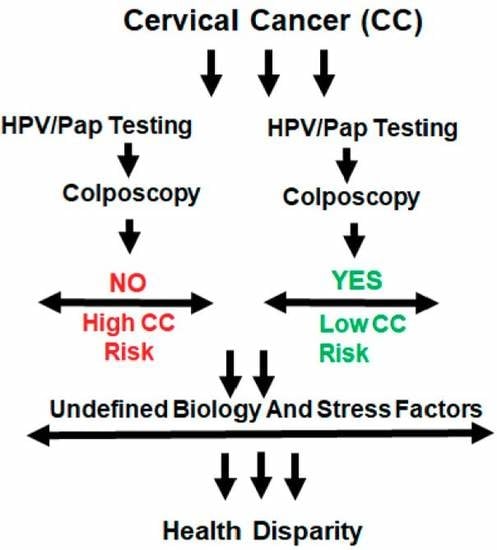
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Crosbie, E.J.; Einstein, M.H.; Franceschi, S.; Kitchener, H.C. Human papilloma virus and cervical cancer. Lancet 2013, 382, 889–899. [Google Scholar] [CrossRef]
- Schiffman, M.; Solomon, D. Clinical practice. Cervical-cancer screening with human papilloma virus and cytologic cotesting. N. Engl. J. Med. 2013, 369, 2324–2331. [Google Scholar] [CrossRef] [PubMed]
- Texas Cancer Registry. Available online: http://www.dshs.texas.gov/tcr/ (accessed on 10 June 2019).
- National Cancer Institute. Available online: https://www.cancer.gov/ (accessed on 14 August 2019).
- Pratte, M.A.; Griffin, A.; Ogazi, C.; Yurasevecz, S.; Blanks, C.A.; McCooey, L.; Kaufman, J.S. Racial/Ethnic Disparities in Cervical Cancer Screening Services Among Contractors of the Connecticut Breast and Cervical Cancer Early Detection Program. Health Equity 2018, 2, 30–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Su, B.; Qin, W.; Xue, F.; Wei, X.; Guan, Q.; Jiang, W.; Wang, S.; Xu, M.; Yu, S. The relation of passive smoking with cervical cancer: A systematic review and meta-analysis. Medicine (Baltimore) 2018, 97, e13061. [Google Scholar] [CrossRef] [PubMed]
- Papillomavirus Episteme. Available online: https://pave.niaid.nih.gov/ (accessed on 27 July 2019).
- Benard, V.B.; Castle, P.E.; Jenison, S.A.; Hunt, W.C.; Kim, J.J.; Cuzick, J.; Lee, J.H.; Du, R.; Robertson, M.; Norville, S.; et al. New Mexico HPV Pap Registry Steering Committee. Population-Based Incidence Rates of Cervical Intraepithelial Neoplasia in the Human Papillomavirus Vaccine Era. JAMA Oncol. 2017, 3, 833–837. [Google Scholar] [CrossRef] [PubMed]
- Kahn, J.A. HPV vaccination for the prevention of cervical intraepithelial neoplasia. N. Engl. J. Med. 2009, 361, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Akinlotan, M.; Bolin, J.N.; Helduser, J.; Ojinnaka, C.; Lichorad, A.; McClellan, D. Cervical Cancer Screening Barriers and Risk Factor Knowledge Among Uninsured Women. J. Community Health 2017, 42, 770–778. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Owusu, G.A.; Eve, S.B.; Cready, C.M.; Koelln, K.; Trevino, F.; Urrutia-Rojas, X.; Baumer, J. Race and ethnic disparities in cervical cancer screening in a safety-net system. Matern Child Health J. 2005, 9, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Dockery, L.E.; Motwani, A.; Ding, K.; Doescher, M.; Dvorak, J.D.; Moore, K.N.; Holman, L.L. Improving cancer care for American Indians with cervical cancer in the Indian Health Service (IHS) system—Navigation may not be enough. Gynecol. Oncol. 2018, 149, 89–92. [Google Scholar] [CrossRef] [PubMed]
- Texas Cancer Registry. Age-Adjusted Cancer Mortality Rates in Texas. 2018. Available online: https://www.cancer-rates.info/tx/ (accessed on 15 June 2018).
- Texas Cancer Registry. Age-adjusted Invasive Cancer Incidence Rates in Texas. 2018. Available online: https://www.dshs.state.tx.us › legislative › 2018-Reports (accessed on 15 June 2018).
- Apgar, B.S.; Zoschnick, L.; Wright, T.C., Jr. The 2001 Bethesda System terminology. Am. Fam. Physician 2003, 68, 1992–1998. [Google Scholar] [PubMed]
- Apgar, B.S.; Kaufman, A.J.; Bettcher, C.; Parker-Featherstone, E. Gynecologic procedures: Colposcopy, treatments for cervical intraepithelial neoplasia and endometrial assessment. Am. Fam. Physician 2013, 87, 836–843. [Google Scholar] [PubMed]
- Wentzensen, N.; Walker, J.; Smith, K.; Gold, M.A.; Zuna, R.; Massad, L.S.; Liu, A.; Silver, M.I.; Dunn, S.T.; Schiffman, M. A prospective study of risk-based colposcopy demonstrates improved detection of cervical precancers. Am. J. Obstet. Gynecol. 2018, 9378, 30153–30154. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C.M.P.; Menezes, L.J.; Paskett, E.D.; Giuliano, A.R. Prevention of invasive cervical cancer in the United States: Past, present, and future. Cancer Epidemiol. Biomarkers Prev. 2012, 21, 1402–1408. [Google Scholar] [CrossRef] [PubMed]
- Kobetz, E.; Seay, J.; Amofah, A.; Pierre, L.; Bispo, J.B.; Trevil, D.D.; Gonzalez, M.; Poitevien, M.; Koru-Sengul, T.; Carrasquillo, O. Mailed HPV self-sampling for cervical cancer screening among underserved minority women: Study protocol for a randomized controlled trial. Trials 2017, 18, 19. [Google Scholar] [CrossRef] [PubMed]
- Feldman, S. Making sense of the new cervical-cancer screening guidelines. N. Engl. J. Med. 2011, 365, 2145–2147. [Google Scholar] [CrossRef] [PubMed]
- Markt, S.C.; Tang, T.; Cronin, A.M.; Katz, I.T.; Howitt, B.E.; Horowitz, N.S.; Lee, L.J.; Wright, A.A. Insurance status and cancer treatment mediate the association between race/ethnicity and cervical cancer survival. PLoS ONE 2018, 13, e0193047. [Google Scholar] [CrossRef] [PubMed]
- Louie, K.S.; de Sanjose, S.; Diaz, M.; Castellsagué, X.; Herrero, R.; Meijer, C.J.; Shah, K.; Franceschi, S.; Muñoz, N.; Bosch, F.X. Early age at first sexual intercourse and early pregnancy are risk factors for cervical cancer in developing countries. Br. J. Cancer 2009, 100, 1191–1197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- QuickFacts. Available online: https://www.census.gov/quickfacts/tylercitytexas. (accessed on 27 July 2019).
- Flores, B.E.; Acton, G.; Arevalo-Flechas, L.; Gill, S.; Mackert, M. Health Literacy and Cervical Cancer Screening Among Mexican-American Women. Health Lit. Res. Pract. 2019, 3, e1–e8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webb, S.; Kelly, P.J.; Wickliffe, J.; Ault, K.; Ramaswamy, M. Validating self-reported cervical cancer screening among women leaving jails. PLoS ONE 2019, 14, e0219178. [Google Scholar] [CrossRef] [PubMed]
- Musa, J.; Achenbach, C.J.; O’Dwyer, L.C.; Evans, C.T.; McHugh, M.; Hou, L.; Simon, M.A.; Murphy, R.L.; Jordan, N. Effect of cervical cancer education and provider recommendation for screening on screening rates: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0183924. [Google Scholar] [CrossRef] [PubMed]

| HPV 3 | OR(95%CI) 4 | p-Value | |||
|---|---|---|---|---|---|
| Factor | Outcome | Positive N (%) | Negative N (%) | ||
| Race | White | 54 (76.1) | 17 (23.9) | Ref | 0.76 |
| Black | 18 (81.8) | 4 (18.2) | 1.42 (0.42, 4.76) | ||
| Hispanic | 13 (72.2) | 5 (27.8) | 0.82 (0.26,2.63) | ||
| Marital Status | Married/Living with partner | 29 (76.3) | 9 (23.7) | 1.18 (0.45, 3.04) | 0.74 |
| Not Married/widowed/divorced | 14 (20.9) | 53 (79.1) | Ref | ||
| BMI 1 | Normal | 26 (78.8) | 7 (21.2) | Ref | 0.94 |
| Overweight | 25 (73.5) | 9 (26.5) | 0.96 (0.32, 2.90) | ||
| Obese | 35 (79.5) | 9 (20.5) | 0.71 (0.25, 2.06) | 0.53 | |
| Insurance | Yes | 30 (88.2) | 4 (11.8) | 3.00 (0.95, 9.52) | 0.05 |
| No | 55 (71.5) | 22 (28.6) | Ref | ||
| Contraception | Yes | 51 (82.3) | 11 (17.7) | 1.93 (0.80, 4.69) | 0.14 |
| No | 36 (70.6) | 15 (29.4) | |||
| Family History of Cancer | Yes | 28 (77.8) | 8 (22.2) | 0.96 (0.33, 2.80) | 0.93 |
| No | 33 (78.6) | 9 (21.4) | |||
| Smoking Status | Yes | 27 (69.2) | 12 (30.8) | 0.55 (0.23, 1.36) | 0.19 |
| No | 57 (80.3) | 14 (19.7) | |||
| Alcohol Consumption | Yes | 17 (68.00) | 8 (32.0) | 0.60 (0.21, 1.70) | 0.34 |
| No | 46 (78.0) | 13 (22.0) | |||
| Age | Mean (standard deviation) | 32.9 (11.1) | 41.5 (12.0) | 0.94 (0.91, 0.98) | 0.002 |
| Number of Pregnancy | Mean (standard deviation) | 2.4 (1.8) | 4.1 (2.7) | 0.70 (0.55, 0.89) | 0.004 |
| Number of Births | Mean (standard deviation) | 2.0 (1.6) | 3.4 (2.2) | 0.68 (0.52, 0.89) | 0.005 |
| Age at Menarche | Mean (standard deviation) | 12.7 (1.4) | 12.5 (1.8) | 1.08 (0.59, 1.98) | 0.81 |
| Pap 2 | Negative/normal | 9 (69.2) | 4 (30.8) | Ref | 0.51 |
| LSIL | 25 (78.1) | 7 (21.9) | 1.593 (0.37, 6.74) | ||
| HSIL | 5 (83.3) | 1 (16.7) | 2.22 (0.19, 25.72) | ||
| ASCUS | 44 (80.01) | 11 (20.0) | 1.78 (0.46, 6.86) | ||
| ASCUS-H | 3 (50.0) | 3 (50.0) | 0.44 (0.06, 3.24) | ||
| AGCUS | 0 (0.0) | 0 (0.0) | - | ||
| Outcome of Colposcopy | Normal | 30 (73.2) | 11 (26.8) | Ref | 0.42 |
| Mild dysplasia | 38 (80.9) | 9 (19.1) | 1.55 (0.57, 4.22) | ||
| Moderate dysplasia | 7 (100.0) | 0 (0.0) | - | ||
| Severe dysplasia | 8 (80.0) | 2 (20.0) | 1.47 (0.27, 8.00) | ||
| Pap Test 3 | OR (95%CI) 4 | p-Value | |||
|---|---|---|---|---|---|
| Factor | Outcome | Positive N (%) | Negative N (%) | ||
| Race | White | 87 (86.1) | 14 (13.9) | Ref | 0.14 |
| Black | 33 (97.1) | 1 (2.9) | 5.31 (0.67, 42.0) | ||
| Hispanic | 29 (93.5) | 2 (6.5) | 2.33 (0.50, 10.89) | ||
| Marital Status | Married/Living with partner | 41 (80.4) | 10 (19.6) | Ref | 0.01 |
| Not Married/widowed/Divorced | 93 (93.9) | 6 (6.1) | 3.78 (1.29, 11.10) | ||
| BMI 1 | Normal | 54 (94.7) | 3 (5.3) | Ref | 0.38 |
| Overweight | 40 (83.3) | 8 (16.7) | 1.90 (0.45, 7.965) | ||
| Obese | 57 (90.5) | 6 (9.5) | 0.53 (0.17, 1.63) | 0.27 | |
| Insurance | Yes | 44 (91.7) | 4 (8.3) | 1.32 (0.41, 4.28) | 0.64 |
| No | 108 (89.32) | 13 (10.7) | Ref | ||
| Contraception | Yes | 86 (92.5) | 7 (7.5) | 1.81 (0.65, 5.00) | 0.25 |
| No | 68 (87.2) | 10 (12.8) | Ref | ||
| Family History of Cancer | Yes | 45 (83.3) | 9 (16.7) | 0.56 (0.17, 1.79) | 0.32 |
| No | 45 (90.0) | 5 (10.0) | Ref | ||
| Smoking Status | Yes | 59 (90.8) | 6 (9.2) | 1.18 (0.41, 3.35) | 0.76 |
| No | 92 (89.3) | 11 (10.7) | Ref | ||
| Alcohol Consumption | Yes | 27 (77.1) | 8 (22.9) | 0.33 (0.11, 0.99) | 0.04 |
| No | 72 (91.1) | 7 (8.9) | Ref | ||
| Age | Mean (standard deviation) | 34.0 (11.1) | 37.1 (11.4) | 0.98 (0.93, 1.02) | 0.28 |
| Number of Pregnancy | Mean (standard deviation) | 2.8 (2.2) | 2.3 (1.9) | 1.14 (0.85, 1.540) | 0.37 |
| Number of Births | Mean (standard deviation) | 2.3 (1.9) | 2.2 (1.4) | 1.04 (0.77, 1.41) | 0.79 |
| Age at Menarche | Mean (standard deviation) | 12.7 (1.4) | 12.1 (1.7) | 1.42 (0.83, 2.44) | 0.20 |
| HPV2 | Negative/normal | 22 (84.6) | 4 (15.4) | Ref | 0.38 |
| Positive | 78 (90.7) | 8 (9.3) | 1.77 (0.48, 6.44) | ||
| Outcome of Colposcopy | Normal | 53 (89.8) | 6 (10.2) | Ref | 0.63 |
| Mild dysplasia | 67 (89.3) | 8 (10.7) | 0.95 (0.31, 2.90) | ||
| Moderate dysplasia | 10 (90.9) | 1 (9.1) | 1.13 (0.12, 10.45) | ||
| Severe dysplasia | 15 (100.0) | 0 (0.0) | - | ||
| Colposcopy | OR (95%CI) 4 | p-Value | |||
|---|---|---|---|---|---|
| Factor | Outcome | Dysplasia N (%) | No Dysplasia N (%) | ||
| Race | White | 60 (63.2) | 35 (36.8) | Ref | 0.27 |
| Black | 22 (66.7) | 11 (33.32) | 1.172 (0.51, 2.69) | ||
| Hispanic | 14 (48.3) | 15 (51.7) | 0.54 (0.24, 1.26) | ||
| Marital Status | Married/Living with partner | 35 (71.4) | 14 (28.6) | Ref | 0.13 |
| Not Married/widowed/Divorced | 55 (58.5) | 39 (41.5) | 0.56 (0.27, 1.19) | ||
| BMI1 | Normal | 35 (66.0) | 18 (34.8) | Ref | 0.55 |
| Overweight | 27 (60.0) | 18 (40.0) | 1.26 (0.59, 2.71) | ||
| Obese | 37 (60.7) | 24 (39.3) | 0.97 (0.44, 2.14) | 0.95 | |
| Insurance | Yes | 28 (60.9) | 18 (39.1) | Ref | 0.87 |
| No | 71 (62.3) | 43 (37.7) | 1.06 (0.53, 2.15) | ||
| Contraception | Yes | 55 (62.5) | 33 (37.5) | 1.01 (0.54, 1.92) | 0.97 |
| No | 46 (62.2) | 28 (37.8) | Ref | ||
| Family History of Cancer | Yes | 38 (70.4) | 16 (29.6) | 1.58 (069, 3.65) | 0.28 |
| No | 27 (60.0) | 18 (40.0) | Ref | ||
| Smoking Status | Yes | 37 (61.7) | 23 (38.3) | 0.97 (0.51, 1.91) | 0.97 |
| No | 62 (62.0) | 38 (38.0) | Ref | ||
| Alcohol Consumption | Yes | 16 (48.5) | 17 (51.5) | 0.44 (0.19, 1.02) | 0.05 |
| No | 51 (68.0) | 24 (32.0) | Ref | ||
| Age | Mean (standard deviation) | 33.5 (10.7) | 35.0 (10.6) | 0.99 (0.96, 1.02) | 0.37 |
| Number of Pregnancy | Mean (standard deviation) | 3.0 (2.3) | 2.4 (1.7) | 1.16 (0.97, 1.39) | 0.10 |
| Number of Births | Mean (standard deviation) | 2.5 (2.0) | 2.1 (1.5) | 1.13 (0.92, 1.37) | 0.24 |
| Age at Menarche | Mean (standard deviation) | 12.6 (1.4) | 12.7 (1.6) | 0.96 (0.66, 1.39) | 0.82 |
| HPV2 | Negative/normal | 11 (50.0) | 11 (50.0) | Ref | 0.73 |
| Positive | 53 (63.9) | 30 (36.1) | 1.77 (0.69, 4.56) | ||
| Pap3 | Normal | 9 (56.3) | 7 (43.8) | Ref | 0.79 |
| LSIL | 40 (63.5) | 23 (36.5) | 1.35 (0.44, 4.12) | ||
| HSIL | 9 (81.8) | 2 (18.2) | 3.50 (0.57, 21.67) | ||
| ASCUS | 33 (62.3) | 20 (37.7) | 1.28 (0.41, 3.99) | ||
| ASCUS-H | 7 (63.6) | 4 (36.4) | 1.36 (0.28, 6.58) | ||
| AGCUS | 3 (50.0) | 3 (50.0) | 0.78 (0.12, 5.10) | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olusola, P.; Ousley, K.; Ndetan, H.; Singh, K.P.; Banerjee, H.N.; Dasgupta, S. Cervical Cancer Prevention in Racially Disparate Rural Populations. Medicines 2019, 6, 93. https://doi.org/10.3390/medicines6030093
Olusola P, Ousley K, Ndetan H, Singh KP, Banerjee HN, Dasgupta S. Cervical Cancer Prevention in Racially Disparate Rural Populations. Medicines. 2019; 6(3):93. https://doi.org/10.3390/medicines6030093
Chicago/Turabian StyleOlusola, Patti, Kia Ousley, Harrison Ndetan, Karan P. Singh, Hirendra Nath Banerjee, and Santanu Dasgupta. 2019. "Cervical Cancer Prevention in Racially Disparate Rural Populations" Medicines 6, no. 3: 93. https://doi.org/10.3390/medicines6030093
APA StyleOlusola, P., Ousley, K., Ndetan, H., Singh, K. P., Banerjee, H. N., & Dasgupta, S. (2019). Cervical Cancer Prevention in Racially Disparate Rural Populations. Medicines, 6(3), 93. https://doi.org/10.3390/medicines6030093