Vacuum and Electromagnetic Fields Treatment to Regenerate a Diffuse Mature Facial Scar Caused by Sulfuric Acid Assault
Abstract
:1. Introduction
V-EMF Treatment
2. Materials and Methods
2.1. Case
2.2. Methods
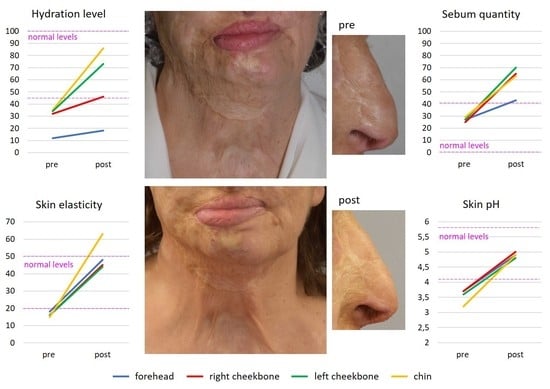
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rasouli, H.R.; Ebrahimi, A.; Motamedi, M.H.K. Raising awareness against acid attacks. Lancet 2015, 385, 772–773. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Maroof, H.; Ahmed, N.; Sheridan, R. Acid attacks: A new public health pandemic in the west? Int. J. Surg. 2017, 48, 32–33. [Google Scholar] [CrossRef] [PubMed]
- Mannan, A.; Ghani, S.; Clarke, A.; Butler, P.E. Cases of chemical assault worldwide: A literature review. Burns 2007, 33, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Karunadasa, K.P.; Perera, C.; Kanagaratnum, V.; Wijerathne, U.P.; Samarasingha, I.; Kannangara, C.K. Burns due to Acid Assaults in Sri Lanka. J. Burn Care Res. 2010, 31, 781–785. [Google Scholar] [CrossRef] [PubMed]
- Peck, M.D. Epidemiology of burns throughout the World. Part II: Intentional burns in adults. Burns 2012, 38, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Herndon, D. Total Burn Care, 5th ed.; Elsevier Saunders: New York, NY, USA, 2017. [Google Scholar]
- Micheau, P.; Lauwers, F.; Vath, S.B.; Seilha, T.C.; Dumurgier, C.; Joly, B. Brûlures caustiques. Étude clinique à propos de 24 observations de brûlures par acide sulfurique au Cambodge [Caustic burns. Clinical study of 24 patients with sulfuric acid burns in Cambodia]. Ann. Chir. Plast. Esthet. 2004, 49, 239–254. [Google Scholar] [CrossRef]
- Behera, C.; Rani, A.; Pradhan, M.; Dikshit, P.C. Fatal corrosive attack: A study of 13 cases from central Delhi, India. Am. J. Forensic Med. Pathol. 2014, 35, 109–112. [Google Scholar] [CrossRef]
- Van Loey, N.E.E.; Van Son, M.J.M. Psychopathology and psychological problems in patients with burn scars: Epidemiology and management. Am. J. Clin. Dermatol. 2003, 4, 245–272. [Google Scholar] [CrossRef]
- Yu, B.-H.; Dimsdale, J.E. Posttraumatic stress disorder in patients with burn injuries. J. Burn Care Rehabil. 1999, 20, 426–433, discussion 422–425. [Google Scholar] [CrossRef]
- Lodha, P.; Shah, B.; Karia, S.; De Sousa, A. Post-Traumatic Stress Disorder (Ptsd) following burn injuries: A comprehensive clinical review. Ann. Burn. Fire Disasters 2020, 33, 276–287. [Google Scholar]
- De Sousa, A.; Sonavane, S.; Kurvey, A. Psychological issues in adult burn patients. Delhi Psychiatry J. 2013, 16, 24–33. [Google Scholar]
- Öster, C.; Sveen, J. The psychiatric sequelae of burn injury. Gen. Hosp. Psychiatry 2014, 36, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Tebble, N.J.; Adams, R.; Thomas, D.W.; Price, P. Anxiety and self-consciousness in patients with facial lacerations one week and six months later. Br. J. Oral Maxillofac. Surg. 2006, 44, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Van den Elzen, M.E.; Versnel, S.L.; Hovius, S.E.; Passchier, J.; Duivenvoorden, H.J.; Mathijssen, I.M. Adults with congenital or acquired facial disfigurement: Impact of appearance on social functioning. J. Cranio-Maxillofac. Surg. 2012, 40, 777–782. [Google Scholar] [CrossRef]
- Hoogewerf, C.J.; van Baar, M.E.; Middelkoop, E.; van Loey, N.E. Impact of facial burns: Relationship between depressive symptoms, self-esteem and scar severity. Gen. Hosp. Psychiatry 2014, 36, 271–276. [Google Scholar] [CrossRef] [Green Version]
- Ziolkowski, N.; Kitto, S.C.; Jeong, D.; Zuccaro, J.; Adams-Webber, T.; Miroshnychenko, A.; Fish, J.S. Psychosocial and quality of life impact of scars in the surgical, traumatic and burn populations: A scoping review protocol. BMJ Open 2019, 9, e021289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewis, C.J.; Al-Mousawi, A.; Jha, A.; Allison, K.P. Is it time for a change in the approach to chemical burns? The role of Diphoterine® in the management of cutaneous and ocular chemical injuries. J. Plast. Reconstr. Aesthetic Surg. 2017, 70, 563–567. [Google Scholar] [CrossRef]
- Gnaneswaran, N.; Perera, E.; Perera, M.; Sawhney, R. Cutaneous chemical burns: Assessment and early management. Aust. Fam. Physician 2015, 44, 135–139. [Google Scholar]
- Press, B. Thermal, electrical and chemical injuries. In Grabb and Smiths’ Plastic Surgery, 5th ed.; Sherrel, J., Aston, M.D., Eds.; Raven Press: New York, NY, USA, 1997; pp. 161–189. [Google Scholar]
- Yeong, E.K.; Chen, M.T.; Mann, R.; Lin, T.-W.; Engrav, L.H. Facial mutilation after an assault with chemicals: 15 cases and literature review. J. Burn Care Rehabil. 1997, 18, 234–237. [Google Scholar] [CrossRef]
- Matshes, E.W.; Taylor, K.A.; Rao, V.J. Sulfuric acid injury. Am. J. Forensic Med. Pathol. 2008, 29, 340–345. [Google Scholar] [CrossRef]
- Akhtar, S.; Kanungo, S.; Khurram, M.F.; Ahmad, I. Epidemiology and outcome of chemical burn patients admitted in Burn Unit of JNMC Hospital, Aligarh Muslim University, Aligarh, Uttar Pradesh, India: A 5-year experience. J. Fam. Med. Prim. Care 2015, 4, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Das, K.K.; Olga, L.; Peck, M.; Morselli, P.G.; Salek, A.J. Management of acid burns: Experience from Bangladesh. Burns 2015, 41, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Hsu, K.-C.; Luan, C.-W.; Tsai, Y.-W. Review of silicone gel sheeting and silicone gel for the prevention of hypertrophic scars and keloids. Wounds A Compend. Clin. Res. Pract. 2017, 29, 154–158. [Google Scholar]
- Tran, B.; Wu, J.J.; Ratner, D.; Han, G. Topical scar treatment products for wounds: A systematic review. Dermatol. Surg. 2020, 46, 1564–1571. [Google Scholar] [CrossRef]
- Shin, J.Y.; Yun, S.-K.; Roh, S.-G.; Lee, N.-H.; Yang, K.-M. Efficacy of 2 representative topical agents to prevent keloid recurrence after surgical excision. J. Oral Maxillofac. Surg. 2017, 75, 401.e1–401.e6. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Wang, H.; Yang, B.; Sun, Y.; Huo, R. Three-dimensional graphene foams loaded with bone marrow derived mesenchymal stem cells promote skin wound healing with reduced scarring. Mater. Sci. Eng. C 2015, 57, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Kant, S.B.; van den Kerckhove, E.; Colla, C.; Tuinder, S.; van der Hulst, R.R.W.J.; de Grzymala, A.A.P. A new treatment of hypertrophic and keloid scars with combined triamcinolone and verapamil: A retrospective study. Eur. J. Plast. Surg. 2018, 41, 69–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sohrabi, C.; Goutos, I. The use of botulinum toxin in keloid scar management: A literature review. Scars Burn. Health 2020, 6, 2059513120926628. [Google Scholar] [CrossRef]
- Krastev, T.K.; Schop, S.J.; Hommes, J.; Piatkowski, A.; van der Hulst, R.R.W.J. Autologous fat transfer to treat fibrosis and scar-related conditions: A systematic review and meta-analysis. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 2033–2048. [Google Scholar] [CrossRef]
- Klinger, M.; Klinger, F.; Caviggioli, F.; Maione, L.; Catania, B.; Veronesi, A.; Giannasi, S.; Bandi, V.; Giaccone, M.; Siliprandi, M.; et al. Fat Grafting for treatment of facial scars. Clin. Plast. Surg. 2020, 47, 131–138. [Google Scholar] [CrossRef]
- To, K.; Crowley, C.; Lim, S.-K.; Khan, W.S. Autologous adipose tissue grafting for the management of the painful scar. Cytotherapy 2019, 21, 1151–1160. [Google Scholar] [CrossRef] [PubMed]
- Grablowitz, D.; Ivezic-Schoenfeld, Z.; Federspiel, I.G.; Gehl, B.; Kopera, D.; Prinz, M. Long-term effectiveness of a hyaluronic acid soft tissue filler in patients with facial lipoatrophy, morphological asymmetry, or debilitating scars. J. Cosmet. Dermatol. 2020, 19, 2536–2541. [Google Scholar] [CrossRef] [PubMed]
- Riccio, M.; Marchesini, A.; Senesi, L.; Skrami, E.; Gesuita, R.; De Francesco, F. Managing pathologic scars by injecting auto-cross-linked hyaluronic acid: A preliminary prospective clinical study. Aesthetic Plast. Surg. 2019, 43, 480–489. [Google Scholar] [CrossRef] [PubMed]
- Van Leeuwen, M.C.E.; Van Der Wal, M.B.A.; Bulstra, A.-E.J.; Galindo-Garre, F.; Molier, J.; Van Zuijlen, P.P.M.; Van Leeuwen, P.A.M.; Niessen, F.B. Intralesional cryotherapy for treatment of keloid scars: A prospective study. Plast. Reconstr. Surg. 2015, 135, 580–589. [Google Scholar] [CrossRef]
- Peng, W.; Zhang, X.; Kong, X.; Shi, K. The efficacy and safety of fractional CO2 laser therapy in the treatment of burn scars: A meta-analysis. Burns 2021, 47, 1469–1477. [Google Scholar] [CrossRef]
- Meynköhn, A.; Fischer, S.; Neuss, C.; Willkomm, L.M.; Kneser, U.; Kotsougiani-Fischer, D. Fractional ablative carbon dioxide laser treatment of facial scars: Improvement of patients’ quality of life, scar quality, and cosmesis. J. Cosmet. Dermatol. 2021, 20, 2132–2140. [Google Scholar] [CrossRef]
- Taudorf, E.H.; Danielsen, P.L.; Paulsen, I.F.; Togsverd-Bo, K.; Dierickx, C.; Paasch, U.; Haedersdal, M. Non-ablative fractional laser provides long-term improvement of mature burn scars-A randomized controlled trial with histological assessment. Lasers Surg. Med. 2015, 47, 141–147. [Google Scholar] [CrossRef]
- Moortgat, P.; Anthonissen, M.; Van Daele, U.; Vanhullebusch, T.; Maertens, K.; De Cuyper, L.; Lafaire, C.; Meirte, J. The effects of shock wave therapy applied on hypertrophic burn scars: A randomised controlled trial. Scars Burn. Health 2020, 6, 2059513120975624. [Google Scholar] [CrossRef]
- Wang, S.; Mi, J.; Li, Q.; Jin, R.; Dong, J. Fractional microplasma radiofrequency technology for non-hypertrophic post-burn scars in Asians: A prospective study of 95 patients. Lasers Surg. Med. 2017, 49, 563–569. [Google Scholar] [CrossRef]
- Juhasz, M.L.W.; Cohen, J.L. Microneedling for the treatment of scars: An update for clinicians. Clin. Cosmet. Investig. Dermatol. 2020, 13, 997–1003. [Google Scholar] [CrossRef]
- Yu, P.-X.; Diao, W.-Q.; Qi, Z.-L.; Cai, J.-L. Effect of dermabrasion and ReCell® on large superficial facial scars caused by burn, trauma and acnes. Chin. Med. Sci. J. 2016, 31, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Barone, N.; Safran, T.; Vorstenbosch, J.; Davison, P.G.; Cugno, S.; Murphy, A.M. Current advances in hypertrophic scar and keloid management. Semin. Plast. Surg. 2021, 35, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Berman, B.; Maderal, A.; Raphael, B. Keloids and hypertrophic scars: Pathophysiology, classification, and treatment. Dermatol. Surg. 2017, 43, S3–S18. [Google Scholar] [CrossRef] [PubMed]
- Veronese, S.; Beatini, A.; Urbani, C.; Lanza, E.; Paz, O.M.; Saussaye, Y.; Lomuto, M.; Sbarbati, A. V-EMF treatment of facial scar: First results. J. Tissue Viability 2022. [Google Scholar] [CrossRef]
- Coccetta, C.A.; Sale, P.; Ferrara, P.E.; Specchia, A.; Maccauro, G.; Ferriero, G.; Ronconi, G. Effects of capacitive and resistive electric transfer therapy in patients with knee osteoarthritis: A randomized controlled trial. Int. J. Rehabil. Res. 2019, 42, 106–111. [Google Scholar] [CrossRef]
- De Sousa-De Sousa, L.; Tebar Sanchez, C.; Maté-Muñoz, J.L.; Hernández-Lougedo, J.; Barba, M.; Lozano-Estevan, M.D.C.; Garnacho-Castaño, M.V.; García-Fernández, P. Application of capacitive-resistive electric transfer in physiotherapeutic clinical practice and sports. Int. J. Environ. Res. Public Health 2021, 18, 12446. [Google Scholar] [CrossRef]
- Nadler, S.F.; Weingand, K.; Kruse, R.J. The physiologic basis and clinical applications of cryotherapy and thermotherapy for the pain practitioner. Pain Physician 2004, 7, 395–399. [Google Scholar] [CrossRef]
- Xuan, X. Joule heating in electrokinetic flow. Electrophoresis 2008, 29, 33–43. [Google Scholar] [CrossRef]
- Song, L.; Yu, L.; Brumme, C.; Shaw, R.; Zhang, C.; Xuan, X. Joule heating effects on electrokinetic flows with conductivity gradients. Electrophoresis 2021, 42, 967–974. [Google Scholar] [CrossRef]
- Tang, G.Y.; Yang, C.; Chai, J.C.; Gong, H.Q. Joule heating effect on electroosmotic flow and mass species transport in a microcapillary. Int. J. Heat Mass Transf. 2004, 47, 215–227. [Google Scholar] [CrossRef]
- Kim, D.; Han, S.A.; Kim, J.H.; Lee, J.-H.; Kim, S.-W.; Lee, S.-W. Biomolecular piezoelectric materials: From amino acids to living tissues. Adv. Mater. 2020, 32, e1906989. [Google Scholar] [CrossRef] [PubMed]
- Lay, R.; Deijs, G.S.; Malmström, J. The intrinsic piezoelectric properties of materials—A review with a focus on biological materials. RSC Adv. 2021, 11, 30657–30673. [Google Scholar] [CrossRef] [PubMed]
- Hawamdeh, M. The effectiveness of capacitive resistive diathermy (Tecartherapy®) in acute and chronic musculoskeletal lesions and pathologies. Eur. J. Sci. Res. 2014, 118, 336–340. [Google Scholar]
- Malanga, G.A.; Yan, N.; Stark, J. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgrad. Med. 2015, 127, 57–65. [Google Scholar] [CrossRef]
- Mace, T.A.; Zhong, L.; Kokolus, K.M.; Repasky, E.A. Effector CD8+T cell IFN-γproduction and cytotoxicity are enhanced by mild hyperthermia. Int. J. Hyperth. 2012, 28, 9–18. [Google Scholar] [CrossRef]
- Tashiro, Y.; Hasegawa, S.; Yokota, Y.; Nishiguchi, S.; Fukutani, N.; Shirooka, H.; Tasaka, S.; Matsushita, T.; Matsubara, K.; Nakayama, Y.; et al. Effect of Capacitive and Resistive electric transfer on haemoglobin saturation and tissue temperature. Int. J. Hyperth. 2017, 33, 696–702. [Google Scholar] [CrossRef] [Green Version]
- Shields, N.; Gormley, J.; O’Hare, N. Short-wave diathermy: Current clinical and safety practices. Physiother. Res. Int. 2002, 7, 191–202. [Google Scholar] [CrossRef]
- Yokota, Y.; Sonoda, T.; Tashiro, Y.; Suzuki, Y.; Kajiwara, Y.; Zeidan, H.; Nakayama, Y.; Kawagoe, M.; Shimoura, K.; Tatsumi, M.; et al. Effect of Capacitive and Resistive electric transfer on changes in muscle flexibility and lumbopelvic alignment after fatiguing exercise. J. Phys. Ther. Sci. 2018, 30, 719–725. [Google Scholar] [CrossRef] [Green Version]
- Bito, T.; Tashiro, Y.; Suzuki, Y.; Kajiwara, Y.; Zeidan, H.; Kawagoe, M.; Sonoda, T.; Nakayama, Y.; Yokota, Y.; Shimoura, K.; et al. Acute effects of capacitive and resistive electric transfer (CRet) on the Achilles tendon. Electromagn. Biol. Med. 2019, 38, 48–54. [Google Scholar] [CrossRef]
- Raeisi, M.; Mohammadi, H.K.; Heshmatipour, M.; Tarrahi, M.J.; Taheri, N. Effect of transfer energy capacitive and resistive therapy on shoulder pain, disability, and range of motion in patients with adhesive capsulitis: A study protocol for a randomized controlled trial. J. Chiropr. Med. 2022. [Google Scholar] [CrossRef]
- Nair, M.; Calahorra, Y.; Kar-Narayan, S.; Best, S.M.; Cameron, R.E. Self-assembly of collagen bundles and enhanced piezoelectricity induced by chemical crosslinking. Nanoscale 2019, 11, 15120–15130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farahani, R.M.; Kloth, L.C. The hypothesis of ‘biophysical matrix contraction’: Wound contraction revisited. Int. Wound J. 2008, 5, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Beck-Broichsitter, B.E.; Lamia, A.; Geuna, S.; Fregnan, F.; Smeets, R.; Becker, S.T.; Sinis, N. Does pulsed magnetic field therapy influence nerve regeneration in the median nerve model of the rat? BioMed Res. Int. 2014, 2014, 401760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gunay, I.; Mert, T. Pulsed magnetic fields enhance the rate of recovery of damaged nerve excitability. Bioelectromagnetics 2011, 32, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Mert, T.; Günay, I.; Gocmen, C.; Kaya, M.; Polat, S. Regenerative effects of pulsed magnetic field on injured peripheral nerves. Altern. Ther. Health Med. 2006, 12, 42–49. [Google Scholar]
- Haastert-Talini, K.; Grothe, C. Electrical stimulation for promoting peripheral nerve regeneration. Int. Rev. Neurobiol. 2013, 109, 111–124. [Google Scholar] [CrossRef]
- Meirte, J.; Moortgat, P.; Anthonissen, M.; Maertens, K.; Lafaire, C.; De Cuyper, L.; Hubens, G.; Van Daele, U. Short-term effects of vacuum massage on epidermal and dermal thickness and density in burn scars: An experimental study. Burn. Trauma 2016, 4, 27. [Google Scholar] [CrossRef] [Green Version]
- Moortgat, P.; Anthonissen, M.; Meirte, J.; Van Daele, U.; Maertens, K. The physical and physiological effects of vacuum massage on the different skin layers: A current status of the literature. Burn. Trauma 2016, 4, 34. [Google Scholar] [CrossRef] [Green Version]
- Chai, H.; Chaudhari, N.; Kornhaber, R.; Cuttle, L.; Fear, M.; Wood, F.; Martin, L. Chemical burn to the skin: A systematic review of first aid impacts on clinical outcomes. Burns 2022, 48, 1527–1543. [Google Scholar] [CrossRef]
- Claytor, R.B.; Sheck, C.G.; Chopra, V. Microneedling outcomes in early post-surgical scars. Plast. Reconstr. Surg. 2022, 150, 557e–561e. [Google Scholar] [CrossRef]
- De Oliveira, G.V.; Gold, M.H. Silicone sheets and new gels to treat hypertrophic scars and keloids: A short review. Dermatol. Ther. 2020, 33, e13705. [Google Scholar] [CrossRef] [PubMed]
- Nicoletti, G.; Perugini, P.; Bellino, S.; Capra, P.; Malovini, A.; Jaber, O.; Tresoldi, M.; Faga, A. Scar remodeling with the association of monopolar capacitive radiofrequency, electric stimulation, and negative pressure. Photomed. Laser Surg. 2017, 35, 246–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alberti, G.; Laura, S. Treatment of stretch marks aged more than twenty years with the synergy of electromagnetic field and vacuum. Clinical case studies and subsequent follow-up. Aesthetic Med. 2019, 5, 14–21. [Google Scholar]
- Scarano, A.; Sbarbati, A.; Amore, R.; Iorio, E.L.; Ferraro, G.; Lorusso, F.; Amuso, D. A New Treatment for stretch marks and skin ptosis with electromagnetic fields and negative pressure: A clinical and histological study. J. Cutan. Aesthet. Surg. 2021, 14, 222–228. [Google Scholar] [CrossRef]
- Bacci, P.A.; Alberti, G.; Amuso, D.; Artigiani, A.; Benitez Roig, V.; Di Nardo, V.; Garcia-Gimenez, V.; Greco, D.; Laura, S.; Pagano, M.; et al. The synergy between vacuum and electromagnetic fields in the treatment of striae distensae: Retrospective study on 917 patients with clinical and histological case records. J. Appl. Cosmetol. 2021, 39, 43–54. [Google Scholar]
- Curtis, K.; Kennedy, B.; Lam, M.K.; Mitchell, R.J.; Black, D.; Burns, B.; White, L.; Loudfoot, A.; D’Amato, A.; Dinh, M.; et al. Cause, treatment costs and 12-month functional outcomes of children with major injury in NSW, Australia. Injury 2020, 51, 2066–2075. [Google Scholar] [CrossRef] [PubMed]
- Baker, C.P.; Russell, W.J.; Meyer, W., III; Blakeney, P. Physical and psychologic rehabilitation outcomes for young adults burned as children. Arch. Phys. Med. Rehabil. 2007, 88 (Suppl. 2), S57–S64. [Google Scholar] [CrossRef]
- Blakeney, P.E.; Rosenberg, L.; Rosenberg, M.; Faber, A.W. Psychosocial care of persons with severe burns. Burns 2008, 34, 433–440. [Google Scholar] [CrossRef]

| Invasiveness | Type | References |
|---|---|---|
| Non-invasive | Silicone sheet coating | [25] |
| Topical treatment | [26,27] | |
| Application of mesenchymal stem cells in tissue scaffolds | [28] | |
| Minimally invasive | Corticosteroid injection | [29] |
| (principally injectable therapies) | Botox injection | [30] |
| Mesenchymal stem cells injection (principally obtained from fat grafting) | [31,32,33] | |
| Hyaluronic acid filler | [34,35] | |
| Invasive | Cryotherapy (generally applied after surgical excision) | [36] |
| Others (more/less invasive) | Laser - minimally invasive—non-ablative - invasive—ablative | [37,38,39] |
| Shock wave therapy | [40] | |
| Radiofrequencies application | [41] | |
| Microneedling | [42] | |
| Dermabrasion (combined with regenerative agents) | [43] |
| Forehead | Right Cheekbone | Left Cheekbone | Chin | |||||
|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T0 | T1 | T0 | T1 | T0 | T1 | |
| Hydration Level | 12 | 18 * | 32 | 46 | 35 | 86 | 34 | 73 |
| normal value | >44/100 | |||||||
| Sebum Quantity | 27 | 43 ** | 25 | 65 ** | 27 | 70 ** | 29 | 63 ** |
| normal value | <40/100 | |||||||
| Skin Elasticity | 18 | 48 | 16 | 45 | 16 | 44 | 15 | 63 ** |
| normal value | >20/50 | |||||||
| Skin pH | 3.7 | 4.9 | 3.6 | 5.0 | 3.6 | 4.8 | 3.2 | 4.9 |
| normal range | 4.1–5.8 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veronese, S.; Brunetti, B.; Minichino, A.M.; Sbarbati, A. Vacuum and Electromagnetic Fields Treatment to Regenerate a Diffuse Mature Facial Scar Caused by Sulfuric Acid Assault. Bioengineering 2022, 9, 799. https://doi.org/10.3390/bioengineering9120799
Veronese S, Brunetti B, Minichino AM, Sbarbati A. Vacuum and Electromagnetic Fields Treatment to Regenerate a Diffuse Mature Facial Scar Caused by Sulfuric Acid Assault. Bioengineering. 2022; 9(12):799. https://doi.org/10.3390/bioengineering9120799
Chicago/Turabian StyleVeronese, Sheila, Bruno Brunetti, Anna Maria Minichino, and Andrea Sbarbati. 2022. "Vacuum and Electromagnetic Fields Treatment to Regenerate a Diffuse Mature Facial Scar Caused by Sulfuric Acid Assault" Bioengineering 9, no. 12: 799. https://doi.org/10.3390/bioengineering9120799
APA StyleVeronese, S., Brunetti, B., Minichino, A. M., & Sbarbati, A. (2022). Vacuum and Electromagnetic Fields Treatment to Regenerate a Diffuse Mature Facial Scar Caused by Sulfuric Acid Assault. Bioengineering, 9(12), 799. https://doi.org/10.3390/bioengineering9120799