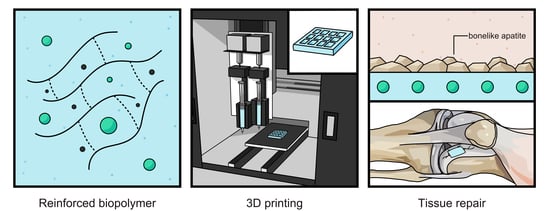
Reinforcement of Alginate-Gelatin Hydrogels with Bioceramics for Biomedical Applications: A Comparative Study
Abstract
:1. Introduction
2. Methodology
2.1. Particles Synthesis
2.2. Hydrogels Preparation
2.3. Instrumentation for Chemical and Mechanical Characterization
2.4. 3D Printing
2.5. Cell Culture and Cell Viability Assay
3. Results and Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Murphy, S.V.; Atala, A. 3D Bioprinting of Tissues and Organs. Nat. Biotechnol. 2014, 32, 773–785. [Google Scholar] [CrossRef]
- Moiduddin, K.; Mian, S.H.; Umer, U.; Alkhalefah, H. Fabrication and Analysis of a Ti6Al4V Implant for Cranial Restoration. NATO Adv. Sci. Inst. Ser. E Appl. Sci. 2019, 9, 2513. [Google Scholar] [CrossRef] [Green Version]
- Norioka, C.; Inamoto, Y.; Hajime, C.; Kawamura, A.; Miyata, T. A Universal Method to Easily Design Tough and Stretchable Hydrogels. NPG Asia Mater. 2021, 13, 1–10. [Google Scholar] [CrossRef]
- Chyzy, A.; Plonska-Brzezinska, M.E. Hydrogel Properties and Their Impact on Regenerative Medicine and Tissue Engineering. Molecules 2020, 25, 5795. [Google Scholar] [CrossRef]
- Huang, J.; Xiong, J.; Wang, D.; Zhang, J.; Yang, L.; Sun, S.; Liang, Y. 3D Bioprinting of Hydrogels for Cartilage Tissue Engineering. Gels 2021, 7, 144. [Google Scholar] [CrossRef]
- Łabowska, M.B.; Cierluk, K.; Jankowska, A.M.; Kulbacka, J.; Detyna, J.; Michalak, I. A Review on the Adaption of Alginate-Gelatin Hydrogels for 3D Cultures and Bioprinting. Materials 2021, 14, 858. [Google Scholar] [CrossRef]
- Chen, C.-Y.; Shie, M.-Y.; Lee, A.K.-X.; Chou, Y.-T.; Chiang, C.; Lin, C.-P. 3D-Printed Ginsenoside Rb1-Loaded Mesoporous Calcium Silicate/Calcium Sulfate Scaffolds for Inflammation Inhibition and Bone Regeneration. Biomedcines 2021, 9, 907. [Google Scholar] [CrossRef]
- Gomez-Florit, M.; Pardo, A.; Domingues, R.M.A.; Graça, A.L.; Babo, P.S.; Reis, R.L.; Gomes, M.E. Natural-Based Hydrogels for Tissue Engineering Applications. Molecules 2020, 25, 5858. [Google Scholar] [CrossRef]
- Daly, A.C.; Riley, L.; Segura, T.; Burdick, J.A. Hydrogel Microparticles for Biomedical Applications. Nat. Rev. Mater. 2019, 5, 20–43. [Google Scholar] [CrossRef]
- Lynch, C.R.; Kondiah, P.P.D.; Choonara, Y.E. Advanced Strategies for Tissue Engineering in Regenerative Medicine: A Biofabrication and Biopolymer Perspective. Molecules 2021, 26, 2518. [Google Scholar] [CrossRef]
- Pérez-Pedroza, R.; Ávila-Ramírez, A.; Khan, Z.; Moretti, M.; Hauser, C.A.E. Supramolecular Biopolymers for Tissue Engineering. Adv. Polym. Technol. 2021, 2021, 1–23. [Google Scholar] [CrossRef]
- Rapid Prototyping in Tissue Engineering: Challenges and Potential. Trends Biotechnol. 2004, 22, 643–652. [CrossRef]
- Zhai, X.; Ma, Y.; Hou, C.; Gao, F.; Zhang, Y.; Ruan, C.; Pan, H.; Lu, W.W.; Liu, W. 3D-Printed High Strength Bioactive Supramolecular Polymer/Clay Nanocomposite Hydrogel Scaffold for Bone Regeneration. ACS Biomater. Sci. Eng. 2017, 3, 1109–1118. [Google Scholar] [CrossRef]
- Rentería-Zamarrón, D.; Cortés-Hernández, D.A.; Bretado-Aragón, L.; Ortega-Lara, W. Mechanical Properties and Apatite-Forming Ability of PMMA Bone Cements. Mater. Des. 2009, 30, 3318–3324. [Google Scholar] [CrossRef]
- Greer, A.I.M.; Goriainov, V.; Kanczler, J.; Black, C.R.M.; Turner, L.-A.; Meek, R.M.D.; Burgess, K.; MacLaren, I.; Dalby, M.J.; Oreffo, R.O.C.; et al. Nanopatterned Titanium Implants Accelerate Bone Formation In Vivo. ACS Appl. Mater. Inter-faces 2020, 12, 33541–33549. [Google Scholar] [CrossRef]
- Webber, R.E.; Shull, K.R. Strain Dependence of the Viscoelastic Properties of Alginate Hydrogels. Macromolecules 2004, 37, 6153–6160. [Google Scholar] [CrossRef]
- Lou, X.; Chirila, T.V. Swelling Behavior and Mechanical Properties of Chemically Cross-Linked Gelatin Gels for Biomedical Use. J. Biomater. Appl. 1999, 14, 184–191. [Google Scholar] [CrossRef]
- Urruela-Barrios, R.; Ramírez-Cedillo, E.; de León, A.D.; Alvarez, A.; Ortega-Lara, W. Alginate/Gelatin Hydrogels Reinforced with TiO2 and β-TCP Fabricated by Microextrusion-Based Printing for Tissue Regeneration. Polymers 2019, 11, 457. [Google Scholar] [CrossRef] [Green Version]
- Urruela Barrios, R.A. Technological Development of Alginate/Gelatin Composite Hydrogel Fabricated by Microextrusion Based Printing for Tissue Regeneration. Repos TEC 2018. Available online: https://repositorio.tec.mx/handle/11285/629912 (accessed on 28 September 2021).
- Qi, X.; Pei, P.; Zhu, M.; Du, X.; Xin, C.; Zhao, S.; Li, X.; Zhu, Y. Three Dimensional Printing of Calcium Sulfate and Mesopo-rous Bioactive Glass Scaffolds for Improving Bone Regeneration in Vitro and in Vivo. Sci. Rep. 2017, 7, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Luo, Y.; Zhai, D.; Huan, Z.; Zhu, H.; Xia, L.; Chang, J.; Wu, C. Three-Dimensional Printing of Hollow-Struts-Packed Bioceram-ic Scaffolds for Bone Regeneration. ACS Appl. Mater. Interfaces 2015, 7, 24377–24383. [Google Scholar] [CrossRef]
- Abbas, S.; Maleksaeedi, S.; Kolos, E.; Ruys, A.J. Processing and Properties of Zirconia-Toughened Alumina Prepared by Gelcasting. Materials 2015, 8, 4344–4362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bone Tissue Engineering in Osteoporosis. Maturitas 2013, 75, 118–124. [CrossRef]
- Safari, B.; Aghanejad, A.; Roshangar, L.; Davaran, S. Osteogenic Effects of the Bioactive Small Molecules and Minerals in the Scaffold-Based Bone Tissue Engineering. Colloids Surf. B Biointerfaces 2021, 198, 111462. [Google Scholar] [CrossRef] [PubMed]
- Baino, F.; Novajra, G.; Vitale-Brovarone, C. Bioceramics and Scaffolds: A Winning Combination for Tissue Engineering. Front. Bioeng. Biotechnol. 2015, 3, 202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Design and Characterization of Gelatin/PVA Hydrogels Reinforced with Ceramics for 3D Printed Prosthesis. Mater. Today Proc. 2019, 13, 324–331. [CrossRef]
- Ortega-Lara, W.; Cortés-Hernández, D.A.; Best, S.; Brooks, R.; Bretado-Aragón, L.; Rentería-Zamarrón, D. In Vitro Bioactivity of Wollastonite–titania Materials Obtained by Sol–gel Method or Solid State Reaction. J. Sol-Gel Sci. Technol. 2008, 48, 362–368. [Google Scholar] [CrossRef]
- Lara, O.; de Lourdes, W. Síntesis, Caracterización y Aplicación de Compuestos Cerámicos del tipo M2Ti6O13(M=Li+, Na+ K+) Como Agentes Fotocatalíticos. Master’s Thesis, Universidad Autónoma de Nuevo León, San Nicolás de los Garza, Mexico, 2003. [Google Scholar]
- Vamvasakis, I.; Georgaki, I.; Vernardou, D.; Kenanakis, G.; Katsarakis, N. Synthesis of WO3 Catalytic Powders: Evaluation of Photocatalytic Activity under NUV/visible Light Irradiation and Alkaline Reaction pH. J. Sol-Gel Sci. Technol. 2015, 1, 120–128. [Google Scholar] [CrossRef]
- Li, Z.; Huang, S.; Liu, Y.; Yao, B.; Hu, T.; Shi, H.; Xie, J.; Fu, X. Tuning Alginate-Gelatin Bioink Properties by Varying Solvent and Their Impact on Stem Cell Behavior. Sci. Rep. 2018, 8, 1–8. [Google Scholar] [CrossRef] [Green Version]
- New Gel-Casting Process for Alumina Ceramics Based on Gelation of Alginate. J. Eur. Ceram. Soc. 2002, 22, 1911–1916. [CrossRef]
- Wang, S.; Lee, J.M.; Yeong, W.Y. Smart Hydrogels for 3D Bioprinting. Int. J. Bioprinting 2015, 1. [Google Scholar] [CrossRef] [Green Version]
- Mechanical Behaviour of Alginate-Gelatin Hydrogels for 3D Bioprinting. J. Mech. Behav. Biomed. Mater. 2018, 79, 150–157. [CrossRef]
- Mondal, A.; Gebeyehu, A.; Miranda, M.; Bahadur, D.; Patel, N.; Ramakrishnan, S.; Rishi, A.K.; Singh, M. Characterization and Printability of Sodium Alginate -Gelatin Hydrogel for Bioprinting NSCLC Co-Culture. Sci. Rep. 2019, 9, 1–12. [Google Scholar] [CrossRef]
- 3D Printing of Hydrogels: Rational Design Strategies and Emerging Biomedical Applications. Mater. Sci. Eng. R Rep. 2020, 140, 100543. [CrossRef]
- Pour, M.M.; Saberi-Riseh, R.; Mohammadinejad, R.; Hosseini, A. Investigating the Formulation of Alginate- Gelatin Encapsu-lated Pseudomonas Fluorescens (VUPF5 and T17-4 Strains) for Controlling Fusarium Solani on Potato. Int. J. Biol. Macromol. 2019, 133, 603–613. [Google Scholar] [CrossRef]
- Functional Crystals. In Modern Inorganic Synthetic Chemistry; Elsevier: Amsterdam, The Netherlands, 2017; pp. 575–611. [CrossRef]
- Avila-Ramírez, A.; Valle-Perez, A.; Susapto, H.; Perez-Pedroza, R.; RBriola, G.; Alrashoudi, A.; Khan, Z.; Bilalis, P.; Hauser, C. Ecologically Friendly Biofunctional Ink for Reconstruction of Rigid Living Systems Under Wet Conditions. Int. J. Bioprinting 2021, 7. [Google Scholar] [CrossRef]
- Sofronia, A.M.; Baies, R.; Anghel, E.M.; Marinescu, C.A.; Tanasescu, S. Thermal and Structural Characterization of Synthetic and Natural Nanocrystalline Hydroxyapatite. Mater. Sci. Eng. C Mater. Biol. Appl. 2014, 43, 153–163. [Google Scholar] [CrossRef]
- Antonakos, A.; Liarokapis, E.; Leventouri, T. Micro-Raman and FTIR Studies of Synthetic and Natural Apatites. Biomaterials 2007, 28, 3043–3054. [Google Scholar] [CrossRef]
- Berzina-Cimdina, L.; Borodajenko, N. Research of Calcium Phosphates Using Fourier Transform Infrared Spectroscopy. Infrared Spectrosc.-Mater. Sci. Eng. Technol. 2012, 12, 251–263. [Google Scholar] [CrossRef] [Green Version]
- Uskoković, V.; Uskoković, D.P. Nanosized Hydroxyapatite and Other Calcium Phosphates: Chemistry of Formation and Application as Drug and Gene Delivery Agents. J. Biomed. Mater. Res. B Appl. Biomater. 2011, 96, 152–191. [Google Scholar] [CrossRef] [Green Version]
- Aguado, B.A.; Mulyasasmita, W.; Su, J.; Lampe, K.J.; Heilshorn, S.C. Improving Viability of Stem Cells during Syringe Needle Flow through the Design of Hydrogel Cell Carriers. Tissue Eng. Part A 2012, 18, 806–815. [Google Scholar] [CrossRef] [Green Version]
- Rheological Properties of Gelatine Hydrogels Affected by Flow- and Horizontally-Induced Cooling Rates during 3D Cryo-Printing. Colloids Surf. A Physicochem. Eng. Asp. 2021, 616, 126356. [CrossRef]
- Liu, Q.; Li, Q.; Xu, S.; Zheng, Q.; Cao, X. Preparation and Properties of 3D Printed Alginate–Chitosan Polyion Complex Hydrogels for Tissue Engineering. Polymers 2018, 10, 664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guerrero-Beltrán, C.E.; Bernal-Ramírez, J.; Lozano, O.; Oropeza-Almazán, Y.; Castillo, E.C.; Garza, J.R.; García, N.; Vela, J.; García-García, A.; Ortega, E.; et al. Silica Nanoparticles Induce Cardiotoxicity Interfering with Energetic Status and Ca Handling in Adult Rat Cardiomyocytes. Am. J. Physiol. Heart Circ. Physiol. 2017, 312, H645–H661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ornelas-Soto, N.; Rubio-Govea, R.; Guerrero-Beltrán, C.E.; Vázquez-Garza, E.; Bernal-Ramírez, J.; García-García, A.; Oro-peza-Almazán, Y.; García-Rivas, G.; Contreras-Torres, F.F. Enhancing Internalization of Silica Particles in Myocardial Cells through Surface Modification. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 79, 831–840. [Google Scholar] [CrossRef]






| %Alginate | Hydrogels % Gelatin | 1% Bioceramic Filler | Label |
|---|---|---|---|
| 3.5 | 0.88 | - | AG1 |
| 3.5 | 0.88 | Al2O3 * | AG2 |
| 3.5 | 0.88 | Na2Ti6O13 | AG3 |
| 3.5 | 0.88 | TiO2 * | AG4 |
| 3.5 | 0.88 | ZrO2 * | AG5 |
| 3.5 | 0.88 | WO3 | AG6 |
| Sample | AG1 | AG2 | AG3 | AG4 | AG5 | AG6 |
|---|---|---|---|---|---|---|
| Bioceramic Filler | Al2O3 | Na2Ti6O13 | TiO2 | ZrO2 | WO3 | |
| Particle Size (nm) | - | 516.2 | 200.5 | 652.2 | 459.2 | 210.2 |
| Oxygen (%) | 57.13 | 77.64 | 65.65 | 71.28 | 77.83 | |
| Calcium (%) | 14.4 | 9.38 | - | 11.66 | 10.56 | |
| Sodium (%) | 12.63 | 6.04 | 8.88 | 6.89 | 6.14 | |
| Chlorine (%) | 14.83 | 4.18 | - | 4.61 | 2.88 | |
| Phosphorus (%) | 2.80 | 0.99 | - | 3.38 | 2.13 | |
| Potassium (%) | 0.46 | - | - | 1.4 | - | |
| Titanium (%) | - | 0.43 | 23.69 | - | - | |
| Aluminum (%) | - | 0.57 | 1.78 | - | - | |
| Silicon (%) | - | 0.34 | - | - | - | |
| Ca/P (%) | - | 5.14 | 9.47 | - | 3.45 | 4.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avila-Ramirez, A.; Catzim-Ríos, K.; Guerrero-Beltrán, C.E.; Ramírez-Cedillo, E.; Ortega-Lara, W. Reinforcement of Alginate-Gelatin Hydrogels with Bioceramics for Biomedical Applications: A Comparative Study. Gels 2021, 7, 184. https://doi.org/10.3390/gels7040184
Avila-Ramirez A, Catzim-Ríos K, Guerrero-Beltrán CE, Ramírez-Cedillo E, Ortega-Lara W. Reinforcement of Alginate-Gelatin Hydrogels with Bioceramics for Biomedical Applications: A Comparative Study. Gels. 2021; 7(4):184. https://doi.org/10.3390/gels7040184
Chicago/Turabian StyleAvila-Ramirez, Alan, Kevin Catzim-Ríos, Carlos Enrique Guerrero-Beltrán, Erick Ramírez-Cedillo, and Wendy Ortega-Lara. 2021. "Reinforcement of Alginate-Gelatin Hydrogels with Bioceramics for Biomedical Applications: A Comparative Study" Gels 7, no. 4: 184. https://doi.org/10.3390/gels7040184
APA StyleAvila-Ramirez, A., Catzim-Ríos, K., Guerrero-Beltrán, C. E., Ramírez-Cedillo, E., & Ortega-Lara, W. (2021). Reinforcement of Alginate-Gelatin Hydrogels with Bioceramics for Biomedical Applications: A Comparative Study. Gels, 7(4), 184. https://doi.org/10.3390/gels7040184