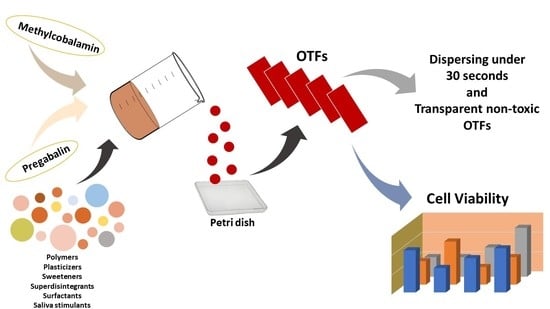
Preparation, Characterization, and Evaluation of Cytotoxicity of Fast Dissolving Hydrogel Based Oral Thin Films Containing Pregabalin and Methylcobalamin
Abstract
:1. Introduction
2. Results and Discussion
2.1. Quantification Method Development and Validation of the Pregabalin and Methylcobalamin
2.1.1. Linearity
2.1.2. Accuracy and Precision
2.1.3. LOD and LOQ
2.1.4. Selectivity (Specificity)
2.1.5. Stability of Active Substances
2.2. Preparation and Organoleptic Evaluation of OTFs
2.3. Moisture Absorption Capacity
2.4. Tensile Strength (Elongation)
2.5. Weight Variability and Thickness
2.6. Folding Endurance (Flexibility)
2.7. Determination of pH Values
2.8. Determination of Swelling Degrees
2.9. Disintegration Test
2.10. Transparency
2.11. Content Uniformity
2.12. Dissolution Rate Test
2.13. Determination of Release Kinetics
2.14. Fourier Transform Infrared (FT-IR) Analysis
2.15. X-ray Diffraction (XRD) Analysis
2.16. Differential Scanning Calorimetry (DSC) Analysis
2.17. Surface and Structural Morphology
2.18. Stability of OTFs
2.19. MTT Cell-Viability Assay
3. Conclusions
4. Materials and Methods
4.1. Material
4.2. Development and Validation of Pregabalin and Methylcobalamin Simultaneous Assay Method
4.3. Preparation of Standard Solutions
4.4. Method Validation
4.4.1. Linearity
4.4.2. Accuracy and Precision
4.4.3. LOD
4.4.4. LOQ
4.4.5. Selectivity (Specificity)
4.4.6. Stability of Active Substances
4.5. Preparation of OTFs
4.6. Organoleptic Evaluation of OTFs
4.7. Moisture Absorption Capacity
4.8. Tensile Strength (Elongation)
4.9. Weight Variability
4.10. Thickness
4.11. Folding Endurance (Flexibility)
4.12. Determination of pH Values
4.13. Determination of Swelling Degrees
4.14. Disintegration Test
4.15. Transparency
4.16. Content Uniformity
4.17. Dissolution Rate Test
4.18. Determination of Release Kinetics
4.19. FT-IR Analysis
4.20. XRD Analysis
4.21. DSC Analysis
4.22. Surface and Structural Morphology
4.23. Stability of OTFs
4.24. Cell Culture and MTT Cell-Viability Assay
4.25. Statistical Evaluations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sharma, D.; Kaur, D.; Verma, S.; Singh, D.; Singh, M.; Singh, G.; Garg, R. Fast dissolving oral films technology: A recent trend for an innovative oral drug delivery system. Int. J. Drug Deliv. 2015, 7, 60–75. [Google Scholar]
- Malke, S.; Shidhaye, S.; Desai, J.; Kadam, V. Oral films-patient compliant dosage form for pediatrics. Int. J. Pediatr. Neonatol. 2010, 11, 1–7. [Google Scholar]
- Ghodake, P.P.; Karande, K.M.; Osmani, R.A.; Bhosale, R.R.; Harkare, B.R.; Kale, B.B. Mouth dissolving films: Innovative vehicle for oral drug delivery. Int. J. Pharm. Res. Rev. 2013, 2, 41–47. [Google Scholar]
- Mahboob, M.B.H.; Riaz, T.; Jamshaid, M.; Bashir, I.; Zulfiqar, S. Oral films: A comprehensive review. Int. Curr. Pharm. J. 2016, 5, 111–117. [Google Scholar] [CrossRef]
- Joshua, J.M.; Hari, R.; Jyothish, F.K.; Surendran, S.A. Fast dissolving oral thin films: An effective dosage form for quick releases. Drugs 2016, 38, 282–289. [Google Scholar]
- Godbole, A.; Joshi, R.; Sontakke, M. Oral thin film technology-current challenges and future scope. IJAREAS 2018, 7, 1–14. [Google Scholar]
- Alam, M.; Tasneem, F.; Pathan, M.S.I. Formulation and evaluation of swellable oral thin film of metoclopramide hydrochloride. Bangladesh Pharm. J. 2014, 17, 102–112. [Google Scholar] [CrossRef]
- Kathpalia, H.; Gupte, A. An introduction to fast dissolving oral thin film drug delivery systems: A review. Curr. Drug Deliv. 2013, 10, 667–684. [Google Scholar] [CrossRef]
- Karki, S.H.; Kim, S.-J.; Na, S.D.; Jo, K.; Lee, J. Thin films as an emerging platform for drug delivery. Asian J. Pharm. 2016, 11, 559–574. [Google Scholar] [CrossRef]
- Metin, S.K.; Meydan, B.; Evman, S.; Dogruyol, T.; Baysungur, V. The effect of pregabalin and methylcobalamin combination on the chronic postthoracotomy pain syndrome. Ann. Thorac. Surg. 2017, 103, 1109–1113. [Google Scholar] [CrossRef]
- Gujral, R.S.; Haque, S.M.; Shanker, P. A sensitive spectrophotometric method for the determination of pregabalin in bulk, pharmaceutical formulations and in human urine samples. Int. J. Biomed. Sci. 2009, 5, 421–427. [Google Scholar]
- Atta, A.; Salama, I.; Gomaa, M.; Mostafa, S. A new HPLC method for simultaneous determination of atenolol and pregabalin in dosage forms and in human urine. Int. J. Pharm. Chem. Biol. Sci. 2016, 6, 48–61. [Google Scholar]
- Vasantakumar, P.K.; Harsha, J.; Gowda, D.V.; Praveen, S.M.S. Development and evaluation of pregabalin capsules using QbD approach. J. Chem. Pharm. Res. 2017, 9, 37–44. [Google Scholar]
- Dongre, Y.U.; Swami, O.C. Sustained-release pregabalin with methylcobalamin in neuropathic pain: An Indian real-life experience. Int. J. Gen. Med. 2013, 6, 413–417. [Google Scholar]
- Saravanan, J.; Shajan, A.; Joshi, N.; Varatharajan, R.; Valliappan, K. A simple and validated RP-HPLC method for the estimation of methylcobalamin in bulk and capsule dosage form. J. Chem. Pharm. Sci. 2010, 1, 13–16. [Google Scholar]
- Narmada, P.; Vijaya Lakshmi, G.; Nalini, G.; Gowtham, Y.; Suhasini, B.; Jogi, K. RP-HPLC method development and validation for the determination of methylcobalamin and pregabalin in combined capsule dosage form. Int. J. Res. Pharm. Sci. 2013, 4, 25–29. [Google Scholar]
- Udayalakshmi, P.; Muthukumaran, M.; Krishnamoorthy, B. Simultaneous estimation of pregabalin and methylcobalamin by RP-HPLC in bulk drug and combined tablet dosage form. Int. J. Pharm. H. Care. Res. 2014, 2, 74–80. [Google Scholar]
- Babu, B.H.; Rao, M.N.; Rambabu, A.; Srinivasan, P. Development and validation of HPLC method for the estimation of methylcobalamine in bulk drugs and pharmaceutical formulations. J. Pharm. Res. 2011, 4, 1685–1687. [Google Scholar]
- Julian, T.; Syeed, R.; Glascow, N.; Angelopoulou, E.; Zis, P. B12 as a treatment for peripheral neuropathic pain: A systematic re-view. Nutrients 2020, 12, 2221. [Google Scholar] [CrossRef]
- Patil, P.; Shrivastava, S.K. Fast dissolving oral films: An innovative drug delivery system. Int. J. Sci. Res. 2014, 3, 2088–2093. [Google Scholar]
- Irfan, M.; Rabel, S.; Bukhtar, Q.; Qadir, M.I.; Jabeen, F.; Khan, A. Orally disintegrating films: A modern expansion in drug delivery system. Saudi Pharm. J. 2016, 24, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, E.M.; Breitenbach, A.; Breitkreutz, J. Advances in orodispersible films for drug delivery. Expert Opin. Drug Deliv. 2011, 8, 299–316. [Google Scholar]
- Panchal, M.S.; Patel, H.; Bagada, A.; Vadalia, K.R. Formulation and evaluation of mouth dissolving film of ropinirole hydrochloride by using pullulan polymers. Int. J. Pharm. Res. Allied Sci. 2012, 1, 60–72. [Google Scholar]
- Sharma, R.; Kamboj, S.; Singh, G.; Rana, V. Development of aprepitant loaded orally disintegrating films for enhanced pharmacokinetic performance. Eur. J. Pharm. Sci. 2016, 84, 55–69. [Google Scholar] [CrossRef]
- Pezik, E.; Gulsun, T.; Sahin, S.; Vural, I. Development and characterization of pullulan-based orally disintegrating films containing amlodipine besylate. Eur. J. Pharm. Sci. 2021, 156, 105597. [Google Scholar] [CrossRef]
- Wasilewska, K.; Winnicka, K. How to assess orodispersible film quality? A review of applied methods and their modifications. Acta Pharm. 2019, 69, 155–176. [Google Scholar] [CrossRef] [Green Version]
- Kumar, M.K.; Nagaraju, K.; Bhanja, S.; Sudhakar, M. Formulation and evaluation of sublingual tablets of terazosin hydrochloride. Int. J. Pharm. Sci. Res. 2014, 5, 417–427. [Google Scholar]
- Lu, T.; Ten Hagen, T.L.M. A novel kinetic model to describe the ultra-fast triggered release of thermosensitive liposomal drug delivery systems. J. Control. Release 2020, 324, 669–678. [Google Scholar] [CrossRef]
- Mircioiu, C.; Voicu, V.; Anuta, V.; Tudose, A.; Celia, C.; Paolino, D.; Fresta, M.; Sandulovici, R.; Mircioiu, I. Mathematical modeling of release kinetics from supramolecular drug delivery systems. Pharmaceutics 2019, 11, 140. [Google Scholar] [CrossRef]
- Wojcik-Pastuszka, D.; Krzak, J.; Macikowski, B.; Berkowski, R.; Osiński, B.; Musiał, W. Evaluation of the release kinetics of a pharmacologically active substance from model intra-articular implants replacing the cruciate ligaments of the knee. Materials 2019, 12, 1202. [Google Scholar] [CrossRef]
- Rençber, S.; Karavana, S.Y.; Yilmaz, F.F.; Eraç, B.; Nenni, M.; Gurer-Orhan, H.; Limoncu, M.H.; Güneri, P.; Ertan, G. Formulation and evaluation of fluconazole loaded oral strips for local treatment of oral candidiasis. J. Drug. Deliv. Sci. Technol. 2019, 49, 615–621. [Google Scholar] [CrossRef]
- Zhang, J.L.A.; Thakkar, R.; Zhang, Y.; Maniruzzaman, M. Development and evaluation of amorphous oral thin films using solvent-free processes: Comparison between 3D printing and hot-melt extrusion technologies. Pharmaceutics 2021, 13, 1613. [Google Scholar] [CrossRef]
- Lamichhane, S.; Park, J.-B.; Sohn, D.H.; Lee, S. Customized novel design of 3D printed pregabalin tablets for intra-gastric floating and controlled release using fused deposition modeling. Pharmaceutics 2019, 11, 564. [Google Scholar] [CrossRef]
- Mohamad, S.A.; Sarhan, H.A.; Abdelkader, H.; Mansour, H.F. Vitamin B12–loaded buccoadhesive films as a noninvasive supplement in vitamin B12 deficiency: In vitro evaluation and in vivo comparative study with intramuscular injection. J. Pharm. Sci. 2017, 106, 1849–1858. [Google Scholar] [CrossRef]
- Asghar, A.; Aamir, M.N.; Sheikh, F.A.; Ahmad, N.; Alotaibi, N.F.; Bukhari, S.N.A. Preparation, characterization of pregabalin and Withania coagulans extract-loaded topical gel and their comparative effect on burn injury. Gels 2022, 8, 402. [Google Scholar] [CrossRef]
- Arafa, M.G.; Ayoub, B.M. DOE optimization of nano-based carrier of pregabalin as hydrogel: New therapeutic & chemometric approaches for controlled drug delivery systems. Sci. Rep. 2017, 7, 41503. [Google Scholar]
- Mazzocato, M.C.; Thomazini, M.; Favaro-Trindade, C.S. Improving stability of vitamin B12 (Cyanocobalamin) using microencapsulation by spray chilling technique. Food Res. Int. 2019, 126, 108663. [Google Scholar] [CrossRef]
- Asghar, A.; Aamir, M.N.; Sheikh, F.A.; Ahmad, N.; Elsherif, M.A.; Bukhari, S.N.A. Co-combination of pregabalin and Withania coagulans-extract-loaded topical gel alleviates allodynia and hyperalgesia in the chronic sciatic nerve constriction injury for neuropathic pain in animal model. Molecules 2022, 27, 4433. [Google Scholar] [CrossRef]
- Riss, T.L.; Moravec, R.A.; Niles, A.L.; Duellman, S.; Benink, H.A.; Worzella, T.J.; Minor, L. Cell viability assays. In Assay Guidance Manual; Markossian, S., Grossman, A., Brimacombe, K., Eds.; Eli Lilly & Company and the National Center for Advancing Translational Sciences: Bethesda, MD, USA, 2004; pp. 1–35. [Google Scholar]
- Tolosa, L.; Donato, M.T.; Gómez-Lechón, M.J. General cytotoxicity assessment by means of the MTT assay. Methods Mol. Biol. 2015, 1250, 333–348. [Google Scholar]
- Kumar, P.; Nagarajan, A.; Uchil, P.D. Analysis of cell viability by the MTT assay. Cold Spring Harb. Protoc. 2018, 6, 469–471. [Google Scholar] [CrossRef]
- Baldewig, M.; Goldbaum, O.; Richter-Landsberg, C.; Weyland, A.; Bantel, C. Short-term incubation of gabapentin or pregabalin does not affect chemically induced injury in neuronal cell models in vitro. J. Pain Res. 2018, 11, 1181. [Google Scholar] [CrossRef] [PubMed]
- Bülbül, E.Ö.; Mesut, B.; Cevher, E.; Öztaş, E.; Özsoy, Y. Product transfer from lab-scale to pilot-scale of quetiapine fumarate orodispersible films using quality by design approach. J. Drug Deliv. Sci. Technol. 2019, 54, 101358. [Google Scholar] [CrossRef]
- Sałat, K.; Librowski, T.; Nawiesniak, B.; Gluch-Lutwin, M. Evaluation of analgesic, antioxidant, cytotoxic and metabolic effects of pregabalin for the use in neuropathic pain. Neurol. Res. 2013, 35, 948–958. [Google Scholar] [CrossRef] [PubMed]
- Prabhoo, R.; Panghate, A.; Dewda, R.P.; More, B.; Prabhoo, T.; Rana, R. Efficacy and tolerability of a fixed dose combination of methylcobalamin and pregabalin in the management of painful neuropathy. N. Am. J. Med. Sci. 2012, 4, 605–607. [Google Scholar]
- Ibrahim, M.M.; Hafez, S.A.; Mahdy, M.M. Organogels, hydrogels and bigels as transdermal delivery systems for diltiazem hydrochloride. Asian J. Pharm. 2013, 8, 48–57. [Google Scholar] [CrossRef]
- Sevinç-Özakar, R.; Seyret, E.; Özakar, E.; Adıgüzel, M.C. Nanoemulsion-based hydrogels and organogels containing propolis and dexpanthenol: Preparation, characterization, and comparative evaluation of stability, antimicrobial, and cytotoxic properties. Gels 2022, 8, 578. [Google Scholar] [CrossRef]
- de Lima, G.G.; de Souza, R.O.; Bozzi, A.D.; Poplawska, M.A.; Devine, D.M.; Nugent, M.J. Extraction method plays critical role in antibacterial activity of propolis-loaded hydrogels. J. Pharm. Sci. 2016, 105, 1248–1257. [Google Scholar] [CrossRef]
- Shapiro, Y.E. Structure and dynamics of hydrogels and organogels: An NMR spectroscopy approach. Prog. Polym. Sci. 2011, 36, 1184–1253. [Google Scholar] [CrossRef]
- Khodaverdi, E.; Tekie, F.S.M.; Hadizadeh, F.; Esmaeel, H.; Mohajeri, S.A.; Tabassi, S.A.S.; Zohuri, G. Hydrogels composed of cyclodextrin inclusion complexes with PLGA-PEG-PLGA triblock copolymers as drug delivery systems. AAPS Pharmscitech 2014, 15, 177–188. [Google Scholar] [CrossRef]
- Qi, X.; Wei, W.; Junjian, L.; Gancheng, Z.; Xihao, P.; Ting, S.; Jianfa, Z.; Wei, D. Salecan-based pH-sensitive hydrogels for insulin delivery. Mol. Pharm. 2017, 14, 431–440. [Google Scholar]
- Yang, Y.; Liu, Y.; Chen, S.; Cheong, K.L.; Teng, B. Carboxymethyl β-cyclodextrin grafted carboxymethyl chitosan hydrogel-based microparticles for oral insulin delivery. Carbohydr. Polym. 2020, 246, 116617. [Google Scholar] [CrossRef]
- Hu, Y.; Shujun, G.; Lu, H.; Jackie, Y.Y. Acid-resistant and physiological pH-responsive DNA hydrogel composed of a-motif and i-motif toward oral insulin delivery. J. Am. Chem. Soc. 2022, 144, 5461–5470. [Google Scholar]
- Özakar, R.S.; Özakar, E. Current overview of oral thin films. Turk. J. Pharm. Sci. 2021, 18, 111–121. [Google Scholar] [CrossRef]
- Sreekanth, D.; Ramya, P.; Vishwanadham, Y.; Vanitha, R. Development and method validation of RP-HPLC for simultaneous determination of pregabalin and methylcobalamin in pure and pharmaceutical dosage form. Asian J. Chem. 2017, 10, 557–565. [Google Scholar] [CrossRef]
- Mohan, A.; Raj Kumar, B.; Bhavya, T.; Ashok Kumar, A. RP-HPLC method development and validation for the simultaneous quantitative estimation of pregabalin, mecobalamin and alpha lipoic acid in capsules. Int. J. Pharm. Pharmsci. 2014, 6, 270. [Google Scholar]
- Pagilla, P.; Vishnu, P.; Konde, A. Formulation and evaluation of lovastatin oral disintegration thin films. GSC Biol. Pharm. Sci. 2018, 3, 35–42. [Google Scholar] [CrossRef]
- Liang, Y.; Li, Z.; Huang, Y.; Yu, R.; Guo, B. Dual-dynamic-bond cross-linked antibacterial adhesive hydrogel sealants with on-demand removability for post-wound-closure and infected wound healing. ACS Nano 2021, 15, 7078–7093. [Google Scholar] [CrossRef]
- Dragan, E.S.; Ghiorghita, C.A.; Dinu, M.V.; Duceac, I.A.; Coseri, S. Fabrication of self-antibacterial chitosan/oxidized starch polyelectrolyte complex sponges for controlled delivery of curcumin. Food Hydrocoll. 2023, 135, 108147. [Google Scholar] [CrossRef]
- Senthilkumar, K.; Vijaya, C. Formulation development of mouth dissolving film of etoricoxib for pain management. Adv. Pharm. 2015, 2015, 1–11. [Google Scholar] [CrossRef]
- Chinnala, K.; Vodithala, S. Formulation and evaluation of fast disintegrating oral thin films of cinitapride hydrogen tartarate. Int. J. Curr. Adv. 2017, 6, 4737–4740. [Google Scholar]
- Venkateswarlu, K. Preparation and evaluation of fast dissolving buccal thin films of bufotenin. J. In Silico In Vitr. Pharm. 2016, 2, 12. [Google Scholar]
- Rani, T.N. Formulation development and optimization of oral thin films of zolpidem tartarate. MSHP 2017, 1, 26–41. [Google Scholar] [CrossRef]
- Jelvehgari, M.; Montazam, S.H.; Soltani, S.; Mohammadi, R.; Azar, K.; Montazam, S.A. Fast dissolving oral thin film drug delivery systems consist of ergotamine tartrate and caffeine anhydrous. Phar. Sci. 2015, 21, 102–110. [Google Scholar] [CrossRef]
- Silva, N.H.; Mota, J.P.; Santos de Almeida, T.; Carvalho, J.P.; Silvestre, A.J.; Vilela, C.; Rosado, C.; Freire, C.S. Topical drug delivery systems based on bacterial nanocellulose: Accelerated stability testing. Int. J. Mol. Sci. 2020, 21, 1262. [Google Scholar] [CrossRef]
- Ibrahim, A.H.; Ibrahim, H.M.; Ismael, H.R.; Samy, A.M. Optimization and evaluation of lyophilized fenofibrate nanoparticles with enhanced oral bioavailability and efficacy. Pharm. Dev. Technol. 2018, 23, 358–369. [Google Scholar] [CrossRef]
- Tawfeek, H.M.; Saleem, I.Y.; Roberts, M. Dissolution enhancement and formulation of rapid-release lornoxicam mini-tablets. J. Pharm. Sci. 2014, 103, 2470–2483. [Google Scholar] [CrossRef]









| Mobile Phase | 0.05 M pH 3.5 Potassium Dihydrogen Orthophosphate Buffer (KH2PO4):ACN (92:8) |
| Column | ACE C18, 250 × 4.6 mm, 5 µm |
| Wavelength (λ) | 205 nm |
| Column temperature | 30 °C |
| Flow and Duration | 1 mL/min |
| Injection Volume | 20 μL |
| For MC | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Theoretical (µg/mL) | Detected (µg/mL) | RSD % | RE % | Theoretical (µg/mL) | Detected (µg/mL) | RSD % | RE % | ||
| 1.25 | 1.2 ± 0.51 | 1.31 ± 0.23 | −1.24 ± 0.48 | 1.25 | 1.2 ± 0.33 | 1.77 ± 0.33 | −0.81 ± 0.03 | ||
| Intraday | 12.5 | 12.6 ± 0.93 | 1.41 ± 0.54 | 1.06 ± 0.26 | Interday | 12.5 | 12.6 ± 0.76 | 1.17 ± 0.40 | 0.87 ± 0.18 |
| 75 | 75.8 ± 1.15 | 0.67 ± 0.33 | 1.09 ± 0.39 | 75 | 75.1 ± 1.38 | 1.51 ± 0.27 | 0.13 ± 0.08 | ||
| For PG | |||||||||
| 37.5 | 37.8 ± 0.90 | 2.05 ± 0.19 | 0.78 ± 0.63 | 37.5 | 38.5 ± 1.41 | 2.01 ± 0.16 | 2.72 ± 0.41 | ||
| Intraday | 150 | 148.4 ± 2.15 | 2.41 ± 0.26 | −1.04 ± 0.51 | Interday | 150 | 148.4 ± 2.08 | 1.70 ± 0.34 | −1.04 ± 0.30 |
| 450 | 461.0 ± 4.28 | 0.37 ± 0.43 | 2.45 ± 0.18 | 450 | 459.4 ± 3.13 | 0.53 ± 0.26 | 2.08 ± 0.11 | ||
| Recovery % | |
|---|---|
| MC | PG |
| 100.00 ± 2.03 | 101.39 ± 2.98 |
| 98.29 ± 2.68 | 103.83 ± 2.37 |
| 98.15 ± 0.84 | 98.91 ± 1.06 |
| Taste | Smell | Texture | Clarity | Thickness (µm) | Flexibility | Homogeneity | ||
|---|---|---|---|---|---|---|---|---|
| Formulation Codes | F1 | ✓ | ✓ | Rough | Clear | 30 ± 0.01 | Fragile | — |
| F2 | — | ✓ | Rough | Opaque | 30 ± 0.00 | Fragile | — | |
| F3 | ✓ | — | Rough | Semi Clear | 30 ± 0.01 | Fragile | — | |
| F4 | — | ✓ | Smooth | Opaque | 30 ± 0.01 | Fragile | ✓ | |
| F5 | ✓ | ✓ | Smooth | Opaque | 30 ± 0.01 | ✓ | ✓ | |
| F6 | — | ✓ | Smooth | Semi Clear | 30 ± 0.00 | ✓ | ✓ | |
| F7 | — | ✓ | Rough | Opaque | 30 ± 0.00 | Fragile | — | |
| F8 | ✓ | ✓ | Smooth | Opaque | 30 ± 0.00 | ✓ | ✓ | |
| F9 | — | ✓ | Smooth | Opaque | 30 ± 0.01 | Fragile | ✓ | |
| F10 | — | ✓ | Smooth | Opaque | 30 ± 0.01 | Fragile | ✓ | |
| F11 | — | ✓ | Smooth | Semi Clear | 30 ± 0.00 | ✓ | — | |
| F12 | — | — | Smooth | Clear | 30 ± 0.01 | ✓ | ✓ | |
| F13 | ✓ | ✓ | Smooth | Opaque | 30 ± 0.00 | ✓ | ✓ | |
| F14 | — | ✓ | Smooth | Semi Clear | 30 ± 0.00 | ✓ | ✓ | |
| F15 | — | — | Smooth | Opaque | 30 ± 0.01 | ✓ | ✓ | |
| F16 | ✓ | — | Smooth | Opaque | 30 ± 0.01 | ✓ | ✓ | |
| F17 | ✓ | — | Smooth | Semi Clear | 30 ± 0.00 | ✓ | — | |
| F18 | — | ✓ | Rough | Opaque | 30 ± 0.01 | Fragile | — | |
| F19 | — | — | Rough | Opaque | 30 ± 0.00 | Fragile | — | |
| F20 | — | ✓ | Rough | Opaque | 30 ± 0.00 | Fragile | ✓ | |
| F21 | — | — | Rough | Semi Clear | 30 ± 0.01 | Fragile | — | |
| F22 | — | — | Rough | Semi Clear | 30 ± 0.01 | Fragile | ✓ | |
| F23 | — | ✓ | Rough | Opaque | 30 ± 0.01 | Fragile | — | |
| F24 | — | ✓ | Rough | Semi Clear | 30 ± 0.01 | Fragile | — |
| Moisture Uptake Capacity | Tensile Strength | Weight Variability | Folding Endurance | pH | Swelling Degree | Disintegration Time (s) | Transparency | ||
|---|---|---|---|---|---|---|---|---|---|
| Formulation Codes | F1 | 1.0 ± 0.89 | 0.0 ± 0.0 | 0.02 ± 0.0 | 5 ± 1.5 | 6.02 ± 0.5 | 576 ± 45 | 477 ± 13 | 206 ± 8.6 |
| F2 | 0.88 ± 0.39 | 0.0 ± 0.0 | 0.02 ± 0.0 | 10 ± 2.0 | 6.05 ± 0.2 | 810 ± 35 | 121 ± 8.0 | 70 ± 3.1 | |
| F3 | 2.4 ± 0.35 | 0.0 ± 0.0 | 0.03 ± 0.0 | 22 ± 4.0 | 6.01 ± 0.7 | 643 ± 28 | 92 ± 5.0 | 129 ± 5.6 | |
| F4 | 0.8 ± 0.11 | 6.0 ± 0.3 | 0.03 ± 0.0 | 150 ± 8.0 | 5.98 ± 0.3 | 269 ± 12 | 74 ± 6.0 | 97 ± 4.3 | |
| F5 | 1.2 ± 0.25 | 2.7 ± 0.2 | 0.03 ± 0.0 | 200 ± 8.5 | 5.50 ± 0.2 | 203 ± 11 | 28 ± 2.0 | 63 ± 2.1 | |
| F6 | 1.5 ± 0.24 | 1.6 ± 0.01 | 0.03 ± 0.0 | 200 ± 12 | 5.55 ± 0.4 | 316 ± 10 | 62 ± 6.0 | 131 ± 5.1 | |
| F7 | 0.7 ± 0.05 | 0.0 ± 0.0 | 0.03 ± 0.0 | 10 ± 1.5 | 5.45 ± 0.5 | 270 ± 8.0 | 27 ± 4.0 | 85 ± 3.2 | |
| F8 | 0.7 ± 0.13 | 10.6 ± 1.5 | 0.03 ± 0.0 | 215 ± 11 | 6.05 ± 0.1 | 111 ± 6.0 | 17 ± 2.0 | 50 ± 3.0 | |
| F9 | 0.8 ± 0.39 | 0.0 ± 0.0 | 0.03 ± 0.0 | 50 ± 6.5 | 5.78 ± 0.5 | 259 ± 10 | 51 ± 3.0 | 63 ± 4.8 | |
| F10 | 0.7 ± 0.13 | 0.0 ± 0.0 | 0.03 ± 0.0 | 42 ± 3.5 | 5.11 ± 0.2 | 408 ± 12 | 67 ± 5.0 | 66 ± 3.4 | |
| F11 | 1.4 ± 0.04 | 40.6 ± 2.4 | 0.02 ± 0.0 | 300 ± 17 | 5.45 ± 0.5 | 176 ± 7.0 | 82 ± 6.0 | 158 ± 6.7 | |
| F12 | 1.6 ± 0.40 | 25.4 ± 1.2 | 0.03 ± 0.0 | 300 ± 14 | 5.25 ± 0.4 | 292 ± 17 | 66 ± 4.0 | 179 ± 8.1 | |
| F13 | 0.47 ± 0.09 | 2.89 ± 0.48 | 0.03 ± 0.0 | 110 ± 4.5 | 6.55 ± 0.1 | 169 ± 11 | 16 ± 2.0 | 59 ± 2.9 | |
| F14 | 1.1 ± 0.15 | 21.3 ± 4.3 | 0.02 ± 0.0 | 115 ± 8.5 | 6.30 ± 0.1 | 358 ± 10 | 246 ± 15 | 95 ± 2.7 | |
| F15 | 1.7 ± 0.17 | 2.7 ± 1.0 | 0.03 ± 0.0 | 300 ± 13 | 5.40 ± 0.2 | 180 ± 16 | 91 ± 3.0 | 72 ± 4.6 | |
| F16 | 1.0 ± 0.15 | 4.0 ± 0.02 | 0.04 ± 0.0 | 300 ± 9.0 | 5.50 ± 0.2 | 215 ± 15 | 48 ± 3.0 | 83 ± 3.5 | |
| F17 | 1.5 ± 0.36 | 14.1 ± 1.1 | 0.03 ± 0.0 | 240 ± 11 | 5.60 ± 0.1 | 347 ± 15 | 129 ± 9.0 | 169 ± 8.0 | |
| F18 | 1.5 ± 0.25 | 0.0 ± 0.0 | 0.03 ± 0.0 | 65 ± 9.0 | 6.02 ± 0.3 | 238 ± 8.0 | 27 ± 3.0 | 60 ± 2.7 | |
| F19 | 1.6 ± 0.10 | 9.0 ± 0.44 | 0.03 ± 0.0 | 150 ± 7.5 | 6.15 ± 0.1 | 434 ± 11 | 18 ± 2.0 | 49 ± 2.1 | |
| F20 | 0.4 ± 0.04 | 3.8 ± 1.42 | 0.03 ± 0.0 | 100 ± 11 | 6.31 ± 0.4 | 376 ± 7.0 | 16 ± 2.0 | 57 ± 4.0 | |
| F21 | 0.3 ± 0.09 | 1.0 ± 0.8 | 0.02 ± 0.0 | 75 ± 7.5 | 5.31 ± 0.2 | 189 ± 13 | 122 ± 2.7 | 131 ± 6.3 | |
| F22 | 1.1 ± 0.24 | 0.0 ± 0.0 | 0.03 ± 0.0 | 28 ± 8.5 | 6.32 ± 0.3 | 211 ± 36 | 131 ± 4.1 | 146 ± 0.7 | |
| F23 | 0.8 ± 0.37 | 6.5 ± 0.3 | 0.03 ± 0.0 | 85 ± 12 | 5.40 ± 1.5 | 382 ± 14 | 68 ± 3.2 | 82 ± 3.3 | |
| F24 | 1.3 ± 0.56 | 2.0 ± 0.0 | 0.03 ± 0.0 | 53 ± 3.0 | 5.38 ± 0.4 | 319 ± 42 | 97 ± 4.7 | 101 ± 5.0 |
| For PG | Formulation Codes | Amount (mg) | For MC | Formulation Codes | Amount (mg) |
| F5 | 24.897 ± 0.518 | F5 | 0.514 ± 0.013 | ||
| F8 | 25.347 ± 0.196 | F8 | 0.518 ± 0.015 | ||
| F13 | 25.127 ± 0.583 | F13 | 0.496 ± 0.014 |
| For PG | Formulation Codes | Time (min) | Cumulative Released % | For MC | Formulation Codes | Time (min) | Cumulative Released % |
| F5 | 0.5 | 9.96 ± 0.81 | F5 | 0.5 | 16.81 ± 0.45 | ||
| 1 | 33.83 ± 1.51 | 1 | 52.69 ± 0.85 | ||||
| 2.5 | 75.70 ± 0.66 | 2.5 | 74.36 ± 1.15 | ||||
| 5 | 101.16 ± 1.9 | 5 | 91.83 ± 1.49 | ||||
| 10 | 100.11 ± 0.4 | 10 | 100.09 ± 0.9 | ||||
| F8 | 0.5 | 12.78 ± 0.23 | F8 | 0.5 | 34.93 ± 0.33 | ||
| 1 | 34.40 ± 0.39 | 1 | 65.68 ± 0.76 | ||||
| 2.5 | 72.89 ± 1.13 | 2.5 | 92.81 ± 0.88 | ||||
| 5 | 100.60 ± 0.9 | 5 | 104.95 ± 1.2 | ||||
| 10 | 100.34 ± 0.7 | 10 | 104.40 ± 0.2 | ||||
| F13 | 0.5 | 4.73 ± 0.12 | F13 | 0.5 | 15.63 ± 0.69 | ||
| 1 | 31.20 ± 0.55 | 1 | 67.17 ± 1.06 | ||||
| 2.5 | 73.78 ± 0.67 | 2.5 | 94.38 ± 0.29 | ||||
| 5 | 104.21 ± 0.9 | 5 | 104.47 ± 0.8 | ||||
| 10 | 104.07 ± 0.9 | 10 | 105.15 ± 1.1 |
| Formulation Codes | Drug | Zero Order | First Order | Higuchi | Korsmeyer-Peppas | |
|---|---|---|---|---|---|---|
| R2 | R2 | R2 | R2 | n | ||
| F5 | PG | 0.66 | 0.52 | 0.82 | 0.85 | 0.762 |
| MC | 0.66 | 0.49 | 0.80 | 0.81 | 0.534 | |
| F8 | PG | 0.69 | 0.55 | 0.84 | 0.88 | 0.693 |
| MC | 0.53 | 0.47 | 0.69 | 0.80 | 0.537 | |
| F13 | PG | 0.68 | 0.48 | 0.81 | 0.84 | 0.987 |
| MC | 0.46 | 0.36 | 0.62 | 0.68 | 0.550 | |
| Test/Analysis | +4 °C | +25 °C | ||||
|---|---|---|---|---|---|---|
| F5 | F8 | F13 | F5 | F8 | F13 | |
| Moisture Uptake Capacity | 1.22 ± 0.11 | 0.68 ± 0.23 | 0.48 ± 0.09 | 1.31 ± 0.41 | 0.73 ± 0.60 | 0.55 ± 0.13 |
| Foldability | 195 ± 5.50 | 205 ± 9.50 | 110 ± 6.50 | 190 ± 7.00 | 200 ± 5.50 | 100 ± 3.50 |
| Elongation Percent | 2.51 ± 0.14 | 9.67 ± 1.13 | 2.66 ± 0.59 | 2.43 ± 0.18 | 9.15 ± 1.81 | 2.51 ± 0.66 |
| Thickness (µm) | 30 ± 0.01 | 30 ± 0.01 | 30 ± 0.01 | 30 ± 0.01 | 30 ± 0.01 | 30 ± 0.01 |
| Transparency | 65 ± 3.20 | 47 ± 1.80 | 61 ± 2.50 | 64 ± 2.00 | 49 ± 1.70 | 57 ± 1.90 |
| Weight Variability | 0.03 ± 0.00 | 0.03 ± 0.00 | 0.03 ± 0.00 | 0.03 ± 0.00 | 0.03 ± 0.00 | 0.03 ± 0.00 |
| Swelling Degree | 197 ± 9.89 | 107 ± 7.45 | 159 ± 9.12 | 207 ± 3.32 | 109 ± 12.48 | 171 ± 6.18 |
| Content Uniformity for PG (mg) | 25.118 ± 0.32 | 24.883 ± 0.29 | 25.212 ± 0.42 | 25.325 ± 0.61 | 25.089 ± 0.12 | 24.913 ± 0.35 |
| Content Uniformity for MC (mg) | 0.497 ± 0.02 | 0.499 ± 0.01 | 0.511 ± 0.02 | 0.505 ± 0.01 | 0.488 ± 0.02 | 0.520 ± 0.03 |
| Disintegration Time (s) | 29 ± 2.87 | 18 ± 1.93 | 17 ± 1.46 | 30 ± 2.52 | 18 ± 2.18 | 17 ± 1.77 |
| Formulation Codes | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 | F9 | F10 | F11 | F12 | F13 | F14 | F15 | F16 | F17 | F18 | F19 | F20 | F21 | F22 | F23 | F24 | |
| Polymers | ||||||||||||||||||||||||
| Pullulan | - | - | - | - | - | 50 | 50 | 50 | 50 | 50 | 50 | 50 | 25 | 25 | 25 | 25 | 20 | 50 | - | - | - | - | - | - |
| NaCMC | 50 | - | - | - | - | - | - | - | - | - | - | - | - | 25 | - | - | 10 | - | 50 | - | - | - | - | - |
| Pectin | - | - | 25 | 25 | - | - | - | - | - | - | - | - | - | - | 25 | 12.5 | 10 | - | - | 50 | - | - | - | - |
| Sodium Alginate | - | 50 | 25 | 25 | 50 | - | - | - | - | - | - | - | 25 | - | - | 12.5 | 10 | - | - | - | - | - | - | - |
| PVP K-25 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 50 | - | - | - |
| PVP K-30 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 50 | - | - |
| HPMC E15 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 50 | - |
| HPMC K100 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 50 |
| Plasticizers | ||||||||||||||||||||||||
| Glycerin | - | - | - | 25 | 25 | 25 | - | 25 | - | - | 25 | 25 | 25 | 25 | 25 | 25 | 25 | - | - | - | - | - | - | - |
| Propylene Glycol | 25 | 25 | 25 | - | - | - | 25 | - | 25 | 25 | - | - | - | - | - | - | - | 25 | - | - | - | - | - | - |
| PEG 400 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 25 | - | - | - | 25 | - |
| PEG 4000 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 25 | - | - | - | 25 |
| D-Sorbitol | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 25 | - | - | - |
| PVA (low MW) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 25 | - | - |
| Saliva Stimulant | ||||||||||||||||||||||||
| Citric Acid | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
| Sweeteners | ||||||||||||||||||||||||
| Sodium Saccharin | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | - | - | - | - | - | - | - |
| Mannitol | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
| Aspartame | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
| Superdisintegrants | ||||||||||||||||||||||||
| NaStarch Glycolate | - | - | - | - | - | 15 | - | 15 | - | 15 | - | - | - | - | - | - | - | - | - | - | - | 15 | 15 | |
| Xanthan Gum | 15 | 15 | 15 | - | - | - | - | - | - | 15 | - | 15 | - | - | - | - | - | - | - | - | 15 | - | - | - |
| NaCroscarmellose | - | - | - | 15 | 15 | - | 15 | 15 | - | - | - | - | 15 | 15 | 15 | 15 | 15 | - | 15 | 15 | - | - | - | - |
| PVP-CL | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 15 | - | - | - | 15 | - | - |
| Flavoring Agent | ||||||||||||||||||||||||
| Vanillin | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 |
| Surfactants | ||||||||||||||||||||||||
| SLS | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
| Poloxamer 407 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
| Ultrapure Water | ||||||||||||||||||||||||
| qs | qs | qs | qs | qs | qs | qs | qs | qs | qs | qs | qs | qs | qs | qs | qs | Qs | qs | qs | qs | qs | qs | qs | qs | |
| Formulation Codes | Contents | Concentration | Storage Condition |
|---|---|---|---|
| Blank | - | - | +4 °C |
| F5 | PG + MC | 5 mg/mL + 0.1 mg/mL | +4 °C |
| F8 | PG + MC | 5 mg/mL + 0.1 mg/mL | +4 °C |
| F13 | PG + MC | 5 mg/mL + 0.1 mg/mL | +4 °C |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Özakar, E.; Sevinç-Özakar, R.; Yılmaz, B. Preparation, Characterization, and Evaluation of Cytotoxicity of Fast Dissolving Hydrogel Based Oral Thin Films Containing Pregabalin and Methylcobalamin. Gels 2023, 9, 147. https://doi.org/10.3390/gels9020147
Özakar E, Sevinç-Özakar R, Yılmaz B. Preparation, Characterization, and Evaluation of Cytotoxicity of Fast Dissolving Hydrogel Based Oral Thin Films Containing Pregabalin and Methylcobalamin. Gels. 2023; 9(2):147. https://doi.org/10.3390/gels9020147
Chicago/Turabian StyleÖzakar, Emrah, Rukiye Sevinç-Özakar, and Bilal Yılmaz. 2023. "Preparation, Characterization, and Evaluation of Cytotoxicity of Fast Dissolving Hydrogel Based Oral Thin Films Containing Pregabalin and Methylcobalamin" Gels 9, no. 2: 147. https://doi.org/10.3390/gels9020147
APA StyleÖzakar, E., Sevinç-Özakar, R., & Yılmaz, B. (2023). Preparation, Characterization, and Evaluation of Cytotoxicity of Fast Dissolving Hydrogel Based Oral Thin Films Containing Pregabalin and Methylcobalamin. Gels, 9(2), 147. https://doi.org/10.3390/gels9020147