Co-Infection with Plasmodium vivax and COVID-19 in Thailand
Abstract
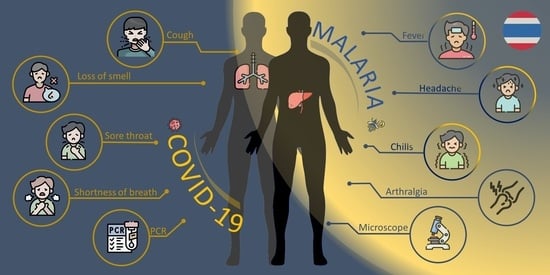
:1. Introduction
2. Case Report
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, L.; Wang, Y.; Ye, D.; Liu, Q. Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence. Int. J. Antimicrob. Agents 2020, 55, 105948. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/table (accessed on 10 February 2022).
- Gutman, J.R.; Lucchi, N.W.; Cantey, P.T.; Steinhardt, L.C.; Samuels, A.M.; Kamb, M.L.; Kapella, B.K.; McElroy, P.D.; Udhayakumar, V.; Lindblade, K.A. Malaria and Parasitic Neglected Tropical Diseases: Potential Syndemics with COVID-19? Am. J. Trop. Med. Hyg. 2020, 103, 572–577. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Malaria Report 2021. Available online: https://www.who.int/publications/i/item/9789240040496 (accessed on 6 December 2021).
- Di Gennaro, F.; Marotta, C.; Locantore, P.; Pizzol, D.; Putoto, G. Malaria and COVID-19: Common and Different Findings. Trop. Med. Infect. Dis. 2020, 5, 141. [Google Scholar] [CrossRef]
- Malaria Online Database, Thailand Malaria Elimination Program. Available online: http://malaria.ddc.moph.go.th/malariar10/index_newversion.php (accessed on 11 May 2022).
- Singh, B.; Ryan, H.; Kredo, T.; Chaplin, M.; Fletcher, T. Chloroquine or hydroxychloroquine for prevention and treatment of COVID-19. Cochrane Database Syst. Rev. 2021, 2, CD013587. [Google Scholar] [CrossRef] [PubMed]
- Emergency Operations Center DoDC, Ministry of Public Health Thailand. The Coronavirus Disease 2019 Situation. Available online: https://ddc.moph.go.th/viralpneumonia/eng/file/situation/situation-no695-061264.pdf (accessed on 6 December 2021).
- Wilairatana, P.; Masangkay, F.R.; Kotepui, K.U.; Milanez, G.J.; Kotepui, M. Prevalence and characteristics of malaria among COVID-19 individuals: A systematic review, meta-analysis, and analysis of case reports. PLoS Negl. Trop. Dis. 2021, 15, e0009766. [Google Scholar] [CrossRef] [PubMed]
- Hussein, R.; Guedes, M.; Ibraheim, N.; Ali, M.M.; El-Tahir, A.; Allam, N.; Abuakar, H.; Pecoits-Filho, R.; Kotanko, P. CLINICAL MICROBIOLOGY AND INFECTION. Available online: https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(22)00167-7/fulltext (accessed on 15 July 2022).
- Achan, J.; Serwanga, A.; Wanzira, H.; Kyagulanyi, T.; Nuwa, A.; Magumba, G.; Kusasira, S.; Sewanyana, I.; Tetteh, K.; Drakeley, C.; et al. Current malaria infection, previous malaria exposure, and clinical profiles and outcomes of COVID-19 in a setting of high malaria transmission: An exploratory cohort study in Uganda. Lancet Microbe 2022, 3, e62–e71. [Google Scholar] [CrossRef]
- Mahajan, N.N.; Gajbhiye, R.K.; Bahirat, S.; Lokhande, P.D.; Mathe, A.; Rathi, S.; Warty, N.; Mahajan, K.N.; Srivastava, V.; Kuppusamy, P.; et al. Co-infection of malaria and early clearance of SARS-CoV-2 in healthcare workers. J. Med. Virol. 2021, 93, 2431–2438. [Google Scholar] [CrossRef] [PubMed]
- Kishore, R.; Dhakad, S.; Arif, N.; Dar, L.; Mirdha, B.R.; Aggarwal, R.; Kabra, S.K. COVID-19: Possible Cause of Induction of Relapse of Plasmodium vivax Infection. Indian J. Pediatr. 2020, 87, 751–752. [Google Scholar] [CrossRef]
- Mahajan, N.N.; Kesarwani, S.N.; Shinde, S.S.; Nayak, A.; Modi, D.N.; Mahale, S.D.; Gajbhiye, R.K. Co-infection of malaria and dengue in pregnant women with SARS-CoV-2. Int. J. Gynecol. Obstet. 2020, 151, 459–462. [Google Scholar] [CrossRef]
- Pusparani, A.; Henrina, J.; Cahyadi, A. Co-infection of COVID-19 and recurrent malaria. J. Infect. Dev. Ctries. 2021, 15, 625–629. [Google Scholar] [CrossRef]
- Ray, M.; Vazifdar, A.; Shivaprakash, S. Co-infection with Malaria and Coronavirus Disease-2019. J. Glob. Infect. Dis. 2020, 12, 162–163. [Google Scholar] [CrossRef]
- Sardar, S.; Sharma, R.; Alyamani, T.Y.M.; Aboukamar, M. COVID-19 and Plasmodium vivax malaria co-infection. IDCases 2020, 21, e00879. [Google Scholar] [CrossRef] [PubMed]
- Shahid, Z.; Karim, N.; Shahid, F.; Yousaf, Z. COVID-19 Associated Imported Plasmodium vivax Malaria Relapse: First Reported Case and Literature Review. Res. Rep. Trop. Med. 2021, 12, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Schantz-Dunn, J.; Nour, N.M. Malaria and pregnancy: A global health perspective. Rev. Obstet. Gynecol. 2009, 2, 186–192. [Google Scholar] [PubMed]
- Caglar, B.; Karaali, R.; Balkan, I.I.; Mete, B.; Aygun, G. COVID-19 and Plasmodium ovale Malaria: A Rare Case of Co-Infection. Korean J. Parasitol. 2021, 59, 399–402. [Google Scholar] [CrossRef]
- Chen, M.; Gao, S.; Ai, L.; Chen, J.; Feng, T.; Chen, Z.; Zhang, X.; Deng, S.; Lin, Z.; Tang, Y.; et al. The First Reported Case of COVID-19 and Plasmodium ovale Malaria Coinfection—Guangdong Province, China, January 2021. China CDC Wkly. 2021, 3, 454–455. [Google Scholar] [CrossRef]
- Papaccio, M.; Castellani, R.; Zanardini, C.; Sartori, E.; Prefumo, F.; Saccani, B. Pregnancy and COVID-19: Do not overlook malaria. Int. J. Gynaecol. Obstet. 2021, 153, 550–551. [Google Scholar] [CrossRef]
- Battle, K.E.; Baird, J.K. The global burden of Plasmodium vivax malaria is obscure and insidious. PLoS Med. 2021, 18, e1003799. [Google Scholar] [CrossRef]
- Kunno, J.; Supawattanabodee, B.; Sumanasrethakul, C.; Wiriyasivaj, B.; Kuratong, S.; Kaewchandee, C. Comparison of Different Waves during the COVID-19 Pandemic: Retrospective Descriptive Study in Thailand. Adv. Prev. Med. 2021, 2021, 5807056. [Google Scholar] [CrossRef]
- Haddawy, P.; Lawpoolsri, S.; Sa-Ngamuang, C.; Su Yin, M.; Barkowsky, T.; Wiratsudakul, A.; Kaewkungwal, J.; Khamsiriwatchara, A.; Sa-Angchai, P.; Sattabongkot, J.; et al. Effects of COVID-19 government travel restrictions on mobility in a rural border area of Northern Thailand: A mobile phone tracking study. PLoS ONE 2021, 16, e0245842. [Google Scholar] [CrossRef]
- Osei, S.A.; Biney, R.P.; Anning, A.S.; Nortey, L.N.; Ghartey-Kwansah, G. Low incidence of COVID-19 case severity and mortality in Africa; Could malaria co-infection provide the missing link? BMC Infect. Dis. 2022, 22, 78. [Google Scholar] [CrossRef] [PubMed]
- Hussein, M.I.H.; Albashir, A.A.D.; Elawad, O.; Homeida, A. Malaria and COVID-19: Unmasking their ties. Malar. J. 2020, 19, 457. [Google Scholar] [CrossRef] [PubMed]
- Nasomsong, W.; Luvira, V.; Phiboonbanakit, D. Case Report: Dengue and COVID-19 Coinfection in Thailand. Am. J. Trop. Med. Hyg. 2020, 104, 487–489. [Google Scholar] [CrossRef] [PubMed]
- Douglas, N.M.; Nosten, F.; Ashley, E.A.; Phaiphun, L.; van Vugt, M.; Singhasivanon, P.; White, N.J.; Price, R.N. Plasmodium vivax recurrence following falciparum and mixed species malaria: Risk factors and effect of antimalarial kinetics. Clin. Infect. Dis. 2011, 52, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Shanks, G.D.; White, N.J. The activation of vivax malaria hypnozoites by infectious diseases. Lancet Infect. Dis. 2013, 13, 900–906. [Google Scholar] [CrossRef]
- Guha, S.K.; Biswas, M.; Gupta, B.; Acharya, A.; Halder, S.; Saha, B.; Chatterjee, M.; Kundu, P.K.; Maji, A.K. A report on incidence of COVID-19 among febrile patients attending a malaria clinic. Trop. Parasitol. 2021, 11, 38–41. [Google Scholar] [CrossRef]
- Orish, V.N.; Boakye-Yiadom, E.; Ansah, E.K.; Alhassan, R.K.; Duedu, K.; Awuku, Y.A.; Owusu-Agyei, S.; Gyapong, J.O. Is malaria immunity a possible protection against severe symptoms and outcomes of COVID-19? Ghana Med. J. 2021, 55, 56–63. [Google Scholar] [CrossRef]


| Laboratory Test | Result | Normal Range |
|---|---|---|
| Hemoglobin (Hb) | 11.5 | 13.8–17.2 g/dL |
| Hematocrit (Hct) | 34 | 40.7–50.3% |
| Red blood cell count | 4.27 | 3.50–5.50 × 106 cell/uL |
| White blood cell count | 4190 | 4000–10,000 cell/cu.m |
| Platelet count | 92,000 | 140,000–400,000 cell/cu.m |
| Mean corpuscular volume (MCV) | 80.4 | 80–100 fL |
| Mean corpuscular hemoglobin (MCH) | 26.9 | 27–31 pg |
| Mean corpuscular hemoglobin concentration (MCHC) | 33.5 | 31–37 g/dL |
| Neutrophil | 59 | 50–70% |
| Lymphocyte | 21 | 20–40% |
| Monocyte | 16 | 3–8% |
| Eosinophil | 2 | 0–5% |
| Basophil | 0 | 0–2% |
| Atypical lymphocyte | 2 | 0 |
| Red blood cell morphology | Normal | Normal |
| Malaria (Thin–Thick film) | Positive | |
| Malaria type | Plasmodium vivax | |
| Parasitemia | 0.35% | |
| SARS-CoV2 Real time RT-PCR | Detected | |
| Nasopharyngeal swab | N gene Ct = 27.01 | |
| ORF1 ab gene Ct = 25.94 | ||
| Dengue NS1 | Negative | |
| Dengue Ab,IgM | Negative | |
| Dengue Ab,IgG | Negative | |
| Leptospira Antibody | IgM weakly positive |
| Laboratory Test | Result | Normal Range |
|---|---|---|
| Blood urea nitrogen (BUN) | 16 | 7–25 mg/dL |
| Creatinine | 0.68 | 0.70–1.17 mg/dL |
| e-GFR | 132.73 | 97.00–137.00 mL/mon/L |
| Sodium (Na) | 133 | 135–145 mmol/L |
| Potassium (K) | 3.6 | 3.5–5.1 mmol/L |
| Chloride (Cl) | 93 | 99–111 mmol/L |
| Carbon dioxide (CO2) | 24 | 22–33 mmol/L |
| Total Protein | 6.8 | 6.0–8.3 g/dL |
| Albumin (Blood) | 3.5 | 3.2–5.2 g/dL |
| Globulin | 3.3 | 2.0–3.0 g/dL |
| Total Bilirubin | 1.6 | 0–2 mg/dL |
| Direct Bilirubin | 0.6 | 0–0.2 mg/dL |
| Aspartate transaminase (AST) | 22 | 0–35 U/L |
| Alanine transaminase (ALT) | 42 | 0–45 U/L |
| Alkaline phosphatase (ALP) | 133 | 53–128 U/L |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boonyarangka, P.; Phontham, K.; Sriwichai, S.; Poramathikul, K.; Harncharoenkul, K.; Kuntawunginn, W.; Maneesrikhum, N.; Srisawath, S.; Seenuan, C.; Thanyakait, C.; et al. Co-Infection with Plasmodium vivax and COVID-19 in Thailand. Trop. Med. Infect. Dis. 2022, 7, 145. https://doi.org/10.3390/tropicalmed7080145
Boonyarangka P, Phontham K, Sriwichai S, Poramathikul K, Harncharoenkul K, Kuntawunginn W, Maneesrikhum N, Srisawath S, Seenuan C, Thanyakait C, et al. Co-Infection with Plasmodium vivax and COVID-19 in Thailand. Tropical Medicine and Infectious Disease. 2022; 7(8):145. https://doi.org/10.3390/tropicalmed7080145
Chicago/Turabian StyleBoonyarangka, Parat, Kittijarankon Phontham, Sabaithip Sriwichai, Kamonporn Poramathikul, Krit Harncharoenkul, Worachet Kuntawunginn, Napat Maneesrikhum, Sarayouth Srisawath, Chanida Seenuan, Chattakorn Thanyakait, and et al. 2022. "Co-Infection with Plasmodium vivax and COVID-19 in Thailand" Tropical Medicine and Infectious Disease 7, no. 8: 145. https://doi.org/10.3390/tropicalmed7080145
APA StyleBoonyarangka, P., Phontham, K., Sriwichai, S., Poramathikul, K., Harncharoenkul, K., Kuntawunginn, W., Maneesrikhum, N., Srisawath, S., Seenuan, C., Thanyakait, C., Inkabajan, K., Pludpiem, S., Pidtana, K., Demons, S., Vesely, B., Wojnarski, M., Griesenbeck, J. S., & Spring, M. (2022). Co-Infection with Plasmodium vivax and COVID-19 in Thailand. Tropical Medicine and Infectious Disease, 7(8), 145. https://doi.org/10.3390/tropicalmed7080145