Geographical Variation in Mental Hospital Discharges in Greece: A Nationwide Study (1999–2012)
Abstract
:1. Introduction
2. Materials and Methods
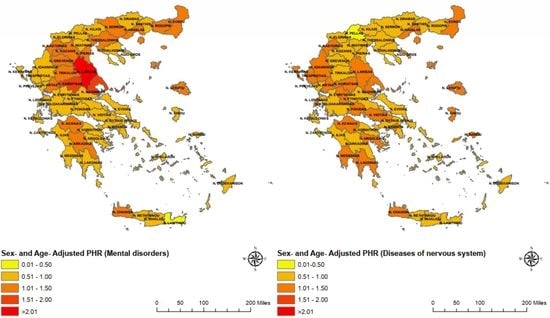
3. Results
3.1. Schizophrenic and Other Psychoses
3.2. Affective Psychoses
3.3. Senile and Presenile Organic Psychotic Conditions
3.4. Alcohol Dependence Syndrome
3.5. Drug Dependence
3.6. Correlation between Sex- and Age-Adjusted PHR and Sociodemographic Characteristics of Each Prefecture
4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Mental Disorders. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 24 May 2021).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Wittchen, H.U.; Jacobi, F.; Rehm, J.; Gustavsson, A.; Svensson, M.; Jönsson, B.; Olesen, J.; Allgulander, C.; Alonso, J.; Faravelli, C.; et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 655–679. [Google Scholar] [CrossRef] [Green Version]
- Skapinakis, P.; Bellos, S.; Koupidis, S.; Grammatikopoulos, I.; Theodorakis, P.N.; Mavreas, V. Prevalence and sociodemographic associations of common mental disorders in a nationally representative sample of the general population of Greece. BMC Psychiatry 2013, 13, 163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kosmidis, M.H.; Vlachos, G.S.; Anastasiou, C.A.; Yannakoulia, M.; Dardiotis, E.; Hadjigeorgiou, G.; Sakka, P.; Ntanasi, E.; Scarmeas, N. Dementia Prevalence in Greece. Alzheimer Dis. Assoc. Disord. 2018, 32, 232–239. [Google Scholar] [CrossRef] [PubMed]
- ESEMeD/MHEDEA 2000 Investigators; Alonso, J.; Angermeyer, M.C.; Bernert, S.; Bruffaerts, R.; Brugha, T.S.; Bryson, H.; de Girolamo, G.; de Graaf, R.; Demyttenaere, K.; et al. Prevalence of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr. Scand. Suppl. 2004, 109, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.L. Rural-urban differences in the prevalence of major depression and associated impairment. Soc. Psychiatry Psychiatr. Epidemiol. 2004, 39, 19–25. [Google Scholar] [CrossRef]
- Marangoni, C.; Hernandez, M.; Faedda, G.L. The role of environmental exposures as risk factors for bipolar disorder: A systematic review of longitudinal studies. J. Affect. Disord. 2016, 193, 165–174. [Google Scholar] [CrossRef]
- Rowland, T.A.; Marwaha, S. Epidemiology and risk factors for bipolar disorder. Ther. Adv. Psychopharmacol. 2018, 8, 251–269. [Google Scholar] [CrossRef]
- Smith, S.; Chakraborty, N. Reasons for prolonged admissions on acute adult psychiatry wards. Prog. Neurol. Psychiatry 2012, 16, 28–31. [Google Scholar] [CrossRef]
- Heslin, K.C.; Weiss, A.J. Hospital Readmissions Involving Psychiatric Disorders, 2012: Statistical Brief #189; Healthcare Cost and Utilization Project (HCUP) Statistical Briefs; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2006.
- Olfson, M.; Ascher-Svanum, H.; Faries, D.E.; Marcus, S.C. Predicting psychiatric hospital admission among adults with schizophrenia. Psychiatr. Serv. 2011, 62, 1138–1145. [Google Scholar] [CrossRef]
- Kingwell, E.; Marriott, J.J.; Jetté, N.; Pringsheim, T.; Makhani, N.; Morrow, S.A.; Fisk, J.D.; Evans, C.; Béland, S.G.; Kulaga, S.; et al. Incidence and prevalence of multiple sclerosis in Europe: A systematic review. BMC Neurol. 2013, 13, 128. [Google Scholar] [CrossRef] [Green Version]
- Luetic, G.; Menichini, M.L. Multiple sclerosis prevalence in Santa Fe province, Argentina. Mult. Scler. Relat. Disord. 2020, 41, 102006. [Google Scholar] [CrossRef] [PubMed]
- Browne, P.; Chandraratna, D.; Angood, C.; Tremlett, H.; Baker, C.; Taylor, B.V.; Thompson, A.J. Atlas of multiple sclerosis 2013: A growing global problem with widespread inequity. Neurology 2014, 83, 1022–1024. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madianos, M.G.; Zacharakis, C.; Tsitsa, C.; Stefanis, C. Geographical variation in mental hospital discharges in Greece and socioeconomic correlates: A nationwide study (1978–1993). Soc. Psychiatry Psychiatr. Epidemiol. 1999, 34, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Dadouli, K.; Ntellas, P.; Anagnostopoulos, L.; Bonotis, K.; Dardiotis, E.; Hadjichristodoulou, C. Geography of hospital admissions for multiple sclerosis in Greece. Mult. Scler. Relat. Disord. 2021, 49, 102735. [Google Scholar] [CrossRef] [PubMed]
- Statistics-ELSTAT. Available online: https://www.statistics.gr/en/statistics/-/publication/SAM03/2011 (accessed on 19 February 2021).
- Statistics-ELSTAT. Available online: https://www.statistics.gr/en/statistics/-/publication/SHE12/2012-M01 (accessed on 19 February 2021).
- Saha, S.; Chant, D.; Welham, J.; McGrath, J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005, 2, e141. [Google Scholar] [CrossRef]
- Bernal, J.L.; Cummins, S.; Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int. J. Epidemiol. 2017, 46, 348–355. [Google Scholar] [CrossRef]
- Age-Standardized Rates. Available online: https://www.statcan.gc.ca/eng/dai/btd/asr (accessed on 13 September 2020).
- Easy Way to Learn Standardization: Direct and Indirect Methods-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/22844209/ (accessed on 13 September 2020).
- Gordis, L. Epidemiology. In The Occurence of Disease, 5th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2014; pp. 75–81. [Google Scholar]
- Ord, J.K.; Getis, A. Local Spatial Autocorrelation Statistics: Distributional Issues and an Application. Geogr. Anal. 1995, 27, 286–306. [Google Scholar] [CrossRef]
- Anselin, L. Local Indicators of Spatial Association—LISA. Geogr. Anal. 1995, 27, 93–115. [Google Scholar] [CrossRef]
- Kεντρική Σελίδα EΛΣTAT-ELSTAT. Available online: https://www.statistics.gr/el/home (accessed on 18 September 2020).
- Bambra, C. Yesterday once more? Unemployment and health in the 21st century. J. Epidemiol. Community Health 2010, 64, 213–215. [Google Scholar] [CrossRef] [Green Version]
- Agriculture, Livestock, Fishery-ELSTAT. Available online: https://www.statistics.gr/en/statistics/agr (accessed on 21 May 2021).
- Penchansky, R.; Thomas, J.W. The concept of access: Definition and relationship to consumer satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef]
- Manjunatha, N.; Singh, G.; Chaturvedi, S.K. Manochaitanya programme for better utilization of primary health centres. Indian J. Med. Res. 2017, 145, 163–165. [Google Scholar] [PubMed]
- Ventriglio, A.; Torales, J.; Castaldelli-Maia, J.M.; De Berardis, D.; Bhugra, D. Urbanization and emerging mental health issues. CNS Spectr. 2021, 26, 43–50. [Google Scholar] [CrossRef] [PubMed]
- McElroy, S.L.; Altshuler, L.L.; Suppes, T.; Keck, P.E., Jr.; Frye, M.A.; Denicoff, K.D.; Nolen, W.A.; Kupka, R.W.; Leverich, G.S.; Rochussen, J.R.; et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am. J. Psychiatry 2001, 158, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Hong, M.; Ha, T.H.; Lee, S.; Oh, S.; Myung, W. Clinical correlates of alcohol use disorder in depressed patients with unipolar and bipolar disorder. Psychiatry Investig. 2019, 16, 926–932. [Google Scholar] [CrossRef]
- Cassidy, F.; Ahearn, E.P.; Carroll, B.J. Substance abuse in bipolar disorder. Bipolar. Disord. 2001, 3, 181–188. [Google Scholar] [CrossRef]
- Hunt, G.E.; Large, M.M.; Cleary, M.; Lai, H.M.X.; Saunders, J.B. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990–2017: Systematic review and meta-analysis. Drug Alcohol Depend. 2018, 191, 234–258. [Google Scholar] [CrossRef]
- Schwarzinger, M.; Pollock, B.G.; Hasan, O.S.; Dufouil, C.; Rehm, J.; Baillot, S.; Guibert, Q.; Planchet, F.; Luchini, S. Contribution of alcohol use disorders to the burden of dementia in France 2008–13: A nationwide retrospective cohort study. Lancet Public Health 2018, 3, e124–e132. [Google Scholar] [CrossRef]
- Lindström, M.; Rosvall, M. Marital status, social capital, economic stress, and mental health: A population-based study. Soc. Sci. J. 2012, 49, 339–342. [Google Scholar] [CrossRef] [Green Version]
- Goel, N.; Behere, P. Effect of Marriage on Clinical Outcome of Persons with Bipolar Affective Disorder: A Case-control Study. Int. J. Sci. Study 2016, 4, 46–50. [Google Scholar]
- Goodwin, F.K.; Jamison, K.R. Personality, personality disorders, and interpersonal functioning. In Manic-Depressive Illness Bipolar Disorders and Recurrent Depression, 2nd ed.; Oxford University Press: New York, NY, USA, 2007; pp. 323–354. [Google Scholar]
- Bauwens, F.; Tracy, A.; Pardoen, D.; Vander Elst, M.; Mendlewicz, J. Social adjustment of remitted bipolar and unipolar out-patients: A comparison with age- and sex-matched controls. Br. J. Psychiatry 1991, 159, 239–244. [Google Scholar] [CrossRef]
- Guze, S.B.; Woodruff, R.A.; Clayton, P.J. ‘Secondary’ affective disorder: A study of 95 cases. Psychol. Med. 1971, 1, 426–428. [Google Scholar] [CrossRef] [PubMed]
- Suppes, T.; Leverich, G.S.; Keck, P.E., Jr.; Nolen, W.A.; Denicoff, K.D.; Altshuler, L.L.; McElroy, S.L.; Rush, A.J.; Kupka, R.; Frye, M.A.; et al. The Stanley Foundation Bipolar Treatment Outcome Network-II. Demographics and illness characteristics of the first 261 patients. J. Affect. Disord. 2001, 67, 45–59. [Google Scholar] [CrossRef]
- Isaac, M.; Chand, P.; Murthy, P. Schizophrenia outcome measures in the wider international community. Br. J. Psychiatry 2007, 191 (Suppl. 50), s71–s77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gariépy, G.; Honkaniemi, H.; Quesnel-Vallée, A. Social support and protection from depression: Systematic review of current findings in western countries. Br. J. Psychiatry 2016, 209, 284–293. [Google Scholar] [CrossRef]





| ICD-9 Codes | Diseases |
|---|---|
| 320–359 | Diseases of the nervous system Inflammatory diseases of the central nervous system (320–326) Hereditary and Degenerative diseases of the central nervous system (330–337) Other disorders of the central nervous system (340–349) Disorders of the peripheral nervous system (350–359) |
| 290–319 | Mental disorders |
| 290 | Senile and presenile organic psychotic conditions |
| 291–295 | Schizophrenic and other psychoses |
| 296 | Affective psychoses |
| 303 | Alcohol dependence syndrome |
| 304 | Drug dependence |
| Condition | Total Hospitalizations | Hospitalizations from 2006–2012 | Annual Average Hospitalizations | Hospitalization Rate Male:Female | Average Number of Days of Treatment per Year | |
|---|---|---|---|---|---|---|
| Male | Female | |||||
| Schizophrenia and other psychoses | 219,046 | 106,978 | 15,646 | 1.7:1 | 296.9 | 341.0 |
| Affective psychoses | 99,234 | 54,733 | 7088 | 1:1.4 | 45.1 | 41.0 |
| Senile and presenile organic psychotic conditions | 37,279 | 21,966 | 2663 | 1:1.7 | 64.8 | 82.5 |
| Alcohol dependence syndrome | 24,570 | 12,636 | 1755 | 7.5:1 | 28.7 | 25.1 |
| Drug dependence syndrome | 23,454 | 12,945 | 1675 | 6.2:1 | 36.3 | 19.2 |
| Sex | Disease | Moran’s Index | z-Score | p-Value |
|---|---|---|---|---|
| Male | Mental disorders | 0.1554 | 3.5630 | <0.001 |
| Diseases of the nervous system | 0.0571 | 1.5405 | 0.123 | |
| Senile and presenile organic psychotic conditions | 0.0763 | 2.0017 | 0.045 | |
| Schizophrenic and other psychoses | 0.2718 | 4.1254 | <0.001 | |
| Affective psychoses | 0.1010 | 1.8694 | 0.062 | |
| Alcohol dependence syndrome | 0.1806 | 2.83499 | 0.005 | |
| Drug dependence | 0.1728 | 2.9360 | 0.003 | |
| Female | Mental disorders | 0.0987 | 1.7667 | 0.077 |
| Diseases of the nervous system | 0.0428 | 0.9782 | 0.328 | |
| Senile and presenile organic psychotic conditions | 0.0790 | 1.4651 | 0.143 | |
| Schizophrenic and other psychoses | 0.2294 | 3.5203 | <0.001 | |
| Affective psychoses | 0.1532 | 2.5596 | 0.010 | |
| Alcohol dependence syndrome | −0.0424 | −0.3340 | 0.738 | |
| Drug dependence | 0.0403 | 0.8764 | 0.381 |
| Alcohol Dependence Syndrome | Drug Dependence | Diseases of the Nervous System | |
|---|---|---|---|
| Diseases of the nervous system | 0.316 | 0.906 | - |
| Schizophrenic and other psychoses | <0.001 R = 0.492 | 0.062 R = 0.260 | 0.859 |
| Affective psychoses | <0.001 R = 0.534 | 0.129 | 0.043 R = 0.282 |
| Senile and presenile organic psychotic conditions | <0.001 R = 0.543 | 0.266 | 0.019 R = 0.323 |
| Alcohol dependence syndrome | - | 0.078 | 0.316 |
| Drug dependence | 0.078 R = 0.247 | - | 0.906 |
| Tertiary Education | Secondary Education | Lower Secondary Education | Primary Education | <6th Grade of Primary Education | |
|---|---|---|---|---|---|
| Schizophrenia psychoses | 0.525 | 0.010 R = −0.356 | 0.007 R = −0.370 | 0.212 | 0.002 R = 0.423 |
| Affective psychoses | 0.283 | 0.503 | 0.040 R = −0.286 | 0.386 | 0.212 |
| Senile and presenile organic psychosis | 0.965 | 0.194 | 0.162 | 0.845 | 0.370 |
| Alcohol dependence syndrome | 0.514 | 0.026 R = −0.308 | 0.045 R = −0.279 | 0.482 | 0.015 R = 0.336 |
| Drug dependence | 0.171 | 0.752 | 0.882 | 0.020 R = −0.323 | 0.450 |
| Schizophrenia and Other Psychoses | Affective Psychoses | Senile and Presenile Organic Psychotic Conditions | Alcohol Dependence Syndrome | Drug Dependence | |
|---|---|---|---|---|---|
| Armed forces occupations | 0.1% | 0.4% | 0.0% | 0.0% | 0.9% |
| Managers | 1.0% | 2.2% | 0.1% | 3.8% | 2.0% |
| Professional | 2.0% | 4.7% | 0.1% | 3.9% | 1.1% |
| Technicians and associate professionals | 0.1% | 0.4% | 0.0% | 0.2% | 0.3% |
| Clerical support workers | 3.8% | 7.9% | 0.1% | 8.0% | 4.3% |
| Service and sales workers | 1.0% | 1.5% | 0.0% | 1.7% | 2.4% |
| Skilled agricultural, forestry and fishery workers | 6.3% | 5.5% | 0.2% | 11.5% | 2.7% |
| Craft and related trades workers | 1.2% | 1.4% | 0.0% | 3.9% | 5.5% |
| Plant and machine operators, and assemblers | 0.4% | 0.6% | 0.0% | 1.2% | 1.4% |
| Elementary occupations | 1.9% | 2.8% | 0.1% | 5.2% | 3.5% |
| Retirees, Housewives, Students | 78.6% | 70.1% | 99.2% | 51.4% | 64.0% |
| Unemployment | 3.5% | 2.5% | 0.1% | 9.2% | 11.9% |
| Schizophrenic and Other Psychoses | Affective Psychoses | Senile and Presenile Organic Psychotic Conditions | Alcohol Dependence Syndrome | Drug Dependence | |
|---|---|---|---|---|---|
| Widow | 6.4% | 6.4% | 44.3% | 2.5% | 0.6% |
| Married | 28.3% | 53.6% | 46.6% | 56.3% | 16.9% |
| Unmarried | 55.9% | 29.8% | 6.2% | 28.4% | 74.5% |
| Divorced | 4.5% | 5.6% | 1.1% | 7.2% | 4.2% |
| Non-responders | 4.9% | 4.7% | 1.9% | 5.6% | 3.9% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dadouli, K.; Hatziefthimiou, A.; Mouchtouri, V.A.; Ntellas, P.; Anagnostopoulos, L.; Koureas, M.; Bonotis, K.; Christodoulou, N.; Hadjichristodoulou, C. Geographical Variation in Mental Hospital Discharges in Greece: A Nationwide Study (1999–2012). Psych 2022, 4, 200-214. https://doi.org/10.3390/psych4020017
Dadouli K, Hatziefthimiou A, Mouchtouri VA, Ntellas P, Anagnostopoulos L, Koureas M, Bonotis K, Christodoulou N, Hadjichristodoulou C. Geographical Variation in Mental Hospital Discharges in Greece: A Nationwide Study (1999–2012). Psych. 2022; 4(2):200-214. https://doi.org/10.3390/psych4020017
Chicago/Turabian StyleDadouli, Katerina, Apostolia Hatziefthimiou, Varvara A. Mouchtouri, Panagiotis Ntellas, Lemonia Anagnostopoulos, Michalis Koureas, Konstantinos Bonotis, Nikolaos Christodoulou, and Christos Hadjichristodoulou. 2022. "Geographical Variation in Mental Hospital Discharges in Greece: A Nationwide Study (1999–2012)" Psych 4, no. 2: 200-214. https://doi.org/10.3390/psych4020017
APA StyleDadouli, K., Hatziefthimiou, A., Mouchtouri, V. A., Ntellas, P., Anagnostopoulos, L., Koureas, M., Bonotis, K., Christodoulou, N., & Hadjichristodoulou, C. (2022). Geographical Variation in Mental Hospital Discharges in Greece: A Nationwide Study (1999–2012). Psych, 4(2), 200-214. https://doi.org/10.3390/psych4020017