Diagnosis and Treatment of Primary and Secondary Lung Cancers
A topical collection in Cancers (ISSN 2072-6694). This collection belongs to the section "Clinical Research of Cancer".
Viewed by 93436Editor
2. Department of Oncology and Hemato-Oncology, University of Milan, 20141 Milan, Italy
Interests: lung cancer surgery; thoracic oncology; early-stage lung cancer; locally advanced lung cancer
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
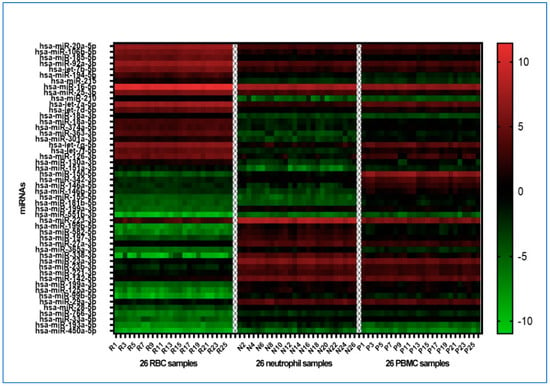
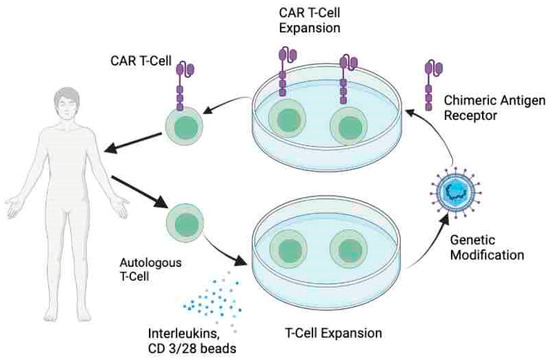
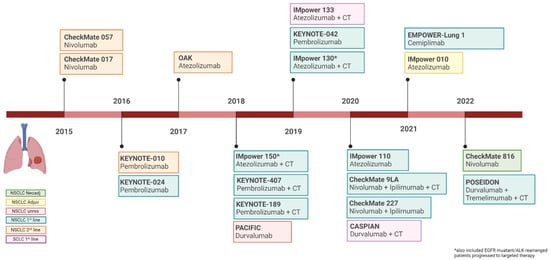
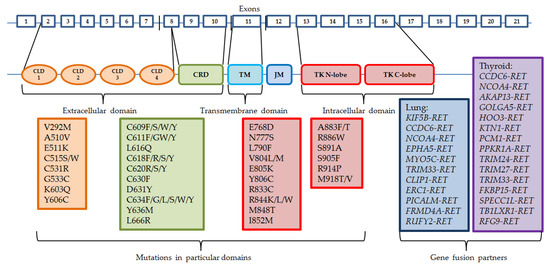
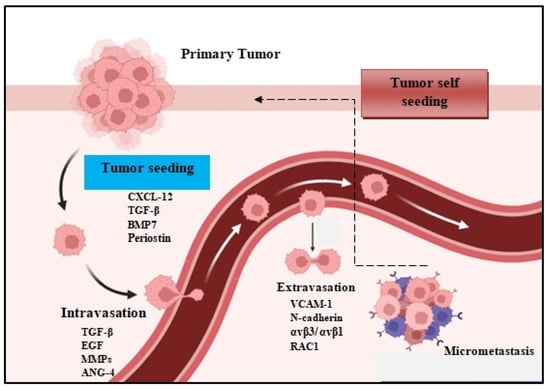
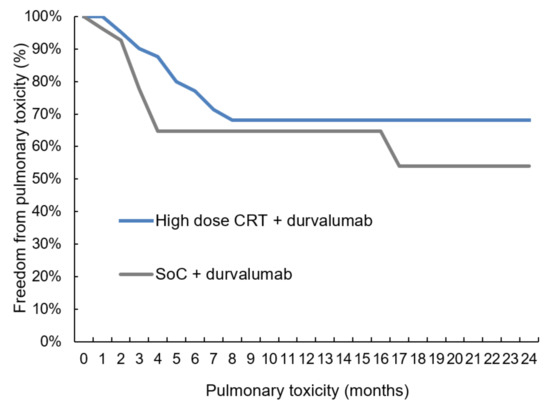
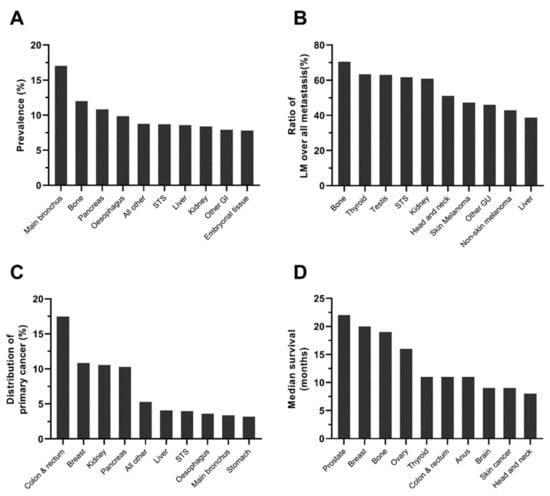
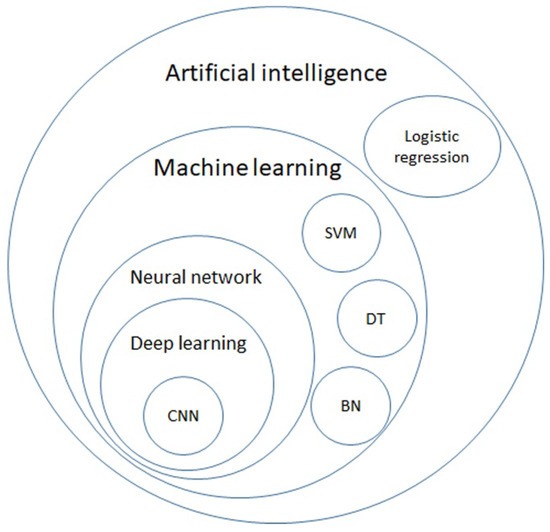
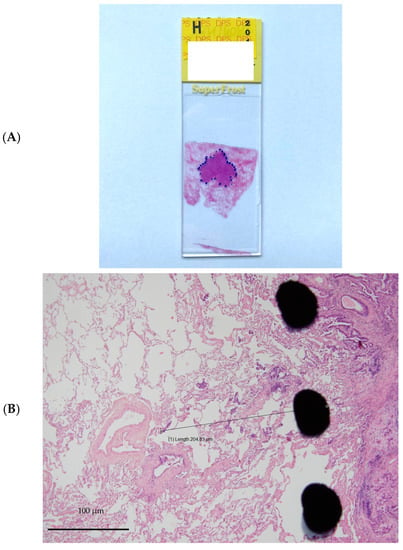
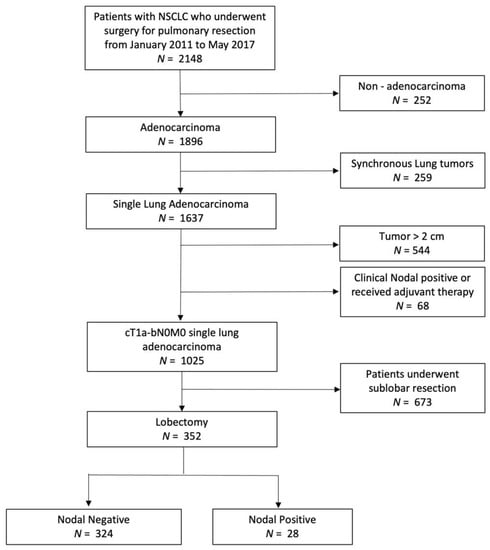
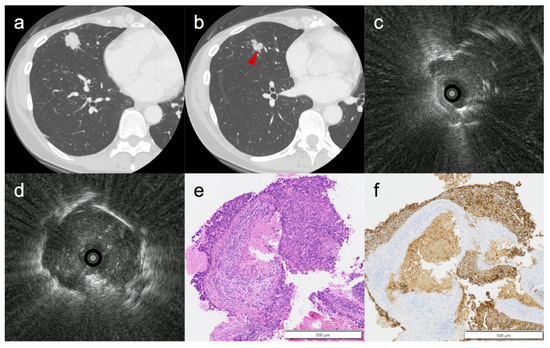
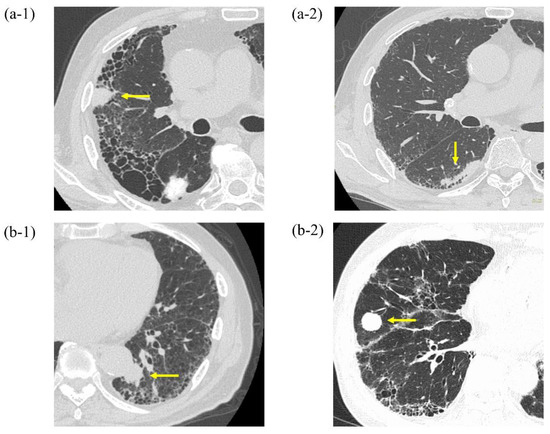
Both primary and secondary tumors of the chest are major issues for clinicians; in fact, on the one hand, primary lung cancer is one of the most frequently diagnosed cancers and is the leading cause of cancer-related death worldwide. On the other hand, the lung is the second most common site of metastases, and pulmonary metastasectomy is the most frequent surgical resection undertaken by thoracic surgeons. Significant developments have recently been shown in clinical settings, both in terms of diagnosis and treatment: for example, the early diagnosis of lung nodules by computed tomography screening, circulating miRNA detection, minimally invasive diagnostic and therapeutic approaches such as endobronchial ultrasound, video-assisted thoracic surgery and robot-assisted thoracic surgery, immunotherapy, TKI inhibitors, and stereotactic body radiation therapy (SBRT) represent only some of the most significant and recent goals.
Moreover, other thoracic malignancies such as chest wall tumors, mediastinal tumors, and mesothelioma, although rare, represent the most advanced frontier of modern oncology.
In this Topical Collection, we would like to focus on the most significant cornerstones in the diagnosis and therapy of both primary and secondary thoracic cancers.
It is our pleasure to lead such a comprehensive Topical Collection, and we look forward to receiving your valuable contributions.
Prof. Francesco Petrella
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cancers is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- lung cancer
- lung metastases
- diagnosis
- lung resection
- computed tomography
- positron emission tomography
- stereotactic body radiation therapy (SBRT)
- immunotherapy