Quality of Life in Cancer Rehabilitation
A topical collection in Cancers (ISSN 2072-6694). This collection belongs to the section "Cancer Survivorship and Quality of Life".
Viewed by 72678Editors
Interests: cancer rehabilitation; supportive care of cancer; outcome research; psycho-oncology
Special Issues, Collections and Topics in MDPI journals
Interests: side effects management; supportive care & cancer rehabilitation; prehabilitation; exercise
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
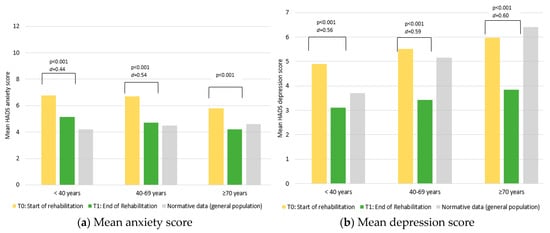
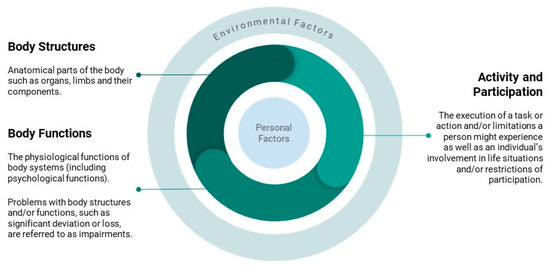
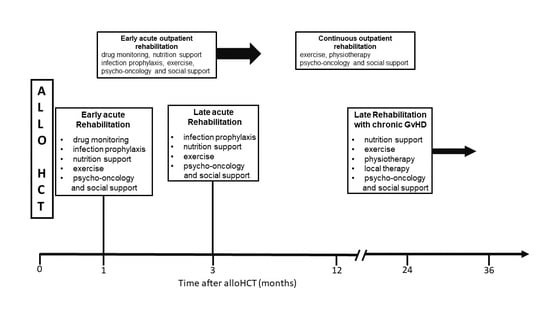
Many cancer survivors suffer from cancer-related symptoms, or adverse effects of surgery, radiotherapy or chemotherapy. These impairments include fatigue, pain, decreased muscular strength and endurance, lymphedema, weight loss, gastrointestinal symptoms, cognitive deficits, and chemotherapy-induced peripheral neuropathy. Thus, activities and participation can become permanently impaired. Some patients cannot return to work after cancer treatment or become dependent on care. Furthermore, psychological distress is common among cancer survivors, mainly depression and fear of cancer progression.
Cancer rehabilitation is aimed at improving cancer survivors’ quality of life by alleviation of these symptoms. It should also improve coping with cancer and help to develop strategies for resilience. To this end, physical therapies, exercise interventions, psycho-educative and emotionally supportive treatment modalities, and art and expression are combined in a multidisciplinary fashion. Other interventions include educational lectures on nutrition and lifestyle interventions for reduction of risk-factors such as smoking.
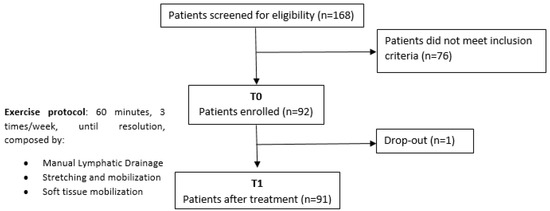
Rehabilitation can be performed as an inpatient or outpatient measure. In the Topical Collection, “Quality of Life in Cancer Rehabilitation”, an overview on current rehabilitative strategies is provided. Recent research on the efficacy of rehabilitation for sustained improvement of health-related quality of life is reported.
Prof. Dr. Thomas Licht
Prof. Dr. Richard Crevenna
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cancers is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- cancer-related symptoms
- cancer rehabilitation
- physical therapy
- medical psycho-oncology
- depression
- anxiety
- fatigue
- patient-reported outcomes
Planned Papers
The below list represents only planned manuscripts. Some of these manuscripts have not been received by the Editorial Office yet. Papers submitted to MDPI journals are subject to peer-review.
Title: Evaluating Oncological Rehabilitation Using Clinical Outcome Assessments: The Growing Importance of Patient-Reported Outcomes
Authors: Prof. Dr. Bernhard Holzner
Affiliation: Department of Psychiatry, Psychotherapy and Psychosomatics, The Medical University of Innsbruck, Innsbruck, Germany
Abstract: Oncological rehabilitation is aimed to help patients regain functioning and social participation. In order to justify and optimize rehabilitation, it is important to measure its outcomes in a structured way. Clinical outcome assessments (COAs) comprise different kinds of outcomes that can be used to evaluate rehabilitation. In this article we review the different types of COAs that are used in oncological rehabilitation: Clinician-Reported Outcomes (ClinROs), Observer-Reported Outcomes (ObsROs), Performance Outcomes (PerfOs), and Patient-Reported Outcomes (PROs). A special focus is placed on PROs, which are commonly defined as any direct report from the patient about their health condition without any interpretation by a third party. We review the current standing of PROs in oncological rehabilitation and trends to use PROs to benchmark value-based care. Further, we provide examples of PRO usage and highlight the benefits of electronic PRO collection, and offer advice on how to implement and integrate PROs in the oncological rehabilitation setting to maximize efficiency.
Title: Therapeutic Education and Physical Activity to Support Self-management of Cancer-related Fatigue in Hematologic Cancer Patients: Results of a Feasibility Randomized Controlled Trial
Authors: Monia Allisen Accogli; Monica Denti; Stefania Costi; Stefania Fugazzaro
Affiliation: 1 Physical Medicine and Rehabilitation Unit, Azienda Unità Sanitaria Locale-IRCCS di Reggio Emilia, Viale Risorgimento n°80, 42123 Reggio Emilia, Italy; 2 Scientific Directorate, Azienda Unità Sanitaria Locale-IRCCS di Reggio Emilia, Viale Umberto I n°50, 42123 Reggio Emilia, Italy 3 Department of Surgery, Medicine, Dentistry and Morphological Sciences, University of Modena and Reggio Emilia, Via del Pozzo n°74, 41100 Modena, Italy
Abstract: Cancer-related fatigue (CRF) is one of the most distressing symptoms reported by patients with cancer. Physical activity and therapeutic education may be beneficial for managing CRF, both during and after cancer treatment. However, there is a lack of evidence specific to hematologic malignancies. This paper describes the results of a feasibility study on Therapeutic Education and Physical Activity (TEPA) intervention to support self-management of CRF in patients with hematologic malignancies. This feasibility RCT involved a convenience sample of 40 newly diagnosed adult individuals, able to take part in a rehabilitation programme, and compared 2 parallel active interventions (Therapeutic Education versus Therapeutic Education and Physical Activity). The primary aim was to estimate the feasibility of TEPA (adherence rate to the intervention). Secondary aims were: to estimate the effect size of TEPA in terms of changes in CRF (FACIT-F), psychological distress (NCCN Distress Thermometer), QoL (EORTC QLQ-C30), physical performance (TUG, 6MWT) and habitual level of physical activity; to collect patient satisfaction, perception of usefulness and data on long-term adherence to an active lifestyle. Data were collected at the time of diagnosis and then at 1-, 3- and 7-month follow-up. Data analyses on feasibility and effect size of TEPA are ongoing. Trial registration: clinicaltrials.gov; Trial registration number: NCT03403075
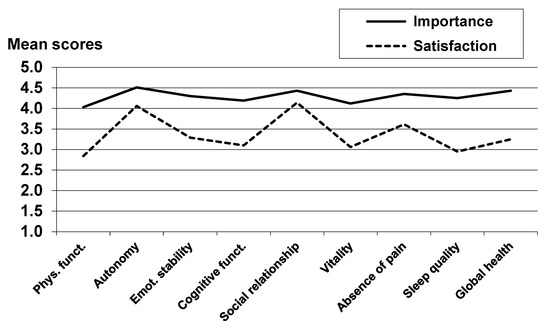
Title: Importance of and Satisfaction with Domains of Health-Related Quality of Life in Cancer Rehabilitation
Authors: Andreas Hinz (correspondence), Thomas Schulte, Jochen Ernst, Anja Mehnert-Theuerkauf
Affiliation: University Medicine Leipzig
Abstract: Instruments for measuring health-related quality of life (HRQoL) generally do not consider the subjective importance of the dimensions they comprise. The aims of this study were to analyze the subjectively perceived importance of dimension of HRQoL and to investigate their relationship to the satisfaction ratings with these dimensions. A total of 1108 participants enrolled in a cancer rehabilitation program were surveyed. Patients rated eight dimensions of HRQoL (physical functioning, autonomy, emotional stability, cognitive functioning, social relationships, vitality, absence of pain, and sleep quality) as well as global health in terms of how important those dimensions are to them and how satisfied they are with them. The dimensions with the highest importance ratings were autonomy and social relationships. There were only small sex differences in the importance ratings, but younger patients rated health as being more important than older patients did. The correlations between the importance ratings and the satisfaction ratings of the specific HRQoL dimensions ranged from -0.06 to 0.40, and the correlation for global health was 0.01. Importance ratings provide relevant information for health care professionals in addition to the HRQoL assessments in the context of cancer rehabilitation.
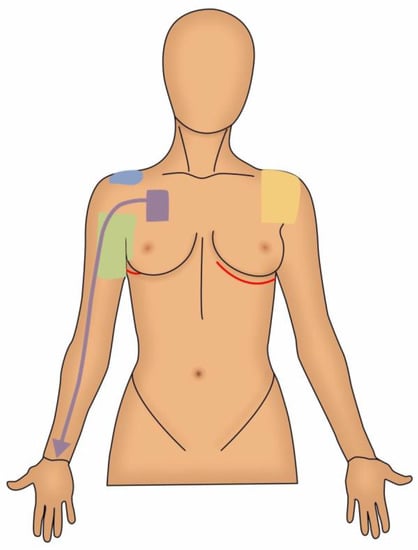
Title: Wellbeing and Complementary Therapies in Breast Cancer Peripheral Neuropathy Care: A Scoping Review Focused on Foot Health
Authors: Raquel Veiga-Seijo; Maria Eva Perez-Lopez; Uxia Fernandez-Lopez; Abian Mosquera-Fernandez; Cristina Gonzalez-Martin
Affiliation: Universidade da Coruña, Department of Health Sciences, Faculty of Nursing and Podiatry, Campus Esteiro, 15471 Ferrol, Spain Universidade da Coruña (UDC), Research Group in Nursing and Health Care, Instituto de Investigación Biomédica de A Coruña (INIBIC), Complexo Hospitalario Universitario de A Coruña (CHUAC), Sergas, 15071 A Coruña, Spain Universidade da Coruña (UDC), Research Group in Rheumatology and Health (GIR-S), Faculty of Physiotherapy, Campus Oza, 15008 A Coruña, Spain. Medical Oncology Department, Hospital Universitario de A Coruña Instituto de Investigación Biomédica de A Coruña (INIBIC), Sergas, 15006 A Coruña, Spain
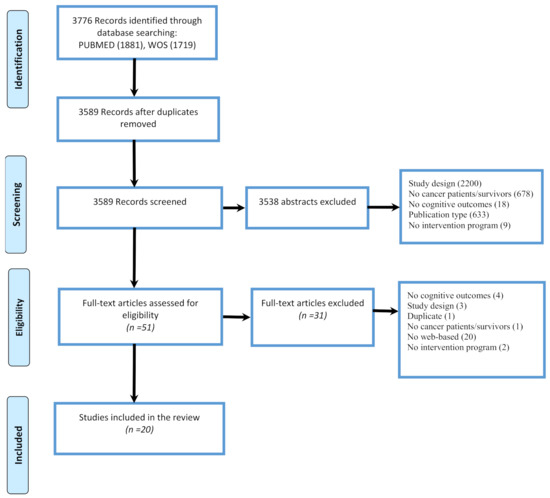
Abstract: Background. Chemotherapy-induced peripheral neuropathy is highly relevant in breast cancer because of the symptoms it triggers and the corresponding quality of life. Objectives. To map the literature on the impact of chemotherapy-induced peripheral neuropathy on the quality of life and foot health of people with breast cancer and to describe the main assessment strategies and complementary therapies. Methods. A scoping review was carried out following the PRISMA-ScR and Arksey and O'Malley guidelines. Different databases (Cochrane Plus, Scopus, Web of Science, and Pubmed) were used. 221 results were identified. 16 articles were included. Results. The thematic analysis obtained the following categories: impact of peripheral neuropathy on the development of comorbidities, foot health and its implications for the gait and quality of life, complementary therapies as a path of new strategies, and the need for clinicians and researchers to get involved in this side effect. Conclusions. Peripheral neuropathy impairs quality of life and adds comorbidity to health status. Implications for foot health and maintaining an active and healthy lifestyle have not been previously reported. Current clinical trials recommend exercise to prevent and alleviate symptoms.
Highlights: Complementary therapies are recommended by scientific evidence, but more research is needed to support their use. Advancing in this field from a comprehensive and holistic care perspective and raising awareness among healthcare professionals will make it possible to incorporate them as part of their evidence-based practice.