Emerging Topics in Vascular Endothelial Cell Biology
Share This Topical Collection
Editors
 Prof. Dr. Julia Schumann
Prof. Dr. Julia Schumann
 Prof. Dr. Julia Schumann
Prof. Dr. Julia Schumann
E-Mail
Website
Collection Editor
Clinic for Anesthesiology and Surgical Intensive Care, University Hospital Halle (Saale), 06120 Halle, Germany
Interests: endothelial dysfunction; macrophage–endothelial interaction; miRNAs; lipid rafts
Special Issues, Collections and Topics in MDPI journals
 Dr. Michael Cross
Dr. Michael Cross
 Dr. Michael Cross
Dr. Michael Cross
E-Mail
Website
Collection Editor
Department of Molecular and Clinical Pharmacology, MRC Centre for Drug Safety Science, Institute of Translational Medicine, University of Liverpool, Sherrington Building, Liverpool L69 3GE, UK
Interests: ERK5 signaling; endothelial cells; cardioprotection
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
Endothelial cells line the blood vessels and control the flow of substances and fluids into and out of tissues and are involved in numerous physiological as well as pathophysiological processes. In this Topical Collection, we will review recent findings on endothelial cell biology. New data on endothelial cell functions, such as coagulation and fibrinolysis, regulation of vascular tone, inflammation, blood vessel formation, and angiogenesis are welcome, as are insights into endothelial dysfunction and the role of endothelial cells in malignancies and coronary artery disease. Original papers, reviews, or perspective articles will be considered.
Prof. Dr. Julia Schumann
Dr. Michael Cross
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cells is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
The Article Processing Charge (APC) for publication in this open access journal is 2700 CHF (Swiss Francs).
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Keywords
- endothelial cells
- endothelial dysfunction
- cancer
- coronary artery disease
- inflammation
- angiogenesis
Published Papers (14 papers)
Open AccessArticle
Non-Psychoactive Phytocannabinoids Inhibit Inflammation-Related Changes of Human Coronary Artery Smooth Muscle and Endothelial Cells
by
Elisa Teichmann, Elane Blessing and Burkhard Hinz
Cited by 2 | Viewed by 1891
Abstract
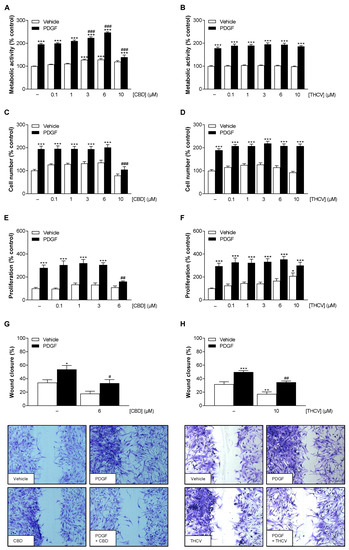
Atherosclerosis is associated with vascular smooth muscle cell proliferation, chronic vascular inflammation, and leukocyte adhesion. In view of the cardioprotective effects of cannabinoids described in recent years, the present study investigated the impact of the non-psychoactive phytocannabinoids cannabidiol (CBD) and tetrahydrocannabivarin (THCV) on
[...] Read more.
Atherosclerosis is associated with vascular smooth muscle cell proliferation, chronic vascular inflammation, and leukocyte adhesion. In view of the cardioprotective effects of cannabinoids described in recent years, the present study investigated the impact of the non-psychoactive phytocannabinoids cannabidiol (CBD) and tetrahydrocannabivarin (THCV) on proliferation and migration of human coronary artery smooth muscle cells (HCASMC) and on inflammatory markers in human coronary artery endothelial cells (HCAEC). In HCASMC, CBD and THCV at nontoxic concentrations exhibited inhibitory effects on platelet-derived growth factor-triggered proliferation (CBD) and migration (CBD, THCV). When interleukin (IL)-1β- and lipopolysaccharide (LPS)-stimulated HCAEC were examined, both cannabinoids showed a concentration-dependent decrease in the expression of vascular cell adhesion molecule-1 (VCAM-1), which was mediated independently of classical cannabinoid receptors and was not accompanied by a comparable inhibition of intercellular adhesion molecule-1. Further inhibitor experiments demonstrated that reactive oxygen species, p38 mitogen-activated protein kinase activation, histone deacetylase, and nuclear factor κB (NF-κB) underlie IL-1β- and LPS-induced expression of VCAM-1. In this context, CBD and THCV were shown to inhibit phosphorylation of NF-κB regulators in LPS- but not IL-1β-stimulated HCAEC. Stimulation of HCAEC with IL-1β and LPS was associated with increased adhesion of monocytes, which, however, could not be significantly abolished by CBD and THCV. In summary, the results highlight the potential of the non-psychoactive cannabinoids CBD and THCV to regulate inflammation-related changes in HCASMC and HCAEC. Considering their effect on both cell types studied, further preclinical studies could address the use of CBD and THCV in drug-eluting stents for coronary interventions.
Full article
►▼
Show Figures
Open AccessArticle
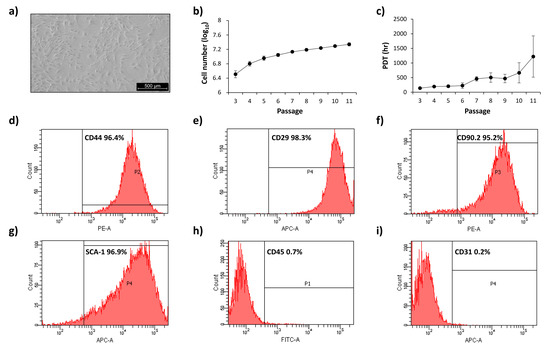
Methylglyoxal Impairs the Pro-Angiogenic Ability of Mouse Adipose-Derived Stem Cells (mADSCs) via a Senescence-Associated Mechanism
by
Alessia Leone, Antonella Nicolò, Immacolata Prevenzano, Federica Zatterale, Michele Longo, Antonella Desiderio, Rosa Spinelli, Michele Campitelli, Domenico Conza, Gregory Alexander Raciti, Francesco Beguinot, Cecilia Nigro and Claudia Miele
Cited by 2 | Viewed by 1684
Abstract
Adipose-derived stem cells (ADSCs) play a crucial role in angiogenesis and repair of damaged tissues. However, in pathological conditions including diabetes, ADSC function is compromised. This work aims at evaluating the effect of Methylglyoxal (MGO), a product of chronic hyperglycemia, on mouse ADSCs’
[...] Read more.
Adipose-derived stem cells (ADSCs) play a crucial role in angiogenesis and repair of damaged tissues. However, in pathological conditions including diabetes, ADSC function is compromised. This work aims at evaluating the effect of Methylglyoxal (MGO), a product of chronic hyperglycemia, on mouse ADSCs’ (mADSCs) pro-angiogenic function and the molecular mediators involved. The mADSCs were isolated from C57bl6 mice. MGO-adducts and p-p38 MAPK protein levels were evaluated by Western Blot. Human retinal endothelial cell (hREC) migration was analyzed by transwell assays. Gene expression was measured by qRT-PCR, and SA-βGal activity by cytofluorimetry. Soluble factor release was evaluated by multiplex assay. MGO treatment does not impair mADSC viability and induces MGO-adduct accumulation. hREC migration is reduced in response to both MGO-treated mADSCs and conditioned media from MGO-treated mADSCs, compared to untreated cells. This is associated with an increase of SA-βGal activity, SASP factor release and p53 and p21 expression, together with a VEGF- and PDGF-reduced release from MGO-treated mADSCs and a reduced p38-MAPK activation in hRECs. The MGO-induced impairment of mADSC function is reverted by senolytics. In conclusion, MGO impairs mADSCs’ pro-angiogenic function through the induction of a senescent phenotype, associated with the reduced secretion of growth factors crucial for hREC migration.
Full article
►▼
Show Figures
Open AccessReview
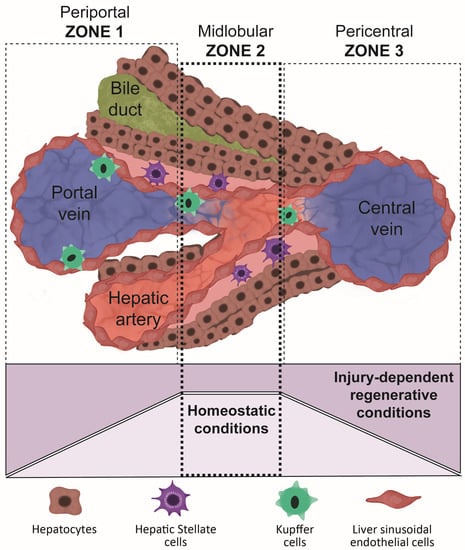
Multicellular Liver Organoids: Generation and Importance of Diverse Specialized Cellular Components
by
Giuseppe Ietto, Valentina Iori, Mattia Gritti, Davide Inversini, Angelita Costantino, Sofia Izunza Barba, Z. Gordon Jiang, Giulio Carcano, Daniela Dalla Gasperina and Giuseppe Pettinato
Viewed by 3049
Abstract
Over 40,000 patients in the United States are estimated to suffer from end-stage liver disease and acute hepatic failure, for which liver transplantation is the only available therapy. Human primary hepatocytes (HPH) have not been employed as a therapeutic tool due to the
[...] Read more.
Over 40,000 patients in the United States are estimated to suffer from end-stage liver disease and acute hepatic failure, for which liver transplantation is the only available therapy. Human primary hepatocytes (HPH) have not been employed as a therapeutic tool due to the difficulty in growing and expanding them in vitro, their sensitivity to cold temperatures, and tendency to dedifferentiate following two-dimensional culture. The differentiation of human-induced pluripotent stem cells (hiPSCs) into liver organoids (LO) has emerged as a potential alternative to orthotropic liver transplantation (OLT). However, several factors limit the efficiency of liver differentiation from hiPSCs, including a low proportion of differentiated cells capable of reaching a mature phenotype, the poor reproducibility of existing differentiation protocols, and insufficient long-term viability in vitro and in vivo. This review will analyze various methodologies being developed to improve hepatic differentiation from hiPSCs into liver organoids, paying particular attention to the use of endothelial cells as supportive cells for their further maturation. Here, we demonstrate why differentiated liver organoids can be used as a research tool for drug testing and disease modeling, or employed as a bridge for liver transplantation following liver failure.
Full article
►▼
Show Figures
Open AccessArticle
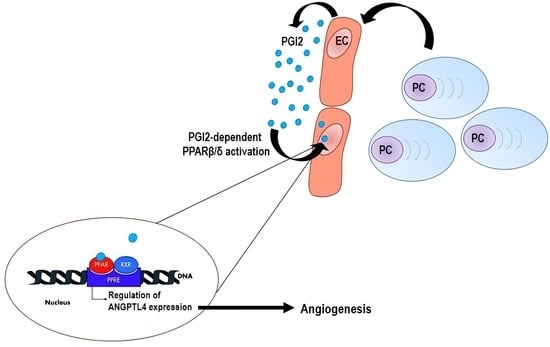
Unraveling the Role of Peroxisome Proliferator-Activated Receptor β/Δ (PPAR β/Δ) in Angiogenesis Associated with Multiple Myeloma
by
Patrizia Leone, Antonio Giovanni Solimando, Marcella Prete, Eleonora Malerba, Nicola Susca, Afshin Derakhshani, Paolo Ditonno, Carolina Terragna, Michele Cavo, Nicola Silvestris and Vito Racanelli
Cited by 2 | Viewed by 1883
Abstract
Growing evidence suggests a role for peroxisome proliferator-activated receptor β/δ (PPAR β/δ) in the angiogenesis, growth, and metastasis of solid tumors, but little is known about its role in multiple myeloma (MM). Angiogenesis in the bone marrow (BM) is characteristic of disease transition
[...] Read more.
Growing evidence suggests a role for peroxisome proliferator-activated receptor β/δ (PPAR β/δ) in the angiogenesis, growth, and metastasis of solid tumors, but little is known about its role in multiple myeloma (MM). Angiogenesis in the bone marrow (BM) is characteristic of disease transition from monoclonal gammopathy of undetermined significance (MGUS) to MM. We examined the expression and function of PPAR β/δ in endothelial cells (EC) from the BM of MGUS (MGEC) and MM (MMEC) patients and showed that PPAR β/δ was expressed at higher levels in MMEC than in MGEC and that the overexpression depended on myeloma plasma cells. The interaction between myeloma plasma cells and MMEC promoted the release of the PPAR β/δ ligand prostaglandin I2 (PGI2) by MMEC, leading to the activation of PPAR β/δ. We also demonstrated that PPAR β/δ was a strong stimulator of angiogenesis in vitro and that PPAR β/δ inhibition by a specific antagonist greatly impaired the angiogenic functions of MMEC. These findings define PGI2-PPAR β/δ signaling in EC as a potential target of anti-angiogenic therapy. They also sustain the use of PPAR β/δ inhibitors in association with conventional drugs as a new therapeutic approach in MM.
Full article
►▼
Show Figures
Open AccessArticle
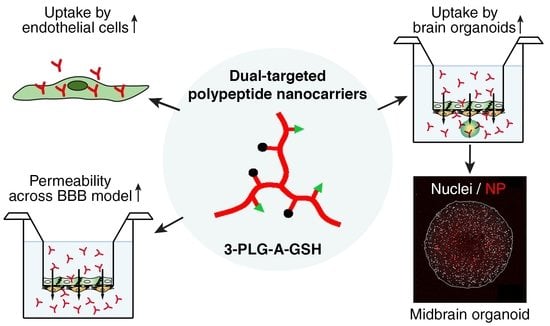
Targeting Human Endothelial Cells with Glutathione and Alanine Increases the Crossing of a Polypeptide Nanocarrier through a Blood–Brain Barrier Model and Entry to Human Brain Organoids
by
Mária Mészáros, Thi Ha My Phan, Judit P. Vigh, Gergő Porkoláb, Anna Kocsis, Emese K. Páli, Tamás F. Polgár, Fruzsina R. Walter, Silvia Bolognin, Jens C. Schwamborn, Jeng-Shiung Jan, Mária A. Deli and Szilvia Veszelka
Cited by 10 | Viewed by 3167
Abstract
Nanoparticles (NPs) are the focus of research efforts that aim to develop successful drug delivery systems for the brain. Polypeptide nanocarriers are versatile platforms and combine high functionality with good biocompatibility and biodegradability. The key to the efficient brain delivery of NPs is
[...] Read more.
Nanoparticles (NPs) are the focus of research efforts that aim to develop successful drug delivery systems for the brain. Polypeptide nanocarriers are versatile platforms and combine high functionality with good biocompatibility and biodegradability. The key to the efficient brain delivery of NPs is the specific targeting of cerebral endothelial cells that form the blood–brain barrier (BBB). We have previously discovered that the combination of two different ligands of BBB nutrient transporters, alanine and glutathione, increases the permeability of vesicular NPs across the BBB. Our aim here was to investigate whether the combination of these molecules can also promote the efficient transfer of 3-armed poly(
l-glutamic acid) NPs across a human endothelial cell and brain pericyte BBB co-culture model. Alanine and glutathione dual-targeted polypeptide NPs showed good cytocompatibility and elevated cellular uptake in a time-dependent and active manner. Targeted NPs had a higher permeability across the BBB model and could subsequently enter midbrain-like organoids derived from healthy and Parkinson’s disease patient-specific stem cells. These results indicate that poly(
l-glutamic acid) NPs can be used as nanocarriers for nervous system application and that the right combination of molecules that target cerebral endothelial cells, in this case alanine and glutathione, can facilitate drug delivery to the brain.
Full article
►▼
Show Figures
Open AccessArticle
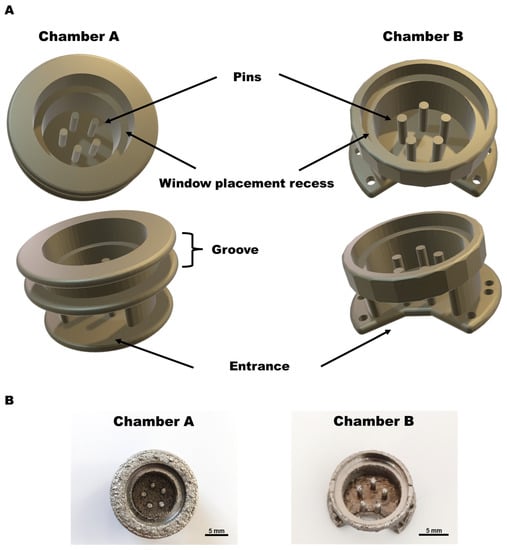
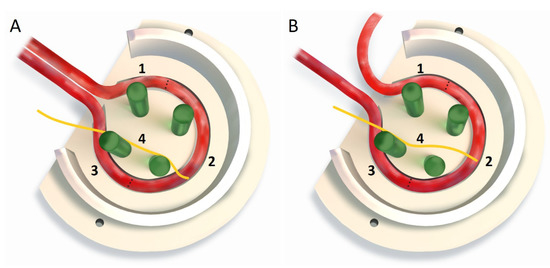
A Novel Window into Angiogenesis—Intravital Microscopy in the AV-Loop-Model
by
Ravikumar Vaghela, Andreas Arkudas, Daniel Gage, Carolin Körner, Stephan von Hörsten, Sahar Salehi, Raymund E. Horch and Maximilian Hessenauer
Cited by 2 | Viewed by 2088
Abstract
Due to the limitations of current in vivo experimental designs, our comprehensive knowledge of vascular development and its implications for the development of large-scale engineered tissue constructs is very limited. Therefore, the purpose of this study was to develop unique in vivo imaging
[...] Read more.
Due to the limitations of current in vivo experimental designs, our comprehensive knowledge of vascular development and its implications for the development of large-scale engineered tissue constructs is very limited. Therefore, the purpose of this study was to develop unique in vivo imaging chambers that allow the live visualization of cellular processes in the arteriovenous (AV) loop model in rats. We have developed two different types of chambers. Chamber A is installed in the skin using the purse sting fixing method, while chamber B is installed subcutaneously under the skin. Both chambers are filled with modified gelatin hydrogel as a matrix. Intravital microscopy (IVM) was performed after the injection of fluorescein isothiocyanate (FITC)-labeled dextran and rhodamine 6G dye. The AV loop was functional for two weeks in chamber A and allowed visualization of the leukocyte trafficking. In chamber B, microvascular development in the AV loop could be examined for 21 days. Quantification of the microvascular outgrowth was performed using Fiji-ImageJ. Overall, by combining these two IVM chambers, we can comprehensively understand vascular development in the AV loop tissue engineering model¯.
Full article
►▼
Show Figures
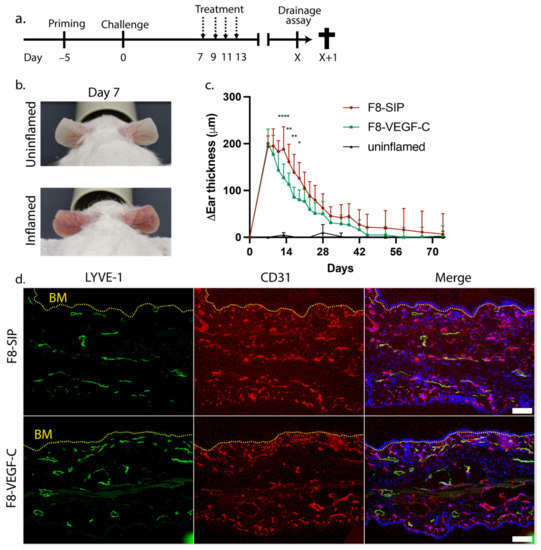
Open AccessArticle
Antibody-Mediated Delivery of VEGF-C Promotes Long-Lasting Lymphatic Expansion That Reduces Recurrent Inflammation
by
Nikola Cousin, Sophie Bartel, Jeannette Scholl, Carlotta Tacconi, Annina Egger, Gudrun Thorhallsdottir, Dario Neri, Lothar C. Dieterich and Michael Detmar
Cited by 5 | Viewed by 2228
Abstract
The lymphatic vascular system plays a fundamental role in inflammation by draining interstitial fluid, immune cells, antigens, and inflammatory mediators from peripheral tissues. Site-specific delivery of the lymphangiogenic growth factor VEGF-C alleviates acute inflammation in mouse models of psoriasis and chronic colitis by
[...] Read more.
The lymphatic vascular system plays a fundamental role in inflammation by draining interstitial fluid, immune cells, antigens, and inflammatory mediators from peripheral tissues. Site-specific delivery of the lymphangiogenic growth factor VEGF-C alleviates acute inflammation in mouse models of psoriasis and chronic colitis by enhancing local drainage. However, it is unclear whether therapeutically induced lymphangiogenesis is transient or long-lasting and whether it might prevent relapses of inflammation. Here, we investigated the long-term effects of targeted VEGF-C delivery in a chronic dermatitis model in mice. Congruent with our previous results, intravenous injection with a VEGF-C fusion protein targeted to the EDA domain of fibronectin initially resulted in reduced inflammation. Importantly, we found that targeted VEGF-C-mediated expansion of lymphatic vessels in the skin persisted for more than 170 days, long after primary inflammation had resolved. Furthermore, the treatment markedly decreased tissue swelling upon inflammatory re-challenge at the same site. Simultaneously, infiltration of leukocytes, including CD4+ T cells, macrophages, and dendritic cells, was significantly reduced in the previously treated group. In conclusion, our data show that targeted delivery of VEGF-C leads to long-lasting lymphatic expansion and long-term protection against repeated inflammatory challenge, suggesting that it is a promising new approach for the treatment of chronic, recurrent inflammatory diseases.
Full article
►▼
Show Figures
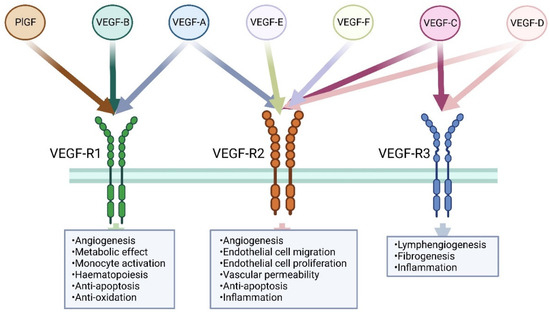
Open AccessReview
Therapeutic Potential of VEGF-B in Coronary Heart Disease and Heart Failure: Dream or Vision?
by
Rahul Mallick and Seppo Ylä-Herttuala
Cited by 6 | Viewed by 3203
Abstract
Coronary heart disease (CHD) is the leading cause of death around the world. Based on the roles of vascular endothelial growth factor (VEGF) family members to regulate blood and lymphatic vessels and metabolic functions, several therapeutic approaches have been attempted during the last
[...] Read more.
Coronary heart disease (CHD) is the leading cause of death around the world. Based on the roles of vascular endothelial growth factor (VEGF) family members to regulate blood and lymphatic vessels and metabolic functions, several therapeutic approaches have been attempted during the last decade. However proangiogenic therapies based on classical VEGF-A have been disappointing. Therefore, it has become important to focus on other VEGFs such as VEGF-B, which is a novel member of the VEGF family. Recent studies have shown the very promising potential of the VEGF-B to treat CHD and heart failure. The aim of this review article is to present the role of VEGF-B in endothelial biology and as a potential therapeutic agent for CHD and heart failure. In addition, key differences between the VEGF-A and VEGF-B effects on endothelial functions are demonstrated.
Full article
►▼
Show Figures
Open AccessArticle
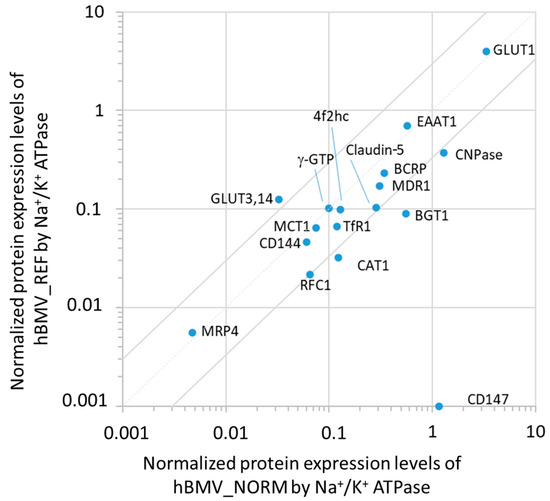
Quantitative Targeted Absolute Proteomics for Better Characterization of an In Vitro Human Blood–Brain Barrier Model Derived from Hematopoietic Stem Cells
by
Marie-Pierre Dehouck, Masanori Tachikawa, Yutaro Hoshi, Kotaro Omori, Claude-Alain Maurage, Guillaume Strecker, Lucie Dehouck, Marie-Christine Boucau, Yasuo Uchida, Fabien Gosselet, Tetsuya Terasaki and Yannis Karamanos
Cited by 10 | Viewed by 2363
Abstract
We previously developed an in vitro model of the human blood–brain barrier (BBB) based on the use of endothelial cells derived from CD34
+-hematopoietic stem cells and cultured with brain pericytes. The purpose of the present study was to provide information on
[...] Read more.
We previously developed an in vitro model of the human blood–brain barrier (BBB) based on the use of endothelial cells derived from CD34
+-hematopoietic stem cells and cultured with brain pericytes. The purpose of the present study was to provide information on the protein expression levels of the transporters, receptors, tight junction/adherence junction molecules, and transporter-associated molecules of human brain-like endothelial cells (hBLECs). The absolute protein expression levels were determined by liquid chromatography–mass spectrometry-based quantitative targeted absolute proteomics and compared with those from human brain microvessels (hBMVs). The protein levels of CD144, CD147, MRP4, Annexin A6 and caveolin-1 showed more than 3-fold abundance in hBLECs, those of MCT1, Connexin 43, TfR1, and claudin-5 showed less than 3-fold differences, and the protein levels of other drug efflux transporters and nutrient transporters were less represented in hBLECs than in hBMVs. It is noteworthy that BCRP was more expressed than MDR1 in hBLECs, as this was the case for hBMVs. These results suggest that transports mediated by MCT1, TfR1, and claudin-5-related tight junction function reflect the in vivo BBB situation. The present study provided a better characterization of hBLECs and clarified the equivalence of the transport characteristics between in vitro BBB models and in vivo BBB models using LC-MS/MS-based protein quantification.
Full article
►▼
Show Figures
Open AccessArticle
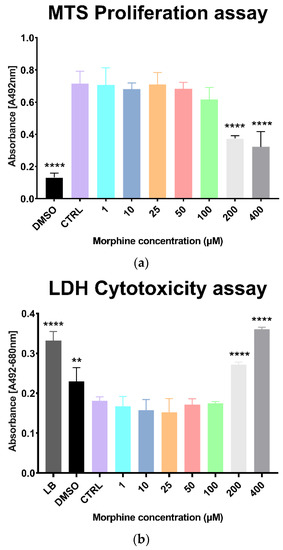
Oxidative Stress and Extracellular Matrix Remodeling Are Signature Pathways of Extracellular Vesicles Released upon Morphine Exposure on Human Brain Microvascular Endothelial Cells
by
Tatjana Vujić, Domitille Schvartz, Izadora Liranço Furlani, Isabel Meister, Víctor González-Ruiz, Serge Rudaz and Jean-Charles Sanchez
Cited by 13 | Viewed by 2666
Abstract
Morphine, a commonly used antinociceptive drug in hospitals, is known to cross the blood-brain barrier (BBB) by first passing through brain endothelial cells. Despite its pain-relieving effect, morphine also has detrimental effects, such as the potential induction of redox imbalance in the brain.
[...] Read more.
Morphine, a commonly used antinociceptive drug in hospitals, is known to cross the blood-brain barrier (BBB) by first passing through brain endothelial cells. Despite its pain-relieving effect, morphine also has detrimental effects, such as the potential induction of redox imbalance in the brain. However, there is still insufficient evidence of these effects on the brain, particularly on the brain endothelial cells and the extracellular vesicles that they naturally release. Indeed, extracellular vesicles (EVs) are nanosized bioparticles produced by almost all cell types and are currently thought to reflect the physiological state of their parent cells. These vesicles have emerged as a promising source of biomarkers by indicating the functional or dysfunctional state of their parent cells and, thus, allowing a better understanding of the biological processes involved in an adverse state. However, there is very little information on the morphine effect on human brain microvascular endothelial cells (HBMECs), and even less on their released EVs. Therefore, the current study aimed at unraveling the detrimental mechanisms of morphine exposure (at 1, 10, 25, 50 and 100 µM) for 24 h on human brain microvascular endothelial cells as well as on their associated EVs. Isolation of EVs was carried out using an affinity-based method. Several orthogonal techniques (NTA, western blotting and proteomics analysis) were used to validate the EVs enrichment, quality and concentration. Data-independent mass spectrometry (DIA-MS)-based proteomics was applied in order to analyze the proteome modulations induced by morphine on HBMECs and EVs. We were able to quantify almost 5500 proteins in HBMECs and 1500 proteins in EVs, of which 256 and 148, respectively, were found to be differentially expressed in at least one condition. Pathway enrichment analysis revealed that the “cell adhesion and extracellular matrix remodeling” process and the “HIF1 pathway”, a pathway related to oxidative stress responses, were significantly modulated upon morphine exposure in HBMECs and EVs. Altogether, the combination of proteomics and bioinformatics findings highlighted shared pathways between HBMECs exposed to morphine and their released EVs. These results put forward molecular signatures of morphine-induced toxicity in HBMECs that were also carried by EVs. Therefore, EVs could potentially be regarded as a useful tool to investigate brain endothelial cells dysfunction, and to a different extent, the BBB dysfunction in patient circulation using these “signature pathways”.
Full article
►▼
Show Figures
Open AccessArticle
Vascularization of Poly-ε-Caprolactone-Collagen I-Nanofibers with or without Sacrificial Fibers in the Neurotized Arteriovenous Loop Model
by
Simon Kratzer, Andreas Arkudas, Marcus Himmler, Dirk W. Schubert, Dominik Schneidereit, Julian Bauer, Oliver Friedrich, Raymund E. Horch and Aijia Cai
Cited by 5 | Viewed by 1822
Abstract
Electrospun nanofibers represent an ideal matrix for the purpose of skeletal muscle tissue engineering due to their highly aligned structure in the nanoscale, mimicking the extracellular matrix of skeletal muscle. However, they often consist of high-density packed fibers, which might impair vascularization. The
[...] Read more.
Electrospun nanofibers represent an ideal matrix for the purpose of skeletal muscle tissue engineering due to their highly aligned structure in the nanoscale, mimicking the extracellular matrix of skeletal muscle. However, they often consist of high-density packed fibers, which might impair vascularization. The integration of polyethylene oxide (PEO) sacrificial fibers, which dissolve in water, enables the creation of less dense structures. This study examines potential benefits of poly-ε-caprolactone-collagen I-PEO-nanoscaffolds (PCP) in terms of neovascularization and distribution of newly formed vessels compared to poly-ε-caprolactone -collagen I-nanoscaffolds (PC) in a modified arteriovenous loop model in the rat. For this purpose, the superficial inferior epigastric artery and vein as well as a motor nerve branch were integrated into a multilayer three-dimensional nanofiber scaffold construct, which was enclosed by an isolation chamber. Numbers and spatial distribution of sprouting vessels as well as macrophages were analyzed via immunohistochemistry after two and four weeks of implantation. After four weeks, aligned PC showed a higher number of newly formed vessels, regardless of the compartments formed in PCP by the removal of sacrificial fibers. Both groups showed cell influx and no difference in macrophage invasion. In this study, a model of combined axial vascularization and neurotization of a PCL-collagen I-nanofiber construct could be established for the first time. These results provide a foundation for the in vivo implantation of cells, taking a major step towards the generation of functional skeletal muscle tissue.
Full article
►▼
Show Figures
Open AccessArticle
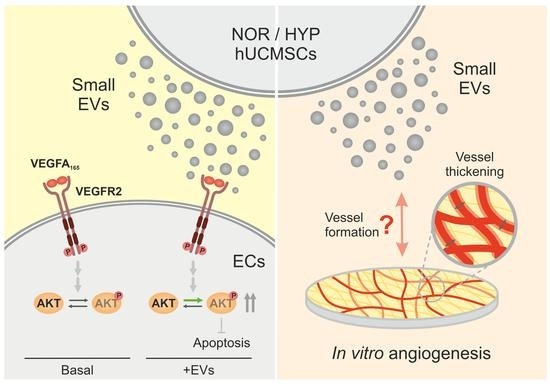
Extracellular Vesicles from Human Umbilical Cord-Derived MSCs Affect Vessel Formation In Vitro and Promote VEGFR2-Mediated Cell Survival
by
Ana Muñiz-García, Bettina Wilm, Patricia Murray and Michael J. Cross
Cited by 4 | Viewed by 2111
Abstract
Mesenchymal stromal cell (MSC)-derived extracellular vesicles (EVs) have emerged as novel tools in regenerative medicine. Angiogenesis modulation is widely studied for the treatment of ischaemic diseases, wound healing, and tissue regeneration. Here, we have shown that EVs from human umbilical cord-derived MSCs can
[...] Read more.
Mesenchymal stromal cell (MSC)-derived extracellular vesicles (EVs) have emerged as novel tools in regenerative medicine. Angiogenesis modulation is widely studied for the treatment of ischaemic diseases, wound healing, and tissue regeneration. Here, we have shown that EVs from human umbilical cord-derived MSCs can affect VEGFR2 signalling, a master regulator of angiogenesis homeostasis, via altering the phosphorylation of AKT. This translates into an inhibition of apoptosis, promoting exclusively cell survival, but not proliferation, in human microvascular endothelial cells. Interestingly, when comparing EVs from normoxic cells to those obtained from hypoxia (1% O
2) preconditioned cells, hypoxia-derived EVs appear to have a slightly enhanced effect. Furthermore, when studied in a longer term endothelial-fibroblast co-culture angiogenesis model in vitro, both EV populations demonstrated a positive effect on vessel formation, evidenced by increased vessel networks with tubes of significantly larger diameters. Our data reveals that EVs selectively target components of the angiogenic pathway, promoting VEGFR2-mediated cell survival via enhancement of AKT activation. Our data show that EVs are able to enhance specific components of the VEGF signalling pathway and may have therapeutic potential to support endothelial cell survival.
Full article
►▼
Show Figures
Open AccessArticle
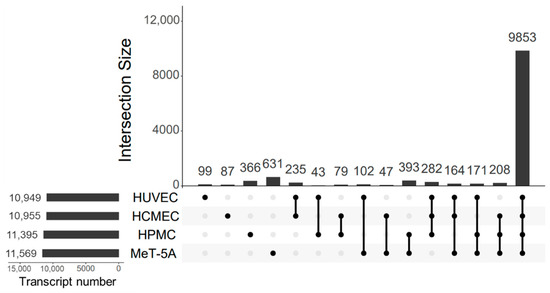
Understanding Cell Model Characteristics—RNA Expression Profiling in Primary and Immortalized Human Mesothelial Cells, and in Human Vein and Microvascular Endothelial Cells
by
Iva Marinovic, Maria Bartosova, Rebecca Herzog, Juan Manuel Sacnun, Conghui Zhang, Robin Hoogenboom, Markus Unterwurzacher, Thilo Hackert, Aurelio A. Teleman, Klaus Kratochwill and Claus Peter Schmitt
Cited by 3 | Viewed by 2541
Abstract
In vitro studies are essential in pre-clinical research. While choice of cell lines is often driven by handling and cost-effectiveness, in-depth knowledge on specific characteristics is scant. Mesothelial cells, which interact with endothelial cells, are widely used in research, including cancer and drug
[...] Read more.
In vitro studies are essential in pre-clinical research. While choice of cell lines is often driven by handling and cost-effectiveness, in-depth knowledge on specific characteristics is scant. Mesothelial cells, which interact with endothelial cells, are widely used in research, including cancer and drug development, but have not been comprehensively profiled. We therefore performed RNA sequencing of polarized, primary peritoneal (HPMC) and immortalized pleural mesothelial cells (MeT-5A), and compared them to endothelial cells from umbilical vein (HUVEC) and cardiac capillaries (HCMEC). Seventy-seven per cent of 12,760 genes were shared between the 4 cell lines, 1003 were mesothelial and 969 were endothelial cell specific. The transcripts reflected major differences between HPMC and MeT-5A in DNA-related processes, extracellular matrix, migration, proliferation, adhesion, transport, growth factor- and immune response, and between HUVEC and HCMEC in DNA replication, extracellular matrix and adhesion organization. Highly variable shared genes were related to six clusters, cell tissue origin and immortalization, but also cell migration capacity, cell adhesion, regulation of angiogenesis and response to hypoxia. Distinct, cell type specific biological processes were further described by cellular component-, molecular function- and Reactome pathway analyses. We provide crucial information on specific features of the most frequently used mesothelial and endothelial cell lines, essential for appropriate use.
Full article
►▼
Show Figures
Open AccessArticle
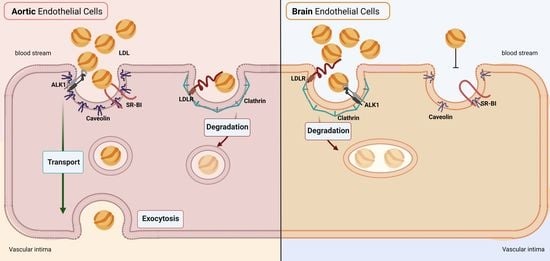
Brain Endothelial Cells in Contrary to the Aortic Do Not Transport but Degrade Low-Density Lipoproteins via Both LDLR and ALK1
by
Sofia Kakava, Eveline Schlumpf, Grigorios Panteloglou, Flavia Tellenbach, Arnold von Eckardstein and Jerome Robert
Cited by 5 | Viewed by 3049
Abstract
The transport of low-density lipoprotein (LDL) through the endothelium is a key step in the development of atherosclerosis, but it is notorious that phenotypic differences exist between endothelial cells originating from different vascular beds. Endothelial cells forming the blood–brain barrier restrict paracellular and
[...] Read more.
The transport of low-density lipoprotein (LDL) through the endothelium is a key step in the development of atherosclerosis, but it is notorious that phenotypic differences exist between endothelial cells originating from different vascular beds. Endothelial cells forming the blood–brain barrier restrict paracellular and transcellular passage of plasma proteins. Here, we systematically compared brain versus aortic endothelial cells towards their interaction with LDL and the role of proteins known to regulate the uptake of LDL by endothelial cells. Both brain endothelial cells and aortic endothelial cells bind and internalize LDL. However, whereas aortic endothelial cells degrade very small amounts of LDL and transcytose the majority, brain endothelial cells degrade but do not transport LDL. Using RNA interference (siRNA), we found that the LDLR–clathrin pathway leads to LDL degradation in either endothelial cell type. Both loss- and gain-of-function experiments showed that ALK1, which promotes transcellular LDL transport in aortic endothelial cells, also limits LDL degradation in brain endothelial cells. SR-BI and caveolin-1, which promote LDL uptake and transport into aortic endothelial cells, limit neither binding nor association of LDL to brain endothelial cells. Together, these results indicate distinct LDL trafficking by brain microvascular endothelial cells and aortic endothelial cells.
Full article
►▼
Show Figures
Planned Papers
The below list represents only planned manuscripts. Some of these
manuscripts have not been received by the Editorial Office yet. Papers
submitted to MDPI journals are subject to peer-review.
Title: Dodonaea viscosa medicinal plant polyphenols including epicatechin down-regulate pro-inflammatory pathways, oxidative stress and permeability damage specifically caused by LPS from Escherichia coli or Porphyromonas gingivalis in cerebral endothelial cells.
Authors: Janice Taïlé; Teva Turpin; Katy Thouvenot; Bryan Veeren; Olivier Meilhac; Marie-Paule Gonthier
Affiliation: /
Abstract: /
Title: Targeting human endothelial cells with glutathione and alanine increases the crossing of a polypeptide nanocarrier through a blood-brain barrier model and entry to human brain organoids
Authors: Maria Deli
Affiliation: /
Abstract: /