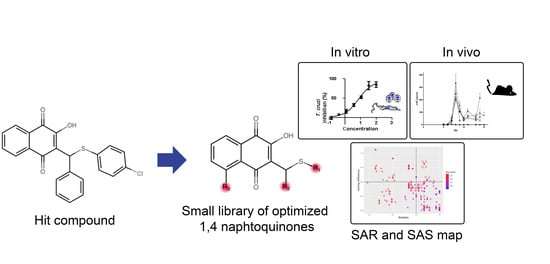
Optimization of 1,4-Naphthoquinone Hit Compound: A Computational, Phenotypic, and In Vivo Screening against Trypanosoma cruzi
Abstract
:1. Introduction
2. Results
2.1. Hit Compound Optimization
2.2. In Vitro Biological Evaluation
2.3. Computational Analysis: Physicochemical Properties, SAR, and SAS Maps
2.4. Trypanocidal Activity in Mouse Model of Acute Infection
3. Discussion
4. Materials and Methods
4.1. Synthetic Compounds
4.2. General Procedure for Preparing 1a–i and 2a–j
4.2.1. 2-((4-chlorophenyl)((4-chlorophenyl)thio)methyl)-3-hydroxynaphthalene-1,4-dione (1a)
4.2.2. 2-((3-chlorophenyl)((4-chlorophenyl)thio)methyl)-3-hydroxynaphthalene-1,4-dione (1b)
4.2.3. 2-((2-chlorophenyl)((4-chlorophenyl)thio)methyl)-3-hydroxynaphthalene-1,4-dione (1c)
4.2.4. 2-(((2,4-dichlorophenyl)thio)(phenyl)methyl)-3-hydroxynaphthalene-1,4-dione (1d)
4.2.5. 2-(((4-chlorophenyl)thio)(1-(3,5-dichlorophenyl)-1H-1,2,3-triazol-4-yl)methyl)-3-hydroxynaphthalene-1,4-dione (1e)
4.2.6. 3-(((4-chlorophenyl)thio)(phenyl)methyl)-2,5-dihydroxynaphthalene-1,4-dione (1f)
4.2.7. 2-(((4-chlorophenyl)thio)(4-methoxyphenyl)methyl)-3-hydroxynaphthalene-1,4-dione (1g)
2.4.8. 2-(((4-chlorophenyl)thio)(2,4-dimethoxyphenyl)methyl)-3-hydroxynaphthalene-1,4-dione (1h)
4.2.9. 2-(((4-chlorophenyl)thio)(2,3,4-trimethoxyphenyl)methyl)-3-hydroxynaphthalene-1,4-dione (1i)
4.2.10. 2-Hydroxy-3-((4-methoxyphenyl)(phenylthio)methyl)naphthalene-1,4-dione (2a)
4.2.11. 2-Hydroxy-3-((4-methoxyphenyl)(o-tolylthio)methyl) naphthalene-1,4-dione (2b)
4.2.12. 2-Hydroxy-3-((4-methoxyphenyl)(m-tolylthio)methyl)naphthalene-1,4-dione (2c)
4.2.13. 2-Hydroxy-3-((4-methoxyphenyl)(p-tolylthio)methyl) naphthalene-1,4-dione (2d)
4.2.14. 2-(((4-fluorophenyl)thio)(4-methoxyphenyl)methyl)-3-hydroxynaphthalene-1,4-dione (2e)
4.2.15. 2-Hydroxy-3-((4-methoxyphenyl)((4-nitrophenyl)thio)methyl)naphthalene-1,4-dione (2f)
4.2.16. 2-Hydroxy-3-((4-methoxyphenyl)(propylthio)methyl)naphthalene-1,4-dione (2g)
4.2.17. 2-Hydroxy-3-((4-methoxyphenyl)(naphthalen-2-ylthio)methyl) naphthalene-1,4-dione (2h)
4.2.18. 2-Hydroxy-3-((4-methoxyphenyl)((4-methoxyphenyl)thio)methyl)naphthalene-1,4-dione (2i)
4.2.19. 2-hydroxy-3-((4-methoxyphenyl)((4-(methylthio)phenyl)thio)methyl)naphthalene-1,4-dione (2j)
4.3. Cell Culture
4.4. Parasites
4.5. Cytotoxicity In Vitro Assay
4.6. Trypanocidal Activity
4.7. In Silico Analysis
4.8. Mouse Acute Toxicity
4.9. In Vivo Experimental T. cruzi Infection
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Sample Availability
References
- World Health Organization. Targets and Milestones for Overcoming Neglected Tropical Diseases 2011–2020. Available online: https://www.who.int/chagas/strategy/en/ (accessed on 7 October 2020).
- Drug for Neglected Disease Initiative (DNDi), Paediatric Benznidazole. Available online: https://www.dndi.org/achievements/paediatric-benznidazole/ (accessed on 7 October 2020).
- Food and Drug Administration. FDA Approves First U.S. Treatment for Chagas Disease. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-first-us-treatment-chagas-disease (accessed on 7 October 2020).
- Hernández, C.; Salazar, C.; Brochero, H.; Teherán, A.; Buitrago, L.S.; Vera, M.; Soto, H.; Florez-Rivadeneira, Z.; Ardila, S.; Parra-Henao, G.; et al. Untangling the transmission dynamics of primary and secondary vectors of Trypanosoma cruzi in Colombia: Parasite infection, feeding sources and discrete typing units. Parasit. Vectors 2016, 9, 620–632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noya, B.A.; Pérez-Chacón, G.; Díaz-Bello, Z.; Dickson, S.; Muñoz-Calderón, A.; Hernández, C.; Pérez, Y.; Mauriello, L.; Moronta, E. Description of an oral Chagas disease outbreak in Venezuela, including a vertically transmitted case. Mem. Inst. Oswaldo Cruz. 2017, 112, 569–571. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, J.D.; Montilla, M.; Cucunubá, Z.M.; Floréz, A.C.; Zambrano, P.; Guhl, F. Molecular epidemiology of human oral Chagas disease outbreaks in Colombia. PLoS Negl. Trop. Dis. 2013, 7, e2041. [Google Scholar] [CrossRef] [PubMed]
- Carod-Artal, F.J. Policy Implications of the Changing Epidemiology of Chagas Disease and Stroke. Stroke 2013, 44, 2356–2360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coronel, M.V.; Frutos, L.O.; Muñoz, E.C.; Valle, D.K.; Rojas, D.H. Adverse systemic reaction to benznidazole. Rev. Soc. Bras. Med. Trop. 2017, 50, 145–147. [Google Scholar] [CrossRef] [Green Version]
- Zingales, B.; Miles, M.A.; Moraes, C.B.; Luquetti, A.; Guhl, F.; Schijman, A.G.; Ribeiro, I. Drug discovery for Chagas disease should consider Trypanosoma cruzi strain diversity. Mem. Inst. Oswaldo Cruz. 2014, 109, 828–833. [Google Scholar] [CrossRef]
- Revollo, S.; Oury, B.; Vela, A.; Tibayrenc, M.; Sereno, D. In Vitro Benznidazole and Nifurtimox Susceptibility Profile of Trypanosoma cruzi Strains Belonging to Discrete Typing Units TcI, TcII, and TcV. Pathogens 2019, 8, 197. [Google Scholar] [CrossRef] [Green Version]
- Sánchez-Valdéz, F.J.; Padilla, A.; Wang, W.; Orr, D.; Tarleton, R.L. Spontaneous dormancy protects Trypanosoma cruzi during extended drug exposure. Elife 2018, 7, e34039. [Google Scholar] [CrossRef]
- Sales Junior, P.A.; Molina, I.; Fonseca Murta, S.M.; Sánchez-Montalvá, A.; Salvador, F.; Corrêa-Oliveira, R.; Carneiro, C.M. Experimental and Clinical Treatment of Chagas Disease: A Review. Am. J. Trop. Med. Hyg. 2017, 97, 1289–1303. [Google Scholar] [CrossRef]
- Morillo, C.A.; Marin-Neto, J.A.; Avezum, A.; Sosa-Estani, S.; Rassi Jr, A.; Rosas, F.; Villena, E.; Quiroz, R.; Bonilla, R.; Britto, C.; et al. BENEFIT Investigators. Randomized Trial of Benznidazole for Chronic Chagas’ Cardiomyopathy. N. Engl. J. Med. 2015, 373, 1295–1306. [Google Scholar] [CrossRef] [Green Version]
- Molina, I.; Gómez, I.; Prat, J.; Salvador, F.; Treviño, B.; Sulleiro, E.; Serre, N.; Pou, D.; Roure, S.; Cabezos, J.; et al. Randomized trial of posaconazole and benznidazole for chronic Chagas’ disease. N. Engl. J. Med. 2014, 370, 1899–1908. [Google Scholar] [CrossRef] [PubMed]
- Morillo, C.A.; Waskin, H.; Sosa-Estani, S.; Del Carmen Bangher, M.; Cuneo, C.; Milesi, R.; Mallagray, M.; Apt, W.; Beloscar, J.; Gascon, J.; et al. STOP-CHAGAS Investigators. Benznidazole and Posaconazole in Eliminating Parasites in Asymptomatic, T. cruzi Carriers: The STOP-CHAGAS Trial. J. Am. Coll. Cardiol. 2019, 69, 939–947. [Google Scholar] [CrossRef] [PubMed]
- Drug for Neglected Disease Initiative (DNDi). Fexinidazole (Chagas). Available online: https://www.dndi.org/diseases-projects/portfolio/fexinidazole-chagas/ (accessed on 7 October 2020).
- Drugs for Neglected Diseases Initiative. The Bendita Study: A Phase Ii Study to Assess Safety, Tolerability, and Efficacy of Different Benznidazole Regimens, Alone and in Combination with Fosravuconazole. Available online: https://dndi.org/wp-content/uploads/2019/03/2page_BenditatStudyOverview_ENG.pdf (accessed on 7 October 2020).
- Cerecetto, H.; González, M. Synthetic Medicinal Chemistry in Chagas’ Disease: Compounds at The Final Stage of “Hit-To-Lead” Phase. Pharmaceuticals 2010, 3, 810–838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fonseca-Berzal, C.; Arán, V.J.; Escario, J.A.; Gómez-Barrio, A. Experimental models in Chagas disease: A review of the methodologies applied for screening compounds against Trypanosoma cruzi. Parasitol. Res. 2018, 117, 3367–3380. [Google Scholar] [CrossRef]
- Meanwell, N.A. Improving drug candidates by design: A focus on physicochemical properties as a means of improving compound disposition and safety. Chem. Res. Toxicol. 2011, 24, 1420–1456. [Google Scholar] [CrossRef]
- Egan, W.J. Predicting ADME properties in drug discovery. In Drug Design: Structure and Ligand-Based Approaches; Merz, K.M., Reynolds, C.H., Eds.; Cambridge University Press: Cambridge, UK, 2010; pp. 165–178. [Google Scholar]
- Guha, R. On exploring structure-activity relationship. Methods Mol. Biol. 2013, 993, 81–94. [Google Scholar]
- Prati, F.; Bolognesi, M.L. Phenotypic Hits in Anti-Trypanosoma Drug Discovery. Chimica Ricerca. 2014. Available online: https://www.soc.chim.it/sites/default/files/chimind/pdf/2014_5_46_ca.pdf (accessed on 7 October 2020).
- Prati, F.; Bergamini, C.; Molina, M.T.; Falchi, F.; Cavalli, A.; Kaiser, M.; Brun, R.; Fato, R.; Bolognesi, M.L. 2-Phenoxy-1,4-naphthoquinones: From a Multitarget Antitrypanosomal to a Potential Antitumor Profile. J. Med. Chem. 2015, 58, 6422–6434. [Google Scholar] [CrossRef] [Green Version]
- Bruno, S.; Uliassi, E.; Zaffagnini, M.; Prati, F.; Bergamini, C.; Amorati, R.; Paredi, G.; Margiotta, M.; Conti, P.; Costi, M.P.; et al. Molecular basis for covalent inhibition of glyceraldehyde-3-phosphate dehydrogenase by a 2-phenoxy-1,4-naphthoquinone small molecule. Chem. Biol. Drug. Des. 2017, 90, 225–235. [Google Scholar] [CrossRef]
- Ogindo, C.O.; Khraiwesh, M.H.; George, M., Jr.; Brandy, Y.; Brandy, N.; Gugssa, A.; Ashraf, M.; Abbas, M.; Southerland, W.M.; Lee, C.M.; et al. Novel drug design for Chagas disease via targeting Trypanosoma cruzi tubulin: Homology modeling and binding pocket prediction on Trypanosoma cruzi tubulin polymerization inhibition by naphthoquinone derivatives. Bioorg. Med. Chem. 2016, 24, 3849–3855. [Google Scholar] [CrossRef] [Green Version]
- Silva Júnior, E.M.; Jardim, G.A.M.; Menna-Barreto, R.F.S.; de Castro, S.L. Anti-Trypanosoma cruzi compounds: Our contribution for the evaluation and insights on the mode of action of naphthoquinones and derivatives. J. Braz. Chem. Soc. 2014, 25, 1780–1798. [Google Scholar]
- Majiene, D.; Kuseliauskyte, J.; Stimbirys, A.; Jekabsone, A. Comparison of the Effect of Native 1,4-Naphthoquinones Plumbagin, Menadione, and Lawsone on Viability, Redox Status, and Mitochondrial Functions of C6 Glioblastoma. Cells Nutr. 2019, 11, 1294–1306. [Google Scholar] [CrossRef] [Green Version]
- Lara, L.S.; Moreira, C.S.; Calvet, C.M.; Lechuga, G.C.; Souza, R.S.; Bourguignon, S.C.; Ferreira, V.F.; Rocha Pereira, M.C.S. Efficacy of 2-hydroxy-3-phenylsulfanylmethyl-[1,4]-naphthoquinone derivatives against different Trypanosoma cruzi discrete type units: Identification of a promising hit compound. Eur. J. Med. Chem. 2018, 144, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Menna-Barreto, R.F.; Corrêa, J.R.; Pinto, A.V.; Soares, M.J.; de Castro, S.L. Mitochondrial disruption and DNA fragmentation in Trypanosoma cruzi induced by naphthoimidazoles synthesized from beta-lapachone. Parasitol. Res. 2007, 101, 895–905. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, E.M.; de Souza, M.C.B.V.; Fernandes, M.C.; Menna-Barreto, R.F.S.; Pinto, M.D.F.R.; Lopes, F.D.; de Simone, C.A.; Andrade, C.K.Z.; Pinto, A.V.; Ferreira, V.F.; et al. Synthesis and anti-Trypanosoma cruzi activity of derivatives from nor-lapachones and lapachones. Bioorg. Med. Chem. 2008, 16, 5030–5038. [Google Scholar] [CrossRef] [PubMed]
- Gruhlke, M.C.; Slusarenko, A.J. The biology of reactive sulfur species (RSS). Plant. Physiol. Biochem. 2012, 59, 98–107. [Google Scholar] [CrossRef]
- Novais, J.S.; Moreira, C.S.; Silva, A.C.J.A.; Loureiro, R.S.; Sá Figueiredo, A.M.; Ferreira, V.F.; Castro, H.C.; da Rocha, D.R. Antibacterial naphthoquinone derivatives targeting resistant strain Gram-negative bacteria in biofilms. Microb. Pathog. 2018, 118, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Da Rocha, D.R.; de Souza, A.C.; Resende, J.A.; Santos, W.C.; dos Santos, E.A.; Pessoa, C.; de Moraes, M.O.; Costa-Lotufo, L.V.; Montenegro, R.C.; Ferreira, V.F. Synthesis of new 9-hydroxy-α- and 7-hydroxy-β-pyran naphthoquinones and cytotoxicity against cancer cell lines. Org. Biomol. Chem. 2011, 9, 4315–4322. [Google Scholar] [CrossRef]
- Takebe, T.; Imai, R.; Ono, S. The Current Status of Drug Discovery and Development as Originated in United States Academia: The Influence of Industrial and Academic Collaboration on Drug Discovery and Development. Clin. Transl. Sci. 2018, 11, 597–606. [Google Scholar] [CrossRef]
- Khurana, G.; Rohilla, A.; Deep, A. Drug Development Process and Novel Drugs Approved by FDA for 2017–18, Applied Clinical Research. Clin. Trials Regul. Aff. 2018, 5, 80–98. [Google Scholar] [CrossRef] [Green Version]
- Jain, N.; Hwang, T.; Franklin, J.M.; Kesselheim, A.S. Association of the Priority Review Voucher with Neglected Tropical Disease Drug and Vaccine Development. JAMA 2017, 318, 388–389. [Google Scholar] [CrossRef]
- Brandão, G.C.; Missias, F.C.; Arantes, L.M.; Soares, L.F.; Roy, K.K.; Doerksen, R.J.; Oliveira, A.B.; Pereira, G.R. Antimalarial naphthoquinones. Synthesis via click chemistry, in vitro activity, docking to PfDHODH and SAR of lapacho-based compounds. Eur. J. Med. Chem. 2018, 145, 191–205. [Google Scholar]
- Da Silva, E.N., Jr.; Jardim, C.; Dhawa, U.; Ackermann, L.; de Castro, S.L. Synthesis of quinones with highlighted biological applications: A critical update on the strategies towards bioactive compounds with emphasis on lapachones. Eur. J. Med. Chem. 2019, 179, 863–915. [Google Scholar] [CrossRef]
- De Castro, S.L.; Batista, D.G.; Batista, M.M.; Batista, W.; Daliry, A.; de Souza, E.M.; Menna-Barreto, R.F.; Oliveira, G.M.; Salomão, K.; Silva, C.F.; et al. Experimental Chemotherapy for Chagas Disease: A Morphological, Biochemical, and Proteomic Overview of Potential Trypanosoma cruzi Targets of Amidines Derivatives and Naphthoquinones. Mol. Biol. Int. 2011, 2011, 306928. [Google Scholar] [CrossRef] [Green Version]
- Gao, Y.; Gesenberg, C.; Zheng, W. Oral Formulations for Preclinical Studies: Principle, Design, and Development Considerations. In Developing Solid Oral Dosage Forms: Pharmaceutical Theory and Practice, 2nd ed.; Qiu, Y., Chen, Y., Zhang, G., Yu, L., Mantri, V.R., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 455–495. [Google Scholar]
- Diogo, E.B.; Dias, G.G.; Rodrigues, B.L.; Guimarães, T.T.; Valença, W.O.; Camara, C.A.; de Oliveira, R.N.; da Silva, M.G.; Ferreira, V.F.; de Paiva, Y.G.; et al. Synthesis and anti-Trypanosoma cruzi activity of naphthoquinone-containing triazoles: Electrochemical studies on the effects of the quinoidal moiety. Bioorg. Med. Chem. 2013, 21, 6337–6348. [Google Scholar] [CrossRef] [Green Version]
- Ramos, E.I.; Garza, K.M.; Krauth-Siegel, R.L.; Bader, J.; Martinez, L.E.; Maldonado, R.A. 2,3-diphenyl-1,4-naphthoquinone: A potential chemotherapeutic agent against Trypanosoma cruzi. J. Parasitol. 2009, 95, 461–466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, A.; Santos, I.; Gaur, P.; Ferreira, V.; Garcia, C.; Rocha, D. Addition of thiols to o-quinone methide: New 2-hydroxy-3-phenylsulfanylmethyl [1,4]-naphthoquinones and their activity against the human malaria parasite Plasmodium falciparum (3D7). Eur. J. Med. Chem. 2013, 59, 48–53. [Google Scholar] [CrossRef]
- Sander, T.; Freyss, J.; von Korff, M.; Rufener, C. DataWarrior: An open-source program for chemistry aware data visualization and analysis. J. Chem. Inf. Model. 2015, 55, 460–473. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development (OECD) Guidelines for the Testing of Chemicals. Available online: https://www.oecd-ilibrary.org/environment/test-no-420-acute-oral-toxicity-fixed-dose-procedure_9789264070943-en (accessed on 7 October 2020).
- Brener, Z. Therapeutic activity and criterion of cure on mice experimentally infected with Trypanosoma cruzi. Rev. Inst. Med. Trop. 1962, 4, 389–396. [Google Scholar]




| Compounds | Trypanocidal Effect IC50Trypomastigotes (Mean ± SD μM) | Vero Cells Toxicity CC50 (Mean ± SD μM) | SI * Trypomastigotes | ||||
|---|---|---|---|---|---|---|---|
| Dm28c-Luc | Y Strain | Dm28c-Luc | Y | ||||
| IC50 | IC90 | IC50 | IC90 | ||||
| 1a | 8.9 ± 0.6 | 25.1 ± 1.6 | 3.1 ± 0.6 | 5.8 ± 0.9 | 43.6 ± 2.3 | 4.8 | 15.0 |
| 1b | 9.8 ± 0.5 | 30.8 ± 2.9 | 3.6 ± 1.6 | 8.1 ± 1.3 | 42.1 ± 1.9 | 4.2 | 11.7 |
| 1c | 8.6 ± 1.4 | 29.6 ± 5.4 | 4.3 ± 3.2 | 7.3 ± 2.2 | 44.1 ± 2.3 | 5.1 | 10.2 |
| 1d | 9.3 ± 1.1 | 23.3 ± 2.1 | 2.8 ± 0.6 | 5.8 ± 1.1 | 82.1 ± 5.1 | 8.9 | 29.3 |
| 1e | 4.5 ± 0.8 | 16.5 ± 2.8 | 4.7 ± 1.9 | 5.5 ± 0.9 | 34.1 ± 2.9 | 7.5 | 7.2 |
| 1f | 9.8 ± 0.7 | 28.1 ± 1.7 | 22.3 ± 0.3 | 10.9 ± 2.1 | 41.1 ± 2.1 | 4.2 | 1.8 |
| 1g | 8.1 ± 0.6 | 19.3 ± 3.4 | 10.2 ± 0.5 | 16.8 ± 2.5 | 99.9 ± 12.5 | 12.3 | 9.8 |
| 1h | 15.4 ± 4.6 | 15.4 ± 4.6 | 22.9 ± 7.1 | 31.9 ± 6.1 | 24.4 ± 2.6 | 1.5 | 1.1 |
| 1i | 21.5 ± 2.9 | 21.5 ± 2.9 | 30.1 ± 2.3 | 38.9 ± 4.3 | 34.2 ± 3.4 | 1.6 | 1.1 |
| 2a | 27.4 ± 2.9 | 32.1 ± 1.6 | 31.2 ± 4.3 | 38.9 ± 5.3 | 45.1 ± 1.9 | 1.6 | 1.4 |
| 2b | 25.9 ± 2.2 | 31.8 ± 0.9 | 27.9 ± 4.1 | 37.9 ± 6.1 | 44.4 ± 3.4 | 1.7 | 1.5 |
| 2c | 52.3 ± 6.4 | 84.6 ± 11.4 | 26.2 ± 4.8 | 32.8 ± 5.1 | 48.9 ± 4.7 | 0.9 | 1.8 |
| 2d | 24.3 ± 3.4 | 82.2 ± 7.7 | 31.1 ± 1.8 | 49.7 ± 7.1 | 141.8 ± 17.6 | 5.4 | 4.5 |
| 2e | 24.4 ± 4.4 | 31.4 ± 4.4 | 20.3 ± 4.1 | 32.3 ± 5.1 | 47.7 ± 3.2 | 1.9 | 2.3 |
| 2f | 6.5 ± 3.1 | 11.5 ± 3.1 | 12.5 ± 1.6 | 19.9 ± 3.6 | 40.6 ± 2.9 | 6.2 | 3.2 |
| 2g | 13.7 ± 4.1 | 28.7 ± 5.1 | 12.7 ± 3.9 | 23.7 ± 4.1 | 47.7 ± 5.2 | 3.5 | 3.7 |
| 2h | 21.7 ± 4.7 | 39.7 ± 5.7 | 24.5 ± 3.6 | 34.5 ± 4.6 | 63.4 ± 7.1 | 2.9 | 2.5 |
| 2i | 24.1 ± 2.7 | 44.9 ± 6.7 | 10.6 ± 0.4 | 31.6 ± 5.4 | 44.8 ± 3.3 | 1.8 | 4.2 |
| 2j | 52.7 ± 12.6 | >100 | 89.6 ± 5.4 | >100 | 93.5 ± 6.6 | 1.7 | 1.1 |
| C2# | 21.3 ± 1.9 | 31.6 ± 0.4 | 10.1 ± 1.0 | 27.8 ± 4.6 | 178.9 ± 6.2 | 8.4 | 17.6 |
| Bz | 17.5 ± 3.3 | >100 | 14.3 ± 3.2 | >100 | >500 | >28.6 | >34.9 |
 | |||||||
| Compounds | R1 | R2 | R3 | IC50 Ama (µM) | IC90 Ama (µM) | CC50 Vero (µM) | SI |
| 1a |  |  | - | 6.2 ± 0.9 | 12.1 ± 1.3 | 43.6 ± 2.3 | 7.0 |
| 1b |  |  | - | 6.9 ± 1.5 | 12.7 ± 1.8 | 42.1 ± 1.9 | 6.1 |
| 1c |  |  | - | 9.3 ± 0.8 | 23.1 ± 3.3 | 44.1 ± 2.3 | 4.7 |
| 1d |  |  | - | 13.5 ± 2.1 | 31.1 ± 3.1 | 82.1 ± 5.1 | 6.2 |
| 1e |  |  | - | 9.1 ± 0.7 | 27.9 ± 3.9 | 34.1 ± 7.5 | 3.7 |
| 1f |  |  |  | 10.1 ± 1.4 | 29.1 ± 2.1 | 41.1 ± 2.1 | 4.1 |
| 1g |  |  | - | 6.7 ± 1.8 | 11.4 ± 2.1 | 99.5 ± 12.5 | 14.9 |
| 1h |  |  | - | 12.1 ± 3.9 | 19.4 ± 3.6 | 24.4 ± 2.6 | 2.0 |
| 1i |  |  | - | 15.9 ± 3.1 | 27.2 ± 3.4 | 34.2 ± 3.4 | 2.1 |
| 2a |  |  | - | 6.7 ± 1.6 | 25.3 ± 1.9 | 45.1 ± 1.9 | 6.7 |
| 2b |  |  | - | 11.3 ± 1.1 | 27.4 ± 2.4 | 44.4 ± 3.4 | 3.9 |
| 2c |  |  | - | 12.6 ± 2.4 | 30.9 ± 4.7 | 48.9 ± 4.7 | 3.8 |
| 2d |  |  | - | 11.9 ± 1.7 | 28.8 ± 4.6 | 141.8 ± 17.6 | 11.9 |
| 2e |  |  | - | 6.8 ± 1.5 | 19.7 ± 3.2 | 47.7 ± 3.2 | 7.0 |
| 2f |  |  | - | 5.7 ± 1.4 | 76.6 ± 4.9 | 40.6 ± 2.9 | 7.1 |
| 2g |  |  | - | 10.3 ± 2.4 | 37.7 ± 4.1 | 47.7 ± 5.2 | 4.6 |
| 2h |  |  | - | 22.4 ± 2.2 | 31.5 ± 6.1 | 63.4 ± 7.1 | 2.8 |
| 2i |  |  | - | 15.8 ± 3.2 | 34.8 ± 5.3 | 44.8 ± 3.3 | 2.8 |
| 2j |  |  | - | 60.2 ± 9.8 | >100 | 93.5 ± 6.6 | 1.5 |
| Bz | - | - | - | 1.4 ± 0.4 | 7.9 ± 1.2 | >500 | >357 |
| C2 * |  |  | - | 9.36 ± 1.90 | 22.6 ± 0.6 | 178.90 ± 6.18 | 19.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lara, L.S.; Lechuga, G.C.; Moreira, C.d.S.; Santos, T.B.; Ferreira, V.F.; da Rocha, D.R.; Pereira, M.C.S. Optimization of 1,4-Naphthoquinone Hit Compound: A Computational, Phenotypic, and In Vivo Screening against Trypanosoma cruzi. Molecules 2021, 26, 423. https://doi.org/10.3390/molecules26020423
Lara LS, Lechuga GC, Moreira CdS, Santos TB, Ferreira VF, da Rocha DR, Pereira MCS. Optimization of 1,4-Naphthoquinone Hit Compound: A Computational, Phenotypic, and In Vivo Screening against Trypanosoma cruzi. Molecules. 2021; 26(2):423. https://doi.org/10.3390/molecules26020423
Chicago/Turabian StyleLara, Leonardo S., Guilherme C. Lechuga, Caroline dos S. Moreira, Thaís B. Santos, Vitor F. Ferreira, David R. da Rocha, and Mirian C. S. Pereira. 2021. "Optimization of 1,4-Naphthoquinone Hit Compound: A Computational, Phenotypic, and In Vivo Screening against Trypanosoma cruzi" Molecules 26, no. 2: 423. https://doi.org/10.3390/molecules26020423
APA StyleLara, L. S., Lechuga, G. C., Moreira, C. d. S., Santos, T. B., Ferreira, V. F., da Rocha, D. R., & Pereira, M. C. S. (2021). Optimization of 1,4-Naphthoquinone Hit Compound: A Computational, Phenotypic, and In Vivo Screening against Trypanosoma cruzi. Molecules, 26(2), 423. https://doi.org/10.3390/molecules26020423