In Vitro and In Silico Study of Analogs of Plant Product Plastoquinone to Be Effective in Colorectal Cancer Treatment
Abstract
:1. Introduction
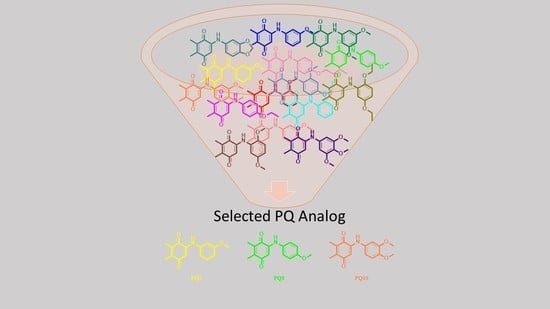
2. Results
2.1. Biological Activity
2.1.1. In Vitro Screening of Antiproliferative Activity at One Dose
2.1.2. Determination of Cell Viability
2.1.3. Determination of Cell Death
2.2. In Silico Prediction of Pharmacokinetic Properties
3. Discussion
4. Materials and Methods
4.1. Chemistry
4.2. Biological Evaluation
4.2.1. In Vitro Antiproliferative Activity at Single-Dose Concentration by NCI
4.2.2. Cell Culture and Drug Treatment
4.2.3. MTT Assay
4.2.4. Detection of Cell Death
4.3. Molecular Docking Studies
4.4. In Silico ADME Estimation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Brannon-Peppas, L.; Blanchette, J.O. Nanoparticle and targeted systems for cancer therapy. Adv. Drug Deliv. Rev. 2004, 56, 1649–1659. [Google Scholar] [CrossRef] [PubMed]
- Hebar, A.; Valent, P.; Selzer, E. The impact of molecular targets in cancer drug development: Major hurdles and future strategies. Expert Rev. Clin. Pharmacol. 2013, 6, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Gewirtz, D.A.; Bristol, M.L.; Yalowich, J.C. Toxicity issues in cancer drug development. Curr. Opin. Investig. Drugs 2010, 11, 612–614. [Google Scholar] [PubMed]
- Cragg, G.M.; Grothaus, P.G.; Newman, D.J. Impact of natural products on developing new anti-cancer agents. Chem. Rev. 2009, 109, 3012–3043. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.J.; Cragg, G.M. Natural products as sources of new drugs over the last 25 years. J. Nat. Prod. 2007, 70, 461–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butler, M.S. Natural products to drugs: Natural product-derived compounds in clinical trials. Nat. Prod. Rep. 2008, 25, 475–516. [Google Scholar] [CrossRef]
- Collett, N.P.; Amin, A.R.M.R.; Bayraktar, S.; Pezzuto, J.M.; Shin, D.M.; Khuri, F.R.; Aggarwal, B.B.; Surh, Y.J.; Kucuk, O. Cancer prevention with natural compounds. Semin. Oncol. 2010, 37, 258–281. [Google Scholar]
- Begleiter, A. Clinical applications of quinone-containing alkylating agents. Front. Biosci. 2000, 5, E153–E171. [Google Scholar] [CrossRef] [Green Version]
- Newman, D.J.; Cragg, G.M. Natural products as sources of new drugs from 1981 to 2014. J. Nat. Prod. 2016, 79, 629–661. [Google Scholar] [CrossRef] [Green Version]
- de Almeida, P.D.O.; Jobim, G.D.B.; Ferreira, C.C.D.; Bernardes, L.R.; Dias, R.B.; Sales, C.B.S.; Valverde, L.D.; Rocha, C.A.G.; Soares, M.B.P.; Bezerra, D.P.; et al. A new synthetic antitumor naphthoquinone induces ROS-mediated apoptosis with activation of the JNK and p38 signaling pathways. Chem. Biol. Interact. 2021, 343, 109444. [Google Scholar] [CrossRef]
- Wellington, K.W.; Kolesnikova, N.I.; Nyoka, N.B.P.; McGaw, L.J. Investigation of the antimicrobial and anticancer activity of aminonaphthoquinones. Drug Dev. Res. 2019, 80, 138–146. [Google Scholar] [CrossRef] [Green Version]
- Wellington, K.W. Understanding cancer and the anticancer activities of naphthoquinones—A review. RSC Adv. 2015, 5, 20309–20338. [Google Scholar] [CrossRef]
- Defant, A.; Mancini, I. Design, synthesis and cancer cell growth inhibition evaluation of new aminoquinone hybrid molecules. Molecules 2019, 24, 2224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nain-Perez, A.; Barbosa, L.C.A.; Rodriguez-Hernandez, D.; Kramell, A.E.; Heller, L.; Csuk, R. Natural abenquines and synthetic analogues: Preliminary exploration of their cytotoxic activity. Bioorg. Med. Chem. Lett. 2017, 27, 1141–1144. [Google Scholar] [CrossRef] [PubMed]
- Aminin, D.; Polonik, S. 1,4-Naphthoquinones: Some biological properties and application. Chem. Pharmacol. Bull. 2020, 68, 46–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kruschel, R.D.; Buzid, A.; Khandavilli, U.B.R.; Lawrence, S.E.; Glennon, J.D.; McCarthy, F.O. Isoquinolinequinone N-oxides as anticancer agents effective against drug resistant cell lines. Org. Biomol. Chem. 2020, 18, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Coutelle, O.; Hornig-Do, H.T.; Witt, A.; Andree, M.; Schiffmann, L.M.; Piekarek, M.; Brinkmann, K.; Seeger, J.M.; Liwschitz, M.; Miwa, S.; et al. Embelin inhibits endothelial mitochondrial respiration and impairs neoangiogenesis during tumor growth and wound healing. EMBO Mol. Med. 2014, 6, 624–639. [Google Scholar] [CrossRef]
- Asaduzzaman Khan, M.A.; Tania, M.; Fu, S.Y.; Fu, J.J. Thymoquinone, as an anticancer molecule: From basic research to clinical investigation. Oncotarget 2017, 8, 51907–51919. [Google Scholar] [CrossRef] [Green Version]
- Mostofa, A.G.M.; Hossain, M.K.; Basak, D.; Bin Sayeed, M.S. Thymoquinone as a potential adjuvant therapy for cancer treatment: Evidence from preclinical studies. Front. Pharmacol. 2017, 8, 295. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Zou, C.; Zhao, W.; Yu, Y.; Cui, Y.; Zhang, H.E.F.; Qiu, Z.; Zou, C.; Gao, X. Juglone eliminates MDSCs accumulation and enhances antitumor immunity. Int. Immunopharmacol. 2019, 73, 118–127. [Google Scholar] [CrossRef]
- Seetha, A.; Devaraj, H.; Sudhandiran, G. Indomethacin and juglone inhibit inflammatory molecules to induce apoptosis in colon cancer cells. J. Biochem. Mol. Toxicol. 2020, 34, e22433. [Google Scholar] [CrossRef]
- Seetha, A.; Devaraj, H.; Sudhandiran, G. Effects of combined treatment with indomethacin and juglone on AOM/DSS induced colon carcinogenesis in Balb/c mice: Roles of inflammation and apoptosis. Life Sci. 2021, 264, 118657. [Google Scholar] [CrossRef] [PubMed]
- Majiene, D.; Kuseliauskyte, J.; Stimbirys, A.; Jekabsone, A. Comparison of the effect of native 1,4-naphthoquinones plumbagin, menadione, and lawsone on viability, redox status, and mitochondrial functions of C6 glioblastoma cells. Nutrients 2019, 11, 1294. [Google Scholar] [CrossRef] [Green Version]
- Kawamukai, M. Biosynthesis and applications of prenylquinones. Biosci. Biotechnol. Biochem. 2018, 82, 963–977. [Google Scholar] [CrossRef] [PubMed]
- Boler, J.; Pardini, R.; Mustafa, H.T.; Folkers, K.; Dilley, R.A.; Crane, F.L. Synthesis of plastoquinone analogs and inhibition of photosynthetic and mammalian enzyme systems. Proc. Natl. Acad. Sci. USA 1972, 69, 3713–3717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, M.M.; Lu, S.F. Plastoquinone and ubiquinone in plants: Biosynthesis, physiological function and metabolic engineering. Front. Plant Sci. 2016, 7, 1898. [Google Scholar] [CrossRef] [Green Version]
- Jannuzzi, A.T.; Yıldız, M.; Bayrak, N.; Yıldırım, H.; Shilkar, D.; Jayaprakash, V.; Tuyun, A.F. Anticancer agents based on Plastoquinone analogs with N-phenylpiperazine: Structure-activity relationship and mechanism of action in breast cancer cells. Chem. Biol. Interact. 2021, 349, 109673. [Google Scholar] [CrossRef]
- Bayrak, N.; Yildirim, H.; Yildiz, M.; Radwan, M.O.; Otsuka, M.; Fujita, M.; Ciftci, H.I.; Tuyun, A.F. A novel series of chlorinated plastoquinone analogs: Design, synthesis, and evaluation of anticancer activity. Chem. Biol. Drug Des. 2020, 95, 343–354. [Google Scholar] [CrossRef]
- Bayrak, N.; Yildirim, H.; Yildiz, M.; Radwan, M.O.; Otsuka, M.; Fujita, M.; Tuyun, A.F.; Ciftci, H.I. Design, synthesis, and biological activity of Plastoquinone analogs as a new class of anticancer agents. Bioorg. Chem. 2019, 92, 103255. [Google Scholar] [CrossRef]
- Ciftci, H.I.; Bayrak, N.; Yildirim, H.; Yildiz, M.; Radwan, M.O.; Otsuka, M.; Fujita, M.; Tuyun, A.F. Discovery and structure-activity relationship of plastoquinone analogs as anticancer agents against chronic myelogenous leukemia cells. Arch. Pharmacol. 2019, 352, 1900170. [Google Scholar] [CrossRef]
- Yildirim, H.; Bayrak, N.; Yildiz, M.; Kara, E.M.; Celik, B.O.; Tuyun, A.F. Thiolated plastoquinone analogs: Synthesis, characterization, and antimicrobial evaluation. J. Mol. Struct. 2019, 1195, 681–688. [Google Scholar] [CrossRef]
- Yildirim, H.; Bayrak, N.; Tuyun, A.F.; Kara, E.M.; Celik, B.O.; Gupta, G.K. 2,3-Disubstituted-1,4-naphthoquinones containing an arylamine with trifluoromethyl group: Synthesis, biological evaluation, and computational study. RSC Adv. 2017, 7, 25753–25764. [Google Scholar] [CrossRef] [Green Version]
- Ibis, C.; Ozsoy-Gunes, Z.; Tuyun, A.F.; Ayla, S.S.; Bahar, H.; Stasevych, M.V.; Musyanovych, R.Y.; Komarovska-Porokhnyavets, O.; Novikov, V. Synthesis, antibacterial and antifungal evaluation of thio- or piperazinyl-substituted 1,4-naphthoquinone derivatives. J. Sulfur Chem. 2016, 37, 477–487. [Google Scholar] [CrossRef]
- Tuyun, A.F.; Bayrak, N.; Yildirim, H.; Onul, N.; Kara, E.M.; Celik, B.O. Synthesis and in vitro biological evaluation of aminonaphthoquinones and benzo[b]phenazine-6,11-dione derivatives as potential antibacterial and antifungal compounds. J. Chem. 2015, 2015, 645902. [Google Scholar] [CrossRef] [Green Version]
- Boyd, M.R.; Pauli, K.D. Some practical considerations and applications of the National-Cancer-Institute in vitro anticancer drug discovery screen. Drug Dev. Res. 1995, 34, 91–109. [Google Scholar] [CrossRef]
- Yin, A.; Jiang, Y.; Zhang, X.; Zhao, J.; Luo, H. Transfection of PDCD5 sensitizes colorectal cancer cells to cisplatin-induced apoptosis in vitro and in vivo. Eur. J. Pharmacol. 2010, 649, 120–126. [Google Scholar] [CrossRef]
- Brogden, A.L.; Hopcroft, N.H.; Searcey, M.; Cardin, C.J. Ligand bridging of the DNA Holliday junction: Molecular recognition of a stacked-X four-way junction by a small molecule. Angew. Chem. Int. Ed. Eng. 2007, 46, 3850–3854. [Google Scholar] [CrossRef]
- Colorectal Cancer. Available online: https://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf (accessed on 19 October 2021).
- Khalife, R.; Hodroj, M.H.; Fakhoury, R.; Rizk, S. Thymoquinone from Nigella sativa seeds promotes the antitumor activity of noncytotoxic doses of topotecan in human colorectal cancer cells in vitro. Planta Med. 2016, 82, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Wirries, A.; Breyer, S.; Quint, K.; Schobert, R.; Ocker, M. Thymoquinone hydrazone derivatives cause cell cycle arrest in p53-competent colorectal cancer cells. Exp. Ther. Med. 2010, 1, 369–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glamočlija, U.; Padhye, S.; Špirtović-Halilović, S.; Osmanović, A.; Veljović, E.; Roca, S.; Novaković, I.; Mandić, B.; Turel, I.; Kljun, J.; et al. Synthesis, biological evaluation and docking studies of benzoxazoles derived from thymoquinone. Molecules 2018, 23, 3297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kadela-Tomanek, M.; Jastrzebska, M.; Marciniec, K.; Chrobak, E.; Bebenek, E.; Latocha, M.; Kusmierz, D.; Boryczka, S. Design, synthesis and biological activity of 1,4-quinone moiety attached to betulin derivatives as potent DT-diaphorase substrate. Bioorg. Chem. 2021, 106, 104478. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, R.M.; Muqbil, I.; Lowe, L.; Yedjou, C.; Hsu, H.Y.; Lin, L.T.; Siegelin, M.D.; Fimognari, C.; Kumar, N.B.; Dou, Q.P.; et al. Broad targeting of resistance to apoptosis in cancer. Semin. Cancer Biol. 2015, 35, S78–S103. [Google Scholar] [CrossRef]
- Jia, L.T.; Chen, S.Y.; Yang, A.G. Cancer gene therapy targeting cellular apoptosis machinery. Cancer Treat. Rev. 2012, 38, 868–876. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kruyt, F.A.; Schuringa, J.J. Apoptosis and cancer stem cells: Implications for apoptosis targeted therapy. Biochem. Pharmacol. 2010, 80, 423–430. [Google Scholar] [CrossRef]
- Bold, R.J.; Termuhlen, P.M.; McConkey, D.J. Apoptosis, cancer and cancer therapy. Surg. Oncol. 1997, 6, 133–142. [Google Scholar] [CrossRef]
- Bayrak, N.; Ciftci, H.I.; Yildiz, M.; Yildirim, H.; Sever, B.; Tateishi, H.; Otsuka, M.; Fujita, M.; Tuyun, A.F. Structure based design, synthesis, and evaluation of anti-CML activity of the quinolinequinones as LY83583 analogs. Chem. Biol. Interact. 2021, 345, 109555. [Google Scholar] [CrossRef]
- Ciftci, H.I.; Bayrak, N.; Yıldız, M.; Yıldırım, H.; Sever, B.; Tateishi, H.; Otsuka, M.; Fujita, M.; Tuyun, A.F. Design, synthesis and investigation of the mechanism of action underlying anti-leukemic effects of the quinolinequinones as LY83583 analogs. Bioorg. Chem. 2021, 114, 105160. [Google Scholar] [CrossRef]
- Kim, T.; Park, H. Computational prediction of octanol-water partition coefficient based on the extended solvent-contact model. J. Mol. Graph. Model. 2015, 60, 108–117. [Google Scholar] [CrossRef]
- Hewitt, M.; Cronin, M.T.; Enoch, S.J.; Madden, J.C.; Roberts, D.W.; Dearden, J.C. In silico prediction of aqueous solubility: The solubility challenge. J. Chem. Inf. Model. 2009, 49, 2572–2587. [Google Scholar] [CrossRef]
- Vallianatou, T.; Lambrinidis, G.; Tsantili-Kakoulidou, A. In silico prediction of human serum albumin binding for drug leads. Expert Opin. Drug Discov. 2013, 8, 583–595. [Google Scholar] [CrossRef]
- Pardridge, W.M. Drug and gene delivery to the brain: The vascular route. Neuron 2002, 36, 555–558. [Google Scholar] [CrossRef] [Green Version]
- Monks, A.; Scudiero, D.; Skehan, P.; Shoemaker, R.; Paull, K.; Vistica, D.; Hose, C.; Langley, J.; Cronise, P.; Vaigrowolff, A.; et al. Feasibility of a high-flux anticancer drug screen using a diverse panel of cultured human tumor cell lines. J. Natl. Cancer Inst. 1991, 83, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Grever, M.R.; Schepartz, S.A.; Chabner, B.A. The National-Cancer-Institute: Cancer drug discovery and development program. Semin. Oncol. 1992, 19, 622–638. [Google Scholar] [PubMed]
- Sever, B.; Altintop, M.D.; Ozdemir, A.; Akalin Ciftci, G.; Ellakwa, D.E.; Tateishi, H.; Radwan, M.O.; Ibrahim, M.A.A.; Otsuka, M.; Fujita, M.; et al. In vitro and in silico evaluation of anticancer activity of new indole-based 1,3,4-oxadiazoles as EGFR and COX-2 inhibitors. Molecules 2020, 25, 5190. [Google Scholar] [CrossRef]
- Ciftci, H.I.; Radwan, M.O.; Sever, B.; Hamdy, A.K.; Emirdağ, S.; Ulusoy, N.G.; Sozer, E.; Can, M.; Yayli, N.; Araki, N.; et al. EGFR-targeted pentacyclic triterpene analogues for glioma therapy. Int. J. Mol. Sci. 2021, 22, 10945. [Google Scholar] [CrossRef]
- Zeytün, E.; Altıntop, M.D.; Sever, B.; Özdemir, A.; Ellakwa, D.E.; Ocak, Z.; Ciftci, H.I.; Otsuka, M.; Fujita, M.; Radwan, M.O. A new series of antileukemic agents: Design, synthesis, in vitro and in silico evaluation of thiazole-based ABL1 kinase inhibitors. Anticancer Agents Med. Chem. 2021, 21, 1099–1109. [Google Scholar] [CrossRef]
- Ciftci, H.I.; Can, M.; Ellakwa, D.E.; Suner, S.C.; Ibrahim, M.A.; Oral, A.; Sekeroglu, N.; Özalp, B.; Otsuka, M.; Fujita, M.; et al. Anticancer activity of Turkish marine extracts: A purple sponge extract induces apoptosis with multitarget kinase inhibition activity. Investig. New Drugs 2020, 38, 1326–1333. [Google Scholar] [CrossRef]
- Tateishi, H.; Monde, K.; Anraku, K.; Koga, R.; Hayashi, Y.; Ciftci, H.I.; DeMirci, H.; Higashi, T.; Motoyama, K.; Arima, H.; et al. A clue to unprecedented strategy to HIV eradication: “Lock-in and apoptosis”. Sci. Rep. 2017, 7, 8957. [Google Scholar] [CrossRef] [PubMed]













| ID | Substitution Groups | Cell Type (IC50, μM) | ||||||
|---|---|---|---|---|---|---|---|---|
| R1 | R2 | R3 | R4 | K562 a | Jurkat a | MT-2 a | PBMC a | |
| PQ2 | H | OCH3 | H | H | 6.40 ± 1.73 | 7.72 ± 1.49 | >100 | >300 |
| PQ3 | H | H | OCH3 | H | 9.66 ± 2.31 | 22.75 ± 1.93 | 53.96 ± 3.81 | 72.68 ± 6.51 |
| PQ10 | H | OCH3 | OCH3 | H | 8.91 ± 1.26 | 14.47 ± 1.35 | 35.79 ± 0.89 | 69.35 ± 7.12 |
| Imatinib b | 7.47 ± 2.22 | 9.49 ± 2.46 | 22.09 ± 1.76 | 39.81 ± 4.38 | ||||
| Panel/Cancer Cell Line | Compounds | ||
|---|---|---|---|
| PQ2 | PQ3 | PQ10 | |
| Growth Percent | |||
| Leukemia | |||
| CCRF-CEM | 15.84 | 70.07 | 28.00 |
| HL-60(TB) | 3.49 | 80.23 | 43.99 |
| K-562 | 12.54 | 66.58 | 86.47 |
| MOLT-4 | 17.89 | 75.57 | 45.57 |
| RPMI-8226 | 17.52 | 73.34 | 73.88 |
| SR | 23.16 | 82.29 | 65.36 |
| NSCLC | |||
| A549/ATCC | 101.36 | 97.30 | 102.53 |
| EKVX | 36.72 | 78.84 | 80.02 |
| HOP-62 | 105.69 | 99.66 | 112.71 |
| HOP-92 | 104.31 | 171.92 | 136.73 |
| NCI-H226 | 97.00 | 97.24 | 109.09 |
| NCI-H23 | ND * | ND * | 69.62 |
| NCI-H322M | 101.88 | 103.08 | 102.13 |
| NCI-H460 | 100.51 | 99.63 | 100.07 |
| NCI-H522 | 49.81 | 82.47 | 86.90 |
| Colorectal Cancer | |||
| COLO 205 | 103.02 | 106.66 | 112.41 |
| HCC-2998 | ND * | ND * | 113.67 |
| HCT-116 | 10.54 | 80.60 | 92.46 |
| HCT-15 | 91.87 | 89.04 | 95.39 |
| HT29 | 98.29 | 109.10 | 105.03 |
| KM12 | 98.44 | 101.37 | 101.36 |
| SW-620 | 101.81 | 101.18 | 102.32 |
| CNS Cancer | |||
| SF-268 | 74.53 | 100.81 | 107.49 |
| SF-295 | 105.11 | 104.94 | 108.44 |
| SF-539 | 21.69 | 104.69 | 117.66 |
| SNB-19 | 97.72 | 99.17 | 101.23 |
| SNB-75 | 99.78 | 123.25 | 110.24 |
| U251 | 95.10 | 92.04 | 100.71 |
| Melanoma | |||
| LOX IMVI | ND * | ND * | 70.80 |
| MALME-3M | 101.18 | 89.92 | 102.29 |
| M14 | 97.05 | 95.56 | 101.40 |
| MDA-MB-435 | 7.25 | 7.80 | 103.13 |
| SK-MEL-2 | 83.57 | 81.83 | 95.65 |
| SK-MEL-28 | 96.53 | 99.39 | 110.98 |
| SK-MEL-5 | ND * | ND * | 97.50 |
| UACC-257 | 54.67 | 45.42 | 87.07 |
| UACC-62 | 91.77 | 95.37 | 97.60 |
| Ovarian Cancer | |||
| IGROV1 | 39.99 | 89.25 | 104.41 |
| OVCAR-3 | 0.29 | 9.94 | 28.72 |
| OVCAR-4 | −1.68 | 43.81 | 42.19 |
| OVCAR-5 | 100.60 | 109.36 | 107.95 |
| OVCAR-8 | 16.95 | 79.12 | 89.21 |
| NCI/ADR-RES | ND * | ND * | 80.54 |
| SK-OV-3 | ND * | ND * | ND * |
| Renal Cancer | |||
| 786-0 | 95.76 | 90.51 | 105.71 |
| A498 | 67.18 | 84.44 | 85.07 |
| ACHN | 70.90 | 96.11 | 96.60 |
| CAKI-1 | 93.02 | 93.46 | 104.67 |
| RXF 393 | 55.80 | 101.91 | 114.84 |
| SN12C | 80.52 | 86.43 | 94.65 |
| TK-10 | 135.29 | 156.13 | 158.01 |
| UO-31 | 86.04 | 81.15 | 98.44 |
| Prostate Cancer | |||
| PC-3 | 36.32 | 71.45 | 81.05 |
| DU-145 | 113.12 | 105.22 | 112.19 |
| Breast Cancer | |||
| MCF7 | 64.11 | 71.87 | 88.94 |
| MDA-MB-231/ATCC | 41.39 | 83.80 | 88.36 |
| HS 578T | 112.09 | 109.96 | 110.28 |
| BT-549 | 127.05 | 118.89 | 123.57 |
| T-47D | 47.75 | 67.51 | 62.22 |
| MDA-MB-468 | 25.85 | 56.98 | 18.15 |
| Compound | 2GWA | ||
|---|---|---|---|
| Docking Score | Glide Score | Glide Emodel | |
| PQ2 | −5.848 | −5.848 | −48.650 |
| PQ3 | −5.628 | −5.628 | −43.682 |
| PQ10 | −5.833 | −5.833 | −44.605 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciftci, H.; Sever, B.; Ocak, F.; Bayrak, N.; Yıldız, M.; Yıldırım, H.; DeMirci, H.; Tateishi, H.; Otsuka, M.; Fujita, M.; et al. In Vitro and In Silico Study of Analogs of Plant Product Plastoquinone to Be Effective in Colorectal Cancer Treatment. Molecules 2022, 27, 693. https://doi.org/10.3390/molecules27030693
Ciftci H, Sever B, Ocak F, Bayrak N, Yıldız M, Yıldırım H, DeMirci H, Tateishi H, Otsuka M, Fujita M, et al. In Vitro and In Silico Study of Analogs of Plant Product Plastoquinone to Be Effective in Colorectal Cancer Treatment. Molecules. 2022; 27(3):693. https://doi.org/10.3390/molecules27030693
Chicago/Turabian StyleCiftci, Halilibrahim, Belgin Sever, Firdevs Ocak, Nilüfer Bayrak, Mahmut Yıldız, Hatice Yıldırım, Hasan DeMirci, Hiroshi Tateishi, Masami Otsuka, Mikako Fujita, and et al. 2022. "In Vitro and In Silico Study of Analogs of Plant Product Plastoquinone to Be Effective in Colorectal Cancer Treatment" Molecules 27, no. 3: 693. https://doi.org/10.3390/molecules27030693
APA StyleCiftci, H., Sever, B., Ocak, F., Bayrak, N., Yıldız, M., Yıldırım, H., DeMirci, H., Tateishi, H., Otsuka, M., Fujita, M., & TuYuN, A. F. (2022). In Vitro and In Silico Study of Analogs of Plant Product Plastoquinone to Be Effective in Colorectal Cancer Treatment. Molecules, 27(3), 693. https://doi.org/10.3390/molecules27030693