Oral Bioactive Self-Nanoemulsifying Drug Delivery Systems of Remdesivir and Baricitinib: A Paradigmatic Case of Drug Repositioning for Cancer Management
Abstract
:1. Introduction
2. Results
2.1. GC-MS Analysis to Determine Active Phytocomponents of FSO and BSO
2.2. Visual Assessment of the Formulations
2.3. Robustness to Dilution
2.4. Thermodynamic Stability
2.5. Droplet Size, Zeta Potential Measurement of the Bio-SNEDDS
2.6. Equilibrium Solubility and Drug Loading in the Bio-SNEDDS
2.7. Viscosity of the Bio-SNEDDS Formulations
2.8. TEM Analysis
2.9. Effect of Different Concentrations of Pure Oils and Their Different Formulations on the Proliferation of Breast Cancer Cell Lines
2.10. Effect of Different Concentrations of Pure Oils and Their Different Formulations on the Proliferation of A549 Lung Cancer Cell Lines
2.11. Effect of Different Concentrations of Pure Oils and Their Different Formulations on the Proliferation of Normal Human Fibroblasts Cell Lines
3. Materials and Methods
3.1. Materials
3.2. Plant Material and Extraction of Bioactive Oils
3.3. GC-MS Analysis to Determine Active Phytocomponents of FSO and BSO
3.3.1. GC-MS Analysis Method
3.3.2. GC-MS Instrumentation
3.4. Selection of Excipients and Bio-SNEDDS Development
3.5. Euilibrium Solubility and Drug Loading into Bio-SNEDDS
3.6. Visual Assessment of the Formulations
3.7. Robustness to Dilution
3.8. Thermodynamic Stability
3.9. Measurement of Droplet Size, Polydispersity Index (PDI), and Zeta Potential
3.10. Viscosity of the Bio-SNEDDS Formulations
3.11. Transmission Electron Microscopy (TEM)
3.12. Cell Lines and Culturing Conditions
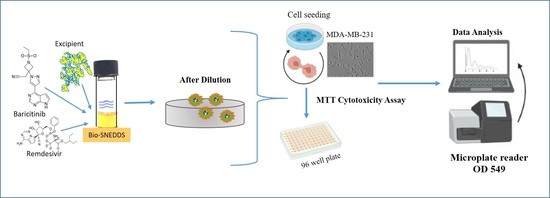
3.13. Anti-Proliferative Activity via MTT Assay
3.14. Statistical Analysis
4. Discussion
- (a)
- The use of high proportion of hydrophilic excipients in the formulation (Type III system) [35].
- (b)
- The inclusion of bioactive oils, which possess good self-emulsification properties as BSO [11].
- (c)
- The inclusion of the polar mixed glycerides in the formulation.
- (d)
- The inclusion of the highly purified and highly hydrophilic surfactant, refined T80 (HLB = 15), which was suggested to adhere to the drug particles’ surfaces, forming a protective layer that reduces solid–liquid interfacial tension, preventing agglomeration of the particles [36].
- (1)
- Drug-free formulation systems and bio-SNEDDS possess superior anti-proliferative activity compared to RMV and BRB.
- (2)
- The very low RMV or BRB concentration in bio-SNEDDS (5 mg/g) could be remarkably masked by bio-SNEDDS activity.
- (3)
- The cosurfactant I988 and/or surfactant refined Tween 80 might possess anti-proliferative activity against breast and lung cancer cells [38].
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Afrin, H.; Salazar, C.J.; Kazi, M.; Ahamad, S.R.; Alharbi, M.; Nurunnabi, M. Methods of screening, monitoring and management of cardiac toxicity induced by chemotherapeutics. Chin. Chem. Lett. 2022, 33, 2773–2782. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA A Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Alshehri, S.; Imam, S.S.; Rizwanullah, M.; Akhter, S.; Mahdi, W.; Kazi, M.; Ahmad, J. Progress of cancer nanotechnology as diagnostics, therapeutics, and theranostics nanomedicine: Preclinical promise and translational challenges. Pharmaceutics 2021, 13, 24. [Google Scholar] [CrossRef] [PubMed]
- The Business Research Company. Global Oncology Drugs Market Report 2022—Market Forecast, Trends and Strategies; The Business Research Company: London, UK, 2022. [Google Scholar]
- Wang, M.; Cao, R.; Zhang, L.; Yang, X.; Liu, J.; Xu, M.; Shi, Z.; Hu, Z.; Zhong, W.; Xiao, G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020, 30, 269–271. [Google Scholar] [CrossRef] [PubMed]
- Newsware, M. Jubilant Reveals Promising Safety, Absorption Data for Oral Form of Covid-19 Drug Remdesivir; MT Newsware: Bethesda, MA, USA, 2021. [Google Scholar]
- Chen, J.; Dai, L.; Kendrick, S.; Post, S.R.; Qin, Z. The Anti-COVID-19 Drug Remdesivir Promotes Oncogenic Herpesvirus Reactivation through Regulation of Intracellular Signaling Pathways. Antimicrob. Agents Chemother. 2022, 66, e0239521. [Google Scholar] [CrossRef]
- Lee, C.M.; Kang, M.-A.; Bae, J.S.; Park, K.; Yang, Y.-H.; Lee, J.; Jang, K.Y.; Park, S.-H. An in vitro study on anti-carcinogenic effect of remdesivir in human ovarian cancer cells via generation of reactive oxygen species. Hum. Exp. Toxicol. 2022, 41, 09603271221089257. [Google Scholar] [CrossRef]
- Cox, R.M.; Wolf, J.D.; Lieber, C.M.; Sourimant, J.; Lin, M.J.; Babusis, D.; DuPont, V.; Chan, J.; Barrett, K.T.; Lye, D.; et al. Oral prodrug of remdesivir parent GS-441524 is efficacious against SARS-CoV-2 in ferrets. Nat. Commun. 2021, 12, 6415. [Google Scholar] [CrossRef]
- Fact Sheet for Healthcare Providers: Emergency Use Authorization (EUA) of Baricitinib. 2021. Available online: https://www.fda.gov/media/143823/download (accessed on 26 February 2023).
- Kazi, M.; Shahba, A.A.; Alrashoud, S.; Alwadei, M.; Sherif, A.Y.; Alanazi, F.K. Bioactive Self-Nanoemulsifying Drug Delivery Systems (Bio-SNEDDS) for Combined Oral Delivery of Curcumin and Piperine. Molecules 2020, 25, 1703. [Google Scholar] [CrossRef] [Green Version]
- Hussain, D.A.S.; Hussain, M.M. Nigella sativa (black seed) is an effective herbal remedy for every disease except death—A prophetic statement which modern scientists confirm unanimously: A review. Adv. Med. Plant Res. 2016, 4, 27–57. [Google Scholar]
- Ahmad, A.; Husain, A.; Mujeeb, M.; Khan, S.A.; Najmi, A.K.; Siddique, N.A.; Damanhouri, Z.A.; Anwar, F. A review on therapeutic potential of Nigella sativa: A miracle herb. Asian Pac. J. Trop. Biomed. 2013, 3, 337–352. [Google Scholar] [CrossRef] [Green Version]
- Khan, M.A.; Chen, H.C.; Tania, M.; Zhang, D.Z. Anticancer activities of Nigella sativa (black cumin). Afr. J. Tradit. Complement. Altern. Med. 2011, 8, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Kazi, M. Lipid-Based Nano-Delivery for Oral Administration of Poorly Water Soluble Drugs (PWSDs): Design, Optimization and in vitro Assessment. In Advanced Technology for Delivering Therapeutics; InTech: London, UK, 2017. [Google Scholar]
- Pandya, M.; Chatterjee, B.; Ganti, S. Self-emulsifying drug delivery system for oral anticancer therapy: Constraints and recent development. Curr. Pharm. Des. 2022, 28, 2538–2553. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, Q.M.; Kazi, M.; Khaleel, M.A.; Al-Deeb, I.; Nasr, A.-R.T.; Phillips, R.M. Utilization of novel self-nanoemulsifying formulations (SNEFs) loaded paclitaxel for the treatment prosperity of bladder cancer. J. Drug Deliv. Sci. Technol. 2020, 56, 101514. [Google Scholar] [CrossRef]
- Kazi, M.; Alanazi, F.K.; Hussain, M.D. In vitro methods for in vitro-in vivo correlation (IVIVC) for poorly water soluble drugs: Lipid based formulation perspective. Curr. Drug Deliv. 2018, 15, 918–929. [Google Scholar] [CrossRef] [PubMed]
- Armaka, M.; Papanikolaou, E.; Sivropoulou, A.; Arsenakis, M. Antiviral properties of isoborneol, a potent inhibitor of herpes simplex virus type 1. Antivir. Res. 1999, 43, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Aparna, V.; Dileep, K.V.; Mandal, P.K.; Karthe, P.; Sadasivan, C.; Haridas, M. Anti-inflammatory property of n-hexadecanoic acid: Structural evidence and kinetic assessment. Chem. Biol. Drug Des. 2012, 80, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Brondz, I. Fatty Acids. In Reference Module in Chemistry, Molecular Sciences and Chemical Engineering; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar] [CrossRef]
- Alshadidi, A.; Shahba, A.A.-W.; Sales, I.; Rashid, M.A.; Kazi, M. Combined Curcumin and Lansoprazole-Loaded Bioactive Solid Self-Nanoemulsifying Drug Delivery Systems (Bio-SSNEDDS). Pharmaceutics 2022, 14, 2. [Google Scholar] [CrossRef]
- Shahba, A.A.-W.; Mohsin, K.; Alanazi, F.K. The studies of phase equilibria and efficiency assessment for self-emulsifying lipid-based formulations. AAPS PharmSciTech 2012, 13, 522–533. [Google Scholar] [CrossRef] [Green Version]
- Shahba, A.A.-W.; Sherif, A.Y.; Elzayat, E.M.; Kazi, M. Combined Ramipril and Black Seed Oil Dosage Forms Using Bioactive Self-Nanoemulsifying Drug Delivery Systems (BIO-SNEDDSs). Pharmaceuticals 2022, 15, 1120. [Google Scholar] [CrossRef]
- Baral, K.C.; Song, J.-G.; Lee, S.H.; Bajracharya, R.; Sreenivasulu, G.; Kim, M.; Lee, K.; Han, H.-K. Enhanced Bioavailability of AC1497, a Novel Anticancer Drug Candidate, via a Self-Nanoemulsifying Drug Delivery System. Pharmaceutics 2021, 13, 1142. [Google Scholar] [CrossRef]
- Shahba, A.A.-W.; Mohsin, K.; Alanazi, F.K.; Abdel-Rahman, S.I. Optimization of self-nanoemulsifying formulations for weakly basic lipophilic drugs: Role of acidification and experimental design. Braz. J. Pharm. Sci. 2016, 52, 653–667. [Google Scholar] [CrossRef] [Green Version]
- Kulkarni, V.R.; Kazi, M.; Shahba, A.A.-W.; Radhanpuri, A.; Maniruzzaman, M. Three-Dimensional Printing of a Container Tablet: A New Paradigm for Multi-Drug-Containing Bioactive Self-Nanoemulsifying Drug-Delivery Systems (Bio-SNEDDSs). Pharmaceutics 2022, 14, 1082. [Google Scholar] [CrossRef]
- Aboul-Soud, M.A.M.; Ashour, A.E.; Challis, J.K.; Ahmed, A.F.; Kumar, A.; Nassrallah, A.; Alahmari, T.A.; Saquib, Q.; Siddiqui, M.A.; Al-Sheikh, Y.; et al. Biochemical and Molecular Investigation of In Vitro Antioxidant and Anticancer Activity Spectrum of Crude Extracts of Willow Leaves Salix safsaf. Plants 2020, 9, 1295. [Google Scholar] [CrossRef] [PubMed]
- Kazi, M.; Nasr, F.A.; Noman, O.; Alharbi, A.; Alqahtani, M.S.; Alanazi, F.K. Development, characterization optimization, and assessment of curcumin-loaded bioactive self-nanoemulsifying formulations and their inhibitory effects on human breast cancer MCF-7 cells. Pharmaceutics 2020, 12, 1107. [Google Scholar] [CrossRef] [PubMed]
- Shahba, A.A.; Alanazi, F.K.; Mohsin, K.; Abdel-Hamid, M. Stability Assessment of Cinnarizine in Self-Emulsifying Drug Delivery Systems. Lat. Am. J. Pharm. 2012, 31, 549–554. [Google Scholar]
- El-Laithy, H.M.; Basalious, E.B.; El-Hoseiny, B.M.; Adel, M.M. Novel self-nanoemulsifying self-nanosuspension (SNESNS) for enhancing oral bioavailability of diacerein: Simultaneous portal blood absorption and lymphatic delivery. Int. J. Pharm. 2015, 490, 146–154. [Google Scholar] [CrossRef]
- McClements, D.J. Nanoemulsions versus microemulsions: Terminology, differences, and similarities. Soft Matter 2012, 8, 1719–1729. [Google Scholar] [CrossRef]
- Solans, C.; Izquierdo, P.; Nolla, J.; Azemar, N.; Garcia-Celma, M.J. Nano-emulsions. Curr. Opin. Colloid Interface Sci. 2005, 10, 102–110. [Google Scholar] [CrossRef]
- Rehman, F.U.; Farid, A.; Shah, S.U.; Dar, M.J.; Rehman, A.U.; Ahmed, N.; Rashid, S.A.; Shaukat, I.; Shah, M.; Albadrani, G.M.; et al. Self-Emulsifying Drug Delivery Systems (SEDDS): Measuring Energy Dynamics to Determine Thermodynamic and Kinetic Stability. Pharmaceuticals 2022, 15, 1064. [Google Scholar] [CrossRef]
- Pouton, C.; Porter, C. Formulation of lipid-based delivery systems for oral administration: Materials, methods and strategies. Adv. Drug Deliv. Rev. 2008, 60, 625–637. [Google Scholar] [CrossRef]
- Li, Q.; Chen, F.; Liu, Y.; Yu, S.; Gai, X.; Ye, M.; Yang, X.; Pan, W. A novel albumin wrapped nanosuspension of meloxicam to improve inflammation-targeting effects. Int. J. Nanomed. 2018, 13, 4711–4725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahba, A.A.; Tashish, A.Y.; Alanazi, F.K.; Kazi, M. Combined Self-Nanoemulsifying and Solid Dispersion Systems Showed Enhanced Cinnarizine Release in Hypochlorhydria/Achlorhydria Dissolution Model. Pharmaceutics 2021, 13, 627. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Ghosh, S.; Kumar, P.; Basu, B.; Nagpal, K. Ellagic acid-loaded, tween 80-coated, chitosan nanoparticles as a promising therapeutic approach against breast cancer: In-vitro and in-vivo study. Life Sci. 2021, 284, 119927. [Google Scholar] [CrossRef] [PubMed]









| S. No | Chemical Constituents | RT (min) | Area | Quality |
|---|---|---|---|---|
| 1. | Trans Thujene | 6.07 | 38,250,124 | 91 |
| 2. | Alpha pinene Dimer | 6.1 | 8,300,185 | 97 |
| 3. | Alpha Thujene | 6.75 | 3,649,660 | 91 |
| 4. | Beta-Pinene | 6.86 | 7,601,772 | 97 |
| 5. | 4-isothyocyanato-1-butene | 6.97 | 1,825,185 | 86 |
| 6. | (+)-4-Carene | 7.47 | 863,913 | 96 |
| 7. | Para Cymenene | 7.66 | 99,930,937 | 94 |
| 8. | 1-Methyl-4-(1-methyl ethyl)-1,4 cyclohexadiene | 8.11 | 2,647,404 | 97 |
| 9. | Beta Terpinene | 8.72 | 3,070,595 | 55 |
| 10. | 1,3,4-trimethyl-3-cyclohexene-1-carboxaldehyde | 9.78 | 1,243,371 | 59 |
| 11. | Terpinen-4-ol | 10.08 | 1,670,144 | 94 |
| 12. | Trans-p-menthone | 10.36 | 1,732,947 | 99 |
| 13. | Thymoquinone | 11.19 | 105,710,772 | 78 |
| 14. | Isoborneol | 11.55 | 613,240 | 99 |
| 15. | Carvacrol | 11.82 | 8,961,583 | 80 |
| 16. | Longipinene | 12.53 | 4,604,900 | 90 |
| 17. | Spatulenol | 12.86 | 492,131 | 89 |
| 18. | Longifolene | 13.46 | 19,892,680 | 76 |
| 19. | Paeonol | 15.75 | 52,505,462 | 99 |
| 20. | (Z)6,(Z)9-Pentadecadien-1-ol | 17.08 | 982,331 | 58 |
| 21. | Gurjunene | 17.29 | 1,421,942 | 96 |
| 22. | Tetradecanoic acid | 18.22 | 7,059,132 | 99 |
| 23. | 1,2,3,4-tetrahydro-6-methoxy-1-salicyl-7-Isoquinolinol | 18.91 | 1,919,745 | 76 |
| 24. | Methyl ester of Hexadecanoic acid | 19.85 | 669,001 | 99 |
| 25. | 2-Methyl-5-methoxy-4H-pyran-4-one | 19.94 | 504,826 | 58 |
| 26. | cis-9-Hexadecenoic acid | 20.17 | 662,779 | 99 |
| 27. | n-Hexadecanoic acid | 20.82 | 296,221,560 | 95 |
| 28. | methyl ester of 9,12-Octadecadienoic acid | 21.5 | 2,553,881 | 91 |
| 29. | methyl ester of 11-Octadecenoic acid | 21.62 | 1,186,279 | 53 |
| 30. | 3,5-dimethyl-Cyclohexanol | 21.76 | 46,556,405 | 93 |
| 31. | Androstane-3,17-diol | 23.37 | 5,925,178 | 90 |
| 32. | 9,12-Octadecadienoic acid | 23.9 | 14,493,017 | 91 |
| 33. | 2-hydroxy-1ethyl ester 9,12Octadecadienoic acid | 24.55 | 5,442,419 | 96 |
| 34. | Erucic acid | 25.4 | 5,733,659 | 96 |
| 35. | 9,17-Octadecadienal | 26.37 | 2,041,292 | 96 |
| 36. | 2,6,10,15,19,23-hexamethyl-2,6,10,14,18,22-Tetracosahexaene | 27.49 | 2,119,364 | 98 |
| S. No | Chemical Constituents | RT | Area | Quality |
|---|---|---|---|---|
| 1. | 4-isothiocyanato-1-Butene | 6.96 | 769,459 | 86 |
| 2. | p-cymenene | 7.6 | 205,984 | 94 |
| 3. | 3,3,5-trimethyl-cis-Cyclohexanol | 10.13 | 125,880 | 91 |
| 4. | Heptadecane | 11.35 | 104,463 | 72 |
| 5. | Decane, 2,3,7-trimethyl- | 11.98 | 100,497 | 58 |
| 6. | Beta-Gurjunene | 13.44 | 74,890 | 64 |
| 7. | (2-isothiocyanatoethyl)-Benzene | 14.38 | 94,519 | 76 |
| 8. | Hexadecane | 14.57 | 139,678 | 90 |
| 9. | 2,4-bis(1,1-dimethylethyl)-Phenol | 14.95 | 107,702 | 96 |
| 10. | alpha,alpha’-Dihydroxy-m-diisopropylbenzene | 16.39 | 236,246 | 50 |
| 11. | n-Tetracosanol-1 | 17.04 | 81,178 | 72 |
| 12. | Cis-pinane | 18.93 | 300,212 | 91 |
| 13. | 9-Eicosyne | 19.2 | 77,787 | 64 |
| 14. | Phytol | 19.39 | 152,478 | 80 |
| 15. | Octacosane | 19.84 | 146,765 | 83 |
| 16. | 7,9-Di-tert-butyl-1-oxaspiro(4,5)deca-6,9-diene-2,8-dione | 19.92 | 136,232 | 98 |
| 17. | Palmitic acid | 20.35 | 5,948,720 | 99 |
| 18. | Methyl palmitate | 21.07 | 77,500 | 86 |
| 19. | methyl ester of 9,12-Octadecadienoic acid | 21.55 | 169,577 | 98 |
| 20. | 12-Methyl-E,E-2,13-octadecadien-1-ol | 21.67 | 185,487 | 53 |
| 21. | Cycloeicosane | 21.74 | 124,790 | 93 |
| 22. | 9,12-Octadecadienoic acid | 22.11 | 36,041,107 | 99 |
| 23. | Octadecanoic acid | 22.27 | 851,731 | 96 |
| 24. | 13-Tetradece-11-yn-1-ol | 24.39 | 144,138 | 60 |
| 25. | Methyl 9,12-heptadecadienoate | 24.44 | 185,487 | 94 |
| 26. | 2-octyl-Cyclopropaneoctanal | 24.66 | 107,616 | 92 |
| 27. | Butyl 9,12-octadecadienoate | 24.84 | 2,895,986 | 98 |
| 28. | 2-Methyl-Z,Z-3,13-octadecadienol | 25.04 | 415,487 | 91 |
| 29. | 9,17-Octadecadienal | 26.33 | 2,417,621 | 96 |
| 30. | cis,cis-7,10,-Hexadecadienal | 26.79 | 98,610 | 95 |
| 31. | Squalene | 27.46 | 1,133,348 | 96 |
| Distilled Water | 0.1 N HCl | Phosphate Buffer (pH 6.8) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 10 | 100 | 1000 | 10 | 100 | 1000 | 10 | 100 | 1000 | |
| F4 (initial) | Very Turbid | Turbid | Semi-transparent | Very Turbid | Turbid | Semi-transparent | Very Turbid | Turbid | Semi-transparent |
| F4 (after storage) | RPS | RPS | RPS | RPS | RPS | Stable as Semitransparent | RPS | RPS | Stable as Semitransparent |
| F5 (initial) | Very Turbid | Turbid | Semi-transparent | Very Turbid | Turbid | Semi-transparent | Very Turbid | Turbid | Semi-transparent |
| F5 (after storage) | RPS | RPS | RPS | RPS | RPS | Stable as Semi-transparent | RPS | RPS | Stable as Semi-transparent |
| Formulation | Centrifugation | Heat–Cool Cycles | Freeze–Thaw Cycles |
|---|---|---|---|
| F4 | Reversible Phase separation | Reversible Phase separation | Reversible Phase separation |
| F5 | Reversible Phase separation | Reversible Phase separation | Reversible Phase separation |
| No. | Formulation (%w/w/w) | Particle Size (nm) | PDI | Zeta Potential (mv) |
|---|---|---|---|---|
| F1 | FSO | >5000 | >1.00 | N/A |
| F2 | BSO | >5000 | >1.00 | N/A |
| F3 | ZRO | >5000 | >1.00 | N/A |
| F4 | FSO/I988/T80R (35/15/50) | 151.60 ± 1.51 | 0.329 ± 0.059 | −16.87 ± 0.55 |
| F5 | BSO/I988/T80R (35/15/50) | 247.03 ± 9.18 | 0.441 ± 0.038 | +28.73 ± 0.86 |
| No. | Formulation (%w/w/w) | Equilibrium Solubility (mg/g) | |
|---|---|---|---|
| BRB | RMV | ||
| F1 | FSO | 3.05 ± 0.09 | 3.17 ± 0.07 |
| F2 | BSO | 4.81 ± 0.08 | 5.90 ± 0.10 |
| F3 | ZRO | 4.22 ± 0.11 | 4.57 ± 0.05 |
| F4 | FSO/I988/T80R (35/15/50) | 6.21 ± 0.05 | 8.20 ± 0.18 |
| F5 | BSO/I988/T80R (35/15/50) | 7.04 ± 0.13 | 10.93 ± 0.07 |
| No. | Formulation (%w/w/w) | Viscosity (Cp) of Drug Free Formulations | Viscosity (Cp) of Drug Loaded Formulations |
|---|---|---|---|
| F4 | FSO/I988/T80R (35/15/50) | 0.717 ± 0.015 | 0.777 ± 0.015 |
| F5 | BSO/I988/T80R (35/15/50) | 0.693 ± 0.006 | 0.717 ± 0.006 |
| Name of Formulation | IC 50 Value (µg/mL) | ||
|---|---|---|---|
| Breast Cancer (MDA-MB-231) Cell Line (*) | Lung Cancer (A549) Cell Line (*) | Human Fibroblasts Cell Line | |
| FSO | NA# | NA# | NA# |
| BSO | 108.09 ± 6.42 a | 197.14 ± 2.5 a | 476.75 ± 38.94 a |
| ZRO | NA# | NA# | NA# |
| F4-loaded RMV (single drug) | 3.95 ± 0.02 b | 4.57 ± 0.42 b | 3.35 ± 0.87 b |
| F4-loaded BRB (single drug) | 2.24 ± 0.69 b | 3.6 ± 0.5 b | 4.88 ± 0.32 b |
| F4-Drug free systems | 4.14 ± 0.22 b | 5.78 ± 0.38 b* | 5.44 ± 0.24 b |
| Pure BRB | 11.1 ± 1.58 c | 15.85 ± 1.9 c | 21.92 ± 1.92 b |
| Pure RMV | 25.92 ± 3.0 d | 76.6 ± 4.05 d | NA# |
| F4-systems (combined RMV + BRB) | 4.2 ± 0.32 b | 5.06 ± 0.08 b | 5.04 ± 0.11 b |
| F5-Bio-SNEDDS (combined RMV + BRB) | 1.9 ± 0.19 b | 2.37 ± 0.22 b** | 3.05 ± 0.11 b |
| Formulation No. | FSO | BSO | ZRO | I988 | T80R | Total | Formulation Type |
|---|---|---|---|---|---|---|---|
| F1 | 100 | - | - | - | - | 100 | LFCS Type I (Oil only) |
| F2 | - | 100 | - | - | - | 100 | LFCS Type I (Oil only) |
| F3 | - | - | 100 | - | - | 100 | LFCS Type I (Oil only) |
| F4 | 35 | - | - | 15 | 50 | 100 | LFCS Type III Systems |
| F5 | - | 35 | - | 15 | 50 | 100 | LFCS Type III (SNEDDS) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kazi, M.; Alanazi, Y.; Kumar, A.; Shahba, A.A.-W.; Rizwan Ahamad, S.; Alghamdi, K.M. Oral Bioactive Self-Nanoemulsifying Drug Delivery Systems of Remdesivir and Baricitinib: A Paradigmatic Case of Drug Repositioning for Cancer Management. Molecules 2023, 28, 2237. https://doi.org/10.3390/molecules28052237
Kazi M, Alanazi Y, Kumar A, Shahba AA-W, Rizwan Ahamad S, Alghamdi KM. Oral Bioactive Self-Nanoemulsifying Drug Delivery Systems of Remdesivir and Baricitinib: A Paradigmatic Case of Drug Repositioning for Cancer Management. Molecules. 2023; 28(5):2237. https://doi.org/10.3390/molecules28052237
Chicago/Turabian StyleKazi, Mohsin, Yousef Alanazi, Ashok Kumar, Ahmad Abdul-Wahhab Shahba, Syed Rizwan Ahamad, and Khalid M. Alghamdi. 2023. "Oral Bioactive Self-Nanoemulsifying Drug Delivery Systems of Remdesivir and Baricitinib: A Paradigmatic Case of Drug Repositioning for Cancer Management" Molecules 28, no. 5: 2237. https://doi.org/10.3390/molecules28052237
APA StyleKazi, M., Alanazi, Y., Kumar, A., Shahba, A. A. -W., Rizwan Ahamad, S., & Alghamdi, K. M. (2023). Oral Bioactive Self-Nanoemulsifying Drug Delivery Systems of Remdesivir and Baricitinib: A Paradigmatic Case of Drug Repositioning for Cancer Management. Molecules, 28(5), 2237. https://doi.org/10.3390/molecules28052237