Cell Surface Markers in Colorectal Cancer Prognosis
Abstract
:1. Introduction
2. Tumour Stroma
3. Inflammation and Infiltrating Leukocytes
4. Cancer Cells
4.1. Tetraspanins and Potential Tetraspanin-Associated Proteins
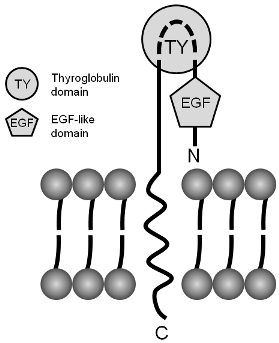
4.2. Epithelial-Specific Cell Adhesion Activation Molecule (EpCAM, TROP-1, CD326)
4.3. Mucins, Carbohydrates, Lectins
4.4. Carcinoembryonic Antigen (CEA) Family
4.5. Annexins
4.6. Claudins
4.7. Chemokine Receptors
4.8. Growth Factor Receptors
4.9. Death Receptors (DR) and Ligands
4.10. Major Histocompatibility Complex (MHC)
4.11. Other Protein Markers in CRC
5. Colorectal Cancer Stem Cells (CSC)
6. CRC Translational Proteomics Research
Acknowledgement
Abbreviations
| CEA | carcinoembryonic antigen |
| CD44v6 | CD44 variant 6 |
| CCR | chemokine receptor |
| CRC | colorectal cancer |
| CSC | colorectal cancer stem cell |
| CXCR | chemokine CXC motif receptor |
| DC | dendritic cells |
| 2D-DIGE | two-dimensional difference gel electrophoresis |
| DR | death receptor |
| EpCAM | epithelial-specific cell adhesion activation molecule |
| FoxP3 | forkhead box P3 |
| MHC | major histocompatibility complex |
| HLA | human leukocyte antigen |
| Met | hepatocyte growth factor receptor |
| MMP | matrix metalloproteinase |
| MMR | DNA mismatch repair |
| MSI | microsatellite instability |
| NK | natural killer |
| TAM | tumour-associated macrophage |
| TEM | tetraspanin-enriched membrane domains |
| TIL | tumour infiltrating lymphocyte |
| Treg | regulatory T-cell |
References
- Puppa, G; Sonzogni, A; Colombari, R; Pelosi, G. TNM staging system of colorectal carcinoma: A critical appraisal of challenging issues. Arch. Pathol. Lab. Med 2010, 134, 837–852. [Google Scholar]
- Zinkin, LD. A critical review of the classifications and staging of colorectal cancer. Dis. Colon. Rectum 1983, 26, 37–43. [Google Scholar]
- Compton, CC. Colorectal carcinoma: Diagnostic, prognostic, and molecular features. Mod. Pathol 2003, 16, 376–388. [Google Scholar]
- O’Connell, JB; Maggard, MA; Ko, CY. Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J. Natl. Cancer Inst 2004, 96, 1420–1425. [Google Scholar]
- Alfonso, P; Canamero, M; Fernandez-Carbonie, F; Nunez, A; Casal, JI. Proteome analysis of membrane fractions in colorectal carcinomas by using 2D-DIGE saturation labeling. J. Proteome Res 2008, 7, 4247–4255. [Google Scholar]
- Andre, M; Le Caer, JP; Greco, C; Planchon, S; El Nemer, W; Boucheix, C; Rubinstein, E; Chamot-Rooke, J; Le Naour, F. Proteomic analysis of the tetraspanin web using LC-ESI-MS/MS and MALDI-FTICR-MS. Proteomics 2006, 6, 1437–1449. [Google Scholar]
- Barderas, R; Babel, I; Casal, JI. Colorectal cancer proteomics, molecular characterization and biomarker discovery. Proteomics-Clin. Appl. Rev 2010, 4, 159–178. [Google Scholar]
- Friedman, DB; Hill, S; Keller, JW; Merchant, NB; Levy, SE; Coffey, RJ; Caprioli, RM. Proteome analysis of human colon cancer by two-dimensional difference gel electrophoresis and mass spectrometry. Proteomics 2004, 4, 793–811. [Google Scholar]
- Gil-Bazo, I. Novel translational strategies in colorectal Cancer Res.earch. World J. Gastroenterol 2007, 13, 5902–5910. [Google Scholar]
- Habermann, JK; Bader, FG; Franke, C; Zimmermann, K; Gemoll, T; Fritzsche, B; Ried, T; Auer, G; Bruch, HP; Roblick, UJ. From the genome to the proteome--biomarkers in colorectal cancer. Langenbecks Arch. Surg 2008, 393, 93–104. [Google Scholar]
- Jimenez, CR; Knol, JC; Meijer, GA; Fijneman, RJ. Proteomics of colorectal cancer: Overview of discovery studies and identification of commonly identified cancer-associated proteins and candidate CRC serum markers. J Proteomics 2010, 73, 1873–1895. [Google Scholar]
- Luque-Garcia, JL; Martinez-Torrecuadrada, JL; Epifano, C; Canamero, M; Babel, I; Casal, JI. Differential protein expression on the cell surface of colorectal cancer cells associated to tumor metastasis. Proteomics 2010, 10, 940–952. [Google Scholar]
- Hlubek, F; Brabletz, T; Budczies, J; Pfeiffer, S; Jung, A; Kirchner, T. Heterogeneous expression of Wnt/beta-catenin target genes within colorectal cancer. Int. J Cancer 2007, 121, 1941–1948. [Google Scholar]
- Li, JQ; Xu, BJ; Shakhtour, B; Deane, N; Merchant, N; Heslin, MJ; Washington, K; Coffey, RJ; Beauchamp, RD; Shyr, Y; Billheimer, D. Variability of in situ proteomic profiling and implications for study design in colorectal tumors. Int. J. Oncol 2007, 31, 103–111. [Google Scholar]
- Ahn, YH; Lee, JY; Kim, YS; Ko, JH; Yoo, JS. Quantitative analysis of an aberrant glycoform of TIMP1 from colon cancer serum by L-PHA-enrichment and SISCAPA with MRM mass spectrometry. J. Proteome Res 2009, 8, 4216–4224. [Google Scholar]
- Rho, JH; Qin, S; Wang, JY; Roehrl, MH. Proteomic expression analysis of surgical human colorectal cancer tissues: Up-regulation of PSB7, PRDX1, and SRP9 and hypoxic adaptation in cancer. J. Proteome Res 2008, 7, 2959–2572. [Google Scholar]
- Petrak, J; Ivanek, R; Toman, O; Cmejla, R; Cmejlova, J; Vyoral, D; Zivny, J; Vulpe, CD. Deja vu in proteomics. A hit parade of repeatedly identified differentially expressed proteins. Proteomics 2008, 8, 1744–1749. [Google Scholar]
- Wang, P; Bouwman, FG; Mariman, EC. Generally detected proteins in comparative proteomics--a matter of cellular stress response? Proteomics 2009, 9, 2955–2566. [Google Scholar]
- Yamasaki, M; Takemasa, I; Komori, T; Watanabe, S; Sekimoto, M; Doki, Y; Matsubara, K; Monden, M. The gene expression profile represents the molecular nature of liver metastasis in colorectal cancer. Int. J. Oncol 2007, 30, 129–138. [Google Scholar]
- Eschrich, S; Yang, I; Bloom, G; Kwong, KY; Boulware, D; Cantor, A; Coppola, D; Kruhoffer, M; Aaltonen, L; Orntoft, TF; Quackenbush, J; Yeatman, TJ. Molecular staging for survival prediction of colorectal cancer patients. J. Clin. Oncol 2005, 23, 3526–3535. [Google Scholar]
- Ellmark, P; Belov, L; Huang, P; Lee, CS; Solomon, MJ; Morgan, DK; Christopherson, RI. Multiplex detection of surface molecules on colorectal cancers. Proteomics 2006, 6, 1791–1802. [Google Scholar]
- Zhou, J; Belov, L; Huang, PY; Shin, JS; Solomon, MJ; Chapuis, PH; Bokey, L; Chan, C; Clarke, C; Clarke, SJ; Christopherson, RI. Surface antigen profiling of colorectal cancer using antibody microarrays with fluorescence multiplexing. J. Immunol Methods 2010, 355, 40–51. [Google Scholar]
- Belov, L; Mulligan, SP; Barber, N; Woolfson, A; Scott, M; Stoner, K; Chrisp, JS; Sewell, WA; Bradstock, KF; Bendall, L; Pascovici, DS; Thomas, M; Erber, W; Huang, P; Sartor, M; Young, GA; Wiley, JS; Juneja, S; Wierda, WG; Green, AR; Keating, MJ; Christopherson, RI. Analysis of human leukaemias and lymphomas using extensive immunophenotypes from an antibody microarray. Br. J. Haematol 2006, 135, 184–197. [Google Scholar]
- Moyret-Lalle, C; Falette, N; Grelier, G; Puisieux, A. Tumour genomics: An unstable landscape. Bull Cancer 2008, 95, 923–930. [Google Scholar]
- McAllister, SS; Weinberg, RA. Tumor-Host Interactions: A Far-Reaching Relationship. J. Clin. Oncol 2010, 28, 4022–4028. [Google Scholar]
- Kaufman, KL; Mactier, S; Kohnke, P; Christopherson, RI. Davis, JR, Ed.; Cell surface oncoproteomics: Cancer biomarker discovery and clinical applications. In Oncoproteins: Types and Detection; Nova Science Publishes, Inc: Hauppauge, NY, USA, 2010. [Google Scholar]
- Leth-Larsen, R; Lund, RR; Ditzel, HJ. Plasma membrane proteomics and its application in clinical cancer biomarker discovery. Mol Cell Proteomics 2010, 9, 1369–1382. [Google Scholar]
- Baldus, SE; Schaefer, KL; Engers, R; Hartleb, D; Stoecklein, NH; Gabbert, HE. Prevalence and heterogeneity of KRAS, BRAF, and PIK3CA mutations in primary colorectal adenocarcinomas and their corresponding metastases. Clin. Cancer Res 2010, 16, 790–799. [Google Scholar]
- Fang, JY; Richardson, BC. The MAPK signalling pathways and colorectal cancer. Lancet Oncol 2005, 6, 322–327. [Google Scholar]
- Markowitz, SD; Bertagnolli, MM. Molecular origins of cancer: Molecular basis of colorectal cancer. N. Engl. J. Med 2009, 361, 2449–2460. [Google Scholar]
- Saif, MW; Chu, E. Biology of colorectal cancer. Cancer J 2010, 16, 196–201. [Google Scholar]
- Sancho, E; Batlle, E; Clevers, H. Signaling pathways in intestinal development and cancer. 2004, 20, 695–723. [Google Scholar]
- Wu, CC; Yates, JR, III. The application of mass spectrometry to membrane proteomics. Nat. Biotechnol 2003, 21, 262–267. [Google Scholar]
- Bird, NC; Mangnall, D; Majeed, AW. Biology of colorectal liver metastases: A review. J. Surg. Oncol 2006, 94, 68–80. [Google Scholar]
- Haier, J; Nasralla, M; Nicolson, GL. Cell surface molecules and their prognostic values in assessing colorectal carcinomas. Ann. Surg 2000, 231, 11–24. [Google Scholar]
- De Wever, O; Mareel, M. Role of tissue stroma in cancer cell invasion. J. Pathol 2003, 200, 429–447. [Google Scholar]
- Sund, M; Kalluri, R. Tumor stroma derived biomarkers in cancer. Cancer Metastasis Rev 2009, 28, 177–183. [Google Scholar]
- Bacman, D; Merkel, S; Croner, R; Papadopoulos, T; Brueckl, W; Dimmler, A. TGF-beta receptor 2 downregulation in tumour-associated stroma worsens prognosis and high-grade tumours show more tumour-associated macrophages and lower TGF-beta1 expression in colon carcinoma: A retrospective study. BMC Cancer 2007, 7, 156. [Google Scholar]
- Kitadai, Y; Sasaki, T; Kuwai, T; Nakamura, T; Bucana, CD; Fidler, IJ. Targeting the expression of platelet-derived growth factor receptor by reactive stroma inhibits growth and metastasis of human colon carcinoma. Am. J. Pathol 2006, 169, 2054–2065. [Google Scholar]
- Kitadai, Y; Sasaki, T; Kuwai, T; Nakamura, T; Bucana, CD; Hamilton, SR; Fidler, IJ. Expression of activated platelet-derived growth factor receptor in stromal cells of human colon carcinomas is associated with metastatic potential. Int. J Cancer 2006, 119, 2567–2574. [Google Scholar]
- Saigusa, S; Toiyama, Y; Tanaka, K; Yokoe, T; Okugawa, Y; Kawamoto, A; Yasuda, H; Inoue, Y; Miki, C; Kusunoki, M. Stromal CXCR4 and CXCL12 expression is associated with distant recurrence and poor prognosis in rectal cancer after chemoradiotherapy. Ann. Surg. Oncol 2010, 17, 2051–2058. [Google Scholar]
- Henry, LR; Lee, HO; Lee, JS; Klein-Szanto, A; Watts, P; Ross, EA; Chen, WT; Cheng, JD. Clinical implications of fibroblast activation protein in patients with colon cancer. Clin. Cancer Res 2007, 13, 1736–1741. [Google Scholar]
- Saito, K; Takeha, S; Shiba, K; Matsuno, S; Sorsa, T; Nagura, H; Ohtani, H. Clinicopathologic significance of urokinase receptor- and MMP-9-positive stromal cells in human colorectal cancer: Functional multiplicity of matrix degradation on hematogenous metastasis. Int. J Cancer 2000, 86, 24–29. [Google Scholar]
- Mesker, WE; Liefers, GJ; Junggeburt, JM; van Pelt, GW; Alberici, P; Kuppen, PJ; Miranda, NF; van Leeuwen, KA; Morreau, H; Szuhai, K; Tollenaar, RA; Tanke, HJ. Presence of a high amount of stroma and downregulation of SMAD4 predict for worse survival for stage I-II colon cancer patients. Cell Oncol 2009, 31, 169–178. [Google Scholar]
- Ogawa, H; Iwaya, K; Izumi, M; Kuroda, M; Serizawa, H; Koyanagi, Y; Mukai, K. Expression of CD10 by stromal cells during colorectal tumor development. Hum. Pathol 2002, 33, 806–811. [Google Scholar]
- Miyanaga, K; Kato, Y; Nakamura, T; Matsumura, M; Amaya, H; Horiuchi, T; Chiba, Y; Tanaka, K. Expression and role of thrombospondin-1 in colorectal cancer. AntiCancer Res 2002, 22, 3941–3948. [Google Scholar]
- Kaio, E; Tanaka, S; Oka, S; Hiyama, T; Kitadai, Y; Haruma, K; Chayama, K. Clinical significance of thrombospondin-1 expression in relation to vascular endothelial growth factor and interleukin-10 expression at the deepest invasive tumor site of advanced colorectal carcinoma. Int. J. Oncol 2003, 23, 901–911. [Google Scholar]
- Maeda, K; Nishiguchi, Y; Kang, SM; Yashiro, M; Onoda, N; Sawada, T; Ishikawa, T; Hirakawa, K. Expression of thrombospondin-1 inversely correlated with tumor vascularity and hematogenous metastasis in colon cancer. Oncol. Rep 2001, 8, 763–766. [Google Scholar]
- Maeda, K; Nishiguchi, Y; Yashiro, M; Yamada, S; Onoda, N; Sawada, T; Kang, SM; Hirakawa, K. Expression of vascular endothelial growth factor and thrombospondin-1 in colorectal carcinoma. Int. J. Mol. Med 2000, 5, 373–378. [Google Scholar]
- Roberts, DD. Regulation of tumor growth and metastasis by thrombospondin-1. FASEB J 1996, 10, 1183–1191. [Google Scholar]
- Sutton, CD; O’Byrne, K; Goddard, JC; Marshall, LJ; Jones, L; Garcea, G; Dennison, AR; Poston, G; Lloyd, DM; Berry, DP. Expression of thrombospondin-1 in resected colorectal liver metastases predicts poor prognosis. Clin. Cancer Res 2005, 11, 6567–6573. [Google Scholar]
- Forssell, J; Oberg, A; Henriksson, ML; Stenling, R; Jung, A; Palmqvist, R. High macrophage infiltration along the tumor front correlates with improved survival in colon cancer. Clin. Cancer Res 2007, 13, 1472–1479. [Google Scholar]
- Klintrup, K; Makinen, JM; Kauppila, S; Vare, PO; Melkko, J; Tuominen, H; Tuppurainen, K; Makela, J; Karttunen, TJ; Makinen, MJ. Inflammation and prognosis in colorectal cancer. Eur. J Cancer 2005, 41, 2645–2654. [Google Scholar]
- Jedinak, A; Dudhgaonkar, S; Sliva, D. Activated macrophages induce metastatic behavior of colon cancer cells. Immunobiology 2010, 215, 242–249. [Google Scholar]
- Kaler, P; Galea, V; Augenlicht, L; Klampfer, L. Tumor associated macrophages protect colon cancer cells from TRAIL-induced apoptosis through IL-1beta-dependent stabilization of Snail in tumor cells. PLoS One 2010, 5, e11700. [Google Scholar]
- Yuan, A; Chen, JJ; Yang, PC. Pathophysiology of tumor-associated macrophages. Adv Clin. Chem 2008, 45, 199–223. [Google Scholar]
- Jedinak, A; Dudhgaonkar, S; Sliva, D. Activated macrophages induce metastatic behavior of colon cancer cells. Immunobiology 2010, 215, 242–249. [Google Scholar]
- Sandel, MH; Dadabayev, AR; Menon, AG; Morreau, H; Melief, CJ; Offringa, R; van der Burg, SH; Janssen-van Rhijn, CM; Ensink, NG; Tollenaar, RA; van de Velde, CJ; Kuppen, PJ. Prognostic value of tumor-infiltrating dendritic cells in colorectal cancer: Role of maturation status and intratumoral localization. Clin. Cancer Res 2005, 11, 2576–2582. [Google Scholar]
- Camus, M; Tosolini, M; Mlecnik, B; Pages, F; Kirilovsky, A; Berger, A; Costes, A; Bindea, G; Charoentong, P; Bruneval, P; Trajanoski, Z; Fridman, WH; Galon, J. Coordination of intratumoral immune reaction and human colorectal cancer recurrence. Cancer Res 2009, 69, 2685–2693. [Google Scholar]
- Nagorsen, D; Voigt, S; Berg, E; Stein, H; Thiel, E; Loddenkemper, C. Tumor-infiltrating macrophages and dendritic cells in human colorectal cancer: Relation to local regulatory T cells, systemic T-cell response against tumor-associated antigens and survival. J. Transl. Med 2007, 5, 62. [Google Scholar]
- Adams, H; Tzankov, A; Lugli, A; Zlobec, I. New time-dependent approach to analyse the prognostic significance of immunohistochemical biomarkers in colon cancer and diffuse large B-cell lymphoma. J. Clin. Pathol 2009, 62, 986–997. [Google Scholar]
- Jass, JR; Ajioka, Y; Allen, JP; Chan, YF; Cohen, RJ; Nixon, JM; Radojkovic, M; Restall, AP; Stables, SR; Zwi, LJ. Assessment of invasive growth pattern and lymphocytic infiltration in colorectal cancer. Histopathology 1996, 28, 543–548. [Google Scholar]
- Katz, SC; Pillarisetty, V; Bamboat, ZM; Shia, J; Hedvat, C; Gonen, M; Jarnagin, W; Fong, Y; Blumgart, L; D’Angelica, M; DeMatteo, RP. T cell infiltrate predicts long-term survival following resection of colorectal cancer liver metastases. Ann. Surg. Oncol 2009, 16, 2524–2530. [Google Scholar]
- Ohtani, H. Focus on TILs: Prognostic significance of tumor infiltrating lymphocytes in human colorectal cancer. Cancer Immun 2007, 7, 4. [Google Scholar]
- Galon, J; Costes, A; Sanchez-Cabo, F; Kirilovsky, A; Mlecnik, B; Lagorce-Pages, C; Tosolini, M; Camus, M; Berger, A; Wind, P; Zinzindohoue, F; Bruneval, P; Cugnenc, PH; Trajanoski, Z; Fridman, WH; Pages, F. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 2006, 313, 1960–1964. [Google Scholar]
- Lee, WS; Park, S; Lee, WY; Yun, SH; Chun, HK. Clinical impact of tumor-infiltrating lymphocytes for survival in stage II colon cancer. Cancer 2010, 116, 5188–5199. [Google Scholar]
- Naito, Y; Saito, K; Shiiba, K; Ohuchi, A; Saigenji, K; Nagura, H; Ohtani, H. CD8+ T cells infiltrated within cancer cell nests as a prognostic factor in human colorectal cancer. Cancer Res 1998, 58, 3491–3494. [Google Scholar]
- Pages, F; Galon, J; Dieu-Nosjean, MC; Tartour, E; Sautes-Fridman, C; Fridman, WH. Immune infiltration in human tumors: A prognostic factor that should not be ignored. Oncogene 2010, 29, 1093–1102. [Google Scholar]
- Strater, J; Herter, I; Merkel, G; Hinz, U; Weitz, J; Moller, P. Expression and prognostic significance of APAF-1, caspase-8 and caspase-9 in stage II/III colon carcinoma: Caspase-8 and caspase-9 is associated with poor prognosis. Int. J Cancer 2010, 127, 873–880. [Google Scholar]
- Deschoolmeester, V; Baay, M; Specenier, P; Lardon, F; Vermorken, JB. A review of the most promising biomarkers in colorectal cancer: One step closer to targeted therapy. Oncologist 2010, 15, 699–731. [Google Scholar]
- Galon, J; Fridman, WH; Pages, F. The adaptive immunologic microenvironment in colorectal cancer: A novel perspective. Cancer Res 2007, 67, 1883–1886. [Google Scholar]
- Halama, N; Michel, S; Kloor, M; Zoernig, I; Pommerencke, T; von Knebel Doeberitz, M; Schirmacher, P; Weitz, J; Grabe, N; Jager, D. The localization and density of immune cells in primary tumors of human metastatic colorectal cancer shows an association with response to chemotherapy. Cancer Immun 2009, 9, 1. [Google Scholar]
- Pages, F; Galon, J; Fridman, WH. The essential role of the in situ immune reaction in human colorectal cancer. J. Leukoc Biol 2008, 84, 981–987. [Google Scholar]
- Simpson, JA; Al-Attar, A; Watson, NF; Scholefield, JH; Ilyas, M; Durrant, LG. Intratumoral T cell infiltration, MHC class I and STAT1 as biomarkers of good prognosis in colorectal cancer. Gut 2010, 59, 926–933. [Google Scholar]
- Laghi, L; Bianchi, P; Miranda, E; Balladore, E; Pacetti, V; Grizzi, F; Allavena, P; Torri, V; Repici, A; Santoro, A; Mantovani, A; Roncalli, M; Malesci, A. CD3+ cells at the invasive margin of deeply invading (pT3-T4) colorectal cancer and risk of post-surgical metastasis: A longitudinal study. Lancet Oncol 2009, 10, 877–884. [Google Scholar]
- Diederichsen, AC; Hjelmborg, JB; Christensen, PB; Zeuthen, J; Fenger, C. Prognostic value of the CD4+/CD8+ ratio of tumour infiltrating lymphocytes in colorectal cancer and HLA-DR expression on tumour cells. Cancer Immunol. Immunother 2003, 52, 423–428. [Google Scholar]
- Dolcetti, R; Viel, A; Doglioni, C; Russo, A; Guidoboni, M; Capozzi, E; Vecchiato, N; Macri, E; Fornasarig, M; Boiocchi, M. High prevalence of activated intraepithelial cytotoxic T lymphocytes and increased neoplastic cell apoptosis in colorectal carcinomas with microsatellite instability. Am. J. Pathol 1999, 154, 1805–1813. [Google Scholar]
- Prall, F; Duhrkop, T; Weirich, V; Ostwald, C; Lenz, P; Nizze, H; Barten, M. Prognostic role of CD8+ tumor-infiltrating lymphocytes in stage III colorectal cancer with and without microsatellite instability. Hum. Pathol 2004, 35, 808–816. [Google Scholar]
- Clark, AJ; Barnetson, R; Farrington, SM; Dunlop, MG. Prognosis in DNA mismatch repair deficient colorectal cancer: Are all MSI tumours equivalent? Fam Cancer 2004, 3, 85–91. [Google Scholar]
- Menon, AG; Janssen-van Rhijn, CM; Morreau, H; Putter, H; Tollenaar, RA; van de Velde, CJ; Fleuren, GJ; Kuppen, PJ. Immune system and prognosis in colorectal cancer: A detailed immunohistochemical analysis. Lab. Invest 2004, 84, 493–501. [Google Scholar]
- Nussler, NC; Strange, BJ; Petzold, M; Nussler, AK; Glanemann, M; Guckelberger, O. Reduced NK-cell activity in patients with metastatic colon cancer. EXCLI J 2007, 6, 1–9. [Google Scholar]
- Koch, M; Beckhove, P; Op den Winkel, J; Autenrieth, D; Wagner, P; Nummer, D; Specht, S; Antolovic, D; Galindo, L; Schmitz-Winnenthal, FH; Schirrmacher, V; Buchler, MW; Weitz, J. Tumor infiltrating T lymphocytes in colorectal cancer: Tumor-selective activation and cytotoxic activity in situ. Ann. Surg 2006, 244, 986–992. [Google Scholar]
- Salama, P; Phillips, M; Grieu, F; Morris, M; Zeps, N; Joseph, D; Platell, C; Iacopetta, B. Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J. Clin. Oncol 2009, 27, 186–192. [Google Scholar]
- Kitayama, J; Nagawa, H; Nakayama, H; Tuno, N; Shibata, Y; Muto, T. Functional expression of beta1 and beta2 integrins on tumor infiltrating lymphocytes (TILs) in colorectal cancer. J. Gastroenterol 1999, 34, 327–333. [Google Scholar]
- Kruger, K; Buning, C; Schriever, F. Activated T lymphocytes bind in situ to stromal tissue of colon carcinoma but lack adhesion to tumor cells. Eur. J. Immunol 2001, 31, 138–145. [Google Scholar]
- Berndt, U; Philipsen, L; Bartsch, S; Wiedenmann, B; Baumgart, DC; Hammerle, M; Sturm, A. Systematic high-content proteomic analysis reveals substantial immunologic changes in colorectal cancer. Cancer Res 2008, 68, 880–888. [Google Scholar]
- Diederichsen, AC; Zeuthen, J; Christensen, PB; Kristensen, T. Characterisation of tumour infiltrating lymphocytes and correlations with immunological surface molecules in colorectal cancer. Eur. J Cancer 1999, 35, 721–726. [Google Scholar]
- Sinicrope, FA; Rego, RL; Ansell, SM; Knutson, KL; Foster, NR; Sargent, DJ. Intraepithelial effector (CD3+)/regulatory (FoxP3+) T-cell ratio predicts a clinical outcome of human colon carcinoma. Gastroenterology 2009, 137, 1270–1279. [Google Scholar]
- Suzuki, H; Chikazawa, N; Tasaka, T; Wada, J; Yamasaki, A; Kitaura, Y; Sozaki, M; Tanaka, M; Onishi, H; Morisaki, T; Katano, M. Intratumoral CD8(+) T/FOXP3 (+) cell ratio is a predictive marker for survival in patients with colorectal cancer. Cancer Immunol. Immunother 2010, 59, 653–661. [Google Scholar]
- Correale, P; Rotundo, MS; Del Vecchio, MT; Remondo, C; Migali, C; Ginanneschi, C; Tsang, KY; Licchetta, A; Mannucci, S; Loiacono, L; Tassone, P; Francini, G; Tagliaferri, P. Regulatory (FoxP3+) T-cell tumor infiltration is a favorable prognostic factor in advanced colon cancer patients undergoing chemo or chemoimmunotherapy. J. Immunother 2010, 33, 435–441. [Google Scholar]
- Frey, DM; Droeser, RA; Viehl, CT; Zlobec, I; Lugli, A; Zingg, U; Oertli, D; Kettelhack, C; Terracciano, L; Tornillo, L. High frequency of tumor-infiltrating FOXP3(+) regulatory T cells predicts improved survival in mismatch repair-proficient colorectal cancer patients. Int. J Cancer 2010, 126, 2635–2643. [Google Scholar]
- Hashida, H; Takabayashi, A; Tokuhara, T; Hattori, N; Taki, T; Hasegawa, H; Satoh, S; Kobayashi, N; Yamaoka, Y; Miyake, M. Clinical significance of transmembrane 4 superfamily in colon cancer. Br. J Cancer 2003, 89, 158–167. [Google Scholar]
- Le Naour, F; Andre, M; Boucheix, C; Rubinstein, E. Membrane microdomains and proteomics: Lessons from tetraspanin microdomains and comparison with lipid rafts. Proteomics 2006, 6, 6447–6454. [Google Scholar]
- Le Naour, F; Andre, M; Greco, C; Billard, M; Sordat, B; Emile, JF; Lanza, F; Boucheix, C; Rubinstein, E. Profiling of the tetraspanin web of human colon cancer cells. Mol Cell Proteomics 2006, 5, 845–857. [Google Scholar]
- Yanez-Mo, M; Barreiro, O; Gordon-Alonso, M; Sala-Valdes, M; Sanchez-Madrid, F. Tetraspanin-enriched microdomains: A functional unit in cell plasma membranes. Trends Cell Biol 2009, 19, 434–446. [Google Scholar]
- Zoller, M. Gastrointestinal tumors: Metastasis and tetraspanins. Z Gastroenterol 2006, 44, 573–586. [Google Scholar]
- Mori, M; Mimori, K; Shiraishi, T; Haraguchi, M; Ueo, H; Barnard, GF; Akiyoshi, T. Motility related protein 1 (MRP1/CD9) expression in colon cancer. Clin. Cancer Res 1998, 4, 1507–1510. [Google Scholar]
- El-Bahrawy, M; Poulsom, R; Rowan, AJ; Tomlinson, IT; Alison, MR. Characterization of the E-cadherin/catenin complex in colorectal carcinoma cell lines. Int. J. Exp. Pathol 2004, 85, 65–74. [Google Scholar]
- Boo, YJ; Park, JM; Kim, J; Chae, YS; Min, BW; Um, JW; Moon, HY. L1 expression as a marker for poor prognosis, tumor progression, and short survival in patients with colorectal cancer. Ann. Surg. Oncol 2007, 14, 1703–1711. [Google Scholar]
- Mohri, Y. Prognostic significance of E-cadherin expression in human colorectal cancer tissue. Surg Today 1997, 27, 606–612. [Google Scholar]
- Tsanou, E; Peschos, D; Batistatou, A; Charalabopoulos, A; Charalabopoulos, K. The E-cadherin adhesion molecule and colorectal cancer. A global literature approach. AntiCancer Res 2008, 28, 3815–3826. [Google Scholar]
- Hayashida, Y; Honda, K; Idogawa, M; Ino, Y; Ono, M; Tsuchida, A; Aoki, T; Hirohashi, S; Yamada, T. E-cadherin regulates the association between beta-catenin and actinin-4. Cancer Res 2005, 65, 8836–8845. [Google Scholar]
- Wanitsuwan, W; Kanngurn, S; Boonpipattanapong, T; Sangthong, R; Sangkhathat, S. Overall expression of beta-catenin outperforms its nuclear accumulation in predicting outcomes of colorectal cancers. World J. Gastroenterol 2008, 14, 6052–6059. [Google Scholar]
- Fang, QX; Lu, LZ; Yang, B; Zhao, ZS; Wu, Y; Zheng, XC. L1, beta-catenin, and E-cadherin expression in patients with colorectal cancer: Correlation with clinicopathologic features and its prognostic significance. J. Surg. Oncol 2010, 102, 433–442. [Google Scholar]
- Hashida, H; Takabayashi, A; Tokuhara, T; Taki, T; Kondo, K; Kohno, N; Yamaoka, Y; Miyake, M. Integrin alpha3 expression as a prognostic factor in colon cancer: Association with MRP-1/CD9 and KAI1/CD82. Int. J Cancer 2002, 97, 518–525. [Google Scholar]
- Fujita, S; Watanabe, M; Kubota, T; Teramoto, T; Kitajima, M. Alteration of expression in integrin beta 1-subunit correlates with invasion and metastasis in colorectal cancer. Cancer Lett 1995, 91, 145–149. [Google Scholar]
- Gao, XQ; Han, JX; Xu, ZF; Zhang, WD; Zhang, HN; Huang, HY. Identification of the differential expressive tumor associated genes in rectal cancers by cDNA microarray. World J. Gastroenterol 2007, 13, 341–348. [Google Scholar]
- Okazaki, K; Nakayama, Y; Shibao, K; Hirata, K; Nagata, N; Itoh, H. Enhancement of metastatic activity of colon cancer as influenced by expression of cell surface antigens. J. Surg. Res 1998, 78, 78–84. [Google Scholar]
- Herlevsen, M; Schmidt, DS; Miyazaki, K; Zoller, M. The association of the tetraspanin D6.1A with the alpha6beta4 integrin supports cell motility and liver metastasis formation. J. Cell Sci 2003, 116, 4373–4390. [Google Scholar]
- Mulder, JW; Kruyt, PM; Sewnath, M; Oosting, J; Seldenrijk, CA; Weidema, WF; Offerhaus, GJ; Pals, ST. Colorectal cancer prognosis and expression of exon-v6-containing CD44 proteins. Lancet 1994, 344, 1470–1472. [Google Scholar]
- Ropponen, KM; Eskelinen, MJ; Lipponen, PK; Alhava, E; Kosma, VM. Expression of CD44 and variant proteins in human colorectal cancer and its relevance for prognosis. Scand. J. Gastroenterol 1998, 33, 301–309. [Google Scholar]
- Vizoso, FJ; Fernandez, JC; Corte, MD; Bongera, M; Gava, R; Allende, MT; Garcia-Muniz, JL; Garcia-Moran, M. Expression and clinical significance of CD44V5 and CD44V6 in resectable colorectal cancer. J. Cancer Res. Clin. Oncol 2004, 130, 679–686. [Google Scholar]
- Ngan, CY; Yamamoto, H; Seshimo, I; Ezumi, K; Terayama, M; Hemmi, H; Takemasa, I; Ikeda, M; Sekimoto, M; Monden, M. A multivariate analysis of adhesion molecules expression in assessment of colorectal cancer. J. Surg. Oncol 2007, 95, 652–662. [Google Scholar]
- Kikuchi, R; Noguchi, T; Takeno, S; Kubo, N; Uchida, Y. Immunohistochemical detection of membrane-type-1-matrix metalloproteinase in colorectal carcinoma. Br. J Cancer 2000, 83, 215–218. [Google Scholar]
- Malhotra, S; Newman, E; Eisenberg, D; Scholes, J; Wieczorek, R; Mignatti, P; Shamamian, P. Increased membrane type 1 matrix metalloproteinase expression from adenoma to colon cancer: A possible mechanism of neoplastic progression. Dis. Colon. Rectum 2002, 45, 537–543. [Google Scholar]
- Shiomi, T; Okada, Y. MT1-MMP and MMP-7 in invasion and metastasis of human cancers. Cancer Metastasis Rev 2003, 22, 145–152. [Google Scholar]
- Mulder, WM; Stern, PL; Stukart, MJ; de Windt, E; Butzelaar, RM; Meijer, S; Ader, HJ; Claessen, AM; Vermorken, JB; Meijer, CJ; Wagstaff, J; Scheper, RJ; Bloemena, E. Low intercellular adhesion molecule 1 and high 5T4 expression on tumor cells correlate with reduced disease-free survival in colorectal carcinoma patients. Clin. Cancer Res 1997, 3, 1923–1930. [Google Scholar]
- Maeda, K; Kang, SM; Sawada, T; Nishiguchi, Y; Yashiro, M; Ogawa, Y; Ohira, M; Ishikawa, T; Hirakawa, YSCK. Expression of intercellular adhesion molecule-1 and prognosis in colorectal cancer. Oncol. Rep 2002, 9, 511–514. [Google Scholar]
- Chaudry, MA; Sales, K; Ruf, P; Lindhofer, H; Winslet, MC. EpCAM an immunotherapeutic target for gastrointestinal malignancy: Current experience and future challenges. Br. J Cancer 2007, 96, 1013–1019. [Google Scholar]
- Gosens, MJ; van Kempen, LC; van de Velde, CJ; van Krieken, JH; Nagtegaal, ID. Loss of membranous Ep-CAM in budding colorectal carcinoma cells. Mod. Pathol 2007, 20, 221–232. [Google Scholar]
- Baeuerle, PA; Gires, O. EpCAM (CD326) finding its role in cancer. Br. J Cancer 2007, 96, 417–423. [Google Scholar]
- Munz, M; Baeuerle, PA; Gires, O. The emerging role of EpCAM in cancer and stem cell signaling. Cancer Res 2009, 69, 5627–5629. [Google Scholar]
- Shiah, S-G; Tai, K-Y; Wu, C-W. Epigenetic regulation of EpCAM in tumor invasion and metastasis. J. Cancer Mol 2008, 3, 165–168. [Google Scholar]
- Trzpis, M; McLaughlin, PM; de Leij, LM; Harmsen, MC. Epithelial cell adhesion molecule: More than a carcinoma marker and adhesion molecule. Am. J. Pathol 2007, 171, 386–395. [Google Scholar]
- Winter, MJ; Nagtegaal, ID; van Krieken, JH; Litvinov, SV. The epithelial cell adhesion molecule (Ep-CAM) as a morphoregulatory molecule is a tool in surgical pathology. Am. J. Pathol 2003, 163, 2139–2148. [Google Scholar]
- Ohmachi, T; Tanaka, F; Mimori, K; Inoue, H; Yanaga, K; Mori, M. Clinical significance of TROP2 expression in colorectal cancer. Clin. Cancer Res 2006, 12, 3057–3063. [Google Scholar]
- Ziegler, A; Heidenreich, R; Braumuller, H; Wolburg, H; Weidemann, S; Mocikat, R; Rocken, M. EpCAM, a human tumor-associated antigen promotes Th2 development and tumor immune evasion. Blood 2009, 113, 3494–3502. [Google Scholar]
- Rao, CG; Chianese, D; Doyle, GV; Miller, MC; Russell, T; Sanders, RA, Jr; Terstappen, LW. Expression of epithelial cell adhesion molecule in carcinoma cells present in blood and primary and metastatic tumors. Int. J. Oncol 2005, 27, 49–57. [Google Scholar]
- Maetzel, D; Denzel, S; Mack, B; Canis, M; Went, P; Benk, M; Kieu, C; Papior, P; Baeuerle, PA; Munz, M; Gires, O. Nuclear signalling by tumour-associated antigen EpCAM. Nat. Cell Biol 2009, 11, 162–171. [Google Scholar]
- Brabletz, T; Jung, A; Reu, S; Porzner, M; Hlubek, F; Kunz-Schughart, LA; Knuechel, R; Kirchner, T. Variable beta-catenin expression in colorectal cancers indicates tumor progression driven by the tumor environment. Proc. Natl. Acad. Sci USA 2001, 98, 10356–10361. [Google Scholar]
- Thiery, JP. Epithelial-mesenchymal transitions in tumour progression. Nat. Rev Cancer 2002, 2, 442–454. [Google Scholar]
- Ueno, H; Murphy, J; Jass, JR; Mochizuki, H; Talbot, IC. Tumour ‘budding’ as an index to estimate the potential of aggressiveness in rectal cancer. Histopathology 2002, 40, 127–132. [Google Scholar]
- Zlobec, I; Lugli, A. Invasive front of colorectal cancer: Dynamic interface of pro-/anti-tumor factors. World J. Gastroenterol 2009, 15, 5898–5906. [Google Scholar]
- Hostettler, L; Zlobec, I; Terracciano, L; Lugli, A. ABCG5-positivity in tumor buds is an indicator of poor prognosis in node-negative colorectal cancer patients. World J. Gastroenterol 2010, 16, 732–739. [Google Scholar]
- Kuhn, S; Koch, M; Nubel, T; Ladwein, M; Antolovic, D; Klingbeil, P; Hildebrand, D; Moldenhauer, G; Langbein, L; Franke, WW; Weitz, J; Zoller, M. A complex of EpCAM, claudin-7, CD44 variant isoforms, and tetraspanins promotes colorectal cancer progression. Mol. Cancer Res 2007, 5, 553–567. [Google Scholar]
- Nubel, T; Preobraschenski, J; Tuncay, H; Weiss, T; Kuhn, S; Ladwein, M; Langbein, L; Zoller, M. Claudin-7 regulates EpCAM-mediated functions in tumor progression. Mol. Cancer Res 2009, 7, 285–299. [Google Scholar]
- Brockhausen, I. Mucin-type O-glycans in human colon and breast cancer: Glycodynamics and functions. EMBO Rep 2006, 7, 599–604. [Google Scholar]
- Hollingsworth, MA; Swanson, BJ. Mucins in cancer: Protection and control of the cell surface. Nat. Rev Cancer 2004, 4, 45–60. [Google Scholar]
- Kufe, DW. Mucins in cancer: Function, prognosis and therapy. Nat. Rev Cancer 2009, 9, 874–885. [Google Scholar]
- Farhat, MH; Barada, KA; Tawil, AN; Itani, DM; Hatoum, HA; Shamseddine, AI. Effect of mucin production on survival in colorectal cancer: A case-control study. World J. Gastroenterol 2008, 14, 6981–6985. [Google Scholar]
- Baldus, SE; Monig, SP; Hanisch, FG; Zirbes, TK; Flucke, U; Oelert, S; Zilkens, G; Madejczik, B; Thiele, J; Schneider, PM; Holscher, AH; Dienes, HP. Comparative evaluation of the prognostic value of MUC1, MUC2, sialyl-Lewis(a) and sialyl-Lewis(x) antigens in colorectal adenocarcinoma. Histopathology 2002, 40, 440–449. [Google Scholar]
- Hiraga, Y; Tanaka, S; Haruma, K; Yoshihara, M; Sumii, K; Kajiyama, G; Shimamoto, F; Kohno, N. Immunoreactive MUC1 expression at the deepest invasive portion correlates with prognosis of colorectal cancer. Oncology 1998, 55, 307–319. [Google Scholar]
- Saeland, E; van Vliet, SJ; Backstrom, M; van den Berg, VC; Geijtenbeek, TB; Meijer, GA; van Kooyk, Y. The C-type lectin MGL expressed by dendritic cells detects glycan changes on MUC1 in colon carcinoma. Cancer Immunol. Immunother 2007, 56, 1225–1236. [Google Scholar]
- Itzkowitz, SH; Yuan, M; Montgomery, CK; Kjeldsen, T; Takahashi, HK; Bigbee, WL; Kim, YS. Expression of Tn, sialosyl-Tn, and T antigens in human colon cancer. Cancer Res 1989, 49, 197–204. [Google Scholar]
- Iwasa, S; Okada, K; Chen, WT; Jin, X; Yamane, T; Ooi, A; Mitsumata, M. Increased expression of seprase, a membrane-type serine protease, is associated with lymph node metastasis in human colorectal cancer. Cancer Lett 2005, 227, 229–236. [Google Scholar]
- Perez, RO; Bresciani, BH; Bresciani, C; Proscurshim, I; Kiss, D; Gama-Rodrigues, J; Pereira, DD; Rawet, V; Cecconnello, I; Habr-Gama, A. Mucinous colorectal adenocarcinoma: Influence of mucin expression (Muc1, 2 and 5) on clinico-pathological features and prognosis. Int. J. Colorectal. Dis 2008, 23, 757–765. [Google Scholar]
- Doekhie, FS; Morreau, H; de Bock, GH; Speetjens, FM; Dekker-Ensink, NG; Putter, H; van de Velde, CJ; Tollenaar, RA; Kuppen, PJ. Sialyl Lewis X expression and lymphatic microvessel density in primary tumors of node-negative colorectal cancer patients predict disease recurrence. Cancer Microenviron 2008, 1, 141–151. [Google Scholar]
- Gunther, K; Dworak, O; Remke, S; Pfluger, R; Merkel, S; Hohenberger, W; Reymond, MA. Prediction of distant metastases after curative surgery for rectal cancer. J. Surg. Res 2002, 103, 68–78. [Google Scholar]
- Nakagoe, T; Fukushima, K; Hirota, M; Kusano, H; Ayabe, H; Tomita, M; Kamihira, S. Immunohistochemical expression of sialyl Lex antigen in relation to survival of patients with colorectal carcinoma. Cancer 1993, 72, 2323–2330. [Google Scholar]
- Nakamori, S; Kameyama, M; Imaoka, S; Furukawa, H; Ishikawa, O; Sasaki, Y; Kabuto, T; Iwanaga, T; Matsushita, Y; Irimura, T. Increased expression of sialyl Lewisx antigen correlates with poor survival in patients with colorectal carcinoma: Clinicopathological and immunohistochemical study. Cancer Res 1993, 53, 3632–3637. [Google Scholar]
- Matsui, T; Kojima, H; Suzuki, H; Hamajima, H; Nakazato, H; Ito, K; Nakao, A; Sakamoto, J. Sialyl Lewisa expression as a predictor of the prognosis of colon carcinoma patients in a prospective randomized clinical trial. Jpn. J. Clin. Oncol 2004, 34, 588–593. [Google Scholar]
- Borsig, L; Wong, R; Hynes, RO; Varki, NM; Varki, A. Synergistic effects of L- and P-selectin in facilitating tumor metastasis can involve non-mucin ligands and implicate leukocytes as enhancers of metastasis. Proc. Natl. Acad. Sci USA 2002, 99, 2193–2198. [Google Scholar]
- Kannagi, R. Carbohydrate antigen sialyl Lewis a--its pathophysiological significance and induction mechanism in cancer progression. Chang Gung Med. J 2007, 30, 189–209. [Google Scholar]
- Kohler, S; Ullrich, S; Richter, U; Schumacher, U. E-/P-selectins and colon carcinoma metastasis: First in vivo evidence for their crucial role in a clinically relevant model of spontaneous metastasis formation in the lung. Br. J Cancer 2010, 102, 602–609. [Google Scholar]
- Napier, SL; Healy, ZR; Schnaar, RL; Konstantopoulos, K. Selectin ligand expression regulates the initial vascular interactions of colon carcinoma cells: The roles of CD44v and alternative sialofucosylated selectin ligands. J. Biol. Chem 2007, 282, 3433–3441. [Google Scholar]
- Endo, K; Kohnoe, S; Tsujita, E; Watanabe, A; Nakashima, H; Baba, H; Maehara, Y. Galectin-3 expression is a potent prognostic marker in colorectal cancer. AntiCancer Res 2005, 25, 3117–3121. [Google Scholar]
- Nagy, N; Legendre, H; Engels, O; Andre, S; Kaltner, H; Wasano, K; Zick, Y; Pector, JC; Decaestecker, C; Gabius, HJ; Salmon, I; Kiss, R. Refined prognostic evaluation in colon carcinoma using immunohistochemical galectin fingerprinting. Cancer 2003, 97, 1849–1858. [Google Scholar]
- Legendre, H; Decaestecker, C; Nagy, N; Hendlisz, A; Schuring, MP; Salmon, I; Gabius, HJ; Pector, JC; Kiss, R. Prognostic values of galectin-3 and the macrophage migration inhibitory factor (MIF) in human colorectal cancers. Mod. Pathol 2003, 16, 491–504. [Google Scholar]
- Song, S; Byrd, JC; Mazurek, N; Liu, K; Koo, JS; Bresalier, RS. Galectin-3 modulates MUC2 mucin expression in human colon cancer cells at the level of transcription via AP-1 activation. Gastroenterology 2005, 129, 1581–1591. [Google Scholar]
- Bresalier, RS; Byrd, JC; Wang, L; Raz, A. Colon cancer mucin: A new ligand for the betagalactoside- binding protein galectin-3. Cancer Res 1996, 56, 4354–4357. [Google Scholar]
- Dudas, SP; Yunker, CK; Sternberg, LR; Byrd, JC; Bresalier, RS. Expression of human intestinal mucin is modulated by the beta-galactoside binding protein galectin-3 in colon cancer. Gastroenterology 2002, 123, 817–826. [Google Scholar]
- Iwase, T; Kushima, R; Mukaisho, K; Mitsufuji, S; Okanoue, T; Hattori, T. Overexpression of CD10 and reduced MUC2 expression correlate with the development and progression of colorectal neoplasms. Pathol. Res. Pract 2005, 201, 83–91. [Google Scholar]
- Jantscheff, P; Terracciano, L; Lowy, A; Glatz-Krieger, K; Grunert, F; Micheel, B; Brummer, J; Laffer, U; Metzger, U; Herrmann, R; Rochlitz, C. Expression of CEACAM6 in resectable colorectal cancer: A factor of independent prognostic significance. J. Clin. Oncol 2003, 21, 3638–3646. [Google Scholar]
- Cosimelli, M; De Peppo, F; Castelli, M; Giannarelli, D; Schinaia, G; Castaldo, P; Buttini, GL; Sciarretta, F; Bigotti, G; Di Filippo, F; et al. Multivariate analysis of a tissue CEA, TPA, and CA 19.9 quantitative study in colorectal cancer patients. A preliminary finding. Dis. Colon. Rectum 1989, 32, 389–397. [Google Scholar]
- Kim, JC; Han, MS; Lee, HK; Kim, WS; Park, SK; Park, KC; Bodmer, WF; Rowan, AJ; Kim, OJ. Distribution of carcinoembryonic antigen and biologic behavior in colorectal carcinoma. Dis. Colon. Rectum 1999, 42, 640–648. [Google Scholar]
- Lorenzi, M; Vindigni, C; Minacci, C; Tripodi, SA; Iroatulam, A; Petrioli, R; Francini, G. Histopathological and prognostic evaluation of immunohistochemical findings in colorectal cancer. Int. J. Biol Markers 1997, 12, 68–74. [Google Scholar]
- Nazato, DM; Matos, LL; Waisberg, DR; Souza, JR; Martins, LC; Waisberg, J. Prognostic value of carcinoembryonic antigen distribution in tumor tissue of colorectal carcinoma. Arq. Gastroenterol 2009, 46, 26–31. [Google Scholar]
- Vogel, I; Francksen, H; Soeth, E; Henne-Bruns, D; Kremer, B; Juhl, H. The carcinoembryonic antigen and its prognostic impact on immunocytologically detected intraperitoneal colorectal cancer cells. Am. J. Surg 2001, 181, 188–193. [Google Scholar]
- Hostetter, RB; Augustus, LB; Mankarious, R; Chi, KF; Fan, D; Toth, C; Thomas, P; Jessup, JM. Carcinoembryonic antigen as a selective enhancer of colorectal cancer metastasis. J. Natl. Cancer Inst 1990, 82, 380–385. [Google Scholar]
- Blumenthal, RD; Hansen, HJ; Goldenberg, DM. Inhibition of adhesion, invasion, and metastasis by antibodies targeting CEACAM6 (NCA-90) and CEACAM5 (Carcinoembryonic Antigen). Cancer Res 2005, 65, 8809–8817. [Google Scholar]
- Messick, CA; Sanchez, J; Dejulius, KL; Hammel, J; Ishwaran, H; Kalady, MF. CEACAM- 7: A predictive marker for rectal cancer recurrence. Surgery 2010, 147, 713–719. [Google Scholar]
- Duncan, R; Carpenter, B; Main, LC; Telfer, C; Murray, GI. Characterisation and protein expression profiling of annexins in colorectal cancer. Br. J Cancer 2008, 98, 426–433. [Google Scholar]
- Emoto, K; Yamada, Y; Sawada, H; Fujimoto, H; Ueno, M; Takayama, T; Kamada, K; Naito, A; Hirao, S; Nakajima, Y. Annexin II overexpression correlates with stromal tenascin-C overexpression: A prognostic marker in colorectal carcinoma. Cancer 2001, 92, 1419–1426. [Google Scholar]
- Xue, G; Hao, LQ; Ding, FX; Mei, Q; Huang, JJ; Fu, CG; Yan, HL; Sun, SH. Expression of annexin a5 is associated with higher tumor stage and poor prognosis in colorectal adenocarcinomas. J. Clin. Gastroenterol 2009, 43, 831–837. [Google Scholar]
- Tsukita, S; Yamazaki, Y; Katsuno, T; Tamura, A. Tight junction-based epithelial microenvironment and cell proliferation. Oncogene 2008, 27, 6930–6938. [Google Scholar]
- de Oliveira, SS; de Oliveira, IM; De Souza, W; Morgado-Diaz, JA. Claudins upregulation in human colorectal cancer. FEBS Lett 2005, 579, 6179–6185. [Google Scholar]
- Resnick, MB; Konkin, T; Routhier, J; Sabo, E; Pricolo, VE. Claudin-1 is a strong prognostic indicator in stage II colonic cancer: A tissue microarray study. Mod. Pathol 2005, 18, 511–518. [Google Scholar]
- Ueda, J; Semba, S; Chiba, H; Sawada, N; Seo, Y; Kasuga, M; Yokozaki, H. Heterogeneous expression of claudin-4 in human colorectal cancer: Decreased claudin-4 expression at the invasive front correlates cancer invasion and metastasis. Pathobiology 2007, 74, 32–41. [Google Scholar]
- Cambien, B; Karimdjee, BF; Richard-Fiardo, P; Bziouech, H; Barthel, R; Millet, MA; Martini, V; Birnbaum, D; Scoazec, JY; Abello, J; Al Saati, T; Johnson, MG; Sullivan, TJ; Medina, JC; Collins, TL; Schmid-Alliana, A; Schmid-Antomarchi, H. Organ-specific inhibition of metastatic colon carcinoma by CXCR3 antagonism. Br. J Cancer 2009, 100, 1755–1764. [Google Scholar]
- Kawada, K; Hosogi, H; Sonoshita, M; Sakashita, H; Manabe, T; Shimahara, Y; Sakai, Y; Takabayashi, A; Oshima, M; Taketo, MM. Chemokine receptor CXCR3 promotes colon cancer metastasis to lymph nodes. Oncogene 2007, 26, 4679–4688. [Google Scholar]
- Kim, J; Takeuchi, H; Lam, ST; Turner, RR; Wang, HJ; Kuo, C; Foshag, L; Bilchik, AJ; Hoon, DS. Chemokine receptor CXCR4 expression in colorectal cancer patients increases the risk for recurrence and for poor survival. J. Clin. Oncol 2005, 23, 2744–2753. [Google Scholar]
- Schimanski, CC; Galle, PR; Moehler, M. Chemokine receptor CXCR4-prognostic factor for gastrointestinal tumors. World J. Gastroenterol 2008, 14, 4721–4724. [Google Scholar]
- Gelmini, S; Mangoni, M; Serio, M; Romagnani, P; Lazzeri, E. The critical role of SDF- 1/CXCR4 axis in cancer and cancer stem cells metastasis. J. Endocrinol. Invest 2008, 31, 809–819. [Google Scholar]
- Zimmermann, T; Moehler, M; Gockel, I; Sgourakis, GG; Biesterfeld, S; Muller, M; Berger, MR; Lang, H; Galle, PR; Schimanski, CC. Low expression of chemokine receptor CCR5 in human colorectal cancer correlates with lymphatic dissemination and reduced CD8+ T-cell infiltration. Int. J. Colorectal. Dis 2010, 25, 417–4124. [Google Scholar]
- de Castro-Carpeno, J; Belda-Iniesta, C; Casado Saenz, E; Hernandez Agudo, E; Feliu Batlle, J; Gonzalez Baron, M. EGFR and colon cancer: A clinical view. Clin. Transl. Oncol 2008, 10, 6–13. [Google Scholar]
- Dasari, A; Messersmith, WA. New strategies in colorectal cancer: Biomarkers of response to epidermal growth factor receptor monoclonal antibodies and potential therapeutic targets in phosphoinositide 3-kinase and mitogen-activated protein kinase pathways. Clin. Cancer Res 2010, 16, 3811–3818. [Google Scholar]
- Markman, B; Capdevila, J; Elez, E; Tabernero, J. New trends in epidermal growth factor receptor-directed monoclonal antibodies. Immunotherapy 2009, 1, 965–982. [Google Scholar]
- Azria, D; Bibeau, F; Barbier, N; Zouhair, A; Lemanski, C; Rouanet, P; Ychou, M; Senesse, P; Ozsahin, M; Pelegrin, A; Dubois, JB; Thezenas, S. Prognostic impact of epidermal growth factor receptor (EGFR) expression on loco-regional recurrence after preoperative radiotherapy in rectal cancer. BMC Cancer 2005, 5, 62. [Google Scholar]
- Galizia, G; Lieto, E; Ferraraccio, F; De Vita, F; Castellano, P; Orditura, M; Imperatore, V; La Mura, A; La Manna, G; Pinto, M; Catalano, G; Pignatelli, C; Ciardiello, F. Prognostic significance of epidermal growth factor receptor expression in colon cancer patients undergoing curative surgery. Ann. Surg. Oncol 2006, 13, 823–835. [Google Scholar]
- Spano, JP; Lagorce, C; Atlan, D; Milano, G; Domont, J; Benamouzig, R; Attar, A; Benichou, J; Martin, A; Morere, JF; Raphael, M; Penault-Llorca, F; Breau, JL; Fagard, R; Khayat, D; Wind, P. Impact of EGFR expression on colorectal cancer patient prognosis and survival. Ann. Oncol 2005, 16, 102–108. [Google Scholar]
- Arkom, C; Preecha, R; Anant, K; Soisuda, S; Sangduan, P; Suleeporn, S. Determination of epidermal growth factor receptor (EGFR) in patients with colorectal cancer (Institutional series). Cancer Ther 2007, 5, 137–142. [Google Scholar]
- Doger, FK; Meteoglu, I; Tuncyurek, P; Okyay, P; Cevikel, H. Does the EGFR and VEGF expression predict the prognosis in colon cancer? Eur. Surg. Res 2006, 38, 540–544. [Google Scholar]
- Zhang, C; Hao, L; Wang, L; Xiao, Y; Ge, H; Zhu, Z; Luo, Y; Zhang, Y. Elevated IGFIR expression regulating VEGF and VEGF-C predicts lymph node metastasis in human colorectal cancer. BMC Cancer 2010, 10, 184. [Google Scholar]
- Osako, T; Miyahara, M; Uchino, S; Inomata, M; Kitano, S; Kobayashi, M. Immunohistochemical study of c-erbB-2 protein in colorectal cancer and the correlation with patient survival. Oncology 1998, 55, 548–555. [Google Scholar]
- Kavanagh, DO; Chambers, G; O’Grady, L; Barry, KM; Waldron, RP; Bennani, F; Eustace, PW; Tobbia, I. Is overexpression of HER-2 a predictor of prognosis in colorectal cancer? BMC Cancer 2009, 9, 1. [Google Scholar]
- Baiocchi, G; Lopes, A; Coudry, RA; Rossi, BM; Soares, FA; Aguiar, S; Guimaraes, GC; Ferreira, FO; Nakagawa, WT. ErbB family immunohistochemical expression in colorectal cancer patients with higher risk of recurrence after radical surgery. Int. J. Colorectal. Dis 2009, 24, 1059–1068. [Google Scholar]
- De Oliveira, AT; Matos, D; Logullo, AF; SR, DAS; Neto, RA; Filho, AL; Saad, SS. MET Is highly expressed in advanced stages of colorectal cancer and indicates worse prognosis and mortality. AntiCancer Res 2009, 29, 4807–4811. [Google Scholar]
- Ginty, F; Adak, S; Can, A; Gerdes, M; Larsen, M; Cline, H; Filkins, R; Pang, Z; Li, Q; Montalto, MC. The relative distribution of membranous and cytoplasmic met is a prognostic indicator in stage I and II colon cancer. Clin. Cancer Res 2008, 14, 3814–3822. [Google Scholar]
- Johnstone, RW; Frew, AJ; Smyth, MJ. The TRAIL apoptotic pathway in cancer onset, progression and therapy. Nat. Rev Cancer 2008, 8, 782–798. [Google Scholar]
- Strater, J; Hinz, U; Walczak, H; Mechtersheimer, G; Koretz, K; Herfarth, C; Moller, P; Lehnert, T. Expression of TRAIL and TRAIL receptors in colon carcinoma: TRAIL-R1 is an independent prognostic parameter. Clin. Cancer Res 2002, 8, 3734–3740. [Google Scholar]
- Bavi, P; Prabhakaran, SE; Abubaker, J; Qadri, Z; George, T; Al-Sanea, N; Abduljabbar, A; Ashari, LH; Alhomoud, S; Al-Dayel, F; Hussain, AR; Uddin, S; Al-Kuraya, KS. Prognostic significance of TRAIL death receptors in Middle Eastern colorectal carcinomas and their correlation to oncogenic KRAS alterations. Mol Cancer 2010, 9, 203. [Google Scholar]
- van Geelen, CM; Westra, JL; de Vries, EG; Boersma-van Ek, W; Zwart, N; Hollema, H; Boezen, HM; Mulder, NH; Plukker, JT; de Jong, S; Kleibeuker, JH; Koornstra, JJ. Prognostic significance of tumor necrosis factor-related apoptosis-inducing ligand and its receptors in adjuvantly treated stage III colon cancer patients. J. Clin. Oncol 2006, 24, 4998–5004. [Google Scholar]
- McLornan, DP; Barrett, HL; Cummins, R; McDermott, U; McDowell, C; Conlon, SJ; Coyle, VM; van Schaeybroeck, S; Wilson, R; Kay, EW; Longley, DB; Johnston, PG. Prognostic significance of TRAIL signaling molecules in stage II and III colorectal cancer. Clin. Cancer Res 2010, 16, 3442–3451. [Google Scholar]
- Ishimura, N; Isomoto, H; Bronk, SF; Gores, GJ. Trail induces cell migration and invasion in apoptosis-resistant cholangiocarcinoma cells. Am. J. Physiol. Gastrointest. Liver Physiol 2006, 290, G129–G136. [Google Scholar]
- Trauzold, A; Siegmund, D; Schniewind, B; Sipos, B; Egberts, J; Zorenkov, D; Emme, D; Roder, C; Kalthoff, H; Wajant, H. TRAIL promotes metastasis of human pancreatic ductal adenocarcinoma. Oncogene 2006, 25, 7434–7439. [Google Scholar]
- Strater, J; Hinz, U; Hasel, C; Bhanot, U; Mechtersheimer, G; Lehnert, T; Moller, P. Impaired CD95 expression predisposes for recurrence in curatively resected colon carcinoma: Cinical evidence for immunoselection and CD95L mediated control of minimal residual disease. Gut 2005, 54, 661–665. [Google Scholar]
- Nozoe, T; Yasuda, M; Honda, M; Inutsuka, S; Korenaga, D. Fas ligand expression is correlated with metastasis in colorectal carcinoma. Oncology 2003, 65, 83–88. [Google Scholar]
- Zhang, W; Ding, EX; Wang, Q; Zhu, DQ; He, J; Li, YL; Wang, YH. Fas ligand expression in colon cancer: A possible mechanism of tumor immune privilege. World J. Gastroenterol 2005, 11, 3632–3635. [Google Scholar]
- Lin, MH; Yao, YH; Yu, JH. Expression and clinical significance of nm23-H1, Fas and FasL in colorectal carcinoma tissues. J. Sichuan Univ. Med. Sci. Edn 2005, 36, 503–505. [Google Scholar]
- Menon, AG; Morreau, H; Tollenaar, RA; Alphenaar, E; van Puijenbroek, M; Putter, H; Janssen-Van Rhijn, CM; van De Velde, CJ; Fleuren, GJ; Kuppen, PJ. Down-regulation of HLA-A expression correlates with a better prognosis in colorectal cancer patients. Lab. Invest 2002, 82, 1725–1733. [Google Scholar]
- Speetjens, FM; de Bruin, EC; Morreau, H; Zeestraten, EC; Putter, H; van Krieken, JH; van Buren, MM; van Velzen, M; Dekker-Ensink, NG; van de Velde, CJ; Kuppen, PJ. Clinical impact of HLA class I expression in rectal cancer. Cancer Immunol. Immunother 2008, 57, 601–609. [Google Scholar]
- Lovig, T; Andersen, SN; Thorstensen, L; Diep, CB; Meling, GI; Lothe, RA; Rognum, TO. Strong HLA-DR expression in microsatellite stable carcinomas of the large bowel is associated with good prognosis. Br. J Cancer 2002, 87, 756–762. [Google Scholar]
- Matsushita, K; Takenouchi, T; Shimada, H; Tomonaga, T; Hayashi, H; Shioya, A; Komatsu, A; Matsubara, H; Ochiai, T. Strong HLA-DR antigen expression on cancer cells relates to better prognosis of colorectal cancer patients: Possible involvement of c-myc suppression by interferon-gamma in situ. Cancer Sci 2006, 97, 57–63. [Google Scholar]
- Sakamoto, J; Kojima, H; Kato, J; Hamashima, H; Suzuki, H. Organ-specific expression of the intestinal epithelium-related antigen A33, a cell surface target for antibody-based imaging and treatment in gastrointestinal cancer. Cancer Chemother. Pharmacol 2000, 46, S27–S32. [Google Scholar]
- Scott, AM; Lee, FT; Jones, R; Hopkins, W; MacGregor, D; Cebon, JS; Hannah, A; Chong, G; Paul, U; Papenfuss, A; Rigopoulos, A; Sturrock, S; Murphy, R; Wirth, V; Murone, C; Smyth, FE; Knight, S; Welt, S; Ritter, G; Richards, E; Nice, EC; Burgess, AW; Old, LJ. A phase I trial of humanized monoclonal antibody A33 in patients with colorectal carcinoma: Biodistribution, pharmacokinetics, and quantitative tumor uptake. Clin. Cancer Res 2005, 11, 4810–4817. [Google Scholar]
- Welt, S; Ritter, G; Williams, C, Jr; Cohen, LS; John, M; Jungbluth, A; Richards, EA; Old, LJ; Kemeny, NE. Phase I study of anticolon cancer humanized antibody A33. Clin. Cancer Res 2003, 9, 1338–1346. [Google Scholar]
- Chong, G; Lee, FT; Hopkins, W; Tebbutt, N; Cebon, JS; Mountain, AJ; Chappell, B; Papenfuss, A; Schleyer, P; Paul, U; Murphy, R; Wirth, V; Smyth, FE; Potasz, N; Poon, A; Davis, ID; Saunder, T; O’Keefe, GJ; Burgess, AW; Hoffman, EW; Old, LJ; Scott, AM. Phase I trial of 131I-huA33 in patients with advanced colorectal carcinoma. Clin. Cancer Res 2005, 11, 4818–4826. [Google Scholar]
- Welt, S; Divgi, CR; Kemeny, N; Finn, RD; Scott, AM; Graham, M; Germain, JS; Richards, EC; Larson, SM; Oettgen, HF; et al. Phase I/II study of iodine 131-labeled monoclonal antibody A33 in patients with advanced colon cancer. J. Clin. Oncol 1994, 12, 1561–1571. [Google Scholar]
- Fujimoto, Y; Nakanishi, Y; Sekine, S; Yoshimura, K; Akasu, T; Moriya, Y; Shimoda, T. CD10 expression in colorectal carcinoma correlates with liver metastasis. Dis. Colon. Rectum 2005, 48, 1883–1889. [Google Scholar]
- Ohji, Y; Yao, T; Eguchi, T; Yamada, T; Hirahashi, M; Iida, M; Tsuneyoshi, M. Evaluation of risk of liver metastasis in colorectal adenocarcinoma based on the combination of risk factors including CD10 expression: Multivariate analysis of clinicopathological and immunohistochemical factors. Oncol. Rep 2007, 17, 525–530. [Google Scholar]
- Yao, T; Takata, M; Tustsumi, S; Nishiyama, K; Taguchi, K; Nagai, E; Tsuneyoshi, M. Phenotypic expression of gastrointestinal differentiation markers in colorectal adenocarcinomas with liver metastasis. Pathology 2002, 34, 556–560. [Google Scholar]
- Fujita, S; Yamamoto, S; Akasu, T; Moriya, Y; Taniguchi, H; Shimoda, T. Quantification of CD10 mRNA in colorectal cancer and relationship between mRNA expression and liver metastasis. Anticancer Res 2007, 27, 3307–3311. [Google Scholar]
- Hashida, H; Takabayashi, A; Kanai, M; Adachi, M; Kondo, K; Kohno, N; Yamaoka, Y; Miyake, M. Aminopeptidase N is involved in cell motility and angiogenesis: Its clinical significance in human colon cancer. Gastroenterology 2002, 122, 376–386. [Google Scholar]
- Durrant, LG; Chapman, MA; Buckley, DJ; Spendlove, I; Robins, RA; Armitage, NC. Enhanced expression of the complement regulatory protein CD55 predicts a poor prognosis in colorectal cancer patients. Cancer Immunol. Immunother 2003, 52, 638–642. [Google Scholar]
- Watson, NF; Durrant, LG; Madjd, Z; Ellis, IO; Scholefield, JH; Spendlove, I. Expression of the membrane complement regulatory protein CD59 (protectin) is associated with reduced survival in colorectal cancer patients. Cancer Immunol. Immunother 2006, 55, 973–980. [Google Scholar]
- Steinert, M; Wobus, M; Boltze, C; Schutz, A; Wahlbuhl, M; Hamann, J; Aust, G. Expression and regulation of CD97 in colorectal carcinoma cell lines and tumor tissues. Am. J. Pathol 2002, 161, 1657–1667. [Google Scholar]
- Weichert, W; Knosel, T; Bellach, J; Dietel, M; Kristiansen, G. ALCAM/CD166 is overexpressed in colorectal carcinoma and correlates with shortened patient survival. J. Clin. Pathol 2004, 57, 1160–1164. [Google Scholar]
- Kaifi, JT; Reichelt, U; Quaas, A; Schurr, PG; Wachowiak, R; Yekebas, EF; Strate, T; Schneider, C; Pantel, K; Schachner, M; Sauter, G; Izbicki, JR. L1 is associated with micrometastatic spread and poor outcome in colorectal cancer. Mod. Pathol 2007, 20, 1183–1190. [Google Scholar]
- Mehlen, P; Fearon, ER. Role of the dependence receptor DCC in colorectal cancer pathogenesis. J. Clin. Oncol 2004, 22, 3420–3428. [Google Scholar]
- Saito, M; Yamaguchi, A; Goi, T; Tsuchiyama, T; Nakagawara, G; Urano, T; Shiku, H; Furukawa, K. Expression of DCC protein in colorectal tumors and its relationship to tumor progression and metastasis. Oncology 1999, 56, 134–141. [Google Scholar]
- Shibata, D; Reale, MA; Lavin, P; Silverman, M; Fearon, ER; Steele, G, Jr; Jessup, JM; Loda, M; Summerhayes, IC. The DCC protein and prognosis in colorectal cancer. N. Engl. J. Med 1996, 335, 1727–1732. [Google Scholar]
- Miyoshi, N; Ishii, H; Mimori, K; Tanaka, F; Nagai, K; Uemura, M; Sekimoto, M; Doki, Y; Mori, M. ATP11A is a novel predictive marker for metachronous metastasis of colorectal cancer. Oncol. Rep 2010, 23, 505–510. [Google Scholar]
- Korkaya, H; Wicha, MS. Cancer stem cells: Nature versus nurture. Nat. Cell Biol 2010, 12, 419–421. [Google Scholar]
- Papailiou, J; Bramis, KJ; Gazouli, M; Theodoropoulos, G. Stem cells in colon cancer. A new era in cancer theory begins. Int J Colorectal Dis 2010, 1022–6. [Google Scholar] [CrossRef]
- Shipitsin, M; Polyak, K. The cancer stem cell hypothesis: In search of definitions, markers, and relevance. Lab. Invest 2008, 88, 459–463. [Google Scholar]
- Tan, BT; Park, CY; Ailles, LE; Weissman, IL. The cancer stem cell hypothesis: A work in progress. Lab. Invest 2006, 86, 1203–1207. [Google Scholar]
- Vermeulen, L; De Sousa, EMF; van der Heijden, M; Cameron, K; de Jong, JH; Borovski, T; Tuynman, JB; Todaro, M; Merz, C; Rodermond, H; Sprick, MR; Kemper, K; Richel, DJ; Stassi, G; Medema, JP. Wnt activity defines colon cancer stem cells and is regulated by the microenvironment. Nat. Cell Biol 2010, 12, 468–476. [Google Scholar]
- Wicha, MS; Liu, S; Dontu, G. Cancer stem cells: An old idea--a paradigm shift. Cancer Res 2006, 66, 1883–1890. [Google Scholar]
- Pang, R; Law, WL; Chu, AC; Poon, JT; Lam, CS; Chow, AK; Ng, L; Cheung, LW; Lan, XR; Lan, HY; Tan, VP; Yau, TC; Poon, RT; Wong, BC. A subpopulation of CD26+ cancer stem cells with metastatic capacity in human colorectal cancer. Cell Stem Cell 2010, 6, 603–615. [Google Scholar]
- Dalerba, P; Dylla, SJ; Park, IK; Liu, R; Wang, X; Cho, RW; Hoey, T; Gurney, A; Huang, EH; Simeone, DM; Shelton, AA; Parmiani, G; Castelli, C; Clarke, MF. Phenotypic characterization of human colorectal cancer stem cells. Proc. Natl. Acad. Sci USA 2007, 104, 10158–10163. [Google Scholar]
- Choi, D; Lee, HW; Hur, KY; Kim, JJ; Park, GS; Jang, SH; Song, YS; Jang, KS; Paik, SS. Cancer stem cell markers CD133 and CD24 correlate with invasiveness and differentiation in colorectal adenocarcinoma. World J. Gastroenterol 2009, 15, 2258–2264. [Google Scholar]
- Horst, D; Kriegl, L; Engel, J; Kirchner, T; Jung, A. Prognostic significance of the cancer stem cell markers CD133, CD44, and CD166 in colorectal cancer. Cancer Invest 2009, 27, 844–850. [Google Scholar]
- Ricci-Vitiani, L; Lombardi, DG; Pilozzi, E; Biffoni, M; Todaro, M; Peschle, C; De Maria, R. Identification and expansion of human colon-cancer-initiating cells. Nature 2007, 445, 111–115. [Google Scholar]
- Shmelkov, SV; Butler, JM; Hooper, AT; Hormigo, A; Kushner, J; Milde, T; St. Clair, R; Baljevic, M; White, I; Jin, DK; Chadburn, A; Murphy, AJ; Valenzuela, DM; Gale, NW; Thurston, G; Yancopoulos, GD; D’Angelica, M; Kemeny, N; Lyden, D; Rafii, S. CD133 expression is not restricted to stem cells, and both CD133+ and CD133- metastatic colon cancer cells initiate tumors. J. Clin. Invest 2008, 118, 2111–2120. [Google Scholar]
- Kawasaki, BT; Farrar, WL. Cancer stem cells, CD200 and immunoevasion. Trends Immunol 2008, 29, 464–468. [Google Scholar]
- Moreaux, J; Veyrune, JL; Reme, T; De Vos, J; Klein, B. CD200: A putative therapeutic target in cancer. Biochem. Biophys. Res. Commun 2008, 366, 117–122. [Google Scholar]
- Kawasaki, BT; Mistree, T; Hurt, EM; Kalathur, M; Farrar, WL. Co-expression of the toleragenic glycoprotein, CD200, with markers for cancer stem cells. Biochem. Biophys. Res. Commun 2007, 364, 778–782. [Google Scholar]
- Chen, JS; Chen, KT; Fan, CW; Han, CL; Chen, YJ; Yu, JS; Chang, YS; Chien, CW; Wu, CP; Hung, RP; Chan, EC. Comparison of membrane fraction proteomic profiles of normal and cancerous human colorectal tissues with gel-assisted digestion and iTRAQ labeling mass spectrometry. FEBS J 2010, 277, 3028–3038. [Google Scholar]
- Krasnov, GS; Oparina, N; Khankin, SL; Mashkova, TD; Ershov, AN; Zatsepina, OG; Karpov, VL; Beresten, SF. Colorectal cancer 2D-proteomics: Identification of altered protein expression. Mol. Biol (Mosk) 2009, 43, 348–356. [Google Scholar]
- Mazzanti, R; Solazzo, M; Fantappie, O; Elfering, S; Pantaleo, P; Bechi, P; Cianchi, F; Ettl, A; Giulivi, C. Differential expression proteomics of human colon cancer. Am. J. Physiol. Gastrointest. Liver Physiol 2006, 290, G1329–G1338. [Google Scholar]
- Pei, H; Zhu, H; Zeng, S; Li, Y; Yang, H; Shen, L; Chen, J; Zeng, L; Fan, J; Li, X; Gong, Y; Shen, H. Proteome analysis and tissue microarray for profiling protein markers associated with lymph node metastasis in colorectal cancer. J. Proteome Res 2007, 6, 2495–4501. [Google Scholar]
- Xing, XM; Wang, YH; Huang, Q; Lu, BJ; Lai, MD. Differential expression of secretagogin and glucose-related protein 78 in colorectal carcinoma: A proteome study. Chin. J. Pathol 2007, 36, 107–112. [Google Scholar]
- Lawrie, LC; Curran, S. Laser capture microdissection and colorectal cancer proteomics. Methods Mol. Biol 2005, 293, 245–253. [Google Scholar]
- Sheehan, KM; Gulmann, C; Eichler, GS; Weinstein, JN; Barrett, HL; Kay, EW; Conroy, RM; Liotta, LA; Petricoin, EF, III. Signal pathway profiling of epithelial and stromal compartments of colonic carcinoma reveals epithelial-mesenchymal transition. Oncogene 2008, 27, 323–331. [Google Scholar]
- Kaufman, KL; Belov, L; Huang, P; Mactier, S; Scolyer, RA; Mann, GJ; Christopherson, RI. An extended antibody microarray for surface profiling metastatic melanoma. J. Immunol Methods 2010, 358, 23–34. [Google Scholar]
- Ahram, M; Litou, ZI; Fang, R; Al-Tawallbeh, G. Estimation of membrane proteins in the human proteome. In Silico Biol 2006, 6, 379–386. [Google Scholar]
- Bitarte, N; Bandres, E; Zarate, R; Ramirez, N; Garcia-Foncillas, J. Moving forward in colorectal Cancer Res.earch, what proteomics has to tell. World J. Gastroenterol 2007, 13, 5813–5821. [Google Scholar]
- Yeoh, LC; Loh, CK; Gooi, BH; Singh, M; Gam, LH. Hydrophobic protein in colorectal cancer in relation to tumor stages and grades. World J. Gastroenterol 2010, 16, 2754–2763. [Google Scholar]
- Ikonomou, G; Samiotaki, M; Panayotou, G. Proteomic methodologies and their application in colorectal Cancer Res.earch. Crit. Rev. Clin. Lab. Sci 2009, 46, 319–342. [Google Scholar]
- Nibbe, RK; Chance, MR. Approaches to biomarkers in human colorectal cancer: Looking back, to go forward. Biomark Med 2009, 3, 385–396. [Google Scholar]
- Soreide, K; Nedrebo, BS; Knapp, JC; Glomsaker, TB; Soreide, JA; Korner, H. Evolving molecular classification by genomic and proteomic biomarkers in colorectal cancer: Potential implications for the surgical oncologist. Surg. Oncol 2009, 18, 31–50. [Google Scholar]
- Pepe, MS; Cai, T; Longton, G. Combining predictors for classification using the area under the receiver operating characteristic curve. Biometrics 2006, 62, 221–229. [Google Scholar]
- Zlobec, I; Lugli, A. Prognostic and predictive factors in colorectal cancer. J. Clin. Pathol 2008, 61, 561–569. [Google Scholar]
- Zlobec, I; Minoo, P; Baumhoer, D; Baker, K; Terracciano, L; Jass, JR; Lugli, A. Multimarker phenotype predicts adverse survival in patients with lymph node-negative colorectal cancer. Cancer 2008, 112, 495–502. [Google Scholar]
- Fernebro, E; Bendahl, PO; Dictor, M; Persson, A; Ferno, M; Nilbert, M. Immunohistochemical patterns in rectal cancer: Application of tissue microarray with prognostic correlations. Int. J Cancer 2004, 111, 921–928. [Google Scholar]
- Lyall, MS; Dundas, SR; Curran, S; Murray, GI. Profiling markers of prognosis in colorectal cancer. Clin. Cancer Res 2006, 12, 1184–1191. [Google Scholar]
- Eckel-Passow, JE; Lohse, CM; Sheinin, Y; Crispen, PL; Krco, CJ; Kwon, ED. Tissue microarrays: One size does not fit all. Diagn. Pathol 2010, 5, 48–57. [Google Scholar]
- Lal, S; Brown, A; Nguyen, L; Braet, F; Dyer, W; Dos Remedios, C. Using antibody arrays to detect microparticles from acute coronary syndrome patients based on cluster of differentiation (CD) antigen expression. Mol Cell Proteomics 2009, 8, 799–804. [Google Scholar]
- Lugli, A; Karamitopoulou, E; Panayiotides, I; Karakitsos, P; Rallis, G; Peros, G; Iezzi, G; Spagnoli, G; Bihl, M; Terracciano, L; Zlobec, I. CD8+ lymphocytes/tumour-budding index: An independent prognostic factor representing a ‘pro-/anti-tumour’ approach to tumour host interaction in colorectal cancer. Br. J Cancer 2009, 101, 1382–1392. [Google Scholar]
- Jang, TJ. Expression of E-cadherin and beta-catenin is altered at tumor budding sites, whose number is associated with the progression of colorectal carcinoma. Korean J. Pathol 2009, 43, 523–527. [Google Scholar]
- Hanash, SM; Pitteri, SJ; Faca, VM. Mining the plasma proteome for cancer biomarkers. Nature 2008, 452, 571–579. [Google Scholar]
- Hong, BS; Cho, JH; Kim, H; Choi, EJ; Rho, S; Kim, J; Kim, JH; Choi, DS; Kim, YK; Hwang, D; Gho, YS. Colorectal cancer cell-derived microvesicles are enriched in cell cyclerelated mRNAs that promote proliferation of endothelial cells. BMC Genomics 2009, 10, 556. [Google Scholar]
- Huber, V; Fais, S; Iero, M; Lugini, L; Canese, P; Squarcina, P; Zaccheddu, A; Colone, M; Arancia, G; Gentile, M; Seregni, E; Valenti, R; Ballabio, G; Belli, F; Leo, E; Parmiani, G; Rivoltini, L. Human colorectal cancer cells induce T-cell death through release of proapoptotic microvesicles: Role in immune escape. Gastroenterology 2005, 128, 1796–804. [Google Scholar]
- Mrvar-Brecko, A; Sustar, V; Jansa, V; Stukelj, R; Jansa, R; Mujagic, E; Kruljc, P; Iglic, A; Hagerstrand, H; Kralj-Iglic, V. Isolated microvesicles from peripheral blood and body fluids as observed by scanning electron microscope. Blood Cells Mol. Dis 2010, 44, 307–312. [Google Scholar]
- Valenti, R; Huber, V; Iero, M; Filipazzi, P; Parmiani, G; Rivoltini, L. Tumor-released microvesicles as vehicles of immunosuppression. Cancer Res 2007, 67, 2912–2915. [Google Scholar]
- Moritz, RL; Skandarajah, AR; Ji, H; Simpson, RJ. Proteomic analysis of colorectal cancer: Prefractionation strategies using two-dimensional free-flow electrophoresis. Comp. Funct Genomics 2005, 6, 236–243. [Google Scholar]
- Qiu, Y; Patwa, TH; Xu, L; Shedden, K; Misek, DE; Tuck, M; Jin, G; Ruffin, MT; Turgeon, DK; Synal, S; Bresalier, R; Marcon, N; Brenner, DE; Lubman, DM. Plasma glycoprotein profiling for colorectal cancer biomarker identification by lectin glycoarray and lectin blot. J. Proteome Res 2008, 7, 1693–1703. [Google Scholar]
- Drake, PM; Cho, W; Li, B; Prakobphol, A; Johansen, E; Anderson, NL; Regnier, FE; Gibson, BW; Fisher, SJ. Sweetening the pot: Adding glycosylation to the biomarker discovery equation. Clin. Chem 2010, 56, 223–236. [Google Scholar]
- Fuster, MM; Esko, JD. The sweet and sour of cancer: Glycans as novel therapeutic targets. Nat. Rev Cancer 2005, 5, 526–542. [Google Scholar]
- Reis, CA; Osorio, H; Silva, L; Gomes, C; David, L. Alterations in glycosylation as biomarkers for cancer detection. J. Clin. Pathol 2010, 63, 322–329. [Google Scholar]
- Taylor, AD; Hancock, WS; Hincapie, M; Taniguchi, N; Hanash, SM. Towards an integrated proteomic and glycomic approach to finding cancer biomarkers. Genome Med 2009, 1, 57. [Google Scholar]
- Wang, H; Tso, VK; Slupsky, CM; Fedorak, RN. Metabolomics and detection of colorectal cancer in humans: A systematic review. Future Oncol 2010, 6, 1395–1406. [Google Scholar]
- Nambiar, PR; Gupta, RR; Misra, V. An “Omics” based survey of human colon cancer. Mutat. Res 2010, 693, 3–18. [Google Scholar]
- Durai, R; Yang, SY; Seifalian, AM; Winslet, MC. Principles and applications of gene therapy in colon cancer. J. Gastrointest. Liver Dis 2008, 17, 59–67. [Google Scholar]
- Habermann, JK; Paulsen, U; Roblick, UJ; Upender, MB; McShane, LM; Korn, EL; Wangsa, D; Kruger, S; Duchrow, M; Bruch, HP; Auer, G; Ried, T. Stage-specific alterations of the genome, transcriptome, and proteome during colorectal carcinogenesis. Genes Chromosomes Cancer 2007, 46, 10–26. [Google Scholar]

© 2011 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Belov, L.; Zhou, J.; Christopherson, R.I. Cell Surface Markers in Colorectal Cancer Prognosis. Int. J. Mol. Sci. 2011, 12, 78-113. https://doi.org/10.3390/ijms12010078
Belov L, Zhou J, Christopherson RI. Cell Surface Markers in Colorectal Cancer Prognosis. International Journal of Molecular Sciences. 2011; 12(1):78-113. https://doi.org/10.3390/ijms12010078
Chicago/Turabian StyleBelov, Larissa, Jerry Zhou, and Richard I. Christopherson. 2011. "Cell Surface Markers in Colorectal Cancer Prognosis" International Journal of Molecular Sciences 12, no. 1: 78-113. https://doi.org/10.3390/ijms12010078
APA StyleBelov, L., Zhou, J., & Christopherson, R. I. (2011). Cell Surface Markers in Colorectal Cancer Prognosis. International Journal of Molecular Sciences, 12(1), 78-113. https://doi.org/10.3390/ijms12010078