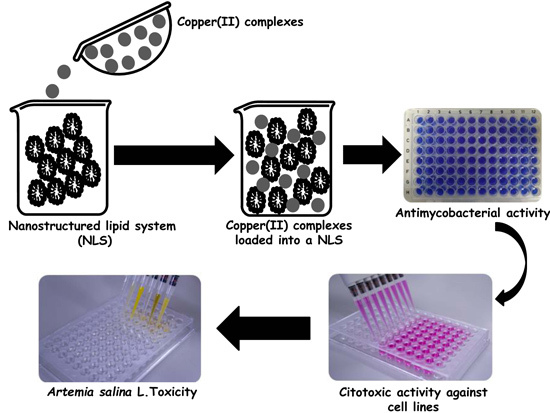
In Vitro Activity of Copper(II) Complexes, Loaded or Unloaded into a Nanostructured Lipid System, against Mycobacterium tuberculosis
Abstract
:1. Introduction
2. Results and Discussion
2.1. Nanostructured Lipid System
2.1.1. Mean Diameter and Polydispersity Index (PDI)
2.1.2. Zeta (ζ) Potential Analysis
2.1.3. Rheological Study
2.2. In Vitro Biological Activity
2.2.1. Antimycobacterial and Cytotoxicity Activities
2.2.2. Artemia salina L. Toxicity
3. Material and Methods
3.1. Materials
3.2. Synthesis of the Copper(II) Complexes
3.3. Preparation of Formulations
3.4. Physicochemical and Structural Characterization of the System
3.4.1. Mean Diameter and Polydispersity Index (PDI)
3.4.2. Zeta Potential Analysis
3.4.3. Rheological Study
Determination of Flow Properties
Oscillatory Analyses
3.5. In Vitro Biological Activity
3.5.1. In Vitro Anti-Mycobacterium tuberculosis
3.5.2. In Vitro Cytotoxic Activity
3.5.3. Selectivity Index
3.5.4. Artemia salina L. Toxicity
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization. Global Tuberculosis Report 2014; World Health Organization Press: Geneva, Switzerland, 2014; p. 171. [Google Scholar]
- World Health Organization. Global Tuberculosis Report 2015; World Health Organization Press: Geneva, Switzerland, 2015; p. 204. [Google Scholar]
- Ronconi, L.; Sadler, P.J. Using coordination chemistry to design new medicines. Coord. Chem. Rev. 2007, 251, 1633–1648. [Google Scholar] [CrossRef]
- Van Rijt, S.H.; Sadler, P.J. Current applications and future potential for bioinorganic chemistry in the development of anticancer drugs. Drug Discov. Today 2009, 14, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Sigel, H. Metal Ions in Biological Systems; Marcel Dekker: New York, NY, USA, 1974; Volume 3. [Google Scholar]
- Sandbhor, U.; Padhye, S.; Billington, D.; Rathbone, D.; Franzblau, S.G.; Anson, C.E.; Powell, A.K. Metal complexes of carboxamidrazone analogs as antitubercular agents 1. Synthesis, X-ray crystal-structures, spectroscopic properties and antimycobacterial activity against Mycobacterium tuberculosis H37Rv. J. Inorg. Biochem. 2002, 90, 127–136. [Google Scholar] [CrossRef]
- Kanwar, S.S.; Lumba, K.; Gupta, S.K.; Katoch, V.M.; Singh, P.; Mishra, A.K.; Kalia, S.B. Synthesis and mycobactericidal properties of metal complexes of isonicotinoyldithiocarbazic acid. Biotechnol. Lett. 2008, 30, 677–680. [Google Scholar] [CrossRef] [PubMed]
- Maccari, R.; Ottana, R.; Bottari, B.; Rotondo, E.; Vigorita, M.G. In vitro advanced antimycobacterial screening of cobalt(II) and copper(II) complexes of fluorinated isonicotinoylhydrazones. Bioorg. Med. Chem. Lett. 2004, 14, 5731–5733. [Google Scholar] [CrossRef] [PubMed]
- Bottari, B.; Maccari, R.; Monforte, F.; Ottanà, R.; Rotondo, E.; Vigorita, M.G. Isoniazid-related copper(II) and nickel(II) complexes with antimycobacterial in vitro activity. Part 9. Bioorg. Med. Chem. Lett. 2000, 10, 657–660. [Google Scholar] [CrossRef]
- Mandewale, M.C.; Thorat, B.; Shelke, D.; Yamgar, R. Synthesis and biological evaluation of new hydrazone derivatives of quinoline and their Cu(II) and Zn(II) complexes against Mycobacterium tuberculosis. Bioinorg. Chem. Appl. 2015, 2015, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Joseph, J.; Nagashri, K.; Janaki, G.B. Novel metal based anti-tuberculosis agent: Synthesis, characterization, catalytic and pharmacological activities of copper complexes. Eur. J. Med. Chem. 2012, 49, 151–163. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.B.; Bonifacio, B.V.; Frem, R.C.G.; Godoy Netto, A.V.; Mauro, A.E.; Da Costa Ferreira, A.M.; Lopes, E.O.; Raddi, M.S.G.; Bauab, T.M.; Pavan, F.R.; et al. A nanostructured lipid system as a strategy to improve the in vitro antibacterial activity of copper(II) complexes. Molecules 2015, 20, 22534–22545. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.B.; Freitas, E.S.; Bernegossi, J.; Gonçalez, M.L.; Sato, M.R.; Leite, C.Q.F.; Pavan, F.R.; Chorilli, M. Nanotechnology-based drug delivery systems for treatment of tuberculosis—A review. J. Biomed. Nanotechnol. 2016, 12, 241–260. [Google Scholar] [CrossRef]
- Freitas, E.S.; Silva, P.B.; Chorilli, M.; Batista, A.A.; Lopes, E.O.; Silva, M.M.; Leite, C.Q.F.; Pavan, F.R. Nanostructured lipid systems as a strategy to improve the in vitro cytotoxicity of ruthenium(II) compounds. Molecules 2014, 19, 5999–6008. [Google Scholar] [CrossRef] [PubMed]
- Sato, M.R.; Silva, P.B.; Souza, R.A.; Santos, K.C.; Chorilli, M. Recent advances in nanoparticle carriers for coordination complexes. Curr. Top. Med. Chem. 2015, 15, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Santos, F.K.; Oyafuso, M.H.; Kiill, C.P.; Gremião, M.P.D.; Chorilli, M. Nanotechnology-based drug delivery systems for treatment of hyperproliferative skin dieases—A review. Curr. Nanosci. 2013, 9, 159–167. [Google Scholar]
- Souza, A.L.R.; Kiill, C.P.; Santos, F.K.; Luz, G.M.; Chorilli, M.; Gremião, M.P.D. Nanotechnology-based drug delivery systems for dermatomycosis treatment. Curr. Nanosci. 2012, 8, 512–519. [Google Scholar] [CrossRef]
- Alvarez, G.; Varela, J.; Marquez, P.; Gabay, M.; Rivas, C.A.; Cuchilla, K.; Echeverria, G.; Piro, O.; Chorilli, M.; Leal, S.; et al. Optimization of antitrypanosomatid agentes: Identification of nonmutagenic drug candidates with in vivo activity. J. Med. Chem. 2014, 57, 3894–3899. [Google Scholar] [CrossRef] [PubMed]
- Cunha Junior, A.D.S.; Fialho, S.L.; Carneiro, L.B.; Oréfice, F. Microemulsions as drug delivery systems for topical ocular administration. Arq. Bras. Oftalmol. 2003, 63, 285–391. [Google Scholar]
- Oliveira, M.B.; Calixto, G.; Graminha, M.; Cerecetto, H.; González, M.; Chorilli, M. Development, characterization, and in vitro biological performance of fluconazole-loaded microemulsions for the topical treatment of cutaneous leishmaniasis. BioMed Res. Int. 2015, 2015, 1–13. [Google Scholar]
- Rigon, R.B.; Fachinetti, N.; Severino, P.; Santana, M.H.A.; Chorilli, M. Skin delivery and in vitro biological evaluation of trans-resveratrol-loaded solid lipid nanoparticles for skin disorder therapies. Molecules 2016, 21, 116–219. [Google Scholar] [CrossRef] [PubMed]
- Mosca, M.; Ceglie, A.; Ambrosone, L. Effect of membrane composition on lipid oxidation in liposomes. Chem. Phys. Lipids 2011, 164, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, F.C.; Calixto, G.M.F.; Hatakeyama, I.N.; Luz, G.M.; Gremião, M.P.; Chorilli, M. Rheological, mechanical, and bioadhesive behavior of hydrogels to optimize skin delivery systems. Drug Dev. Ind. Pharm. 2013, 39, 1750–1757. [Google Scholar] [CrossRef] [PubMed]
- Calixto, G.M.F.; Yoshii, A.C.; Rocha e Silva, H.; Stringhetti Ferreira Cury, B.; Chorilli, M. Polyacrylic acid polymers hydrogels intended to topical drug delivery preparation and characterization. Pharm. Dev. Technol. 2015, 20, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Ceulemans, J.; Vinckier, I.; Ludwig, A. The use of xantan gum in an ophthalmic liquid dosage form: Rheological characterization of the interaction with mucin. J. Pharm. Sci. 2002, 91, 1117–1127. [Google Scholar] [CrossRef] [PubMed]
- Palomino, J.C.; Martin, A.; Camacho, M.; Guerra, H.; Swings, J.; Portaels, F. Resazurin microtiter assay plate: Simple and inexpensive method for detection of drug resistance in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2002, 46, 2720–2722. [Google Scholar] [CrossRef] [PubMed]
- Pavan, F.R.; Sato, D.N.; Leite, C.Q.F. An approach to the search for new drugs against tuberculosis. In Understanding Tuberculosis—New Approaches to Fighting Against Drug Resistance; Cardonar, P.J., Ed.; Intech: Rijeka, Croatia, 2012; pp. 147–156. [Google Scholar]
- Gonçalez, M.L.; Marcussi, D.G.; Calixto, G.M.F.; Corrêa, M.A.; Chorilli, M. Structural characterization and in vitro antioxidant activity of kojic dipalmitate loaded w/o/w multiple emulsions intended for skin disorders. BioMed Res. Int. 2015, 2015, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Ramos, M.A.; Calixto, G.; de Toledo, L.G.; Bonifácio, B.V.; dos Santos, L.C.; de Almeida, M.T.; Chorilli, M.; Bauab, T.M. Liquid crystal precursor mucoadhesive system as a strategy to improve the prophylactic action of Syngonanthus. nitens (Bong.) Ruhland against infection by Candida krusei. Int. J. Nanomed. 2015, 10, 7455–7466. [Google Scholar] [CrossRef] [PubMed]
- Cintra, G.A.D.S.; Pinto, L.A.; Calixto, G.M.F.; Soares, C.P.; Von Zuben, E.D.S.; Scarpa, M.V.; Chorilli, M. Bioadhesive surfactant systems for methotrexate skin delivery. Molecules 2016, 21, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Chuan, J.; Li, Y.; Yang, L.; Sun, X.; Zhang, Q.; Gong, T.; Zhang, Z. Enhanced rifampicin delivery to alveolar macrophages by solid lipid nanoparticles. J. Nanopart. Res. 2013, 15, 1634–1642. [Google Scholar] [CrossRef]
- Orme, I. Search for new drugs for treatment of tuberculosis. Antimicrob. Agents Chemother. 2001, 45, 1943–1946. [Google Scholar] [PubMed]
- Al-Adham, I.S.; Al-Hmoud, N.D.; Khalil, E.; Kierans, M.; Collier, P.J. Microemulsions are highly effective anti-biofilm agents. Lett. Appl. Microbiol. 2003, 36, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Parra, A.L.; Yhebra, R.S.; Sardiñas, I.G.; Buela, L.I. Comparative study of the assay of Artemia salina L. and the estimate of the medium lethal dose (LD50 value) in mice, to determine oral acute toxicity of plant extracts. Phytomedicine 2001, 8, 395–400. [Google Scholar]
- Ferraz, K.O.; Wardell, S.M.; Wardell, J.L.; Louro, S.R.; Beraldo, H. Copper(II) complexes with 2-pyridineformamide-derived thiosemicarbazones: Spectral studies and toxicity against Artemia salina. Spectrochim. Acta A 2009, 73, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Formariz, T.P.; Chiavacci, L.A.; Scarpa, M.V.; Silva, A.A., Jr.; Egito, E.S.T.; Terrugi, C.H.B.; Franzini, C.M.; Sarmento, V.H.V.; Oliveira, A.G. Structure and viscoelastic behavior of pharmaceutical biocompatible anionic microemulsions containing the antitumoral drug compound doxorubicin. Colloids Surf. B 2010, 77, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Pavan, F.R.; Maia, P.I.; Leite, S.R.A.; Deflon, V.M.; Batista, A.A.; Sato, D.N.; Franzblau, S.G.; Leite, C.Q.F. Thiosemicarbazones, semicarbazones, dithiocarbazates and hydrazide/hydrazones: Anti-Mycobacterium tuberculosis activity and cytotoxicity. Eur. J. Med. Chem. 2010, 45, 1898–1905. [Google Scholar] [CrossRef] [PubMed]
- Valdivieso-Garcia, A.; Clarke, R.C.; Rahn, K.; Durette, A.; MacLeod, D.L.; Gyles, C.L. Neutral red assay for measurement of quantitative Vero cell cytotoxicity. Appl. Environ. Microbiol. 1993, 59, 1981–1983. [Google Scholar] [PubMed]
- Formariz, T.P.; Chiavacci, L.A.; Sarmento, V.H.V.; Franzini, C.M.; Silva, A.A., Jr.; Scarpa, M.V.; Santilli, C.V.; Egito, E.S.T.; Oliveira, A.G. Structural changes of biocompatible neutral microemulsions stabilized by mixed surfactant containing soya phosphatidylcholine and their relationship with doxorubicin release. Colloids Surf. B 2008, 63, 287–295. [Google Scholar] [CrossRef] [PubMed]


| Formulation | Mean Diameter ± S.D. (nm) * | Mean PDI ± S.D. * |
|---|---|---|
| NLS | 169.5 ± 0.7095 | 0.135 ± 0.0130 |
| 1-Loaded | 211.1 ± 0.8963 | 0.200 ± 0.00900 |
| 2-Loaded | 205.5 ± 1.652 | 0.226 ± 0.0150 |
| 3-Loaded | 209.8 ± 0.8083 | 0.236 ± 0.00100 |
| Formulation | ζ Potential ± S.D. (mV) * |
|---|---|
| NLS | −0.100 ± 0.103 |
| 1-Loaded | −0.0433 ± 0.214 |
| 2-Loaded | −0.00690 ± 0.0896 |
| 3-Loaded | −8.43 ± 1.63 |
| Formulations | η | K |
|---|---|---|
| NLS | 0.45 | 1.09 |
| 1-Loaded | 0.20 | 9.41 |
| 2-Loaded | 0.37 | 4.73 |
| 3-Loaded | 0.20 | 9.57 |
| Complexes | MIC (μg·mL−1) | IC50 Vero (μg·mL−1) | SI | IC50 J774.A1 (μg·mL−1) | SI | IC50 MRC-5 (μg·mL−1) | SI |
|---|---|---|---|---|---|---|---|
| 1-Not loaded | 20.46 | 109.5 | 5.351 | 80.11 | 3.915 | 76.80 | 3.754 |
| 1-Loaded | 0.3970 | 367.6 | 926.0 | 10.47 | 26.37 | 9.120 | 22.97 |
| 2-Not loaded | 5.913 | 314.3 | 53.15 | 75.36 | 12.74 | 51.90 | 8.777 |
| 2-Loaded | 0.2190 | >500.0 | 2283 | 68.48 | 312.7 | 11.77 | 53.74 |
| 3-Not loaded | 1.459 | 325.3 | 223.0 | 184.0 | 126.1 | 132.0 | 90.47 |
| 3-Loaded | 0.3130 | >500.0 | 1597 | 66.13 | 211.2 | 22.82 | 72.90 |
| Complexes | LC50 (μg·mL−1) |
|---|---|
| 1-Not loaded | 17.10 |
| 1-Loaded | 297.7 |
| 2-Not loaded | 7.800 |
| 2-Loaded | 378.8 |
| 3-Not loaded | 244.1 |
| 3-Loaded | 479.2 |
| DMSO 2% | >1500 |
| NLS | 170.0 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, P.B.d.; Souza, P.C.d.; Calixto, G.M.F.; Lopes, E.D.O.; Frem, R.C.G.; Netto, A.V.G.; Mauro, A.E.; Pavan, F.R.; Chorilli, M. In Vitro Activity of Copper(II) Complexes, Loaded or Unloaded into a Nanostructured Lipid System, against Mycobacterium tuberculosis. Int. J. Mol. Sci. 2016, 17, 745. https://doi.org/10.3390/ijms17050745
Silva PBd, Souza PCd, Calixto GMF, Lopes EDO, Frem RCG, Netto AVG, Mauro AE, Pavan FR, Chorilli M. In Vitro Activity of Copper(II) Complexes, Loaded or Unloaded into a Nanostructured Lipid System, against Mycobacterium tuberculosis. International Journal of Molecular Sciences. 2016; 17(5):745. https://doi.org/10.3390/ijms17050745
Chicago/Turabian StyleSilva, Patricia B. da, Paula C. de Souza, Giovana Maria Fioramonti Calixto, Erica De O. Lopes, Regina C. G. Frem, Adelino V. G. Netto, Antonio E. Mauro, Fernando R. Pavan, and Marlus Chorilli. 2016. "In Vitro Activity of Copper(II) Complexes, Loaded or Unloaded into a Nanostructured Lipid System, against Mycobacterium tuberculosis" International Journal of Molecular Sciences 17, no. 5: 745. https://doi.org/10.3390/ijms17050745
APA StyleSilva, P. B. d., Souza, P. C. d., Calixto, G. M. F., Lopes, E. D. O., Frem, R. C. G., Netto, A. V. G., Mauro, A. E., Pavan, F. R., & Chorilli, M. (2016). In Vitro Activity of Copper(II) Complexes, Loaded or Unloaded into a Nanostructured Lipid System, against Mycobacterium tuberculosis. International Journal of Molecular Sciences, 17(5), 745. https://doi.org/10.3390/ijms17050745