Comprehensive Evaluation of TFF3 Promoter Hypomethylation and Molecular Biomarker Potential for Prostate Cancer Diagnosis and Prognosis
Abstract
:1. Introduction
2. Results
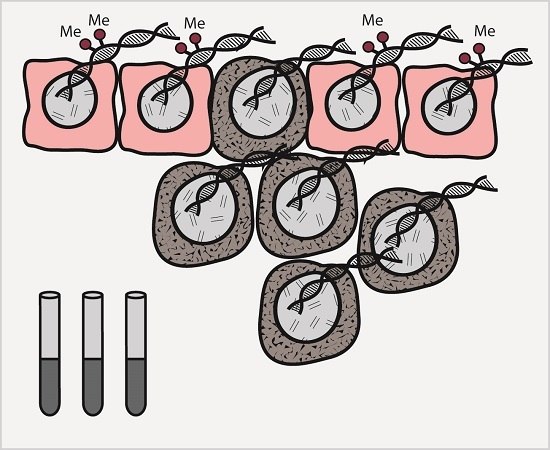
2.1. Hypomethylation of the Trefoil Factor 3 (TFF3) Promoter Region in Prostate Cancer (PC) Samples
2.2. Correlation between TFF3 Promoter Methylation, Clinicopathological Parameters, and ERG, ETS Transcription Factor (ERG) Status
2.3. Survival Analysis
2.4. TFF3 RNA Expression Patterns in Public Datasets for PC
2.5. Prognostic Potential of TFF3 RNA Expression
3. Discussion
4. Materials and Methods
4.1. Patient Material
4.2. Quantitative Methylation Specific PCR (qMSP)
4.3. Microarray and RNAseq Data
4.4. Statistical Analysis
4.5. Ethical Approval
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| 450K | Illumina 450K DNA methylation array |
| AN | Adjacent normal |
| AUC | Area under the curve |
| BPH | Benign prostatic hyperplasia |
| CI | Confidence interval |
| CPM | Count per million |
| FFPE | Formalin-fixed paraffin embedded |
| HE | Hematoxylin and eosin |
| HR | Hazard ratio |
| NM | Non-malignant |
| OR | Odds ratio |
| Path | Pathological |
| PC | Prostate cancer |
| PIN | Prostatic intraepithelial neoplasia |
| PSA | Prostate specific antigen |
| qMSP | Quantitative methylation specific PCR |
| RNAseq | RNA sequencing |
| ROC | Receiver operating characteristics |
| RP | Radical prostatectomy |
| TCGA | The Cancer Genome Atlas |
| TFF3 | Trefoil factor 3 |
| TMA | Tissue microarray |
References
- Ferlay, J.; Steliarova-Foucher, E.; Lortet-Tieulent, J.; Rosso, S.; Coebergh, J.W.; Comber, H.; Forman, D.; Bray, F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries in 2012. Eur. J. Cancer 2013, 49, 1374–1403. [Google Scholar] [CrossRef] [PubMed]
- Loeb, S.; Bjurlin, M.A.; Nicholson, J.; Tammela, T.L.; Penson, D.F.; Carter, H.B.; Carroll, P.; Etzioni, R. Overdiagnosis and overtreatment of prostate cancer. Eur. Urol. 2014, 65, 1046–1055. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.A. Functions of DNA methylation: Islands, start sites, gene bodies and beyond. Nat. Rev. Genet. 2012, 13, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Sproul, D.; Kitchen, R.R.; Nestor, C.E.; Dixon, J.M.; Sims, A.H.; Harrison, D.J.; Ramsahoye, B.H.; Meehan, R.R. Tissue of origin determines cancer-associated CpG island promoter hypermethylation patterns. Genome Biol. 2012, 13, R84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haldrup, C.; Mundbjerg, K.; Vestergaard, E.M.; Lamy, P.; Wild, P.; Schulz, W.A.; Arsov, C.; Visakorpi, T.; Borre, M.; Høyer, S.; et al. DNA methylation signatures for prediction of biochemical recurrence after radical prostatectomy of clinically localized prostate cancer. J. Clin. Oncol. 2013, 31, 3250–3258. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, H.; Haldrup, C.; Strand, S.; Mundbjerg, K.; Mortensen, M.M.; Thorsen, K.; Ostenfeld, M.S.; Wild, P.J.; Arsov, C.; Goering, W.; et al. Hypermethylation of the GABRE~miR-452~miR-224 promoter in prostate cancer predicts biochemical recurrence after radical prostatectomy. Clin. Cancer Res. 2014, 20, 2169–2181. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y. Promoter hypermethylation as a biomarker in prostate adenocarcinoma. Methods Mol. Biol. 2015, 1238, 607–625. [Google Scholar] [PubMed]
- Haldrup, C.; Lynnerup, A.S.; Storebjerg, T.M.; Vang, S.; Wild, P.; Visakorpi, T.; Arsov, C.; Schulz, W.A.; Lindberg, J.; Grönberg, H.; et al. Large-scale evaluation of SLC18A2 in prostate cancer reveals diagnostic and prognostic biomarker potential at three molecular levels. Mol. Oncol. 2016, 10, 825–837. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, K.D.; Abildgaard, M.O.; Haldrup, C.; Ulhøi, B.P.; Kristensen, H.; Strand, S.; Parker, C.; Høyer, S.; Borre, M.; Ørntoft, T.F. Prognostic significance of aberrantly silenced ANPEP expression in prostate cancer. Br. J. Cancer 2013, 108, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, K.D.; Borre, M.; Ørntoft, T.F.; Dyrskjøt, L.; Tørring, N. Chromosomal deletion, promoter hypermethylation and downregulation of FYN in prostate cancer. Int. J. Cancer 2008, 122, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Strand, S.H.; Orntoft, T.F.; Sorensen, K.D. Prognostic DNA methylation markers for prostate cancer. Int. J. Mol. Sci. 2014, 15, 16544–16576. [Google Scholar] [CrossRef] [PubMed]
- Banez, L.L.; Sun, L.; van Leenders, G.J.; Wheeler, T.M.; Bangma, C.H.; Freedland, S.J.; Ittmann, M.M.; Lark, A.L.; Madden, J.F.; Hartman, A.; et al. Multicenter clinical validation of PITX2 methylation as a prostate specific antigen recurrence predictor in patients with post-radical prostatectomy prostate cancer. J. Urol. 2010, 184, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Schatz, P.; Dietrich, D.; Koenig, T.; Burger, M.; Lukas, A.; Fuhrmann, I.; Kristiansen, G.; Stoehr, R.; Schuster, M.; Lesche, R.; et al. Development of a diagnostic microarray assay to assess the risk of recurrence of prostate cancer based on PITX2 DNA methylation. J. Mol. Diagn. 2010, 12, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Weiss, G.; Cottrell, S.; Distler, J.; Schatz, P.; Kristiansen, G.; Ittmann, M.; Haefliger, C.; Lesche, R.; Hartmann, A.; Corman, J.; et al. DNA methylation of the PITX2 gene promoter region is a strong independent prognostic marker of biochemical recurrence in patients with prostate cancer after radical prostatectomy. J. Urol. 2009, 181, 1678–1685. [Google Scholar] [CrossRef] [PubMed]
- Augello, C.; Gianelli, U.; Falcone, R.; Tabano, S.; Savi, F.; Bonaparte, E.; Ciboddo, M.; Paganini, L.; Parafioriti, A.; Ricca, D.; et al. PDGFB hypomethylation is a favourable prognostic biomarker in primary myelofibrosis. Leuk. Res. 2015, 39, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Tang, H.; Zhang, Z.; Li, W.; Wang, Z.; Zheng, Y.; Wu, M.; Li, G. POTEH hypomethylation, a new epigenetic biomarker for glioma prognosis. Brain Res. 2011, 1391, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Kjellev, S. The trefoil factor family—Small peptides with multiple functionalities. Cell. Mol. Life Sci. 2009, 66, 1350–1369. [Google Scholar] [CrossRef] [PubMed]
- Longman, R.J.; Douthwaite, J.; Sylvester, P.A.; Poulsom, R.; Corfield, A.P.; Thomas, M.G.; Wright, N.A. Coordinated localisation of mucins and trefoil peptides in the ulcer associated cell lineage and the gastrointestinal mucosa. Gut 2000, 47, 792–800. [Google Scholar] [CrossRef] [PubMed]
- Kindon, H.; Pothoulakis, C.; Thim, L.; Lynch-Devaney, K.; Podolsky, D.K. Trefoil peptide protection of intestinal epithelial barrier function: Cooperative interaction with mucin glycoprotein. Gastroenterology 1995, 109, 516–523. [Google Scholar] [CrossRef]
- Madsen, J.; Nielsen, O.; Tornøe, I.; Thim, L.; Holmskov, U. Tissue localization of human trefoil factors 1, 2, and 3. J. Histochem. Cytochem. 2007, 55, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, W. Trefoil factors TFF (trefoil factor family) peptide-triggered signals promoting mucosal restitution. Cell. Mol. Life Sci. 2005, 62, 2932–2938. [Google Scholar] [CrossRef] [PubMed]
- Jatoi, A.; Vierkant, R.A.; Hawthorne, K.M.; Block, M.S.; Ramus, S.J.; Larson, N.B.; Fridley, B.L.; Goode, E.L. Clinical and Emergent biomarkers and their relationship to the prognosis of ovarian cancer. Oncology 2016, 90, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.R.; Griffiths, A.B.; Tilby, M.T.; Westley, B.R.; May, F.E. TFF3 is a normal breast epithelial protein and is associated with differentiated phenotype in early breast cancer but predisposes to invasion and metastasis in advanced disease. Am. J. Pathol. 2012, 180, 904–916. [Google Scholar] [CrossRef] [PubMed]
- Abols, A.; Ducena, K.; Andrejeva, D.; Sadovska, L.; Zandberga, E.; Vilmanis, J.; Narbuts, Z.; Tars, J.; Eglitis, J.; Pirags, V.; et al. Trefoil factor 3 is required for differentiation of thyroid follicular cells and acts as a context-dependent tumor suppressor. Neoplasma 2015, 62, 914–924. [Google Scholar] [CrossRef] [PubMed]
- Morito, K.; Nakamura, J.; Kitajima, Y.; Kai, K.; Tanaka, T.; Kubo, H.; Miyake, S.; Noshiro, H. The value of trefoil factor 3 expression in predicting the longterm outcome and early recurrence of colorectal cancer. Int. J. Oncol. 2015, 46, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Zheng, L.; Zhang, L.; Chen, S.; Zhu, M.; Li, X.; Wang, Y. TFF3 and HER2 expression and their correlation with survival in gastric cancer. Tumour Biol. 2015, 36, 3001–3007. [Google Scholar] [CrossRef] [PubMed]
- Ding, A.; Zhao, W.; Shi, X.; Yao, R.; Zhou, F.; Yue, L.; Liu, S.; Qiu, W. Impact of NPM, TFF3 and TACC1 on the prognosis of patients with primary gastric cancer. PLoS ONE 2013, 8, e82136. [Google Scholar] [CrossRef] [PubMed]
- Pandey, V.; Wu, Z.S.; Zhang, M.; Li, R.; Zhang, J.; Zhu, T.; Lobie, P.E. Trefoil factor 3 promotes metastatic seeding and predicts poor survival outcome of patients with mammary carcinoma. Breast Cancer Res. 2014, 16, 429. [Google Scholar] [CrossRef] [PubMed]
- Perera, O.; Evans, A.; Pertziger, M.; MacDonald, C.; Chen, H.; Liu, D.X.; Lobie, P.E.; Perry, J.K. Trefoil factor 3 (TFF3) enhances the oncogenic characteristics of prostate carcinoma cells and reduces sensitivity to ionising radiation. Cancer Lett. 2015, 361, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Faith, D.A.; Isaacs, W.B.; Morgan, J.D.; Fedor, H.L.; Hicks, J.L.; Mangold, L.A.; Walsh, P.C.; Partin, A.W.; Platz, E.A.; Luo, J.; et al. Trefoil factor 3 overexpression in prostatic carcinoma: Prognostic importance using tissue microarrays. Prostate 2004, 61, 215–227. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Chiu, Y.L.; Rubin, M.A.; Demichelis, F.; Mosquera, J.M. V-ets erythroblastosis virus E26 oncogene homolog (avian)/Trefoil factor 3/high-molecular-weight cytokeratin triple immunostain: A novel tissue-based biomarker in prostate cancer with potential clinical application. Hum. Pathol. 2013, 44, 2282–2292. [Google Scholar] [CrossRef] [PubMed]
- Garraway, I.P.; Seligson, D.; Said, J.; Horvath, S.; Reiter, R.E. Trefoil factor 3 is overexpressed in human prostate cancer. Prostate 2004, 61, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Terry, S.; Nicolaiew, N.; Basset, V.; Semprez, F.; Soyeux, P.; Maillé, P.; Vacherot, F.; Ploussard, G.; Londoño-Vallejo, A.; de la Taille, A.; et al. Clinical value of ERG, TFF3, and SPINK1 for molecular subtyping of prostate cancer. Cancer 2015, 121, 1422–1430. [Google Scholar] [CrossRef] [PubMed]
- Adamo, P.; Ladomery, M.R. The oncogene ERG: A key factor in prostate cancer. Oncogene 2016, 35, 403–414. [Google Scholar] [CrossRef] [PubMed]
- Bostrom, P.J.; Bjartell, A.S.; Catto, J.W.; Eggener, S.E.; Lilja, H.; Loeb, S.; Schalken, J.; Schlomm, T.; Cooperberg, M.R. Genomic predictors of outcome in prostate cancer. Eur. Urol. 2015, 68, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, E.M.; Nexø, E.; Tørring, N.; Borre, M.; Ørntoft, T.F.; Sørensen, K.D. Promoter hypomethylation and upregulation of trefoil factors in prostate cancer. Int. J. Cancer 2010, 127, 1857–1865. [Google Scholar] [CrossRef] [PubMed]
- Strand, S.H.; Switnicki, M.; Moller, M.; Haldrup, C.; Storebjerg, T.M.; Hedegaard, J.; Nordentoft, I.; Hoyer, S.; Borre, M.; Pedersen, J.S.; et al. RHCG and TCAF1 promoter hypermethylation predicts biochemical recurrence in prostate cancer patients treated by radical prostatectomy. Oncotarget 2017, 8, 5774–5788. [Google Scholar] [CrossRef] [PubMed]
- TCGA. The Molecular Taxonomy of Primary Prostate Cancer. Cell 2015, 163, 1011–1025. [Google Scholar]
- Strand, S.H.; Hoyer, S.; Lynnerup, A.-S.; Haldrup, C.; Storebjerg, T.M.; Borre, M.; Orntoft, T.F.; Sorensen, K.D. High levels of 5-hydroxymethylcytosine (5hmC) is an adverse predictor of biochemical recurrence after prostatectomy in ERG-negative prostate cancer. Clin. Epigenet. 2015, 7, 111. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.S.; Schultz, N.; Hieronymus, H.; Gopalan, A.; Xiao, Y.; Carver, B.S.; Arora, V.K.; Kaushik, P.; Cerami, E.; Reva, B.; et al. Integrative genomic profiling of human prostate cancer. Cancer Cell 2010, 18, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, M.M.; Høyer, S.; Lynnerup, A.-S.; Ørntoft, T.F.; Sørensen, K.D.; Borre, M.; Dyrskjøt, L. Expression profiling of prostate cancer tissue delineates genes associated with recurrence after prostatectomy. Sci. Rep. 2015, 5, 16018. [Google Scholar] [CrossRef] [PubMed]
- Rickman, D.S.; Chen, Y.B.; Banerjee, S.; Pan, Y.; Yu, J.; Vuong, T.; Perner, S.; Lafargue, C.J.; Mertz, K.D.; Setlur, S.R.; et al. ERG cooperates with androgen receptor in regulating trefoil factor 3 in prostate cancer disease progression. Neoplasia 2010, 12, 1031–1040. [Google Scholar] [CrossRef] [PubMed]
- Jeronimo, C.; Usadel, H.; Henrique, R.; Oliveira, J.; Lopes, C.; Nelson, W.G.; Sidransky, D. Quantitation of GSTP1 methylation in non-neoplastic prostatic tissue and organ-confined prostate adenocarcinoma. J. Natl. Cancer Inst. 2001, 93, 1747–1752. [Google Scholar] [CrossRef] [PubMed]
- Eilers, T.; Machtens, S.; Tezval, H.; Blaue, C.; Lichtinghagen, R.; Hagemann, J.; Jonas, U.; Serth, J. Prospective diagnostic efficiency of biopsy washing DNA GSTP1 island hypermethylation for detection of adenocarcinoma of the prostate. Prostate 2007, 67, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Roehl, K.A.; Antenor, J.A.; Catalona, W.J. Serial biopsy results in prostate cancer screening study. J. Urol. 2002, 167, 2435–2439. [Google Scholar] [CrossRef]
- Djavan, B.; Mazal, P.; Zlotta, A.; Wammack, R.; Ravery, V.; Remzi, M.; Susani, M.; Borkowski, A.; Hruby, S.; Boccon-Gibod, L.; et al. Pathological features of prostate cancer detected on initial and repeat prostate biopsy: Results of the prospective European Prostate Cancer Detection study. Prostate 2001, 47, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Loeb, S.; Vellekoop, A.; Ahmed, H.U.; Catto, J.; Emberton, M.; Nam, R.; Rosario, D.J.; Scattoni, V.; Lotan, Y. Systematic review of complications of prostate biopsy. Eur. Urol. 2013, 64, 876–892. [Google Scholar] [CrossRef] [PubMed]
- Brikun, I.; Nusskern, D.; Gillen, D.; Lynn, A.; Murtagh, D.; Feczko, J.; Nelson, W.G.; Freije, D. A panel of DNA methylation markers reveals extensive methylation in histologically benign prostate biopsy cores from cancer patients. Biomark. Res. 2014, 2, 25. [Google Scholar] [CrossRef] [PubMed]
- Trock, B.J.; Brotzman, M.J.; Mangold, L.A.; Bigley, J.W.; Epstein, J.I.; McLeod, D.; Klein, E.A.; Jones, J.S.; Wang, S.; McAskill, T.; et al. Evaluation of GSTP1 and APC methylation as indicators for repeat biopsy in a high-risk cohort of men with negative initial prostate biopsies. BJU Int. 2012, 110, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Troyer, D.A.; Lucia, M.S.; de Bruïne, A.P.; Mendez-Meza, R.; Baldewijns, M.M.; Dunscomb, N.; van Engeland, M.; McAskill, T.; Bierau, K.; Louwagie, J.; et al. Prostate cancer detected by methylated gene markers in histopathologically cancer-negative tissues from men with subsequent positive biopsies. Cancer Epidemiol. Biomark. Prev. 2009, 18, 2717–2722. [Google Scholar] [CrossRef] [PubMed]
- Moller, M.; Strand, S.H.; Mundbjerg, K.; Liang, G.; Gill, I.; Haldrup, C.; Borre, M.; Høyer, S.; Ørntoft, T.F.; Sørensen, K.D. Heterogeneous patterns of DNA methylation-based field effects in histologically normal prostate tissue from cancer patients. Sci. Rep. 2017, 7, 40636. [Google Scholar] [CrossRef] [PubMed]
- Carroll, P.R.; Parsons, J.K.; Andriole, G.; Bahnson, R.R.; Castle, E.P.; Catalona, W.J.; Dahl, D.M.; Davis, J.W.; Epstein, J.I.; Etzioni, R.B.; et al. NCCN guidelines insights: Prostate cancer early detection, version 2.2016. J. Natl. Compr. Cancer Netw. 2016, 14, 509–519. [Google Scholar] [CrossRef]
- Vestergaard, E.M.; Borre, M.; Poulsen, S.S.; Nexø, E.; Tørring, N. Plasma levels of trefoil factors are increased in patients with advanced prostate cancer. Clin. Cancer Res. 2006, 12, 807–812. [Google Scholar] [CrossRef] [PubMed]
- Esserman, L.J.; Thompson, I.M.; Reid, B.; Nelson, P.; Ransohoff, D.F.; Welch, H.G.; Hwang, S.; Berry, D.A.; Kinzler, K.W.; Black, W.C.; et al. Addressing overdiagnosis and overtreatment in cancer: A prescription for change. Lancet Oncol. 2014, 15, e234–e242. [Google Scholar] [CrossRef]
- Mottet, N.; Bellmunt, J.; Bolla, M.; Briers, E.; Cumberbatch, M.G.; de Santis, M.; Fossati, N.; Gross, T.; Henry, A.M.; Joniau, S.; et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: Screening, diagnosis, and local treatment with curative intent. Eur. Urol. 2017, 71, 618–629. [Google Scholar] [CrossRef] [PubMed]
- McGrath, S.; Christidis, D.; Perera, M.; Hong, S.K.; Manning, T.; Vela, I.; Lawrentschuk, N. Prostate cancer biomarkers: Are we hitting the mark? Prostate Int. 2016, 4, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Tomlins, S.A.; Mudaliar, K.M.; Chiu, Y.L.; Esgueva, R.; Mehra, R.; Suleman, K.; Varambally, S.; Brenner, J.C.; MacDonald, T.; et al. Antibody-based detection of ERG rearrangement-positive prostate cancer. Neoplasia 2010, 12, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Braun, M.; Goltz, D.; Shaikhibrahim, Z.; Vogel, W.; Böhm, D.; Scheble, V.; Sotlar, K.; Fend, F.; Tan, S.H.; Dobi, A.; et al. ERG protein expression and genomic rearrangement status in primary and metastatic prostate cancer—A comparative study of two monoclonal antibodies. Prostate Cancer Prostatic Dis. 2012, 15, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Dedeurwaerder, S.; Defrance, M.; Calonne, E.; Denis, H.; Sotiriou, C.; Fuks, F. Evaluation of the infinium methylation 450K technology. Epigenomics 2011, 3, 771–784. [Google Scholar] [CrossRef] [PubMed]
- Trapnell, C.; Pachter, L.; Salzberg, S.L. TopHat: Discovering splice junctions with RNA-Seq. Bioinformatics 2009, 25, 1105–1111. [Google Scholar] [CrossRef] [PubMed]
- Langmead, B.; Trapnell, C.; Pop, M.; Salzberg, S.L. Ultrafast and memory-efficient alignment of short DNA sequences to the human genome. Genome Biol. 2009, 10, R25. [Google Scholar] [CrossRef] [PubMed]
- Anders, S.; Pyl, P.T.; Huber, W. HTSeq—A Python framework to work with high-throughput sequencing data. Bioinformatics 2015, 31, 166–169. [Google Scholar] [CrossRef] [PubMed]



| Variable | PC Samples Analyzed by qMSP (n = 292) | PC Samples Analyzed by 450K and/or RNAseq (n = 498) |
|---|---|---|
| Age (years) | ||
| Median (range) | 63 (46–73) | 61 (41–78) |
| pT-stage | ||
| pT2 | 183 (62.7%) | 188 (37.8%) |
| pT3 | 107 (36.6%) | 293 (58.8%) |
| pT4 | 2 (0.7%) | 10 (2.0%) |
| Unknown | 0 (0%) | 7 (1.4%) |
| Gleason score | ||
| <7 | 113 (38.7%) | 86 (17.3%) |
| 7 | 142 (48.6%) | 240 (48.2%) |
| >7 | 36 (12.3%) | 170 (34.1%) |
| Unknown | 1 (0.3%) | 2 (0.4%) |
| Pre-op. serum PSA (ng/mL) | ||
| Median (range) | 11.8 (0.6–64.2) | 7.5 (0.7–107) |
| 0–10 | 114 (39.0%) | 331 (66.5%) |
| >10 | 177 (60.1%) | 152 (30.5%) |
| Unknown | 1 (0.3%) | 15 (3.0%) |
| pN-stage | ||
| pN0 | 252 (86.3%) | 0 (0.0%) |
| pN1 | 5 (1.7%) | 0 (0.0%) |
| Unknown | 35 (12.0%) | 498 (100.0%) |
| Surgical margin status | ||
| Negative | 196 (57.9%) | 316 (63.5%) |
| Positive | 92 (31.5%) | 152 (30.5%) |
| Unknown | 4 (1.4%) | 30 (6.0%) |
| PSA recurrence | ||
| Yes | 132 (45.2%) | 46 (9.2%) |
| No | 160 (54.8%) | 346 (69.5%) |
| Unknown | 0 (0.0%) | 106 (21.3%) |
| Follow-up (months) | ||
| Median (range) | 65 (5–151) | 20 (3–154) |
| ERG status (IHC) | ||
| Pos | 59 (20.2%) | 0 (0.0%) |
| Neg | 43 (14.7%) | 0 (0.0%) |
| Unknown | 190 (65.1%) | 495 (100.0%) |
| Non/pre-malignant samples | Age/years | Age/years |
| Median (range) | Median (range) | |
| AN (n = 18, n = 67) | 62 (56–72) | 61 (43–72) |
| BPH (n = 15) | 70 (56–83) | - |
| PIN (n = 11) | 63 (54–68) | - |
| Variable | Logistic Regression | Variable Value (Dichotomized) | Median TFF3 Methylation (95% CI) | Mann–Whitney p-Value | |
|---|---|---|---|---|---|
| OR | p-Value | ||||
| Age | 0.999 | 0.992 | - | - | - |
| Pre-operative PSA | 0.958 | 0.053 | 0–10 ng/mL | 0.13 (0.10–0.15) | 0.202 |
| >10 ng/mL | 0.15 (0.13–0.20) | ||||
| Gleason score | 0.264 | <0.001 * | GS < 7 | 0.16 (0.13–0.22) | 0.007 * |
| GS ≥ 7 | 0.13 (0.11–0.15) | ||||
| Pathological T-stage | - | - | pT2 | 0.14 (0.12–0.19) | 0.331 |
| pT3–4 | 0.13 (0.11–0.17) | ||||
| Pathological N-stage | - | - | pN0 | 0.15 (0.13–0.19) | 0.367 |
| pN1 | 0.10 (0.00–0.44) | ||||
| Margin status | - | - | Neg | 0.15 (0.12–0.19) | 0.261 |
| Pos | 0.14 (0.11–0.19) | ||||
| PSA recurrence status | - | - | No | 0.13 (0.10–0.15) | 0.258 |
| Yes | 0.16 (0.13–0.21) | ||||
| ERG status (IHC) | - | - | Neg | 0.22 (0.16–0.30) | 0.578 |
| Pos | 0.22 (0.15–0.28) | ||||
| Variable | HR (95% CI) | p-Value | |
|---|---|---|---|
| TFF3 methylation | Cont. | 1.01 (0.44–2.29) | 0.986 |
| Age | Cont. | 0.98 (0.95–1.01) | 0.136 |
| Pre-op. PSA | Cont. | 1.05 (1.03–1.06) | <0.001 * |
| Gleason score | <7 vs. ≥7 | 2.19 (1.46–3.28) | <0.001 * |
| Path. T-stage | pT2 vs. pT3–4 | 3.64 (2.58–5.12) | <0.001 * |
| Path. N-stage | pN0 vs. pN1 | 4.00 (1.62–9.85) | 0.003 * |
| Surgical margin status | Neg vs. pos | 3.28 (2.32–4.63) | <0.001 * |
| ERG status (IHC) | Neg vs. pos | 1.13 (0.71–1.82) | 0.606 |
| Variable | HR (95% CI) | p-Value | |
|---|---|---|---|
| TFF3 methylation, cg21970261 | Cont. | 1.96 (0.28–13.75) | 0.497 |
| TFF3 methylation, cg04806409 | Cont. | 0.04 (0.00–1.79) | 0.096 |
| TFF3 methylation, cg14283447 | Cont. | 0.97 (0.03–31.95) | 0.985 |
| TFF3 RNA expression | Cont. | 0.84 (0.74–0.97) | 0.013 * |
| Age | Cont. | 1.02 (0.97–1.06) | 0.479 |
| Pre-op. PSA | Cont. | 1.02 (1.00–1.04) | 0.065 |
| Path. Gleason score | <7 vs. ≥7 | 4.75 (1.15–19.61) | 0.031 * |
| Path. T-stage | pT2 vs. pT3–4 | 6.02 (2.16–16.81) | 0.001 * |
| Surgical margin status | Neg vs. pos | 1.47 (0.82–2.65) | 0.198 |
| ERG RNA expression | Low vs. high | 0.95 (0.50–1.63) | 0.741 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nørgaard, M.; Haldrup, C.; Storebjerg, T.M.; Vestergaard, E.M.; Wild, P.J.; Høyer, S.; Borre, M.; Ørntoft, T.F.; Sørensen, K.D. Comprehensive Evaluation of TFF3 Promoter Hypomethylation and Molecular Biomarker Potential for Prostate Cancer Diagnosis and Prognosis. Int. J. Mol. Sci. 2017, 18, 2017. https://doi.org/10.3390/ijms18092017
Nørgaard M, Haldrup C, Storebjerg TM, Vestergaard EM, Wild PJ, Høyer S, Borre M, Ørntoft TF, Sørensen KD. Comprehensive Evaluation of TFF3 Promoter Hypomethylation and Molecular Biomarker Potential for Prostate Cancer Diagnosis and Prognosis. International Journal of Molecular Sciences. 2017; 18(9):2017. https://doi.org/10.3390/ijms18092017
Chicago/Turabian StyleNørgaard, Maibritt, Christa Haldrup, Tine Maj Storebjerg, Else Marie Vestergaard, Peter J. Wild, Søren Høyer, Michael Borre, Torben Falck Ørntoft, and Karina Dalsgaard Sørensen. 2017. "Comprehensive Evaluation of TFF3 Promoter Hypomethylation and Molecular Biomarker Potential for Prostate Cancer Diagnosis and Prognosis" International Journal of Molecular Sciences 18, no. 9: 2017. https://doi.org/10.3390/ijms18092017
APA StyleNørgaard, M., Haldrup, C., Storebjerg, T. M., Vestergaard, E. M., Wild, P. J., Høyer, S., Borre, M., Ørntoft, T. F., & Sørensen, K. D. (2017). Comprehensive Evaluation of TFF3 Promoter Hypomethylation and Molecular Biomarker Potential for Prostate Cancer Diagnosis and Prognosis. International Journal of Molecular Sciences, 18(9), 2017. https://doi.org/10.3390/ijms18092017