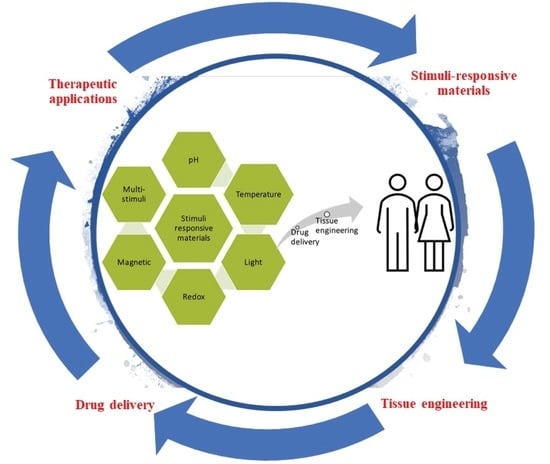
Stimuli-Responsive Materials for Tissue Engineering and Drug Delivery
Abstract
:1. Introduction
2. pH-Responsive Materials
3. Thermoresponsive Materials
3.1. Natural Thermoresponsive Materials
3.2. Synthetic Thermoresponsive Materials
4. Light-Responsive Materials
5. Redox-Responsive Materials and Electroactive Polymers
5.1. Polymers Containing Disulfide Bonds
5.2. Ferrocene Containing Polymers
5.3. Viologens
5.4. Tetrathiafulvalene
5.5. Electroactive Polymers for Tissue Regeneration
6. Magnetic Responsive Nanomaterials
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lumelsky, N.; O’Hayre, M.; Chander, P.; Shum, L.; Somerman, M.J. Autotherapies: Enhancing Endogenous Healing and Regeneration. Trends Mol. Med. 2018, 24, 919–930. [Google Scholar] [CrossRef] [PubMed]
- Lavrador, P.; Gaspar, V.M.; Mano, J.F. Stimuli-responsive nanocarriers for delivery of bone therapeutics–Barriers and progresses. J. Control. Release 2018, 273, 51–67. [Google Scholar] [CrossRef] [PubMed]
- Rogina, A.; Ressler, A.; Matić, I.; Gallego Ferrer, G.; Marijanović, I.; Ivanković, M.; Ivanković, H. Cellular hydrogels based on pH-responsive chitosan-hydroxyapatite system. Carbohydr. Polym. 2017, 166, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Echazú, M.I.A.; Olivetti, C.E.; Peralta, I.; Alonso, M.R.; Anesini, C.; Perez, C.J.; Alvarez, G.S.; Desimone, M.F. Development of pH-responsive biopolymer-silica composites loaded with Larrea divaricata Cav. extract with antioxidant activity. Colloids Surfaces B Biointerfaces 2018, 169, 82–91. [Google Scholar] [CrossRef]
- Parani, M.; Lokhande, G.; Singh, A.; Gaharwar, A.K. Engineered Nanomaterials for Infection Control and Healing Acute and Chronic Wounds. ACS Appl. Mater. Interfaces 2016, 8, 10049–10069. [Google Scholar] [CrossRef]
- Hamdan, S.; Pastar, I.; Drakulich, S.; Dikici, E.; Tomic-Canic, M.; Deo, S.; Daunert, S. Nanotechnology-Driven Therapeutic Interventions in Wound Healing: Potential Uses and Applications. ACS Cent. Sci. 2017, 3, 163–175. [Google Scholar] [CrossRef]
- Bose, S.; Robertson, S.F.; Bandyopadhyay, A. Surface modification of biomaterials and biomedical devices using additive manufacturing. Acta Biomater. 2018, 66, 6–22. [Google Scholar] [CrossRef]
- Wu, G.; Li, P.; Feng, H.; Zhang, X.; Chu, P.K. Engineering and functionalization of biomaterials via surface modification. J. Mater. Chem. B 2015, 3, 2024–2042. [Google Scholar] [CrossRef]
- Pezzoni, M.; Catalano, P.N.; Pizarro, R.A.; Desimone, M.F.; Soler-Illia, G.J.A.A.; Bellino, M.G.; Costa, C.S. Antibiofilm effect of supramolecularly templated mesoporous silica coatings. Mater. Sci. Eng. C 2017, 77. [Google Scholar] [CrossRef]
- Catalano, P.N.; Pezzoni, M.; Costa, C.; Soler-Illia, G.J.D.A.A.; Bellino, M.G.; Desimone, M.F. Optically transparent silver-loaded mesoporous thin film coating with long-lasting antibacterial activity. Microporous Mesoporous Mater. 2016, 236. [Google Scholar] [CrossRef]
- Bellino, M.G.; Golbert, S.; De Marzi, M.C.; Soler-Illia, G.J.A.A.; Desimone, M.F. Controlled adhesion and proliferation of a human osteoblastic cell line by tuning the nanoporosity of titania and silica coatings. Biomater. Sci. 2013, 1. [Google Scholar] [CrossRef] [PubMed]
- Badeau, B.A.; DeForest, C.A. Programming Stimuli-Responsive Behavior into Biomaterials. Annu. Rev. Biomed. Eng. 2019, 21, 241–265. [Google Scholar] [CrossRef] [PubMed]
- Ooi, H.W.; Hafeez, S.; van Blitterswijk, C.A.; Moroni, L.; Baker, M.B. Hydrogels that listen to cells: A review of cell-responsive strategies in biomaterial design for tissue regeneration. Mater. Horizons 2017, 4, 1020–1040. [Google Scholar] [CrossRef]
- Kondiah, P.; Choonara, Y.; Kondiah, P.; Marimuthu, T.; Kumar, P.; du Toit, L.; Pillay, V. A Review of Injectable Polymeric Hydrogel Systems for Application in Bone Tissue Engineering. Molecules 2016, 21, 1580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albert, K.; Hsu, H.-Y. Carbon-Based Materials for Photo-Triggered Theranostic Applications. Molecules 2016, 21, 1585. [Google Scholar] [CrossRef]
- Shen, L. Biocompatible Polymer/Quantum Dots Hybrid Materials: Current Status and Future Developments. J. Funct. Biomater. 2011, 2, 355–372. [Google Scholar] [CrossRef] [Green Version]
- Galdopórpora, J.M.; Morcillo, M.F.; Ibar, A.; Perez, C.J.; Tuttolomondo, M.V.; Desimone, M.F. Development of Silver Nanoparticles/Gelatin Thermoresponsive Nanocomposites: Characterization and Antimicrobial Activity. Curr. Pharm. Des. 2019, 25, 4121–4129. [Google Scholar]
- Mousavi, S.T.; Harper, G.R.; Municoy, S.; Ashton, M.D.; Townsend, D.; Alsharif, G.H.K.; Oikonomou, V.K.; Firlak, M.; Au-Yong, S.; Murdock, B.E.; et al. Electroactive Silk Fibroin Films for Electrochemically Enhanced Delivery of Drugs. Macromol. Mater. Eng. 2020, n/a, 2000130. [Google Scholar] [CrossRef]
- Gonçalves, G.A.R.; Paiva, R.D.M.A. Gene therapy: Advances, challenges and perspectives. Einstein (São Paulo) 2017, 15, 369–375. [Google Scholar] [CrossRef] [Green Version]
- Pattni, B.S.; Torchilin, V.P. Targeted Drug Delivery Systems: Strategies and Challenges. In Targeted Drug Delivery: Concepts and Design; Devarajan, P.V., Jain, S., Eds.; Springer International Publishing: Cham, Switzerland, 2015; pp. 3–38. ISBN 978-3-319-11354-8. [Google Scholar]
- Khademhosseini, A.; Langer, R. A decade of progress in tissue engineering. Nat. Protoc. 2016, 11, 1775–1781. [Google Scholar] [CrossRef]
- Mura, S.; Nicolas, J.; Couvreur, P. Stimuli-responsive nanocarriers for drug delivery. Nat. Mater. 2013, 12, 991–1003. [Google Scholar] [CrossRef] [PubMed]
- Gracia, R.; Mecerreyes, D. Polymers with redox properties: Materials for batteries, biosensors and more. Polym. Chem. 2013, 4, 2206–2214. [Google Scholar] [CrossRef]
- Huo, M.; Yuan, J.; Tao, L.; Wei, Y. Redox-responsive polymers for drug delivery: from molecular design to applications. Polym. Chem. 2014, 5, 1519–1528. [Google Scholar] [CrossRef]
- Hardy, J.G.; Lee, J.Y.; Schmidt, C.E. Biomimetic conducting polymer-based tissue scaffolds. Curr. Opin. Biotechnol. 2013, 24, 847–854. [Google Scholar] [CrossRef] [Green Version]
- Rajabi, A.H.; Jaffe, M.; Arinzeh, T.L. Piezoelectric materials for tissue regeneration: A review. Acta Biomater. 2015, 24, 12–23. [Google Scholar] [CrossRef] [Green Version]
- Baxter, F.R.; Bowen, C.R.; Turner, I.G.; Dent, A.C.E. Electrically active bioceramics: A review of interfacial responses. Ann. Biomed. Eng. 2010, 38, 2079–2092. [Google Scholar] [CrossRef]
- Ribeiro, C.; Sencadas, V.; Correia, D.M.; Lanceros-Méndez, S. Piezoelectric polymers as biomaterials for tissue engineering applications. Colloids Surfaces B Biointerfaces 2015, 136, 46–55. [Google Scholar] [CrossRef] [Green Version]
- Chorsi, M.T.; Curry, E.J.; Chorsi, H.T.; Das, R.; Baroody, J.; Purohit, P.K.; Ilies, H.; Nguyen, T.D. Piezoelectric Biomaterials for Sensors and Actuators. Adv. Mater. 2018, 31, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Yuan, H.; Lei, T.; Qin, Y.; He, J.H.; Yang, R. Design and application of piezoelectric biomaterials. J. Phys. D. Appl. Phys. 2019, 52, 194002–194012. [Google Scholar] [CrossRef] [Green Version]
- Kapat, K.; Shubhra, Q.T.H.; Zhou, M.; Leeuwenburgh, S. Piezoelectric Nano-Biomaterials for Biomedicine and Tissue Regeneration. Adv. Funct. Mater. 2020, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Kocak, G.; Tuncer, C.; Bütün, V. pH-Responsive polymers. Polym. Chem. 2017, 8, 144–176. [Google Scholar] [CrossRef]
- Omidi, M.; Yadegari, A.; Tayebi, L. Wound dressing application of pH-sensitive carbon dots/chitosan hydrogel. RSC Adv. 2017, 7, 10638–10649. [Google Scholar] [CrossRef] [Green Version]
- Banerjee, I.; Mishra, D.; Das, T.; Maiti, T.K. Wound pH-Responsive Sustained Release of Therapeutics from a Poly(NIPAAm-co-AAc) Hydrogel. J. Biomater. Sci. Polym. Ed. 2012, 23, 111–132. [Google Scholar] [CrossRef] [PubMed]
- Ninan, N.; Forget, A.; Shastri, V.P.; Voelcker, N.H.; Blencowe, A. Antibacterial and Anti-Inflammatory pH-Responsive Tannic Acid-Carboxylated Agarose Composite Hydrogels for Wound Healing. ACS Appl. Mater. Interfaces 2016, 8, 28511–28521. [Google Scholar] [CrossRef]
- Qiao, Y.; Wan, J.; Zhou, L.; Ma, W.; Yang, Y.; Luo, W.; Yu, Z.; Wang, H. Stimuli-responsive nanotherapeutics for precision drug delivery and cancer therapy. WIREs Nanomed. Nanobiotechnol. 2019, 11, e1527. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, N.N.; Ferreira, L.M.B.; Cardoso, V.M.O.; Boni, F.I.; Souza, A.L.R.; Gremião, M.P.D. Recent advances in smart hydrogels for biomedical applications: From self-assembly to functional approaches. Eur. Polym. J. 2018, 99, 117–133. [Google Scholar] [CrossRef] [Green Version]
- Karimi, M.; Eslami, M.; Sahandi-Zangabad, P.; Mirab, F.; Farajisafiloo, N.; Shafaei, Z.; Ghosh, D.; Bozorgomid, M.; Dashkhaneh, F.; Hamblin, M.R. pH-Sensitive stimulus-responsive nanocarriers for targeted delivery of therapeutic agents. WIREs Nanomed. Nanobiotechnol. 2016, 8, 696–716. [Google Scholar] [CrossRef] [Green Version]
- Adedoyin, A.A.; Ekenseair, A.K. Biomedical applications of magneto-responsive scaffolds. Nano Res. 2018, 11, 5049–5064. [Google Scholar] [CrossRef]
- Katz, J.S.; Burdick, J.A. Light-responsive biomaterials: Development and applications. Macromol. Biosci. 2010, 10, 339–348. [Google Scholar] [CrossRef]
- Ward, M.A.; Georgiou, T.K. Thermoresponsive Polymers for Biomedical Applications. Polymers 2011, 3, 1215–1242. [Google Scholar] [CrossRef] [Green Version]
- Sponchioni, M.; Capasso Palmiero, U.; Moscatelli, D. Thermo-responsive polymers: Applications of smart materials in drug delivery and tissue engineering. Mater. Sci. Eng. C 2019, 102, 589–605. [Google Scholar] [CrossRef] [PubMed]
- Zarrintaj, P.; Jouyandeh, M.; Ganjali, M.R.; Hadavand, B.S.; Mozafari, M.; Sheiko, S.S.; Vatankhah-Varnoosfaderani, M.; Gutiérrez, T.J.; Saeb, M.R. Thermo-sensitive polymers in medicine: A review. Eur. Polym. J. 2019, 117, 402–423. [Google Scholar] [CrossRef]
- Zhang, J.; Jiang, X.; Wen, X.; Xu, Q.; Zeng, H.; Zhao, Y.; Liu, M.; Wang, Z.; Hu, X.; Wang, Y. Bio-responsive smart polymers and biomedical applications. J. Phys. Mater. 2019, 2, 32004. [Google Scholar] [CrossRef]
- Fu, X.; Hosta-Rigau, L.; Chandrawati, R.; Cui, J. Multi-Stimuli-Responsive Polymer Particles, Films, and Hydrogels for Drug Delivery. Chem 2018, 4, 2084–2107. [Google Scholar] [CrossRef] [Green Version]
- Hajebi, S.; Rabiee, N.; Bagherzadeh, M.; Ahmadi, S.; Rabiee, M.; Roghani-Mamaqani, H.; Tahriri, M.; Tayebi, L.; Hamblin, M.R. Stimulus-responsive polymeric nanogels as smart drug delivery systems. Acta Biomater. 2019, 92, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Sood, N.; Bhardwaj, A.; Mehta, S.; Mehta, A. Stimuli-responsive hydrogels in drug delivery and tissue engineering. Drug Deliv. 2016, 23, 748–770. [Google Scholar] [CrossRef] [Green Version]
- Koetting, M.C.; Peters, J.T.; Steichen, S.D.; Peppas, N.A. Stimulus-responsive hydrogels: Theory, modern advances, and applications. Mater. Sci. Eng. R Reports 2015, 93, 1–49. [Google Scholar] [CrossRef]
- Shah, A.; Malik, M.S.; Khan, G.S.; Nosheen, E.; Iftikhar, F.J.; Khan, F.A.; Shukla, S.S.; Akhter, M.S.; Kraatz, H.-B.; Aminabhavi, T.M. Stimuli-responsive peptide-based biomaterials as drug delivery systems. Chem. Eng. J. 2018, 353, 559–583. [Google Scholar] [CrossRef]
- Khan, F.; Tanaka, M. Designing Smart Biomaterials for Tissue Engineering. Int. J. Mol. Sci. 2018, 19, 17. [Google Scholar] [CrossRef] [Green Version]
- Webb, B.A.; Chimenti, M.; Jacobson, M.P.; Barber, D.L. Dysregulated pH: A perfect storm for cancer progression. Nat. Rev. Cancer 2011, 11, 671–677. [Google Scholar] [CrossRef]
- Sahle, F.F.; Gulfam, M.; Lowe, T.L. Design strategies for physical-stimuli-responsive programmable nanotherapeutics. Drug Discov. Today 2018, 23, 992–1006. [Google Scholar] [CrossRef]
- Hu, Y.B.; Dammer, E.B.; Ren, R.J.; Wang, G. The endosomal-lysosomal system: From acidification and cargo sorting to neurodegeneration. Transl. Neurodegener. 2015, 4, 18–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, L.; Neumann, M.; Fu, T.; Li, W.; Cheng, X.; Su, B.-L. Porous and responsive hydrogels for cell therapy. Curr. Opin. Colloid Interface Sci. 2018, 38, 135–157. [Google Scholar] [CrossRef]
- Perez, R.A.; Singh, R.K.; Kim, T.-H.; Kim, H.-W. Silica-based multifunctional nanodelivery systems toward regenerative medicine. Mater. Horizons 2017, 4, 772–799. [Google Scholar] [CrossRef]
- Wang, Y.; Byrne, J.D.; Napier, M.E.; DeSimone, J.M. Engineering nanomedicines using stimuli-responsive biomaterials. Adv. Drug Deliv. Rev. 2012, 64, 1021–1030. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schneider, L.A.; Korber, A.; Grabbe, S.; Dissemond, J. Influence of pH on wound-healing: A new perspective for wound-therapy? Arch. Dermatol. Res. 2007, 298, 413–420. [Google Scholar] [CrossRef]
- Zhu, L.; Bratlie, K.M. pH sensitive methacrylated chitosan hydrogels with tunable physical and chemical properties. Biochem. Eng. J. 2018, 132, 38–46. [Google Scholar] [CrossRef]
- You, J.-O.; Rafat, M.; Almeda, D.; Maldonado, N.; Guo, P.; Nabzdyk, C.S.; Chun, M.; LoGerfo, F.W.; Hutchinson, J.W.; Pradhan-Nabzdyk, L.K.; et al. pH-responsive scaffolds generate a pro-healing response. Biomaterials 2015, 57, 22–32. [Google Scholar] [CrossRef]
- Yang, C.; Guo, W.; Cui, L.; Xiang, D.; Cai, K.; Lin, H.; Qu, F. pH-responsive controlled-release system based on mesoporous bioglass materials capped with mineralized hydroxyapatite. Mater. Sci. Eng. C 2014, 36, 237–243. [Google Scholar] [CrossRef]
- Cicuéndez, M.; Doadrio, J.C.; Hernández, A.; Portolés, M.T.; Izquierdo-Barba, I.; Vallet-Regí, M. Multifunctional pH sensitive 3D scaffolds for treatment and prevention of bone infection. Acta Biomater. 2018, 65, 450–461. [Google Scholar] [CrossRef] [Green Version]
- Gulzar, A.; Gai, S.; Yang, P.; Li, C.; Ansari, M.B.; Lin, J. Stimuli responsive drug delivery application of polymer and silica in biomedicine. J. Mater. Chem. B 2015, 3, 8599–8622. [Google Scholar] [CrossRef] [PubMed]
- Lennox, K.A.; Owczarzy, R.; Thomas, D.M.; Walder, J.A.; Behlke, M.A. Improved Performance of Anti-miRNA Oligonucleotides Using a Novel Non-Nucleotide Modifier. Mol. Ther. Nucleic Acids 2013, 2, e117. [Google Scholar] [CrossRef] [PubMed]
- Makovitzki, A.; Fink, A.; Shai, Y. Suppression of human solid tumor growth inmice by intratumor and systemic inoculation of histidine-rich and pH-dependent host defense–like lytic peptides. Cancer Res. 2009, 69, 3458–3463. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Q.; Ran, R.; Zhang, L.; Liu, Y.; Mei, L.; Zhang, Z.; Gao, H.; He, Q. Simultaneous delivery of therapeutic antagomirs with paclitaxel for the management of metastatic tumors by a pH-responsive anti-microbial peptide-mediated liposomal delivery system. J. Control. Release 2015, 197, 208–218. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Li, X.; Shen, Y.; Chang, G.; Yang, J.; Gu, Z. Self-healing pH-sensitive cytosine- and guanosine-modified hyaluronic acid hydrogels via hydrogen bonding. Polymer 2017, 108, 348–360. [Google Scholar] [CrossRef]
- Han, D.; Steckl, A.J. Selective pH-Responsive Core–Sheath Nanofiber Membranes for Chem/Bio/Med Applications: Targeted Delivery of Functional Molecules. ACS Appl. Mater. Interfaces 2017, 9, 42653–42660. [Google Scholar] [CrossRef] [PubMed]
- Tagami, T.; Foltz, W.D.; Ernsting, M.J.; Lee, C.M.; Tannock, I.F.; May, J.P.; Li, S.-D. MRI monitoring of intratumoral drug delivery and prediction of the therapeutic effect with a multifunctional thermosensitive liposome. Biomaterials 2011, 32, 6570–6578. [Google Scholar] [CrossRef]
- Yang, H.Y.; Li, Y.; Lee, D.S. Multifunctional and Stimuli-Responsive Magnetic Nanoparticle-Based Delivery Systems for Biomedical Applications. Adv. Ther. 2018, 1800011, 1–17. [Google Scholar] [CrossRef]
- Miguel, S.P.; Ribeiro, M.P.; Brancal, H.; Coutinho, P.; Correia, I.J. Thermoresponsive chitosan–agarose hydrogel for skin regeneration. Carbohydr. Polym. 2014, 111, 366–373. [Google Scholar] [CrossRef]
- Katas, H.; Wen, C.Y.; Siddique, M.I.; Hussain, Z.; Mohd Fadhil, F.H. Thermoresponsive curcumin/DsiRNA nanoparticle gels for the treatment of diabetic wounds: Synthesis and drug release. Ther. Deliv. 2017, 8, 137–150. [Google Scholar] [CrossRef]
- Mellati, A.; Fan, C.-M.; Tamayol, A.; Annabi, N.; Dai, S.; Bi, J.; Jin, B.; Xian, C.; Khademhosseini, A.; Zhang, H. Microengineered 3D cell-laden thermoresponsive hydrogels for mimicking cell morphology and orientation in cartilage tissue engineering. Biotechnol. Bioeng. 2016, 114, 217–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, C.; Zeng, Z.; Qazvini, N.T.; Yu, X.; Zhang, R.; Yan, S.; Shu, Y.; Zhu, Y.; Duan, C.; Bishop, E.; et al. Thermoresponsive Citrate-Based Graphene Oxide Scaffold Enhances Bone Regeneration from BMP9-Stimulated Adipose-Derived Mesenchymal Stem Cells. ACS Biomater. Sci. Eng. 2018, 4, 2943–2955. [Google Scholar] [CrossRef] [PubMed]
- Meewes, M.; Ricka, J.; De Silva, M.; Nyffenegger, R.; Binkert, T. Coil-globule transition of poly(N-isopropylacrylamide): A study of surfactant effects by light scattering. Macromolecules 1991, 24, 5811–5816. [Google Scholar] [CrossRef]
- Zhu, Y.; Batchelor, R.; Lowe, A.B.; Roth, P.J. Design of Thermoresponsive Polymers with Aqueous LCST, UCST, or Both: Modification of a Reactive Poly(2-vinyl-4,4-dimethylazlactone) Scaffold. Macromolecules 2016, 49, 672–680. [Google Scholar] [CrossRef] [Green Version]
- Mah, E.; Ghosh, R.; Mah, E.; Ghosh, R. Thermo-Responsive Hydrogels for Stimuli-Responsive Membranes. Processes 2013, 1, 238–262. [Google Scholar] [CrossRef]
- Vanparijs, N.; Nuhn, L.; De Geest, B.G. Transiently thermoresponsive polymers and their applications in biomedicine. Chem. Soc. Rev. 2017, 46, 1193–1239. [Google Scholar] [CrossRef]
- Ye, J.; Wang, J.; Zhu, Y.; Wei, Q.; Wang, X.; Yang, J.; Tang, S.; Liu, H.; Fan, J.; Zhang, F.; et al. A thermoresponsive polydiolcitrate-gelatin scaffold and delivery system mediates effective bone formation from BMP9-transduced mesenchymal stem cells. Biomed. Mater. 2016. [Google Scholar] [CrossRef]
- Slemming-Adamsen, P.; Song, J.; Dong, M.; Besenbacher, F.; Chen, M. In Situ Cross-Linked PNIPAM/Gelatin Nanofibers for Thermo-Responsive Drug Release. Macromol. Mater. Eng. 2015. [Google Scholar] [CrossRef]
- Han, S.; Li, M.; Liu, X.; Gao, H.; Wu, Y. Construction of amphiphilic copolymer nanoparticles based on gelatin as drug carriers for doxorubicin delivery. Colloids Surfaces B Biointerfaces 2013. [Google Scholar] [CrossRef]
- Peng, Y.; Li, J.; Li, J.; Fei, Y.; Dong, J.; Pan, W. Optimization of thermosensitive chitosan hydrogels for the sustained delivery of venlafaxine hydrochloride. Int. J. Pharm. 2013, 441, 482–490. [Google Scholar] [CrossRef]
- Dang, Q.; Liu, K.; Zhang, Z.; Liu, C.; Liu, X.; Xin, Y.; Cheng, X.; Xu, T.; Cha, D.; Fan, B. Fabrication and evaluation of thermosensitive chitosan/collagen/α, β-glycerophosphate hydrogels for tissue regeneration. Carbohydr. Polym. 2017, 167, 145–157. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, F.; Fu, Q.; Liu, Y.; Wang, Z.; Qi, N. In vitro proliferation and osteogenic differentiation of human dental pulp stem cells in injectable thermo-sensitive chitosan/β-glycerophosphate/hydroxyapatite hydrogel. J. Biomater. Appl. 2016, 31, 317–327. [Google Scholar] [CrossRef]
- Cochis, A.; Bonetti, L.; Sorrentino, R.; Contessi Negrini, N.; Grassi, F.; Leigheb, M.; Rimondini, L.; Farè, S. 3D Printing of Thermo-Responsive Methylcellulose Hydrogels for Cell-Sheet Engineering. Materials 2018, 11, 579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thirumala, S.; Gimble, J.; Devireddy, R.; Thirumala, S.; Gimble, J.M.; Devireddy, R.V. Methylcellulose Based Thermally Reversible Hydrogel System for Tissue Engineering Applications. Cells 2013, 2, 460–475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandri, G.; Bonferoni, M.C.; Rossi, S.; Ferrari, F.; Mori, M.; Del Fante, C.; Perotti, C.; Caramella, C. Thermosensitive eyedrops containing platelet lysate for the treatment of corneal ulcers. Int. J. Pharm. 2012, 426, 1–6. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, J.R.; Callahan, D.J.; Chilkoti, A. Drug delivery to solid tumors by elastin-like polypeptides. Adv. Drug Deliv. Rev. 2010, 62, 1456–1467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.; Zha, Z.; Ge, Z. Thermo-Responsive Polyplex Micelles with PEG Shells and PNIPAM Layer to Protect DNA Cores for Systemic Gene Therapy. In Non-Viral Gene Delivery Vectors: Methods and Protocols; Candiani, G., Ed.; Springer: New York, NY, USA, 2016; pp. 269–276. ISBN 978-1-4939-3718-9. [Google Scholar]
- Purushotham, S.; Chang, P.E.J.; Rumpel, H.; Kee, I.H.C.; Ng, R.T.H.; Chow, P.K.H.; Tan, C.K.; Ramanujan, R. V Thermoresponsive core-shell magnetic nanoparticles for combined modalities of cancer therapy. Nanotechnology 2009, 20, 305101–305112. [Google Scholar] [CrossRef]
- Kesti, M.; Müller, M.; Becher, J.; Schnabelrauch, M.; D’Este, M.; Eglin, D.; Zenobi-Wong, M. A versatile bioink for three-dimensional printing of cellular scaffolds based on thermally and photo-triggered tandem gelation. Acta Biomater. 2015, 11, 162–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, H.; Ramirez, C.M.; Miljkovic, N.; Li, H.; Rubin, J.P.; Marra, K.G. Thermosensitive injectable hyaluronic acid hydrogel for adipose tissue engineering. Biomaterials 2009, 30, 6844–6853. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brunelle, A.R.; Horner, C.B.; Low, K.; Ico, G.; Nam, J. Electrospun thermosensitive hydrogel scaffold for enhanced chondrogenesis of human mesenchymal stem cells. Acta Biomater. 2018, 66, 166–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- op’t Veld, R.C.; van den Boomen, O.I.; Lundvig, D.M.S.; Bronkhorst, E.M.; Kouwer, P.H.J.; Jansen, J.A.; Middelkoop, E.; Von den Hoff, J.W.; Rowan, A.E.; Wagener, F.A.D.T.G. Thermosensitive biomimetic polyisocyanopeptide hydrogels may facilitate wound repair. Biomaterials 2018, 181, 392–401. [Google Scholar] [CrossRef] [PubMed]
- Zimoch, J.; Padial, J.S.; Klar, A.S.; Vallmajo-Martin, Q.; Meuli, M.; Biedermann, T.; Wilson, C.J.; Rowan, A.; Reichmann, E. Polyisocyanopeptide hydrogels: A novel thermo-responsive hydrogel supporting pre-vascularization and the development of organotypic structures. Acta Biomater. 2018, 70, 129–139. [Google Scholar] [CrossRef]
- Hsieh, F.-Y.; Lin, H.-H.; Hsu, S. 3D bioprinting of neural stem cell-laden thermoresponsive biodegradable polyurethane hydrogel and potential in central nervous system repair. Biomaterials 2015, 71, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Mouser, V.H.M.; Abbadessa, A.; Levato, R.; Hennink, W.E.; Vermonden, T.; Gawlitta, D.; Malda, J. Development of a thermosensitive HAMA-containing bio-ink for the fabrication of composite cartilage repair constructs. Biofabrication 2017, 9, 15026–15055. [Google Scholar] [CrossRef]
- Shi, K.; Liu, Z.; Yang, C.; Li, X.-Y.; Sun, Y.-M.; Deng, Y.; Wang, W.; Ju, X.-J.; Xie, R.; Chu, L.-Y. Novel Biocompatible Thermoresponsive Poly(N-vinyl Caprolactam)/Clay Nanocomposite Hydrogels with Macroporous Structure and Improved Mechanical Characteristics. ACS Appl. Mater. Interfaces 2017, 9, 21979–21990. [Google Scholar] [CrossRef]
- Bhullar, S.K.; Lala, N.L.; Ramkrishna, S. Smart Biomaterials—A review. Rev. Adv. Mater. Sci 2015, 40, 303–314. [Google Scholar] [CrossRef]
- Ruskowitz, E.R.; Deforest, C.A. Photoresponsive biomaterials for targeted drug delivery and 4D cell culture. Nat. Rev. Mater. 2018, 3, 17087–17104. [Google Scholar] [CrossRef]
- Leung, S.J.; Romanowski, M. Light-activated content release from liposomes. Theranostics 2012, 2, 1020–1036. [Google Scholar] [CrossRef]
- Jerca, F.A.; Jerca, V.; Stancu, I.-C. Development and Characterization of Photoresponsive Polymers. In Polymer and Photonic Materials Towards Biomedical Breakthroughs; Springer International Publishing: Cham, Switzerland, 2018. [Google Scholar]
- Ercole, F.; Davis, T.P.; Evans, R.A. Photo-responsive systems and biomaterials: Photochromic polymers, light-triggered self-assembly, surface modification, fluorescence modulation and beyond. Polym. Chem. 2010, 1, 37–54. [Google Scholar] [CrossRef]
- Wu, S.; Butt, H.-J. Near-Infrared-Sensitive Materials Based on Upconverting Nanoparticles. Adv. Mater. 2016, 28, 1208–1226. [Google Scholar] [CrossRef]
- Linsley, C.S.; Wu, B.M. Recent advances in light-responsive on- demand drug-delivery systems. Ther. Deliv 2017, 8, 89–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandarab, H.M.D.; Burdette, S.C. Photoisomerization in different classes of azobenzene. Chem. Soc. Rev. 2012, 41, 1809–1825. [Google Scholar] [CrossRef]
- Udayabhaskararao, T.; Kundu, P.K.; Ahrens, J.; Klajn, R. Reversible Photoisomerization of Spiropyran on the Surfaces of Au25 Nanoclusters. ChemPhysChem 2015, 17, 1805–1809. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, Z.; Shah, A.; Siddiq, M.; Kraatz, H.B. Polymeric micelles as drug delivery vehicles. RSC Adv. 2014, 4, 17028–17038. [Google Scholar] [CrossRef]
- Madaan, K.; Kumar, S.; Poonia, N.; Lather, V.; Pandita, D. Dendrimers in drug delivery and targeting: Drug-dendrimer interactions and toxicity issues. J. Pharm. Bioallied Sci. 2014, 6, 139–150. [Google Scholar] [CrossRef]
- Alavi, M.; Karimi, N.; Safaei, M. Application of various types of liposomes in drug delivery systems. Adv. Pharm. Bull. 2017, 7, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Urban, P.; Pritzl, S.D.; Konrad, D.B.; Frank, J.A.; Pernpeintner, C.; Roeske, C.R.; Trauner, D.; Lohmüller, T. Light-Controlled Lipid Interaction and Membrane Organization in Photolipid Bilayer Vesicles. Langmuir 2018, 34, 13368–13374. [Google Scholar] [CrossRef]
- Yao, C.; Wang, P.; Li, X.; Hu, X.; Hou, J.; Wang, L.; Zhang, F. Near-Infrared-Triggered Azobenzene-Liposome/Upconversion Nanoparticle Hybrid Vesicles for Remotely Controlled Drug Delivery to Overcome Cancer Multidrug Resistance. Adv. Mater. 2016, 28, 9341–9348. [Google Scholar] [CrossRef]
- Liu, D.; Wang, S.; Xu, S.; Liu, H. Photocontrollable intermittent release of doxorubicin hydrochloride from liposomes embedded by azobenzene-contained glycolipid. Langmuir 2017, 33, 1004–1012. [Google Scholar] [CrossRef]
- Cui, Z.-K.; Phoeung, T.; Rousseau, P.-A.; Rydzek, G.; Zhang, Q.; Bazuin, C.G.; Lafleur, M. Nonphospholipid Fluid Liposomes with Switchable Photocontrolled Release. Langmuir 2014, 30, 10818–10825. [Google Scholar] [CrossRef]
- Pearson, S.; Vitucci, D.; Khine, Y.Y.; Dag, A.; Lu, H.; Save, M.; Billon, L.; Stenzel, M.H. Light-responsive azobenzene-based glycopolymer micelles for targeted drug delivery to melanoma cells. Eur. Polym. J. 2015, 69, 616–627. [Google Scholar] [CrossRef]
- Son, S.; Shin, E.; Kim, B.S. Light-responsive micelles of spiropyran initiated hyperbranched polyglycerol for smart drug delivery. Biomacromolecules 2014, 15, 628–634. [Google Scholar] [CrossRef]
- Petriashvili, G.; Devadze, L.; Zurabishvili, T.; Sepashvili, N.; Chubinidze, K. Light controlled drug delivery containers based on spiropyran doped liquid crystal micro spheres. Biomed. Opt. Express 2016, 7, 442–446. [Google Scholar] [CrossRef] [Green Version]
- Baroli, B. Photopolymerization of biomaterials: Issues and potentialities in drug delivery, tissue engineering, and cell encapsulation applications. J. Chem. Technol. Biotechnol. 2006, 81, 491–499. [Google Scholar] [CrossRef]
- Nguyen, K.T.; West, J.L. Photopolymerizable hydrogels for tissue engineering applications. Biomaterials 2002, 23, 4307–4314. [Google Scholar] [CrossRef]
- Cao, Z.; Bian, Q.; Chen, Y.; Liang, F.; Wang, G. Light-Responsive Janus-Particle-Based Coatings for Cell Capture and Release. ACS Macro Lett. 2017, 6, 1124–1128. [Google Scholar] [CrossRef]
- Yu, L.; Schlaich, C.; Hou, Y.; Zhang, J.; Noeske, P.-L.M.; Haag, R. Photoregulating Antifouling and Bioadhesion Functional Coating Surface Based on Spiropyran. Chem. A Eur. J. 2018, 24, 7742–7748. [Google Scholar] [CrossRef]
- Fedele, C.; Netti, P.A.; Cavalli, S. Azobenzene-based polymers: Emerging applications as cell culture platforms. Biomater. Sci. 2018, 6, 990–995. [Google Scholar] [CrossRef]
- Shi, P.; Ju, E.; Yan, Z.; Gao, N.; Wang, J.; Hou, J.; Zhang, Y.; Ren, J.; Qu, X. Spatiotemporal control of cell-cell reversible interactions using molecular engineering. Nat. Commun. 2016, 7, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Pennacchio, F.A.; Fedele, C.; De Martino, S.; Cavalli, S.; Vecchione, R.; Netti, P.A. Three-Dimensional Microstructured Azobenzene-Containing Gelatin as a Photoactuable Cell Confining System. ACS Appl. Mater. Interfaces 2018, 10, 91–97. [Google Scholar] [CrossRef]
- Lee, I.N.; Dobre, O.; Richards, D.; Ballestrem, C.; Curran, J.M.; Hunt, J.A.; Richardson, S.M.; Swift, J.; Wong, L.S. Photoresponsive Hydrogels with Photoswitchable Mechanical Properties Allow Time-Resolved Analysis of Cellular Responses to Matrix Stiffening. ACS Appl. Mater. Interfaces 2018, 10, 7765–7776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Brien, P.; Thomas, P.J. Nanoscience; Specialist Periodical Reports; Royal Society of Chemistry: Cambridge, UK, 2013; ISBN 9781849737623. [Google Scholar]
- Chen, Y.; Li, H.; Deng, Y.; Sun, H.; Ke, X.; Ci, T. Near-infrared light triggered drug delivery system for higher efficacy of combined chemo-photothermal treatment. Acta Biomater. 2017, 51, 374–392. [Google Scholar] [CrossRef] [PubMed]
- Guha, S.; Shaw, S.K.; Spence, G.T.; Roland, F.M.; Smith, B.D. Clean Photothermal Heating and Controlled Release from Near-Infrared Dye Doped Nanoparticles without Oxygen Photosensitization. Langmuir 2015, 31, 7826–7834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bao, Z.; Liu, X.; Liu, Y.; Liu, H.; Zhao, K. Near-infrared light-responsive inorganic nanomaterials for photothermal therapy. Asian J. Pharm. Sci. 2016, 11, 349–364. [Google Scholar] [CrossRef] [Green Version]
- Ou, Y.-C.; Webb, J.A.; Faley, S.; Shae, D.; Talbert, E.M.; Lin, S.; Cutright, C.C.; Wilson, J.T.; Bellan, L.M.; Bardhan, R. Gold Nanoantenna-Mediated Photothermal Drug Delivery from Thermosensitive Liposomes in Breast Cancer. ACS omega 2016, 1, 234–243. [Google Scholar] [CrossRef]
- Guerrero, A.R.; Hassan, N.; Escobar, C.A.; Albericio, F.; Kogan, M.J.; Araya, E. Gold nanoparticles for photothermally controlled drug release. Nanomedicine 2014, 9, 2023–2039. [Google Scholar] [CrossRef]
- Alkilany, A.M.; Thompson, L.B.; Boulos, S.P.; Sisco, P.N.; Murphy, C.J. Gold nanorods: Their potential for photothermal therapeutics and drug delivery, tempered by the complexity of their biological interactions. Adv. Drug Deliv. Rev. 2012, 64, 190–199. [Google Scholar] [CrossRef]
- Mathiyazhakan, M.; Wiraja, C.; Xu, C. A Concise Review of Gold Nanoparticles-Based Photo-Responsive Liposomes for Controlled Drug Delivery. Nano-Micro Lett. 2018, 10, 10–20. [Google Scholar] [CrossRef] [Green Version]
- Norouzi, H.; Khoshgard, K.; Akbarzadeh, F. In vitro outlook of gold nanoparticles in photo-thermal therapy: a literature review. Lasers Med. Sci. 2018, 33, 917–926. [Google Scholar] [CrossRef]
- Lajunen, T.; Viitala, L.; Kontturi, L.S.; Laaksonen, T.; Liang, H.; Vuorimaa-Laukkanen, E.; Viitala, T.; Le Guével, X.; Yliperttula, M.; Murtomäki, L.; et al. Light induced cytosolic drug delivery from liposomes with gold nanoparticles. J. Control. Release 2015, 203, 85–98. [Google Scholar] [CrossRef]
- Xing, R.; Liu, K.; Jiao, T.; Zhang, N.; Ma, K.; Zhang, R.; Zou, Q.; Ma, G.; Yan, X. An Injectable Self-Assembling Collagen-Gold Hybrid Hydrogel for Combinatorial Antitumor Photothermal/Photodynamic Therapy. Adv. Mater. 2016, 28, 3669–3676. [Google Scholar] [CrossRef] [PubMed]
- Martino, N.; Feyen, P.; Porro, M.; Bossio, C.; Zucchetti, E.; Ghezzi, D.; Benfenati, F.; Lanzani, G.; Antognazza, M.R. Photothermal cellular stimulation in functional bio-polymer interfaces. Sci. Rep. 2015, 5, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bao, C.; Zhu, L.; Lin, Q.; Tian, H. Building biomedical materials using photochemical bond cleavage. Adv. Mater. 2015, 27, 1647–1662. [Google Scholar] [CrossRef] [PubMed]
- Barhoumi, A.; Liu, Q.; Kohane, D.S. Ultraviolet light-mediated drug delivery: Principles, applications, and challenges. J. Control. Release 2015, 219, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Chin, A.L.; Zhong, Y.; Tong, R. Emerging strategies in near-infrared light triggered drug delivery using organic nanomaterials. Biomater. Sci. 2017, 5, 1491–1499. [Google Scholar] [CrossRef] [PubMed]
- Yan, B.; Boyer, J.-C.; Branda, N.R.; Zhao, Y. Near-Infrared Light-Triggered Dissociation of Block Copolymer Micelles Using Upconverting Nanoparticles. J. Am. Chem. Soc. 2011, 133, 19714–19717. [Google Scholar] [CrossRef]
- Klán, P.; Šolomek, T.; Bochet, C.G.; Blanc, A.; Givens, R.; Rubina, M.; Popik, V.; Kostikov, A.; Wirz, J. Photoremovable protecting groups in chemistry and biology: Reaction mechanisms and efficacy. Chem. Rev. 2013, 113, 119–191. [Google Scholar] [CrossRef]
- Liu, G.; Dong, C.-M.M. Photoresponsive Poly(S-(o-nitrobenzyl)-l-cysteine)-b-PEO from a l-Cysteine N-Carboxyanhydride Monomer: Synthesis, Self-Assembly, and Phototriggered Drug Release. Biomacromolecules 2012, 13, 1573–1583. [Google Scholar] [CrossRef]
- Zhang, D.; Liu, Z.; Konetski, D.; Wang, C.; Worrell, B.T.; Bowman, C.N. Liposomes formed from photo-cleavable phospholipids:: In situ formation and photo-induced enhancement in permeability. RSC Adv. 2018, 8, 14669–14675. [Google Scholar] [CrossRef] [Green Version]
- Chandra, B.; Subramaniam, R.; Mallik, S.; Srivastava, D.K. Formulation of photocleavable liposomes and the mechanism of their content release. Org. Biomol. Chem. 2006, 4, 1730–1740. [Google Scholar] [CrossRef]
- Bayer, A.M.; Alam, S.; Mattern-Schain, S.I.; Best, M.D. Triggered liposomal release through a synthetic phosphatidylcholine analogue bearing a photocleavable moiety embedded within the sn-2 acyl chain. Chem. A Eur. J. 2014, 20, 3350–3357. [Google Scholar] [CrossRef] [PubMed]
- Griffin, D.R.; Kasko, A.M. Photodegradable macromers and hydrogels for live cell encapsulation and release. J Am Chem Soc. 2012, 134, 13103–13107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, H.; Song, Z.; Chen, X. Photo-controllable molecular hydrogels for drug delivery. J. Nanosci. Nanotechnol. 2014, 14, 4837–4842. [Google Scholar] [CrossRef]
- Kloxin, A.M.; Kasko, A.M.; Salinas, C.N.; Anseth, K.S. Photodegradable hydrogels for dynamic tuning of physical and chemical properties. Science 2009, 324, 59–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azagarsamy, M.A.; McKinnon, D.D.; Alge, D.L.; Anseth, K.S. Coumarin-based photodegradable hydrogel: Design, synthesis, gelation, and degradation kinetics. ACS Macro Lett. 2014, 3, 515–519. [Google Scholar] [CrossRef]
- De Gracia Lux, C.; Lux, J.; Collet, G.; He, S.; Chan, M.; Olejniczak, J.; Foucault-Collet, A.; Almutairi, A. Short Soluble Coumarin Crosslinkers for Light-Controlled Release of Cells and Proteins from Hydrogels. Biomacromolecules 2015, 16, 3286–3296. [Google Scholar] [CrossRef]
- Kim, S.H.; Sun, Y.; Kaplan, J.A.; Grinstaff, M.W.; Parquette, J.R. Photo-crosslinking of a self-assembled coumarin-dipeptide hydrogel. New J. Chem. 2015, 39, 3225–3228. [Google Scholar] [CrossRef]
- Givens, R.S.; Rubina, M.; Wirz, J. Applications of p-hydroxyphenacyl (pHP) and coumarin-4-ylmethyl photoremovable protecting groups. Photochem. Photobiol. Sci. 2012, 11, 472–488. [Google Scholar] [CrossRef] [Green Version]
- Ngwuluka, N. Application of in situ polymerization for design and development of oral drug delivery systems. AAPS PharmSciTech 2010, 11, 1603–1611. [Google Scholar] [CrossRef] [Green Version]
- Williams, C.G.; Malik, A.N.; Kim, T.K.; Manson, P.N.; Elisseeff, J.H. Variable cytocompatibility of six cell lines with photoinitiators used for polymerizing hydrogels and cell encapsulation. Biomaterials 2005, 26, 1211–1218. [Google Scholar] [CrossRef]
- Bryant, S.J.; Nuttelman, C.R.; Anseth, K.S. Cytocompatibility of UV and visible light photoinitiating systems on cultured NIH/3T3 fibroblasts in vitro. J. Biomater. Sci. Polym. Ed. 2000, 11, 439–457. [Google Scholar] [CrossRef] [PubMed]
- Pereira, R.F.; Bártolo, P.J. 3D Photo-Fabrication for Tissue Engineering and Drug Delivery. Engineering 2015, 1, 90–112. [Google Scholar] [CrossRef] [Green Version]
- Hillel, A.T.; Unterman, S.; Nahas, Z.; Reid, B.; Coburn, J.M.; Axelman, J.; Chae, J.J.; Guo, Q.; Trow, R.; Thomas, A.; et al. Photoactivated Composite Biomaterial for Soft Tissue Restoration in Rodents and in Humans. Sci. Transl. Med. 2011, 3, 93ra67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, H.; Patel, A.; Gaharwar, A.K.; Mihaila, S.M.; Iviglia, G.; Mukundan, S.; Bae, H.; Yang, H.; Khademhosseini, A. Hyperbranched polyester hydrogels with controlled drug release and cell adhesion properties. Biomacromolecules 2013, 14, 1299–1310. [Google Scholar] [CrossRef] [Green Version]
- Milo, R.; Phillips, R. Cell Biology by the Numbers, 1st ed.; Garland Science Taylor and Francis Group: New York, NY, USA, 2015; ISBN 9780815345374. [Google Scholar]
- Ortega, A.L.; Mena, S.; Estrela, J.M. Glutathione in cancer cell death. Cancers 2011, 3, 1285–1310. [Google Scholar] [CrossRef] [Green Version]
- Gamcsik, M.P.; Kasibhatla, M.S.; Teeter, S.D.; Colvin, O.M. Glutathione levels in human tumors. Biomarkers 2012, 17, 671–691. [Google Scholar] [CrossRef]
- Su, Y.; Hu, Y.; Du, Y.; Huang, X.; He, J.; You, J.; Yuan, H.; Hu, F. Redox-responsive polymer-drug conjugates based on doxorubicin and chitosan oligosaccharide- g -stearic acid for cancer therapy. Mol. Pharm. 2015, 12, 1193–1202. [Google Scholar] [CrossRef]
- Nehate, C.; Nayal, A.; Koul, V. Redox Responsive Polymersomes for Enhanced Doxorubicin Delivery. ACS Biomater. Sci. Eng. 2018, 2, 511–517. [Google Scholar] [CrossRef]
- Thambi, T.; Park, J.H.; Lee, D.S. Stimuli-responsive polymersomes for cancer therapy. Biomater. Sci. 2016, 4, 55–69. [Google Scholar] [CrossRef]
- Zhi, X.; Liu, P.; Li, Y.; Li, P.; Yuan, J.; Lin, J. One-step fabricated keratin nanoparticles as pH and redox-responsive drug nanocarriers. J. Biomater. Sci. Polym. Ed. 2018, 29, 1920–1934. [Google Scholar] [CrossRef]
- Li, Q.; Yang, S.; Zhu, L.; Kang, H.; Qu, X.; Liu, R.; Huang, Y. Dual-stimuli sensitive keratin graft PHPMA as physiological trigger responsive drug carriers. Polym. Chem. 2015, 6, 2869–2878. [Google Scholar] [CrossRef]
- Senapati, S.; Mahanta, A.K.; Kumar, S.; Maiti, P. Controlled drug delivery vehicles for cancer treatment and their performance. Signal Transduct. Target. Ther. 2018, 3, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, X.; Cheng, Y.; Zhao, X.; Luo, Y.; Chen, J.; Yuan, W.-E. Advances in redox-responsive drug delivery systems of tumor microenvironment. J. Nanobiotechnology 2018, 16, 74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pietschnig, R. Polymers with pendant ferrocenes. Chem. Soc. Rev. 2016, 45, 5216–5231. [Google Scholar] [CrossRef] [Green Version]
- Wu, J.; Wang, L.; Yu, H.; Zain-ul-Abdin; Khan, R.U.; Haroon, M. Ferrocene-based redox-responsive polymer gels: Synthesis, structures and applications. J. Organomet. Chem. 2017, 828, 38–51. [Google Scholar] [CrossRef]
- Chen, J.; Huang, Y.; Ma, X.; Lei, Y. Functional self-healing materials and their potential applications in biomedical engineering. Adv Compos Hybrid Mater 2018, 1, 94–113. [Google Scholar] [CrossRef]
- Taylor, D.L.; in het Panhuis, M. Self-Healing Hydrogels. Adv. Mater. 2016, 28, 9060–9093. [Google Scholar] [CrossRef]
- Nakahata, M.; Takashima, Y.; Yamaguchi, H.; Harada, A. Redox-responsive self-healing materials formed from host-guest polymers. Nat. Commun. 2011, 2, 511–517. [Google Scholar] [CrossRef] [Green Version]
- Fang, Y.; Wang, C.F.; Zhang, Z.H.; Shao, H.; Chen, S. Robust self-healing hydrogels assisted by cross-linked nanofiber networks. Sci. Rep. 2013, 3, 2811–2818. [Google Scholar] [CrossRef]
- Wajs, E.; Nielsen, T.T.; Larsen, K.L.; Fragoso, A. Preparation of stimuli-responsive nano-sized capsules based on cyclodextrin polymers with redox or light switching properties. Nano Res. 2016, 9, 2070–2078. [Google Scholar] [CrossRef]
- Greene, A.F.; Danielson, M.K.; Delawder, A.O.; Liles, K.P.; Li, X.; Natraj, A.; Wellen, A.; Barnes, J.C. Redox-Responsive Artificial Molecular Muscles: Reversible Radical-Based Self-Assembly for Actuating Hydrogels. Chem. Mater. 2017, 29, 9498–9508. [Google Scholar] [CrossRef]
- Tamesue, S.; Noguchi, S.; Kimura, Y.; Endo, T. Reversing Redox Responsiveness of Hydrogels due to Supramolecular Interactions by Utilizing Double-Network Structures. ACS Appl. Mater. Interfaces 2018, 10, 27381–27390. [Google Scholar] [CrossRef] [PubMed]
- Riba-Moliner, M.; Gómez-Rodríguez, A.; Amabilino, D.B.; Puigmartí-Luis, J.; González-Campo, A. Functional supramolecular tetrathiafulvalene-based films with mixed valences states. Polymer (Guildf). 2016, 103, 251–260. [Google Scholar] [CrossRef]
- Schröder, H.V.; Schalley, C.A. Tetrathiafulvalene – a redox-switchable building block to control motion in mechanically interlocked molecules. Beilstein J. Org. Chem. 2018, 14, 2163–2185. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zeng, Y.; Yu, T.; Chen, J.; Yang, G.; Li, Y. Tetrathiafulvalene terminal-decorated PAMAM dendrimers for triggered release synergistically stimulated by redox and CB[7]. Langmuir 2014, 30, 718–726. [Google Scholar] [CrossRef]
- Bigot, J.; Charleux, B.; Cooke, G.; Fournier, D.; Woisel, P. Poly (N-isopropylacrylamide): A New Class of Amphiphilic Polymer for the Creation of Multistimuli Responsive Micelles. J. Am. Chem. Soc. 2010, 132, 10796–10801. [Google Scholar] [CrossRef]
- Ning, C.; Zhou, Z.; Tan, G.; Zhu, Y.; Mao, C. Electroactive polymers for tissue regeneration: Developments and perspectives. Prog. Polym. Sci. 2018. [Google Scholar] [CrossRef]
- Clancy, K.F.A.; Hardy, J.G. Gene Delivery with Organic Electronic Biomaterials. Curr. Pharm. Des. 2017, 23, 3614–3625. [Google Scholar]
- Svirskis, D.; Travas-Sejdic, J.; Rodgers, A.; Garg, S. Electrochemically controlled drug delivery based on intrinsically conducting polymers. J. Control. Release 2010, 146, 6–15. [Google Scholar] [CrossRef]
- Zhao, Y.H.; Niu, C.M.; Shi, J.Q.; Wang, Y.Y.; Yang, Y.M.; Wang, H.B. Novel conductive polypyrrole/silk fibroin scaffold for neural tissue repair. Neural Regen. Res. 2018, 13, 1455–1464. [Google Scholar] [CrossRef]
- Guex, A.G.; Puetzer, J.L.; Armgarth, A.; Littmann, E.; Stavrinidou, E.; Giannelis, E.P.; Malliaras, G.G.; Stevens, M.M. Highly porous scaffolds of PEDOT:PSS for bone tissue engineering. Acta Biomater. 2017, 62, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Gelmi, A.; Ljunggren, M.K.; Rafat, M.; Jager, E.W.H. Influence of conductive polymer doping on the viability of cardiac progenitor cells. J. Mater. Chem. B 2014, 2, 3860–3867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baumgartner, J.; Jönsson, J.I.; Jager, E.W.H. Switchable presentation of cytokines on electroactive polypyrrole surfaces for hematopoietic stem and progenitor cells. J. Mater. Chem. B 2018, 6, 4665–4675. [Google Scholar] [CrossRef] [Green Version]
- Balint, R.; Cassidy, N.J.; Cartmell, S.H. Conductive polymers: Towards a smart biomaterial for tissue engineering. Acta Biomater. 2014, 10, 2341–2353. [Google Scholar] [CrossRef] [PubMed]
- Fortunato, M.G.; De Maria, C.; Eglin, D.; Serra, T.; Vozzi, G. An ink-jet printed electrical stimulation platform for muscle tissue regeneration. Bioprinting 2018, 11, e00035. [Google Scholar] [CrossRef]
- Pires, F.; Ferreira, Q.; Rodrigues, C.A.V.; Morgado, J.; Ferreira, F.C. Neural stem cell differentiation by electrical stimulation using a cross-linked PEDOT substrate: Expanding the use of biocompatible conjugated conductive polymers for neural tissue engineering. Biochim. Biophys. Acta Gen. Subj. 2015, 1850, 1158–1168. [Google Scholar] [CrossRef]
- Hoop, M.; Chen, X.Z.; Ferrari, A.; Mushtaq, F.; Ghazaryan, G.; Tervoort, T.; Poulikakos, D.; Nelson, B.; Pané, S. Ultrasound-mediated piezoelectric differentiation of neuron-like PC12 cells on PVDF membranes. Sci. Rep. 2017, 7, 4028–4036. [Google Scholar] [CrossRef] [Green Version]
- Vannozzi, L.; Ricotti, L.; Filippeschi, C.; Sartini, S.; Coviello, V.; Piazza, V.; Pingue, P.; La Motta, C.; Dario, P.; Menciassi, A. Nanostructured ultra-thin patches for ultrasound-modulated delivery of anti-restenotic drug. Int. J. Nanomedicine 2015, 11, 69–92. [Google Scholar] [CrossRef] [Green Version]
- Kim, O.; Shin, T.J.; Park, M.J. Fast low-voltage electroactive actuators using nanostructured polymer electrolytes. Nat. Commun. 2013, 4, 2208. [Google Scholar] [CrossRef] [Green Version]
- Shin, S.R.; Jung, S.M.; Zalabany, M.; Kim, K.; Zorlutuna, P.; Kim, S.B.; Nikkhah, M.; Khabiry, M.; Azize, M.; Kong, J.; et al. Carbon-nanotube-embedded hydrogel sheets for engineering cardiac constructs and bioactuators. ACS Nano 2013, 7, 2369–2380. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.; Wu, C.; Zhang, Z.; Wu, W.; Wang, X.; Yu, Z. Synthesis, functionalization, and nanomedical applications of functional magnetic nanoparticles. Chinese Chem. Lett. 2018, 29, 1601–1608. [Google Scholar] [CrossRef]
- Tuttolomondo, M.V.; Villanueva, M.E.; Alvarez, G.S.; Desimone, M.F.; Díaz, L.E. Preparation of submicrometer monodispersed magnetic silica particles using a novel water in oil microemulsion: properties and application for enzyme immobilization. Biotechnol. Lett. 2013, 35, 1571–1577. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Fan, T.; Chen, J.; Su, J.; Zhi, X.; Pan, P.; Zou, L.; Zhang, Q. Magnetic bioinspired micro/nanostructured composite scaffold for bone regeneration. Colloids Surfaces B Biointerfaces 2019, 174, 70–79. [Google Scholar] [CrossRef]
- Ridi, F.; Bonini, M.; Baglioni, P. Magneto-responsive nanocomposites: Preparation and integration of magnetic nanoparticles into films, capsules, and gels. Adv. Colloid Interface Sci. 2014, 207, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Abu-Dief, A.M.; Abdel-Fatah, S.M. Development and functionalization of magnetic nanoparticles as powerful and green catalysts for organic synthesis. Beni-Suef Univ. J. Basic Appl. Sci. 2018, 7, 55–67. [Google Scholar] [CrossRef]
- Kayode, B.; Abdul, A. Journal of Magnetism and Magnetic Materials Recent advances in synthesis and surface modi fi cation of superparamagnetic iron oxide nanoparticles with silica. J. Magn. Magn. Mater. 2016, 416, 275–291. [Google Scholar] [CrossRef]
- Silva Diorato Teixeira de Mendonça, E.; Britto de Faria, A.C.; Loureiro Dias, S.C.; Aragón, F.F.H.; Mantilla, J.C.; Coaquira, J.A.H.; Dias, J.A. Effects of silica coating on the magnetic properties of magnetite nanoparticles. Surfaces and Interfaces 2018, 14, 34–43. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhen, B.; Li, H.; Feng, Y. Preparation of water-soluble magnetic nanoparticles with controllable silica coating. Chinese J. Chem. Eng. 2018, 26, 213–217. [Google Scholar] [CrossRef]
- Bui, T.Q.; Ngo, H.T.M.; Tran, H.T. Surface-protective assistance of ultrasound in synthesis of superparamagnetic magnetite nanoparticles and in preparation of mono-core magnetite-silica nanocomposites. J. Sci. Adv. Mater. Devices 2018, 3, 323–330. [Google Scholar] [CrossRef]
- Hou, Y.; Sellmyer, D.J. Magnetic Nanomaterials: Fundamentals, Synthesis and Applications; Wiley: Hoboken, NJ, USA, 2017; ISBN 9783527803248. [Google Scholar]
- Basith, M.A.; Quader, A.; Rahman, M.A.; Ngo, D.-T.; Mølhave, K.; Sinha, B.L.; Ahmmad, B.; Hirose, F. Simple top-down preparation of magnetic Bi0.9Gd0.1Fe1−xTixO3 nanoparticles by ultrasonication of multiferroic bulk material. Nanoscale 2014, 6, 14336–14342. [Google Scholar] [CrossRef] [Green Version]
- Laurent, S.; Forge, D.; Port, M.; Roch, A.; Robic, C.; Elst, L.V.; Muller, R.N. Magnetic Iron Oxide Nanoparticles: Synthesis, Stabilization, Vectorization, Physicochemical Characterizations, and Biological Applications. Chem. Rev. 2008, 108, 2064–2110. [Google Scholar] [CrossRef] [PubMed]
- Gul, S.; Khan, S.B.; Rehman, I.U.; Khan, M.A.; Khan, M.I. A Comprehensive Review of Magnetic Nanomaterials Modern Day Theranostics. Front. Mater. 2019, 6, 179. [Google Scholar] [CrossRef] [Green Version]
- Frey, N.A.; Peng, S.; Cheng, K.; Sun, S. Magnetic nanoparticles: synthesis, functionalization, and applications in bioimaging and magnetic energy storage. Chem. Soc. Rev. 2009, 38, 2532–2542. [Google Scholar] [CrossRef] [PubMed]
- Schmid, G.; Fenske, D. Metal clusters and nanoparticles. Philos. Trans. R. Soc. A Math. Phys. Eng. Sci. 2010, 368, 1207–1210. [Google Scholar] [CrossRef] [PubMed]
- Neoh, K.G.; Kang, E.T. Surface modification of magnetic nanoparticles for stem cell labeling. Soft Matter 2012, 8, 2057–2069. [Google Scholar] [CrossRef]
- Schladt, T.D.; Schneider, K.; Schild, H.; Tremel, W. Synthesis and bio-functionalization of magnetic nanoparticles for medical diagnosis and treatment. Dalt. Trans. 2011, 40, 6315–6343. [Google Scholar] [CrossRef]
- Thong-On, B.; Rutnakornpituk, B.; Wichai, U.; Rutnakornpituk, M. Magnetite nanoparticle coated with amphiphilic bilayer surfactant of polysiloxane and poly(poly(ethylene glycol) methacrylate). J. Nanoparticle Res. 2012, 14, 953–965. [Google Scholar] [CrossRef]
- Wang, X.; Tilley, R.D.; Watkins, J.J. Simple Ligand Exchange Reactions Enabling Excellent Dispersibility and Stability of Magnetic Nanoparticles in Polar Organic, Aromatic, and Protic Solvents. Langmuir 2014, 30, 1514–1521. [Google Scholar] [CrossRef]
- Lassalle, V.; Agotegaray, M. Silica-Coated Magnetic Nanoparticles: An Insight into Targeted Drug Delivery and Toxicology; Springer International Publishing: Cham, Switzerland, 2017; ISBN 978-3-319-50157-4. [Google Scholar]
- Gao, J.; Gu, H.; Xu, B. Multifunctional Magnetic Nanoparticles: Design, Synthesis, and Biomedical Applications. Acc. Chem. Res. 2009, 42, 1097–1107. [Google Scholar] [CrossRef]
- Singh, D.; Mcmillan, J.E.M.; Kabanov, A.V.; Sokolsky-Papkov, M.; Gendelman, H.E. Bench-to-bedside translation of magnetic nanoparticles. Nanomedicine 2014, 9, 501–516. [Google Scholar] [CrossRef] [Green Version]
- Xia, Y.; Sun, J.; Zhao, L.; Zhang, F.; Liang, X.J.; Guo, Y.; Weir, M.D.; Reynolds, M.A.; Gu, N.; Xu, H.H.K. Magnetic field and nano-scaffolds with stem cells to enhance bone regeneration. Biomaterials 2018, 183, 151–170. [Google Scholar] [CrossRef]
- Lu, J.-W.; Yang, F.; Ke, Q.-F.; Xie, X.-T.; Guo, Y.-P. Magnetic nanoparticles modified-porous scaffolds for bone regeneration and photothermal therapy against tumors. Nanomedicine Nanotechnology, Biol. Med. 2018, 14, 811–822. [Google Scholar] [CrossRef] [PubMed]
- Rotherham, M.; Henstock, J.R.; Qutachi, O.; El Haj, A.J. Remote regulation of magnetic particle targeted Wnt signaling for bone tissue engineering. Nanomedicine Nanotechnology, Biol. Med. 2018, 14, 173–184. [Google Scholar] [CrossRef] [PubMed]
- Ito, A.; Kamihira, M. Tissue engineering using magnetite nanoparticles. Prog. Mol. Biol. Transl. Sci. 2011, 104, 355–395. [Google Scholar] [CrossRef]
- Rao, K.M.; Kumar, A.; Han, S.S. Polysaccharide-based magnetically responsive polyelectrolyte hydrogels for tissue engineering applications. J. Mater. Sci. Technol. 2018, 34, 1371–1377. [Google Scholar] [CrossRef]
- Municoy, S.; Ibañez, I.L.; Durán, H.; Bellino, M.G. A catalase-magnetic switch for cell proliferation. RSC Adv. 2014, 4, 15077. [Google Scholar] [CrossRef]
- Mørup, S.; Hansen, M.F.; Frandsen, C. Magnetic Nanoparticles. In Reference Module in Materials Science and Materials Engineering; Elsevier: Amsterdam, The Netherlands, 2018; ISBN 978-0-12-374396-1. [Google Scholar]
- Zavisova, V.; Koneracka, M.; Gabelova, A.; Svitkova, B.; Ursinyova, M.; Kubovcikova, M.; Antal, I.; Khmara, I.; Jurikova, A.; Molcan, M.; et al. Effect of magnetic nanoparticles coating on cell proliferation and uptake. J. Magn. Magn. Mater. 2019, 472, 66–73. [Google Scholar] [CrossRef]
- Alipour, A.; Soran-Erdem, Z.; Utkur, M.; Sharma, V.K.; Algin, O.; Saritas, E.U.; Demir, H.V. A new class of cubic SPIONs as a dual-mode T1 and T2 contrast agent for MRI. Magn. Reson. Imaging 2018, 49, 16–24. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.M.; Park, C.W.; Park, S.; Kim, J.D. Cross-linked magnetic nanoparticles with a biocompatible amide bond for cancer-targeted dual optical/magnetic resonance imaging. Colloids Surfaces B Biointerfaces 2018, 161, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, G.R.; López-Abarrategui, C.; de la Serna Gómez, I.; Dias, S.C.; Otero-González, A.J.; Franco, O.L. Antimicrobial magnetic nanoparticles based-therapies for controlling infectious diseases. Int. J. Pharm. 2019, 555, 356–367. [Google Scholar] [CrossRef]












| Stimulus | Material | Drug | Reference |
|---|---|---|---|
| pH | Chitosan hydrogels | Anti-inflammatory factors and antibiotics | [58] |
| HEMA (2-hydroxyethyl methacrylate)/DMAEMA (dimethylaminoethyl methacrylate | [59] | ||
| Mesoporous bioglass (MBG) with hydroxyapatite (HAp) | Metformin hydrochloride (MH) | [60] | |
| Mesoporous ceramics with hydroxypatite (HAp) | Levofloxacin (Levo) | [61] | |
| Liposomes | Antagomir-10b y Paclitaxel (PTX) | [63,64,65] | |
| Hydrogels based on cytosine (C) and guanosine (G) modified hyaluronic acid (HA) via hydrogen bonding, with 1,6-hexamethylenediamine (HMDA) | [66] |
| Stimulus | Material | Drug | Reference |
|---|---|---|---|
| Temperature | Biodegradable citrate-based, poly(polyethyleneglycol citrate-co-N-isopropylacrylamide) (PPCN) mixed with gelatin (PPCNG) | BMP9 (growth differentiation factor) | [78] |
| 1-ethyl-3-(3-dimethyl-aminopropyl)-1-carbodiimide hydrochloride and N-hydroxysuccinimide | Doxorubicin (DOX) | [79] | |
| Nanoparticles based on gelatin, poly(lactide) and 1,2-dipalmitoyl-sn-glycero-3-phosphoethanolamine (DPPE) (gelatin-co-PLA-DPPE) | Doxorubicin (DOX) | [80] | |
| Chitosan/β-glycerophosphate | Venlafaxine hydrochloride | [81] | |
| Chitosan/collagen/β-glycerophosphate | [82] | ||
| Chitosan/β-glycerophosphate/hydroxyapatite | [83] | ||
| Methyl cellulose | [84] | ||
| Methyl cellulose and Collagen | [85] | ||
| Hydroxypropylmethyl cellulose associated with chondroitin-6-sulphate sodium | [86] | ||
| Polypeptides (ELP) | [87] | ||
| poly(N-alkyl substituted acrylamide) PNIPPAm | Doxorubicin (DOX) | [88] | |
| PNIPPAm with methacrylated hyaluronan | [89] | ||
| PEG and PNIPPAm | DNA | [90] | |
| Hyaluronic acid-g-poly(N-isopropylacrylamide) and PNIPAAm (AHA-g-PNIPAAm) | [91] | ||
| Chitosan (CS) and poly(ethylene glycol)-poly(N-isopropylacrylamide) (PEGPNIPAAm) | Mesenchymal stem cells (MSCs) | [72] | |
| Polyisocyanopeptide (PIC) | [93,94] | ||
| Polyurethane dispersion (PU2) | Neural stem cells (NSCs) | [95] | |
| Methacrylated hyaluronic acid (HAMA), methacrylated poly[N-(2-hydroxypropyl)methacrylamide mono/dilactate] (pHPMAlac)/polyethylene glycol (PEG) and polycaprolactone (PCL) | [96] | ||
| Poly(polyethyleneglycol citrate-co-N-isopropylacrylamide) (PPCN) mixed with gelatin (PPCNG) and Graphene oxide | MSCs with BMP9 | [73] | |
| Poly(N-vinyl caprolactam) (PVCL) with Clay nanocomposite | [97] |
| Stimulus | Material | Drug | Reference |
|---|---|---|---|
| Light | Azobenzene-glycolipid into liposome | [112] | |
| Liposomes formed by decyl-azobenzyl-triethylammonium and cholesterol sulfate | Hydrophobic content | [113] | |
| Micelles of polyglycerol using spiropyran | Hydrophobic content | [115,116] | |
| Polyacrylamide-based hydrogel with azobenzene | Mesenchymal stem cells | [124] | |
| Colloidal gold encapsulated in liposomes | [132] | ||
| Liposomes with multibranched gold nanoantennas | [129] | ||
| poly(3-hexylthiophene) | [136] | ||
| Micelle from poly(S-(o-nitrobenzyl)-L-cysteine)-b-poly(ethylene glycol) block copolymers | [142] | ||
| The nitrobenzyl group incorporated into liposomes | [143,145] | ||
| Poly(ethylene glycol) (PEG)-based hydrogel | [149] | ||
| PEG and hyaluronic acid (HA) | [157] | ||
| Polyesters hydrogels | [158] |
| Stimulus | Material | Drug | Reference |
|---|---|---|---|
| Redox | Glycolipid, chitosan, and stearic acid | Doxorubicin (DOX) | [162] |
| Polyethylene glycol and polycaprolactone | Doxorubicin (DOX) | [163] | |
| Keratin nanoparticles | [165] | ||
| Keratin grafted poly(N-(2-hydroxypropy l)methacrylamide) | Doxorubicin (DOX) | [166] | |
| Poly(acrylic acid) modified with cyclodextrins (pAA-CDs) | [173] | ||
| pAA with ferrocene (pAA-Fc) | |||
| Poly (1-vinyl-2-pyrrolidinone) modified with O-carboxymethyl chitosan and acrylamide | [174] | ||
| Ferrocene complexes with cyclodextrins | [175] | ||
| Oligoviologen | [176] | ||
| Viologen-cyclodextrin complexes | [177] | ||
| Polyamidoamine (PAMAM) dendrimers with tetrathiafulvalene (TTF) | [180] | ||
| TTF with poly(NIPAM) | [181] | ||
| Polypyrrole (PPy) | Interleukin IL-3 | [188] | |
| Poly (3,4-ethylenedioxythiophene) (PEDOT) and polystyrene-sulfonate (PSS) | [190,191] | ||
| Polymers polyvinylidene fluoride (PVDF) | [192] | ||
| Poly (lactic acid) and barium titanate nanoparticles | [193] | ||
| Carbon nanotube (SWCNT) | [194] | ||
| Carbon nanotube (CNT)-gelatin methacrylate (GelMA) | [195] |
| Stimulus | Material | Drug | Reference |
|---|---|---|---|
| Magnetic | Peptide-MNPs (magnetic nanoparticles) | [220] | |
| Iron oxide MNPs | [221] | ||
| MNPs with polysaccharide-based polymers | [222] | ||
| Enzyme-MNP complex | [223] | ||
| Iron oxide nanoparticles (USPION) | [216,226,227] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Municoy, S.; Álvarez Echazú, M.I.; Antezana, P.E.; Galdopórpora, J.M.; Olivetti, C.; Mebert, A.M.; Foglia, M.L.; Tuttolomondo, M.V.; Alvarez, G.S.; Hardy, J.G.; et al. Stimuli-Responsive Materials for Tissue Engineering and Drug Delivery. Int. J. Mol. Sci. 2020, 21, 4724. https://doi.org/10.3390/ijms21134724
Municoy S, Álvarez Echazú MI, Antezana PE, Galdopórpora JM, Olivetti C, Mebert AM, Foglia ML, Tuttolomondo MV, Alvarez GS, Hardy JG, et al. Stimuli-Responsive Materials for Tissue Engineering and Drug Delivery. International Journal of Molecular Sciences. 2020; 21(13):4724. https://doi.org/10.3390/ijms21134724
Chicago/Turabian StyleMunicoy, Sofia, María I. Álvarez Echazú, Pablo E. Antezana, Juan M. Galdopórpora, Christian Olivetti, Andrea M. Mebert, María L. Foglia, María V. Tuttolomondo, Gisela S. Alvarez, John G. Hardy, and et al. 2020. "Stimuli-Responsive Materials for Tissue Engineering and Drug Delivery" International Journal of Molecular Sciences 21, no. 13: 4724. https://doi.org/10.3390/ijms21134724
APA StyleMunicoy, S., Álvarez Echazú, M. I., Antezana, P. E., Galdopórpora, J. M., Olivetti, C., Mebert, A. M., Foglia, M. L., Tuttolomondo, M. V., Alvarez, G. S., Hardy, J. G., & Desimone, M. F. (2020). Stimuli-Responsive Materials for Tissue Engineering and Drug Delivery. International Journal of Molecular Sciences, 21(13), 4724. https://doi.org/10.3390/ijms21134724