Tissue Engineered Esophageal Patch by Mesenchymal Stromal Cells: Optimization of Electrospun Patch Engineering
Abstract
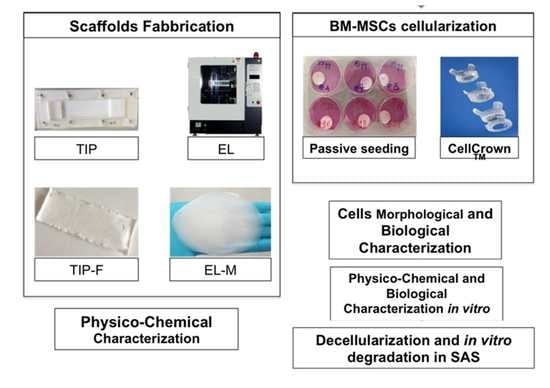
:1. Introduction
2. Results
2.1. p-MSC Characterization
2.2. Patches Physicochemical Characterization
2.2.1. Scanning Electron Microscopy (SEM)
2.2.2. Contact Angle (θ) Measurement
2.2.3. In Vitro Degradation Test
2.3. Biological Characterization
2.3.1. p-MSC Seeding on Floating Matrices
2.3.2. Cell Seeding Using CellCrownTM System
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Methods
4.2.1. Polymeric Patches Preparation
Temperature-Induced Precipitation (TIP) Technique
Electrospinning (EL) Technique
4.2.2. Prototypes Sterilization
4.2.3. p-MSC Expansion and Characterization
4.2.4. Patch Physicochemical Characterization
Scanning Electron Microscopy (SEM)
Contact Angle (θ) Measurements
In Vitro Degradation Test
Gel Permeation Chromatography
4.2.5. Biological Characterization
Cell Seeding on Floating Matrices
Cell Seeding Using CellCrownTM System
Cell Viability Determination
Cell Fixation Protocol for SEM Analysis
Staining by DAPI
4.2.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ASS | Artificial Simulated Saliva |
| Ctr- | Negative Control |
| Ctr+ | Positive Control |
| DM | Decellularized matrix |
| DCM | Dichloromethane |
| DMEM | Dulbecco’s Modified Eagle Medium |
| DMEM-LG | Dulbecco’s Modified Eagle Medium low glucose |
| DMF | N,N-dimethylformamide |
| DMSO | Dimethyl sulfoxide |
| ECM | Extra Cellular Matrix |
| EL | Electrospinning |
| EL-Ms | Electrospun Matrices |
| EMA/CHMP/CVMP/QWP/BWP | European Medicines Agency/Committee for Medicinal Products for Human Use/Committee for Medicinal Products for Veterinary Use/Quality Working Party/Biologics Working Party |
| FCS | Fetal Calf Serum |
| FITC | Fluorescein Isothiocyanate |
| GDA | Glutaraldehyde |
| GPC | Gel permeation Chromatography |
| HDMS | Hexamethyldisilazane |
| LENA | Laboratorio di Energia Nucleare Applicata |
| ML | Mass Loss |
| Mn | Number Average Molecular Weight |
| MNCs | Mononuclear cells |
| MsCs | Mesenchymal stem cells |
| MTT | (3-(4,5-Dimethylthiazol-2-yl)-2,5-Diphenyltetrazolium Bromide) |
| Mw | Weight average molecular weight |
| PBS | Phosphate-Buffered Saline |
| PCL | Caprolactone |
| PE | Phycoerythrin |
| PFA | Paraformaldehyde |
| PI | Polydispersity index (PI = Mw/Mn) |
| PLA | Polylactide |
| PLA-PCL | Polylactide-co-caprolactone |
| PLGA | poly lactide–co- glycolide |
| PLC | L-lactide/Caprolactone |
| p-MSCs | Porcine - bone marrow mesenchymal stem cells |
| pBM-MSCs | Porcine bone marrow- mesenchymal stem cells |
| RH | Relative Humidity |
| SCB | Sodium Cacodilate Buffer |
| SD | Standard Deviation |
| SEM | Scanning Electron Microscopy |
| TE | Tissue Engineering |
| THF | Tetrahydrofuran |
| TIP | Temperature-induced precipitation |
| TIP-Fs | Temperature induced precipitation polymeric films |
| UV–vis | Ultraviolet-visible |
| α-MEM | Alpha- Minimum Essential Medium Eagle |
References
- Zani, A.; Pierro, A.; Elvassore, N.; De Coppi, P. Tissue engineering: An option for esophageal replacement? Semin. Pediatric Surg. 2009, 18, 57–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arakelian, L.; Kanai, N.; Dua, K.; Durand, M.; Cattan, P.; Ohki, T. Esophageal Tissue Engineering: From Bench to Bedside: Esophageal Tissue Engineering; New York Academy of Sciences: New York, NY, USA, 2018; Volume 1434. [Google Scholar]
- Gust, L.; Ouattara, M.; Coosemans, W.; Nafteux, P.; Thomas, P.A.; D’Journo, X.B. European perspective in Thoracic surgery—Eso-coloplasty: When and how? J. Thorac. Dis. 2016, S387–S398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, H.; Wan, X.J.; Yang, C.Q. Comparison of endoscopic balloon dilation with metal stent placement in the treatment of achalasia. J. Dig. Dis. 2015, 16, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Londono, R.; Badylak, S.F. Regenerative Medicine Strategies for Esophageal Repair. Tissue Eng. Part. B Rev. 2015, 21, 393–410. [Google Scholar] [CrossRef] [Green Version]
- Chen, K.-N. Managing complications I: Leaks, strictures, emptying, reflux, chylothorax. J. Thorac. Dis. 2014, 6 (Suppl. 3), S355–S363. [Google Scholar] [CrossRef]
- Luc, G.; Charles, G.; Gronnier, C.; Cabau, M.; Kalisky, C.; Meulle, M.; Bareille, R.; Roques, S.; Couraud, L.; Rannou, J.; et al. Decellularized and matured esophageal scaffold for circumferential esophagus replacement: Proof of concept in a pig model. Biomaterials 2018, 175, 1–18. [Google Scholar] [CrossRef]
- Lin, M.; Firoozi, N.; Tsai, C.-T.; Wallace, M.B.; Kang, Y. 3D-printed flexible polymer stents for potential applications in inoperable esophageal malignancies. Acta Biomater. 2019, 83, 119–129. [Google Scholar] [CrossRef]
- Barron, M.R.; Blanco, E.W.; Aho, J.M.; Chakroff, J.; Johnson, J.; Cassivi, S.D.; Carey, W.A.; Wigle, D.A. Full-thickness oesophageal regeneration in pig using a polyurethane mucosal cell seeded graft. J. Tissue Eng. Regen. Med. 2018, 12, 175–185. [Google Scholar] [CrossRef] [Green Version]
- Langer, R.; Tirrell, D.A. Designing materials for biology and medicine. Nature 2004, 428, 487–492. [Google Scholar] [CrossRef]
- Atashrouz, S.; Hatampoor, A.; Yadegari, A.; Ghasemi, H.; Tayebi, L.; Rasoulianboroujeni, M. Mathematical modeling of oxygen transfer in porous scaffolds for stem cell growth: The effects of porosity, cell type, scaffold architecture and cell distribution. Mater. Chem. Phys. 2019, 222, 377–383. [Google Scholar] [CrossRef]
- Dorati, R.; DeTrizio, A.; Genta, I.; Grisoli, P.; Merelli, A.; Tomasi, C.; Conti, B. An experimental design approach to the preparation of pegylated polylactide-co-glicolide gentamicin loaded microparticles for local antibiotic delivery. Mater. Sci. Eng. C 2016, 58, 909–917. [Google Scholar] [CrossRef] [PubMed]
- Mallis, P.; Chachlaki, P.; Katsimpoulas, M.; Stavropoulos-Giokas, C.; Michalopoulos, E. Optimization of Decellularization Procedure in Rat Esophagus for Possible Development of a Tissue Engineered Construct. Bioengineering 2018, 6, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Badylak, S.; Meurling, S.; Chen, M.; Spievack, A.; Simmons-Byrd, A. Resorbable bioscaffold for esophageal repair in a dog model. J. Pediatric Surg. 2000, 35, 1097–1103. [Google Scholar] [CrossRef] [PubMed]
- Lopes, M.; Cabrita, A.; Ilharco, J.; Pessa, P.; Patrício, J. Grafts of Porcine Intestinal Submucosa for Repair of Cervical and Abdominal Esophageal Defects in the Rat. J. Investig. Surg. 2006, 19, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Jensen, T.; Wanczyk, H.; Sharma, I.; Mitchell, A.; Sayej, W.N.; Finck, C. Polyurethane scaffolds seeded with autologous cells can regenerate long esophageal gaps: An esophageal atresia treatment model. J. Pediatric Surg. 2019, 54, 1744–1754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensen, T.; Blanchette, A.; Vadasz, S.; Dave, A.; Canfarotta, M.; Sayej, W.N.; Finck, C. Biomimetic and synthetic esophageal tissue engineering. Biomaterials 2015, 57, 133–141. [Google Scholar] [CrossRef]
- Aikawa, M.; Miyazawa, M.; Okamoto, K.; Okada, K.; Akimoto, N.; Sato, H.; Koyama, I.; Yamaguchi, S.; Ikada, Y. A bioabsorbable polymer patch for the treatment of esophageal defect in a porcine model. J. Gastroenterol. 2013, 48, 822–829. [Google Scholar] [CrossRef]
- Jansen, P.; Klinge, U.; Anurov, M.; Titkova, S.; Mertens, P.; Jansen, M. Surgical Mesh as a Scaffold for Tissue Regeneration in the Esophagus. Eur. Surg. Res. 2004, 36, 104–111. [Google Scholar] [CrossRef]
- Pisani, S.; Dorati, R.; Conti, B.; Modena, T.; Bruni, G.; Genta, I. Design of copolymer PLA-PCL electrospun matrix for biomedical applications. React. Funct. Polym. 2018, 124, 77–89. [Google Scholar] [CrossRef]
- Theron, S.A.; Zussman, E.; Yarin, A.L. Experimental investigation of the governing parameters in the electrospinning of polymer solutions. Polymer 2004, 45, 2017–2030. [Google Scholar] [CrossRef]
- La Francesca, S.; Aho, J.M.; Barron, M.R.; Blanco, E.W.; Soliman, S.; Kalenjian, L.; Hanson, A.D.; Todorova, E.; Marsh, M.; Burnette, K.; et al. Long-term regeneration and remodeling of the pig esophagus after circumferential resection using a retrievable synthetic scaffold carrying autologous cells. Sci. Rep. 2018, 8, 4123. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.I. Adult mesenchymal stem cells for tissue engineering versus regenerative medicine. J. Cell. Physiol. 2007, 213, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Soliman, S.; Laurent, J.; Kalenjian, L.; Burnette, K.; Hedberg, B.; La Francesca, S. A multilayer scaffold design with spatial arrangement of cells to modulate esophageal tissue growth. J. Biomed. Mater. Res. Part. B Appl. Biomater. 2019, 107, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Sagnella, S.; Anderson, E.; Sanabria, N.; Marchant, R.E.; Kottke-Marchant, K. Human endothelial cell interaction with biomimetic surfactant polymers containing Peptide ligands from the heparin binding domain of fibronectin. Tissue Eng. 2005, 11, 226–236. [Google Scholar] [CrossRef] [Green Version]
- Sheridan, W.S.; Duffy, G.P.; Murphy, B.P. Mechanical characterization of a customized decellularized scaffold for vascular tissue engineering. J. Mech. Behav. Biomed. Mater. 2012, 8, 58–70. [Google Scholar] [CrossRef]
- Stefani, I.; Asnaghi, M.A.; Cooper-White, J.J.; Mantero, S. A double chamber rotating bioreactor for enhanced tubular tissue generation from human mesenchymal stem cells: A promising tool for vascular tissue regeneration. J. Tissue Eng. Regen. Med. 2018, 12, e42–e52. [Google Scholar] [CrossRef] [Green Version]
- Nasseri, B.A.; Pomerantseva, I.; Kaazempur-Mofrad, M.R.; Sutherland, F.W.; Perry, T.; Ochoa, E.; Thompson, C.A.; Mayer, J.E., Jr.; Oesterle, S.N.; Vacanti, J.P. Dynamic Rotational Seeding and Cell Culture System for Vascular Tube Formation. Tissue Eng. 2003, 9, 291–299. [Google Scholar] [CrossRef]
- Oda, A.; Takamiya, R.; Kaneko, R.; Yoshida, H.; Yanagita, Y.; Sekiguchi, H.; Nobe, Y.; Muramatsu, K. Utility of a rotation/revolution-type agitator for chondrocyte isolation during preparation of engineered cartilage. J. Biosci. Bioeng. 2019. [Google Scholar] [CrossRef]
- Chen, M.; Michaud, H.; Bhowmick, S. Controlled Vacuum Seeding as a Means of Generating Uniform Cellular Distribution in Electrospun Polycaprolactone (PCL) Scaffolds. J. Biomech. Eng. 2009, 131, 074521–074528. [Google Scholar] [CrossRef]
- Udelsman, B.; Hibino, N.; Villalona, G.A.; McGillicuddy, E.; Nieponice, A.; Sakamoto, Y.; Matsuda, S.; Vorp, D.A.; Shinoka, T.; Breuer, C.K. Development of an operator-independent method for seeding tissue-engineered vascular grafts. Tissue Eng. Part. C Methods 2011, 17, 731–736. [Google Scholar] [CrossRef]
- Beşkardeş, I.G.; Aydın, G.; Bektaş, Ş.; Cengiz, A.; Gümüşderelioğlu, M. A systematic study for optimal cell seeding and culture conditions in a perfusion mode bone-tissue bioreactor. Biochem. Eng. J. 2018, 132, 100–111. [Google Scholar] [CrossRef]
- Totonelli, G.; Maghsoudlou, P.; Fishman, J.M.; Orlando, G.; Ansari, T.; Sibbons, P.; Birchall, M.A.; Pierro, A.; Eaton, S.; De Coppi, P. Esophageal tissue engineering: A new approach for esophageal replacement. World J. Gastroenterol. 2012, 18, 6900–6907. [Google Scholar] [CrossRef] [PubMed]
- Takase, K.; Aikawa, M.; Okada, K.; Watanabe, Y.; Okamoto, K.; Sato, H.; Nonaka, K.; Yamaguchi, S.; Sakuramoto, S.; Koyama, I.; et al. Development of novel treatment with a bioabsorbable esophageal patch for benign esophageal stricture. Dis. Esophagus 2015, 28, 728–734. [Google Scholar] [CrossRef] [PubMed]
- Dorati, R.; De Trizio, A.; Marconi, S.; Ferrara, A.; Auricchio, F.; Genta, I.; Modena, T.; Benazzo, M.; Benazzo, A.; Volpato, G.; et al. Design of a Bioabsorbable Multilayered Patch for Esophagus Tissue Engineering. Macromol. Biosci. 2017, 17, 1600426. [Google Scholar] [CrossRef] [PubMed]
- Casasola, R.; Thomas, N.L.; Trybala, A.; Georgiadou, S. Electrospun poly lactic acid (PLA) fibres: Effect of different solvent systems on fibre morphology and diameter. Polymer 2014, 55, 4728–4737. [Google Scholar] [CrossRef] [Green Version]
- Dorati, R.; Pisani, S.; Maffeis, G.; Conti, B.; Modena, T.; Chiesa, E.; Bruni, G.; Musazzi, U.M.; Genta, I. Study on hydrophilicity and degradability of chitosan/polylactide-co-polycaprolactone nanofibre blend electrospun membrane. Carbohydr. Polym. 2018, 199, 150–160. [Google Scholar] [CrossRef]
- EMA/CHMP/CVMP/QWP/BWP/850374/2015. Guideline on the sterilisation of the medicinal product, 7 active substance, excipient and primary container. Eur. Med. Agency 2016, 3–15, 1–25.
- European Pharmacopeia 10.09, Chpt 5.1. Available online: https://www.edqm.eu/en/european_pharmacopoeia_10th_edition (accessed on 1 January 2020).
- Dorati, R.; Colonna, C.; Tomasi, C.; Genta, I.; Modena, T.; Faucitano, A.; Buttafava, A.; Conti, B. gamma-irradiation of PEGd,lPLA and PEG-PLGA multiblock copolymers: II. effect of oxygen and EPR investigation. AAPS PharmSciTech 2008, 9, 1110–1118. [Google Scholar] [CrossRef] [Green Version]
- Dorati, R.; Colonna, C.; Serra, M.; Genta, I.; Modena, T.; Pavanetto, F.; Perugini, P.; Conti, B. γ-Irradiation of PEGd,lPLA and PEG-PLGA multiblock copolymers: I. effect of irradiation doses. AAPS PharmSciTech 2008, 9, 718–725. [Google Scholar] [CrossRef]
- Dorati, R.; Genta, I.; Colzani, B.; Modena, T.; Bruni, G.; Tripodo, G.; Conti, B. Stability Evaluation of Ivermectin-Loaded Biodegradable Microspheres. AAPS PharmSciTech 2015, 16, 1129–1139. [Google Scholar] [CrossRef] [Green Version]
- Dorati, R.; Colonna, C.; Tomasi, C.; Bruni, G.; Genta, I.; Modena, T.; Conti, B. Long-Term Effect of Gamma Irradiation on the Functional Properties and Cytocompatibility of Multiblock Co-Polymer Films. J. Biomater. Sci. Polym. Ed. 2011, 23. [Google Scholar] [CrossRef]
- Conti, B.; Dorati, R.; Colonna, C.; Genta, I. Effects of ionizing radiation sterilization on microparticulate drug delivery systems based on poly-α-hydroxyacids: An overview. J. Drug Deliv. Sci. Technol. 2009, 19, 99–112. [Google Scholar] [CrossRef]
- Comite, P.; Cobianchi, L.; Avanzini, M.A.; Zonta, S.; Mantelli, M.; Achille, V.; De Martino, M.; Cansolino, L.; Ferrari, C.; Alessiani, M.; et al. Isolation and Ex Vivo Expansion of Bone Marrow–Derived Porcine Mesenchymal Stromal Cells: Potential for Application in an Experimental Model of Solid Organ Transplantation in Large Animals. Transplant. Proc. 2010, 42, 1341–1343. [Google Scholar] [CrossRef] [PubMed]







© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pisani, S.; Croce, S.; Chiesa, E.; Dorati, R.; Lenta, E.; Genta, I.; Bruni, G.; Mauramati, S.; Benazzo, A.; Cobianchi, L.; et al. Tissue Engineered Esophageal Patch by Mesenchymal Stromal Cells: Optimization of Electrospun Patch Engineering. Int. J. Mol. Sci. 2020, 21, 1764. https://doi.org/10.3390/ijms21051764
Pisani S, Croce S, Chiesa E, Dorati R, Lenta E, Genta I, Bruni G, Mauramati S, Benazzo A, Cobianchi L, et al. Tissue Engineered Esophageal Patch by Mesenchymal Stromal Cells: Optimization of Electrospun Patch Engineering. International Journal of Molecular Sciences. 2020; 21(5):1764. https://doi.org/10.3390/ijms21051764
Chicago/Turabian StylePisani, Silvia, Stefania Croce, Enrica Chiesa, Rossella Dorati, Elisa Lenta, Ida Genta, Giovanna Bruni, Simone Mauramati, Alberto Benazzo, Lorenzo Cobianchi, and et al. 2020. "Tissue Engineered Esophageal Patch by Mesenchymal Stromal Cells: Optimization of Electrospun Patch Engineering" International Journal of Molecular Sciences 21, no. 5: 1764. https://doi.org/10.3390/ijms21051764
APA StylePisani, S., Croce, S., Chiesa, E., Dorati, R., Lenta, E., Genta, I., Bruni, G., Mauramati, S., Benazzo, A., Cobianchi, L., Morbini, P., Caliogna, L., Benazzo, M., Avanzini, M. A., & Conti, B. (2020). Tissue Engineered Esophageal Patch by Mesenchymal Stromal Cells: Optimization of Electrospun Patch Engineering. International Journal of Molecular Sciences, 21(5), 1764. https://doi.org/10.3390/ijms21051764