Vitamin D Status in Patients before Thyroidectomy
Abstract
:1. Introduction
2. Results
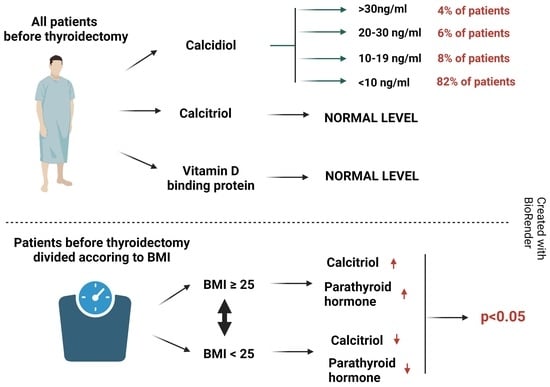
2.1. Vitamin D Status among All Patients before Thyroidectomy Procedure
2.2. Vitamin D Status between Patients with Normal and Increased BMI
2.3. Vitamin D Concentration and Type of Thyroid Tumor
2.4. Calcium Status after Surgery
3. Materials and Methods
3.1. Patients
3.2. Biochemical Analysis
3.3. Statistical Analysis
3.4. Vitamin D Suplemmentation
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Dağlar, G.; Kiliç, M.Ö.; Çelik, C.; Yüksel, C.; Terzioğlu, S.G.; Özden, S.; İçen, D. Is There A Relationship Between Vitamin D Status And Hypocalcemia After Total Thyroidectomy? Acta Endocrinol. 2016, 12, 291–296. [Google Scholar] [CrossRef]
- Biello, A.; Kinberg, E.C.; Wirtz, E.D. Thyroidectomy; StatPearls Publishing: Tampla, FL, USA, 2022. [Google Scholar]
- Dean, D.S.; Gharib, H. Epidemiology of Thyroid Nodules. Best Pract. Res. Clin. Endocrinol. Metab. 2008, 22, 901–911. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, E.J.; Mortimer, R.H. 6: Thyroid Nodules and Thyroid Cancer. Med. J. Aust. 2004, 180, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, W.; Kaplan, B.J. Diagnosis and Management of Patients with Thyroid Nodules. J. Surg. Oncol. 2002, 80, 157–170. [Google Scholar] [CrossRef] [PubMed]
- Seib, C.D.; Sosa, J.A. Evolving Understanding of the Epidemiology of Thyroid Cancer. Endocrinol. Metab. Clin. N. Am. 2019, 48, 23–35. [Google Scholar] [CrossRef]
- Molinaro, E.; Romei, C.; Biagini, A.; Sabini, E.; Agate, L.; Mazzeo, S.; Materazzi, G.; Sellari-Franceschini, S.; Ribechini, A.; Torregrossa, L.; et al. Anaplastic Thyroid Carcinoma: From Clinicopathology to Genetics and Advanced Therapies. Nat. Rev. Endocrinol. 2017, 13, 644–660. [Google Scholar] [CrossRef]
- Araque, K.A.; Gubbi, S.; Klubo-Gwiezdzinska, J. Updates on the Management of Thyroid Cancer. Horm. Metab. Res. 2020, 52, 562–577. [Google Scholar] [CrossRef]
- 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Available online: https://pubmed.ncbi.nlm.nih.gov/26462967 (accessed on 2 November 2022).
- Kant, R.; Davis, A.; Verma, V. Thyroid Nodules: Advances in Evaluation and Management. Am. Fam. Physician 2020, 102, 298–304. [Google Scholar]
- Axelsson, T.A.; Hrafnkelsson, J.; Olafsdottir, E.J.; Jonasson, J.G. Tall Cell Variant of Papillary Thyroid Carcinoma: A Population-Based Study in Iceland. Thyroid 2015, 25, 216–220. [Google Scholar] [CrossRef]
- Büttner, M.; Hinz, A.; Singer, S.; Musholt, T.J. Quality of Life of Patients More than 1 Year after Surgery for Thyroid Cancer. Hormones 2020, 19, 233–243. [Google Scholar] [CrossRef]
- Balentine, C.J.; Sippel, R.S. Outpatient Thyroidectomy: Is It Safe? Surg. Oncol. Clin. N. Am. 2016, 25, 61–75. [Google Scholar] [CrossRef] [PubMed]
- Smulever, A.; Pitoia, F. High Rate Incidence of Post-Surgical Adverse Events in Patients with Low-Risk Papillary Thyroid Cancer Who Did Not Accept Active Surveillance. Endocrine 2020, 69, 587–595. [Google Scholar] [CrossRef] [PubMed]
- Almquist, M.; Ivarsson, K.; Nordenström, E.; Bergenfelz, A. Mortality in Patients with Permanent Hypoparathyroidism after Total Thyroidectomy. Br. J. Surg. 2018, 105, 1313–1318. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.-W.; Chen, C.-W.; Yuan, K.-C.; Wang, I.-T.; Hung, F.-M.; Wang, A.-Y.; Wang, Y.-C.; Kuo, Y.-T.; Lin, Y.-C.; Shih, M.-C.; et al. Prevalence of Vitamin D Deficiency and Associated Factors in Critically Ill Patients: A Multicenter Observational Study. Front. Nutr. 2021, 8, 768804. [Google Scholar] [CrossRef]
- Choi, E.H.E.; Qeadan, F.; Alkhalili, E.; Lovato, C.; Burge, M.R. Preoperative Vitamin D Deficiency Is Associated with Increased Risk of Postoperative Hypocalcemia after Total Thyroidectomy. J. Investig. Med. 2021, 69, 1175–1181. [Google Scholar] [CrossRef]
- Lips, P. Vitamin D Physiology. Prog. Biophys. Mol. Biol. 2006, 92, 4–8. [Google Scholar] [CrossRef]
- Mackawy, A.M.H.; Al-ayed, B.M.; Al-rashidi, B.M. Vitamin D Deficiency and Its Association with Thyroid Disease. Int. J. Health Sci. 2013, 7, 267–275. [Google Scholar] [CrossRef]
- Dawson-Hughes, B.; Heaney, R.P.; Holick, M.F.; Lips, P.; Meunier, P.J.; Vieth, R. Estimates of Optimal Vitamin D Status. Osteoporos. Int. 2005, 16, 713–716. [Google Scholar] [CrossRef]
- Malik, M.Z.; Mirza, A.A.; Farooqi, S.A.; Chaudhary, N.A.; Waqar, M.; Bhatti, H.W. Role of Preoperative Administration of Vitamin D and Calcium in Postoperative Transient Hypocalcemia after Total Thyroidectomy. Cureus 2019, 11, e4579. [Google Scholar] [CrossRef]
- Tolone, S.; Roberto, R.; del Genio, G.; Brusciano, L.; Parmeggiani, D.; Amoroso, V.; Casalino, G.; Verde, I.; Bosco, A.; D’Alessandro, A.; et al. The Impact of Age and Oral Calcium and Vitamin D Supplements on Postoperative Hypocalcemia after Total Thyroidectomy. A Prospective Study. BMC Surg. 2013, 13 (Suppl. 2), S11. [Google Scholar] [CrossRef]
- Khundmiri, S.J.; Murray, R.D.; Lederer, E. PTH and Vitamin D. Compr. Physiol. 2016, 6, 561–601. [Google Scholar] [CrossRef] [PubMed]
- Pitroda, A.P.; Harris, S.S.; Dawson-Hughes, B. The Association of Adiposity with Parathyroid Hormone in Healthy Older Adults. Endocrine 2009, 36, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Valiña-Tóth, A.L.B.; Lai, Z.; Yoo, W.; Abou-Samra, A.; Gadegbeku, C.A.; Flack, J.M. Relationship of Vitamin D and Parathyroid Hormone to Obesity and Body Composition in African Americans. Clin. Endocrinol. 2010, 72, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, A.; Grant, W.B. Vitamin D and Cancer: An Historical Overview of the Epidemiology and Mechanisms. Nutrients 2022, 14, 1448. [Google Scholar] [CrossRef]
- Kim, D. The Role of Vitamin D in Thyroid Diseases. Int. J. Mol. Sci. 2017, 18, 1949. [Google Scholar] [CrossRef]
- Clinckspoor, I.; Verlinden, L.; Mathieu, C.; Bouillon, R.; Verstuyf, A.; Decallonne, B. Vitamin D in Thyroid Tumorigenesis and Development. Prog. Histochem. Cytochem. 2013, 48, 65–98. [Google Scholar] [CrossRef]
- Roskies, M.; Dolev, Y.; Caglar, D.; Hier, M.P.; Mlynarek, A.; Majdan, A.; Payne, R.J. Vitamin D Deficiency as a Potentially Modifiable Risk Factor for Thyroid Cancer. J. Otolaryngol. Head Neck Surg. 2012, 41, 160–163. [Google Scholar]
- Sahin, M.; Uçan, B.; Giniş, Z.; Topaloğlu, O.; Güngüneş, A.; Bozkurt, N.Ç.; Arslan, M.S.; Ünsal, İ.Ö.; Akkaymak, E.T.; Demirci, T.; et al. Vitamin D3 Levels and Insulin Resistance in Papillary Thyroid Cancer Patients. Med. Oncol. 2013, 30, 589. [Google Scholar] [CrossRef]
- Kim, J.R.; Kim, B.H.; Kim, S.M.; Oh, M.Y.; Kim, W.J.; Jeon, Y.K.; Kim, S.S.; Lee, B.J.; Kim, Y.K.; Kim, I.J. Low Serum 25 Hydroxyvitamin D Is Associated with Poor Clinicopathologic Characteristics in Female Patients with Papillary Thyroid Cancer. Thyroid 2014, 24, 1618–1624. [Google Scholar] [CrossRef]
- Stepien, T.; Krupinski, R.; Sopinski, J.; Kuzdak, K.; Komorowski, J.; Lawnicka, H.; Stepien, H. Decreased 1-25 Dihydroxyvitamin D3 Concentration in Peripheral Blood Serum of Patients with Thyroid Cancer. Arch. Med. Res. 2010, 41, 190–194. [Google Scholar] [CrossRef]
- Penna-Martinez, M.; Ramos-Lopez, E.; Stern, J.; Kahles, H.; Hinsch, N.; Hansmann, M.-L.; Selkinski, I.; Grünwald, F.; Vorländer, C.; Bechstein, W.O.; et al. Impaired Vitamin D Activation and Association with CYP24A1 Haplotypes in Differentiated Thyroid Carcinoma. Thyroid 2012, 22, 709–716. [Google Scholar] [CrossRef] [PubMed]
- Penna-Martinez, M.; Ramos-Lopez, E.; Stern, J.; Hinsch, N.; Hansmann, M.-L.; Selkinski, I.; Grünwald, F.; Vorländer, C.; Wahl, R.A.; Bechstein, W.O.; et al. Vitamin D Receptor Polymorphisms in Differentiated Thyroid Carcinoma. Thyroid 2009, 19, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Shapses, S.A.; Lee, E.J.; Sukumar, D.; Durazo-Arvizu, R.; Schneider, S.H. The Effect of Obesity on the Relationship Between Serum Parathyroid Hormone and 25-Hydroxyvitamin D in Women. J. Clin. Endocrinol. Metab. 2013, 98, E886–E890. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, M.; Karwasra, R.K.; Parshad, S. Effect of Preoperative Vitamin D Deficiency on Postoperative Hypocalcemia after Thyroid Surgery. Thyroid Res. 2014, 7, 8. [Google Scholar] [CrossRef]
- Henn, M.; Martin-Gorgojo, V.; Martin-Moreno, J.M. Vitamin D in Cancer Prevention: Gaps in Current Knowledge and Room for Hope. Nutrients 2022, 14, 4512. [Google Scholar] [CrossRef]


| Vitamin D Status | Normal BMI | Incresed BMI | p | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| 25-OHD [ng/mL] | 8.55 | 40.04 | 4.25 | 44.21 | 0.17 |
| 1.25-(OH)2D [pg/mL] | 44.77 | 5.73 | 53.4 | 8.03 | 0.01 |
| VDBP [ng/mL] | 29.77 | 22.11 | 30.37 | 23.20 | 0.57 |
| PTH [pg/mL] | 15.45 | 17.72 | 24.4 | 24.6 | 0.02 |
| Vitamin D Status | Benign Nodules | Thyroid Cancers | p | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| 25-OHD [ng/mL] | 4.96 | 2.51 | 4.25 | 2.49 | 0.31 |
| 1.25-OHD [pg/mL] | 48.51 | 14.95 | 49.51 | 16.71 | 0.45 |
| VDBR [ng/mL] | 30.28 | 14.40 | 29.63 | 8.75 | 0.62 |
| Calcium Status | Before Surgery | After Surgery | p | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| Ca [mmol/L] | 1.19 | 0.16 | 1.09 | 0.17 | 0.002 |
| Patients Characteristics n = 167 | Median | IQR |
|---|---|---|
| Age [years] | 48 | 24 |
| Men [%] | 29 | - |
| Benign nodules [%] | 79 | - |
| Thyroid cancers [%] | 21 | - |
| Body mass index (BMI) [kg/m2], * (18.5–25) | 27.76 | 7.79 |
| TSH [uIU/mL], * (0.27–2.4) | 1.29 | 0.78 |
| Creatinine [mg/dL], * (0.5–0.9) | 0.72 | 0.18 |
| FT3 [pg/mL], * (2–4.4) | 3.16 | 0.46 |
| FT4 [ng/dL], * (0.93–1.7) | 1.28 | 0.29 |
| PTH [pg/mL], * (15–65) | 19.7 | 22.18 |
| Ca [mmol/L], * (1.0–1.3) | 1.19 | 0.16 |
| 25-OHD [ng/mL], * (0–30) | 6.13 | 2.51 |
| 1,25-(OH)2D [pg/mL] * (20–60) | 48.69 | 15.17 |
| VDBP [ng/mL] | 30.12 | 14.13 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maciejewska-Markiewicz, D.; Kochman, J.; Jakubczyk, K.; Bargiel, P.; Szlosser, Z.; Stachowska, E.; Markowska, M.; Bucka, A.; Czapla, N.; Petriczko, J.; et al. Vitamin D Status in Patients before Thyroidectomy. Int. J. Mol. Sci. 2023, 24, 3228. https://doi.org/10.3390/ijms24043228
Maciejewska-Markiewicz D, Kochman J, Jakubczyk K, Bargiel P, Szlosser Z, Stachowska E, Markowska M, Bucka A, Czapla N, Petriczko J, et al. Vitamin D Status in Patients before Thyroidectomy. International Journal of Molecular Sciences. 2023; 24(4):3228. https://doi.org/10.3390/ijms24043228
Chicago/Turabian StyleMaciejewska-Markiewicz, Dominika, Joanna Kochman, Karolina Jakubczyk, Piotr Bargiel, Zbigniew Szlosser, Ewa Stachowska, Marta Markowska, Anna Bucka, Norbert Czapla, Jan Petriczko, and et al. 2023. "Vitamin D Status in Patients before Thyroidectomy" International Journal of Molecular Sciences 24, no. 4: 3228. https://doi.org/10.3390/ijms24043228
APA StyleMaciejewska-Markiewicz, D., Kochman, J., Jakubczyk, K., Bargiel, P., Szlosser, Z., Stachowska, E., Markowska, M., Bucka, A., Czapla, N., Petriczko, J., Surówka, A., Hertman, S., Puchalski, P., & Prowans, P. (2023). Vitamin D Status in Patients before Thyroidectomy. International Journal of Molecular Sciences, 24(4), 3228. https://doi.org/10.3390/ijms24043228