Web of Objects Based Ambient Assisted Living Framework for Emergency Psychiatric State Prediction
Abstract
:1. Introduction
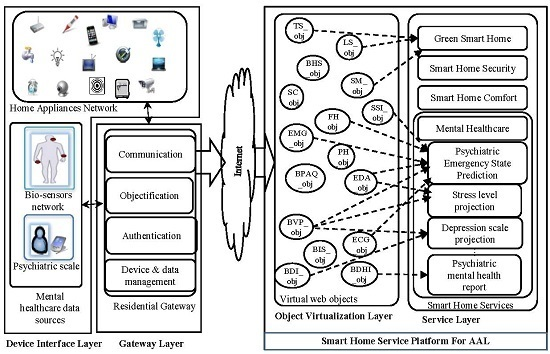
- Ambient assisted living framework: A web of objects-based smart home framework is presented in Section 3 for in-home personalized psychiatric care. In order to predict and monitor an emergency psychiatric state, collaboration among the objects is required. Therefore, a mental healthcare ontology is developed for presenting and extracting semantic relationships among the web of objects in a psychiatric care scenario. The framework enables a platform to cooperate, harmonize and share the mental healthcare objects for ambient assisted living services (e.g., emergency psychiatry).
- Emergency psychiatric state prediction: Decoding the psychiatric state of a patient through indirect channels of non-invasive biosensors is challenging. The discriminative features of putative risk factors for emergency psychiatric states are extracted from biosensor observations. For structured prediction, the emergency psychiatric states are modeled through an HMM. The psychophysiological features along with the psychometric features and patient histories are used as the observations to predict psychiatric state. Additionally, an emergency psychiatric state prediction algorithm is proposed for inferring the risk of psychiatric emergency. The probabilistic model parameters are estimated, and the accuracy of the model is validated over a training and testing dataset. The prototype is developed and tested.
2. Literature Review and Related Works
2.1. Emergency Psychiatry
2.2. Related Works
3. Materials and Methods
3.1. Web of Objects-Based Smart Home Framework for Ambient Assisted Living
3.1.1. Device Interface Layer
3.1.2. Gateway Layer
3.1.3. Object Virtualization Layer
3.1.4. Service Layer
PREFIX men:<http://semanticsweb.org/ontologies/mentalhealth.owl> PREFIX kosis:<http://kosis.kr/DeathsByCause/rdf-schema> Select? FamilyHistory Where? FamilyHistory men:G.H.Park men: Relatives koisis:DeathCause
|———————-| | Family History | |———————-|———————————————————| |men:Father: C.H. Park koisis:DeathCause:Assassination | |men:Mother: Y.S. Yuk koisis:DeathCause:Assassination | |men:Brother: J.M. Park koisis: DeathCause: | |men:Sister: G.Y. Park koisis: DeathCause: | |———————————————————————————|
3.2. Prediction of Psychiatric State
3.2.1. Emergency Psychiatric State Modeling
3.2.2. Data Collection
3.2.3. Feature Extraction
3.2.4. Training and Validation
3.2.5. Prediction of Emergency Psychiatric State
| Algorithm 1: Psychiatric state prediction. |
 |
- (a)
- The run lengths of each of the individual state were counted, and the state having the LRL was considered as the candidate state, as presented in Steps 3 to 6 of Algorithm 1 and in Row 2 of Table 1.
- (b)
- The frequencies of each of the individual states in Q were counted, and the state having the HFC was considered as the candidate state as presented in Step 2 of Algorithm 1, Algorithm 2 and in Row 3 of Table 1.
- (c)
- The state corresponding to the most recent time slot (i.e., ) was the MRS and was also considered as the candidate state as presented in Step 7 of Algorithm 1 and in Row 4 of Table 1.
| Algorithm 2: The Relax(S, Q) procedure. |
 |
4. Prototype Implementation and Performance Evaluation
4.1. Prototype Implementation
4.2. Performance Evaluation
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| A | Atypical |
| AAL | Ambient Assisted Living |
| Acc | Accuracy |
| AUC | Area Under the ROC Curve |
| BDI | Beck Depression Inventory |
| BVP | Blood Volume Pulse |
| BDHI | Buss–Durkee Hostility Inventory |
| BHS | Beck Hopelessness Scale |
| BIS | Baratt’s Impulsiveness Scale |
| BPAQ | Buss–Perry Aggression Questionnaire |
| BDHI | Buss–Durkee Hostility Inventory |
| CI | Confidence Interval |
| CRF | Conditional Random Field |
| DOR | Diagnostic Odds Ratio |
| DSM | Diagnostic and Statistical Manual of Mental Disorders |
| E | Emergency |
| EDA | Electro-Dermal Activity |
| ECG | Electrocardiogram |
| EMG | Electromyography |
| FNR | False Negative Error Rate |
| FPR | False Positive Error Rate |
| FM | F-measure |
| FP | False Positive |
| FN | False Negative |
| FH | Family History |
| GDA | Generalized Discriminant Analysis |
| GAD | Generalized Anxiety Disorder |
| HMM | Hidden Markov Model |
| HRSD | Hamilton Rating Scale for Depression |
| HFC | Highest Frequency Count |
| LS | Light Sensor |
| LRL | Longest Run Length |
| MRS | Most Recent Candidate State |
| mRMR | minimal-Redundancy-Maximal-Relevance |
| MV | Majority Voting |
| N | Normal |
| PH | Patients’ History |
| PHQ | Patient Health Questionnaire |
| PCA | Principal Component Analysis |
| ROC | Receiver Operating Characteristic |
| SOA | Service Oriented Architecture |
| SM | Smart Meter |
| SC | Smart Camera |
| SSI | Scale of Suicide Ideation |
| SCST | Stress and Coping Self-Test |
| SVI | Stochastic Variational Inference |
| SWLDA | Stepwise Linear Discriminant Analysis |
| Sen | Sensitivity |
| Spe | Specificity |
| TP | True Positive |
| TN | True Negative |
| TS | Temperature Sensor |
| VPC | Viterbi Path Count |
| WoO | Web of Objects |
References
- Trček, D. Wireless Sensors Grouping Proofs for Medical Care and Ambient Assisted-Living Deployment. Sensors 2016, 16, 33. [Google Scholar] [CrossRef] [PubMed]
- Uddin, M.Z.; Kim, T.S.; Kim, J.T. A spatiotemporal robust approach for human activity recognition. Int. J. Adv. Robot. Syst. 2013, 10, 502–512. [Google Scholar]
- Kau, L.J.; Chen, C.S. A smart phone-based pocket fall accident detection, positioning, and rescue system. IEEE J. Biomed. Health Inform. 2015, 19, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.M.; Lee, J.H.; Huh, E.N. An efficient model for smart home by the virtualization of wireless sensor network. Int. J. Distrib. Sens. Netw. 2013, 2013, 1715–1717. [Google Scholar] [CrossRef] [PubMed]
- Fahim, M.; Idris, M.; Ali, R.; Nugent, C.; Kang, B.; Huh, E.N.; Lee, S. ATHENA: A personalized platform to promote an active lifestyle and wellbeing based on physical, mental and social health primitives. Sensors 2014, 14, 9313–9329. [Google Scholar] [CrossRef] [PubMed]
- Dawadi, P.N.; Cook, D.J.; Schmitter-Edgecombe, M. Automated cognitive health assessment using smart home monitoring of complex tasks. IEEE Trans. Syst. Man Cybern. Syst. 2013, 43, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.L.; Liao, C.F.; Fu, L.C. Service-oriented smart-home architecture based on OSGi and mobile-agent technology. IEEE Trans. Syst Man Cybern. Part C Appl. Rev. 2007, 37, 193–205. [Google Scholar] [CrossRef]
- Shamszaman, Z.U.; Ara, S.S.; Chong, I.; Jeong, Y.K. Web-of-Objects (WoO)-based context aware emergency fire management systems for the Internet of Things. Sensors 2014, 14, 2944–2966. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.G.R.; Haw, R.; Hong, C.S. Emergency Psychiatric State Prediction for Ambient Assisted Living. In Proceedings of the IEEE International Conference on Consumer Electronics, Las Vegas, NV, USA, 9–12 January 2015; pp. 235–236.
- Beck, A.T.; Robert, A.S.; Brown, G.K. Manual for the Beck Depression Inventory-II; TX, Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Koller, D.; Friedman, N. Probabilistic Graphical Models: Principles and Techniques, 2nd ed.; Dietterich, T., Bishop, C., Heckerman, D., Jordan, M., Kearns, M., Eds.; The MIT Press: Cambridge, MA, USA; London, UK, 2009; pp. 202–675. [Google Scholar]
- Alam, M.G.R.; Cho, E.J.; Huh, E.N.; Hong, C.S. Cloud Based Mental State Monitoring System for Suicide Risk Reconnaissance Using Wearable Bio-sensors. In Proceedings of the 8th International Conference on Ubiquitous Information Management and Communication, Siem Reap, Cambodia, 9–11 January 2014; p. 56.
- Mann, J.J.; Waternaux, C.; Haas, G.L.; Malone, K.M. Toward a clinical model of suicidal behavior in psychiatric patients. Am. J. Psychiatry 1999, 156, 181–189. [Google Scholar] [PubMed]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The measurement of pessimism: the Hopelessness Scale. J. Consult. Clin. Psychol. 1974, 42, 861–865. [Google Scholar] [CrossRef] [PubMed]
- Moore, P.; Little, M.; McSharry, P.; Geddes, J.; Goodwin, G. Forecasting Depression in Bipolar Disorder. IEEE Trans. Biomed. Eng. 2012, 59, 2801–2807. [Google Scholar] [CrossRef] [PubMed]
- Bruckner, D.; Zeilinger, H.; Dietrich, D. Cognitive automation—Survey of novel artificial general intelligence methods for the automation of human technical environments. IEEE Trans. Ind. Inform. 2012, 8, 206–215. [Google Scholar] [CrossRef]
- Mayora, O. The MONARCA Project for Bipolar Disorder Treatment. J. CyberTher. Rehabil. 2011, 1, 14–15. [Google Scholar]
- Dobscha, S.K.; Corson, K.; Pruitt, S.; Crutchfield, M.; Gerrity, M.S. Measuring depression and pain with home health monitors. Telemed. J. E-Health 2006, 12, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef] [PubMed]
- Kazis, L.; Skinner, K.; Rogers, W. Health status of veterans: Physical and mental component summary scores (SF-36V). In National Survey of Ambulatory Care Patients. Executive Report; Veterans Health Administration: Washington, DC, USA, 1998. [Google Scholar]
- Niculescu, H.L.; Levey, D.F.; Ayalew, M.; Palmer, L.; Gavrin, L.M.; Jain, N.; Winiger, E.; Bhosrekar, S.; Shankar, G.; Rade, M.; et al. Discovery and validation of blood biomarkers for suicidality. Mol. Psychiatry 2013, 18, 1249–1264. [Google Scholar] [CrossRef] [PubMed]
- Cornella, K.S.; Gravenhorst, F.; Schumm, J.; Arnrich, B.; Tröster, G. Towards long term monitoring of electrodermal activity in daily life. Pers. Ubiquitous Comput. 2013, 17, 261–271. [Google Scholar]
- Imaoka, K.; Inoue, H.; Inoue, Y.; Hazama, H.; Tanaka, T.; Yamane, N. R-R Intervals of ECG in Depression. Psychiatry Clin. Neurosci. 1985, 39, 485–487. [Google Scholar] [CrossRef]
- Reilly, J.G.; Ayis, S.A.; Ferrier, I.N.; Jones, S.J.; Thomas, S.H.L. QTc-interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet 2000, 355, 1048–1052. [Google Scholar] [CrossRef]
- Riseberg, J.; Klein, J.; Fernandez, R.; Picard, R.W. Frustrating the user on purpose: Using bio-signals in a pilot study to detect the user’s emotional state. In Proceedings of the CHI 98 Conference Summary on Human Factors in Computing Systems, Los Angeles, CA, USA, 18–23 April 1998; pp. 227–228.
- Buss, A.H.; Perry, M. The aggression questionnaire. J. Pers. Soc. Psychol. 1992, 63, 452. [Google Scholar] [CrossRef] [PubMed]
- Patton, J.H.; Stanford, M.S. Factor structure of the Barratt impulsiveness scale. J. Clin. Psychol. 1995, 51, 768–774. [Google Scholar] [CrossRef]
- Bushman, B.J.; Cooper, H.M.; Lemke, K.M. Meta-analysis of factor analyses: An illustration using the Buss-Durkee Hostility Inventory. Pers. Soc. Psychol. Bull. 1991, 17, 344–349. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Ranieri, W. Scale for Suicide Ideation: Psychometric Properties of a self-report version. J. Clin. Psychol. 1998, 44, 499–505. [Google Scholar] [CrossRef]
- Khan, A.W.; Abdullah, A.H.; Razzaque, M.A.; Bangash, J.I. VGDRA: A virtual grid-based dynamic routes adjustment scheme for mobile sink-based wireless sensor networks. IEEE Sens. J. 2015, 15, 526–534. [Google Scholar] [CrossRef]
- Haghighi, P.D.; Burstein, F.; Zaslavsky, A.; Arbon, P. Development and evaluation of ontology for intelligent decision support in medical emergency management for mass gatherings. Decis. Support Syst. 2013, 54, 1192–1204. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Gibbon, M.E.; Skodol, A.E.; Williams, J.B.; First, M.B. DSM-IV-TR Casebook: A Learning Companion to the Diagnostic and Statistical Manual of Mental Disorders (Text Rev.); American Psychiatric Publishing, Inc.: Washington, DC, USA, 2002. [Google Scholar]
- Guenterberg, E.; Yang, A.Y.; Ghasemzadeh, H.; Jafari, R.; Bajcsy, R.; Sastry, S.S. A method for extracting temporal parameters based on hidden Markov models in body sensor networks with inertial sensors. IEEE Trans. Inf. Technol. Biomed. 2009, 13, 1019–1030. [Google Scholar] [CrossRef] [PubMed]
- Uddin, M.Z. Human activity recognition using segmented body part and body joint features with hidden Markov models. Multimedia Tools Appl. 2016, 1–30. [Google Scholar] [CrossRef]
- Mining Mind Dataset. Available online: https://www.dropbox.com/s/pio44t6glykueut/PsychiatricState Dataset.xlsx?dl=0 (accessed on 17 August 2015).
- Kim, K.H.; Bang, S.W.; Kim, S.R. Emotion recognition system using short-term monitoring of physiological signals. Med. Biol. Eng. Comput. 2004, 42, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Sedghamiz, H. An Online Algorithm for R, S and T Wave Detection. Available online: http://www.mathworks.com/matlabcentral/fileexchange/45404-ecg-q-r-s-wave-online-detector (accessed on 10 June 2015).
- Vaneghi, F.M.; Oladazimi, M.; Shiman, F.; Kordi, A.; Safari, M.J.; Ibrahim, F. A comparative approach to ECG feature extraction methods. In Proceedings of the 3rd International Conference on Intelligent Systems Modeling and Simulation, Kota Kinabalu, Malaysia, 8–10 February 2012; pp. 8–10.
- Braithwaite, J.J.; Watson, D.G.; Jones, R.; Rowe, M. A guide for analysing electrodermal activity (EDA) & skin conductance responses (SCRs) for psychological experiments. Psychophysiology 2013, 49, 1017–1034. [Google Scholar]
- Elgendi, M. On the analysis of fingertip photoplethysmogram signals. Curr. Cardiol. Rev. 2012, 8, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Oyama-Higa, M.; Pham, T.D. Identification of Mental Disorders by Hidden Markov Modeling of Photoplethysmograms. Biomed. Inform. Technol. 2014, 404, 29–39. [Google Scholar]
- Bhavana, V.; Vidya, M.J.; Padmaja, K.V. Feasibility of Authenticating Medical Data Using Photoplethysmography(ppg) as Signature Mark. Int. J. Adv. Res. Comput. Sci. Softw. Eng. 2014, 4, 635–641. [Google Scholar]
- Wijsman, J.; Grundlehner, B.; Penders, J.; Hermens, H.J. Trapezius muscle EMG as predictor of mental stress. ACM Trans. Embed. Comput. Syst. 2010, 12, 155–163. [Google Scholar]
- Stress & Coping Self-Test. Available online: http://livewellsiouxfalls.org/images/uploads/main/Stress_and_Coping_Self_Test.pdf (accessed on 06 April 2015).
- Jayalakshmi, T.; Santhakumaran, A. Statistical Normalization and Back Propagation for Classification. Int. J. Comput. Theory Eng. 2011, 3, 89. [Google Scholar] [CrossRef]
- Peng, H.; Long, F.; Din, C. Feature selection based on mutual information criteria of max-dependency, max-relevance, and min-redundancy. IEEE Trans. Pattern Anal. Mach. Intell. 2005, 27, 1226–1238. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.; Liu, F.; Zhou, X.; Li, Q. An Efficient Data Compression Model Based on Spatial Clustering and Principal Component Analysis in Wireless Sensor Networks. Sensors 2015, 15, 19443–19465. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Fang, B.; Tang, Y.Y.; Shang, Z.; Xu, B. Generalized discriminant analysis: A matrix exponential approach. IEEE Trans. Syst. Man Cybern. Part B (Cybern.) 2010, 40, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Foti, N.J.; Xu, J.; Laird, D.; Fox, E.B. Stochastic variational inference for hidden Markov models. In Proceedings of the Advances in Neural Information Processing Systems, Montreal, PQ, Canada, 8–13 December 2014; Volume 4, pp. 3599–3607.
- IEEE 802.15 WPAN™ Task Group 4 (TG4). Available online: http://www.ieee802.org/15/pub/TG4.html (accessed on 21 July 2016).
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Introduction to the SOAP HTTP binding. Available online: http://www.informit.com/articles/article.aspx? p=102285 (accessed on 15 January 2016).
- GlassFish Server 4.1. Available online: https://glassfish.java.net/ (accessed on 28 February 2015).
- Java Servlet Technology. Available online: http://www.oracle.com/technetwork/java/index-jsp-135475.html (accessed on 03 March 2015).
- Citrix XenServer 6.5. Available online: http://www.poppelgaard.com/citrix-xenserver-6-5 (accessed on 17 March 2015).
- Protégé 5.0.0. Available online: http://protege.stanford.edu/ (accessed on 22 April 2015).
- Apache Jena. Available online: https://jena.apache.org/tutorials/sparql.html (accessed on 23 April 2015).
- Rathore, S.; Hussain, M.; Khan, A. GECC: Gene expression based ensemble classification of colon samples. IEEE/ACM Trans. Comput. Biol. Bioinform. 2014, 11, 1131–1145. [Google Scholar] [CrossRef] [PubMed]
- Siddiqi, M.H.; Ali, R.; Khan, A.M.; Park, Y.T.; Lee, S.Y. Human Facial Expression Recognition Using Stepwise Linear Discriminant Analysis and Hidden Conditional Random Fields. IEEE Trans. Image Proc. 2015, 24, 1386–1398. [Google Scholar] [CrossRef] [PubMed]
















| Processing Steps | Candidate Results | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Viterbi | N | N | A | E | E | E | A | E | E | A | - |
| LRL | N:2 | A:1 | E:3 | A:1 | E:2 | A:1 | E | ||||
| HFC | N:2 | A:3 | E:5 | E | |||||||
| MRS | A | A | |||||||||
| Ensemble | E | E | A | - | |||||||
| MV | E:2 | A:1 | E |
| Test Cases | Test Settings | Sensitivity | Specificity |
|---|---|---|---|
| Test Case 1 | Without sensor observations (Only using patients’ medical, demographic and family histories) | 0.4286 | 0.5177 |
| Test Case 2 | EDA sensor observations with patients’ history | 0.6167 | 0.6493 |
| Test Case 3 | ECG and EDA sensors observation with patients’ history | 0.6332 | 0.7281 |
| Test Case 4 | BVP, ECG and EDA sensors observation with patients’ | 0.6871 | 0.8014 |
| Test Case 5 | EMG, BVP, ECG and EDA sensors observation with patients’ history | 0.7273 | 0.8636 |
| Psychiatric State | TP | FP | TN | FN | FPR = FP/(FP + TN) | FNR = FN/(FN + TP) | DOR = (TP × TN)/(FP × FN) | Confidence Interval (CI) |
|---|---|---|---|---|---|---|---|---|
| N | 21 | 4 | 26 | 4 | 0.1333 | 0.16 | 34.125 | (3.6, 6.7) |
| A | 12 | 4 | 32 | 7 | 0.111 | 0.3684 | 13.714 | (2.4, 5.2) |
| E | 8 | 6 | 38 | 3 | 0.1364 | 0.2727 | 16.889 | (2.5, 5.7) |
| Average = | 0.1269 | 0.2670 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alam, M.G.R.; Abedin, S.F.; Al Ameen, M.; Hong, C.S. Web of Objects Based Ambient Assisted Living Framework for Emergency Psychiatric State Prediction. Sensors 2016, 16, 1431. https://doi.org/10.3390/s16091431
Alam MGR, Abedin SF, Al Ameen M, Hong CS. Web of Objects Based Ambient Assisted Living Framework for Emergency Psychiatric State Prediction. Sensors. 2016; 16(9):1431. https://doi.org/10.3390/s16091431
Chicago/Turabian StyleAlam, Md Golam Rabiul, Sarder Fakhrul Abedin, Moshaddique Al Ameen, and Choong Seon Hong. 2016. "Web of Objects Based Ambient Assisted Living Framework for Emergency Psychiatric State Prediction" Sensors 16, no. 9: 1431. https://doi.org/10.3390/s16091431
APA StyleAlam, M. G. R., Abedin, S. F., Al Ameen, M., & Hong, C. S. (2016). Web of Objects Based Ambient Assisted Living Framework for Emergency Psychiatric State Prediction. Sensors, 16(9), 1431. https://doi.org/10.3390/s16091431