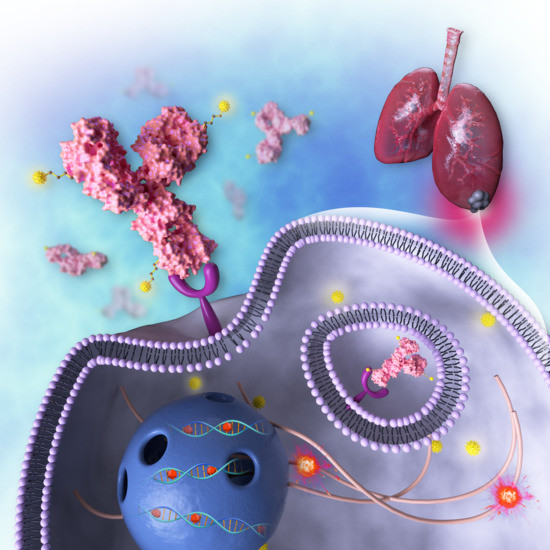
Targeting and Efficacy of Novel mAb806-Antibody-Drug Conjugates in Malignant Mesothelioma
Abstract
:1. Introduction
2. Results
2.1. EGFR and mAb806 Epitope Expression
2.2. Cell Proliferation
2.3. In Vivo Therapy Studies with mAb806-Based ADCs in Mesothelioma Xenograft and PDX Tumor Models
2.4. Molecular Imaging and Quantitation of 806 Expression in MSTO-211H Mesothelioma Xenograft Model with 89Zr-ch806
3. Discussion
4. Materials and Methods
4.1. Antibodies, ADCs and Chemotherapeutics
4.2. Cell Cultures
4.3. FACS Analysis
4.4. Western Blot
4.5. Cytotoxicity Assays
4.6. Immunohistochemistry Analysis
4.7. In Vivo Studies
4.8. Chelation and Radiolabeling of 89Zr-Labeled-ch806
4.9. Quality Control and In Vitro Characterization of 89Zr-Labeled-ch806
4.10. Biodistribution and Imaging Study with 89Zr-Labeled-ch806
4.11. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Olsen, N.J.; Franklin, P.J.; Reid, A.; De Klerk, N.; Threlfall, T.J.; Shilkin, K.; Musk, B. Increasing incidence of malignant mesothelioma after exposure to asbestos during home maintenance and renovation. Med. J. Aust. 2011, 195, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Landrigan, P.J.; Kazemi, H. Third Wave of Asbestos Disease; New York Academy of Sciences: New York, NY, USA, 1991. [Google Scholar]
- Destro, A.; Ceresoli, G.L.; Falleni, M.; Zucali, P.A.; Morenghi, E.; Bianchi, P.; Pellegrini, C.; Vaira, V.; Alloisio, M.; Rizzi, A.; et al. EGFR overexpression in malignant pleural mesothelioma. An immunohistochemical and molecular study with clinico-pathological correlations. Lung Cancer 2006, 51, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Okuda, K.; Sasaki, H.; Kawano, O.; Yukiue, H.; Yokoyama, T.; Yano, M.; Fujii, Y. Epidermal growth factor receptor gene mutation, amplification and protein expression in malignant pleural mesothelioma. J. Cancer Res. Clin. Oncol. 2008, 134, 1105–1111. [Google Scholar] [CrossRef]
- Rena, O.; Boldorini, R.; Gaudino, E.; Casadio, C. Epidermal growth factor receptor overexpression in malignant pleural mesothelioma: Prognostic correlations. J. Surg. Oncol. 2011, 104, 701–705. [Google Scholar] [CrossRef] [PubMed]
- Garland, L.L.; Rankin, C.; Gandara, D.R.; Rivkin, S.E.; Scott, K.M.; Nagle, R.B.; Klein-Szanto, A.J.; Testa, J.R.; Altomare, D.A.; Borden, E.C. Phase II study of erlotinib in patients with malignant pleural mesothelioma: A Southwest oncology group study. J. Clin. Oncol. 2007, 25, 2406–2413. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, V.; Lind, M.J.; Cawkwell, L. Targeted epidermal growth factor receptor therapy in malignant pleural mesothelioma: Where do we stand? Cancer Treat. Rev. 2011, 37, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Jackman, D.M.; Kindler, H.L.; Yeap, B.Y.; Fidias, P.; Salgia, R.; Lucca, J.; Morse, L.K.; Ostler, P.A.; Johnson, B.E.; Jänne, P.A. Erlotinib plus bevacizumab in previously treated patients with malignant pleural mesothelioma. Cancer 2008, 113, 808–814. [Google Scholar] [CrossRef]
- Clinical Trials.gov. Erlotinib Hydrochloride in Treating Patients with Malignant Peritoneal Mesothelioma (NCT01592383). 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT01592383 (accessed on 1 October 2020).
- University Hospital, G. Study of Cetuximab Combined with Cisplatin or Carboplatin/Pemetrexed as First Line Treatment in Patients with Malignant Pleural Mesothelioma (MesoMab NCT00996567). Available online: https://clinicaltrials.gov/ct2/show/NCT00996567 (accessed on 1 October 2020).
- Govindan, R. Gefitinib in patients with malignant mesothelioma: A Phase II study by the Cancer and Leukemia Group B. Clin. Cancer Res. 2005, 11, 2300–2304. [Google Scholar] [CrossRef] [Green Version]
- Johns, T.G.; Adams, T.E.; Cochran, J.R.; Hall, N.E.; Hoyne, P.A.; Olsen, M.; Kim, Y.-S.; Rothacker, J.; Nice, E.C.; Walker, F.; et al. Identification of the epitope for the epidermal growth factor receptor-specific monoclonal antibody 806 reveals that it preferentially recognizes an untethered form of the receptor. J. Biol. Chem. 2004, 279, 30375–30384. [Google Scholar] [CrossRef] [Green Version]
- Gan, H.K.; Burgess, A.W.; Clayton, A.H.A.; Scott, A.M. Targeting of a conformationally exposed, tumor-specific epitope of EGFR as a strategy for cancer therapy. Cancer Res. 2012, 72, 2924–2930. [Google Scholar] [CrossRef] [Green Version]
- Cleary, J.M.; Reardon, D.A.; Azad, N.; Gandhi, L.; Shapiro, G.I.; Chaves, J.; Pedersen, M.; Ansell, P.; Ames, W.; Xiong, H.; et al. A phase 1 study of ABT-806 in subjects with advanced solid tumors. Investig. New Drugs 2015, 33, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Phillips, A.C.; Boghaert, E.; Vaidya, K.S.; Mitten, M.J.; Norvell, S.; Falls, H.D.; Devries, P.J.; Cheng, N.; Meulbroek, J.A.; Buchanan, F.G.; et al. ABT-414, an antibody-drug conjugate targeting a tumor-selective EGFR epitope. Mol. Cancer Ther. 2016, 15, 661–669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bent, M.J.V.D.; Gan, H.K.; Lassman, A.B.; Kumthekar, P.; Merrell, R.; Butowski, N.; Lwin, Z.; Mikkelsen, T.; Nabors, B.; Papadopoulos, K.P.; et al. Efficacy of depatuxizumab mafodotin (ABT-414) monotherapy in patients with EGFR-amplified, recurrent glioblastoma: Results from a multi-center, international study. Cancer Chemother. Pharmacol. 2017, 80, 1209–1217. [Google Scholar] [CrossRef] [PubMed]
- Lassman, A.B.; Bent, M.J.V.D.; Gan, H.K.; Reardon, D.A.; Kumthekar, P.; Butowski, N.; Lwin, Z.; Mikkelsen, T.; Nabors, L.B.; Papadopoulos, K.P.; et al. Safety and efficacy of depatuxizumab mafodotin + temozolomide in patients withEGFR-amplified, recurrent glioblastoma: Results from an international phase I multicenter trial. Neuro-Oncology 2018, 21, 106–114. [Google Scholar] [CrossRef] [Green Version]
- Phillips, A.C.; Boghaert, E.R.; Vaidya, K.S.; Falls, H.D.; Mitten, M.J.; Devries, P.J.; Benatuil, L.; Hsieh, C.-M.; Meulbroek, J.A.; Panchal, S.C.; et al. Characterization of ABBV-221, a tumor-selective EGFR-targeting antibody drug conjugate. Mol. Cancer Ther. 2018, 17, 795–805. [Google Scholar] [CrossRef] [Green Version]
- Calvo, E.; Cleary, J.M.; Moreno, V.; Gifford, M.; Roberts-Rapp, L.; Ansell, P.J.; Mittapalli, R.K.; Lee, H.-J.; Hu, B.; Barch, D.; et al. Preliminary results from a phase 1 study of the antibody-drug conjugate ABBV-221 in patients with solid tumors likely to express EGFR. J. Clin. Oncol. 2017, 35, 2510. [Google Scholar] [CrossRef]
- Cleary, J.M.; Calvo, E.; Moreno, V.; Juric, D.; Shapiro, G.I.; Vanderwal, C.A.; Hu, B.; Gifford, M.; Barch, D.; Roberts-Rapp, L.; et al. A phase 1 study evaluating safety and pharmacokinetics of losatuxizumab vedotin (ABBV-221), an anti-EGFR antibody-drug conjugate carrying monomethyl auristatin E, in patients with solid tumors likely to overexpress EGFR. Investig. New Drugs 2020, 2020, 1–12. [Google Scholar] [CrossRef]
- Anderson, M.G.; Falls, H.D.; Mitten, M.J.; Oleksijew, A.; Vaidya, K.S.; Boghaert, E.R.; Gao, W.; Palma, J.P.; Cao, D.; Chia, P.-L.; et al. Targeting multiple EGFR expressing tumors with a highly potent tumor-selective antibody drug conjugate. Mol. Cancer Ther. 2020. [Google Scholar] [CrossRef]
- Jeffrey, S.C.; Burke, P.J.; Lyon, R.P.; Meyer, D.W.; Sussman, D.; Anderson, M.; Hunter, J.H.; Leiske, C.I.; Miyamoto, J.B.; Nicholas, N.D.; et al. A potent anti-CD70 antibody–drug conjugate combining a dimeric pyrrolobenzodiazepine drug with site-specific conjugation technology. Bioconjug. Chem. 2013, 24, 1256–1263. [Google Scholar] [CrossRef]
- Panousis, C.; Rayzman, V.M.; Johns, T.G.; Renner, C.; Liu, Z.; Cartwright, G.; Lee, F.-T.; Wang, D.-N.; Gan, H.; Cao, D.; et al. Engineering and characterisation of chimeric monoclonal antibody 806 (ch806) for targeted immunotherapy of tumours expressing de2-7 EGFR or amplified EGFR. Br. J. Cancer 2005, 92, 1069–1077. [Google Scholar] [CrossRef]
- Nayak, T.K.; Garmestani, K.; Milenic, D.E.; Baidoo, K.E.; Brechbiel, M.W. HER1-Targeted 86Y-panitumumab possesses superior targeting characteristics than 86Y-cetuximab for PET imaging of human malignant mesothelioma tumors xenografts. PLoS ONE 2011, 6, e18198. [Google Scholar] [CrossRef] [PubMed]
- Kurai, J.; Chikumi, H.; Hashimoto, K.; Takata, M.; Sako, T.; Yamaguchi, K.; Kinoshita, N.; Watanabe, M.; Touge, H.; Makino, H.; et al. Therapeutic antitumor efficacy of anti-epidermal growth factor receptor antibody, cetuximab, against malignant pleural mesothelioma. Int. J. Oncol. 2012, 41, 1610–1618. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salvi, S.; Varesano, S.; Boccardo, S.; Ravetti, J.L.; Canessa, P.A.; Pistillo, M.P.; Ferro, P.; Fedeli, F.; Roncella, S. EGFR status in mesothelioma: Possible implications for the efficacy of anti-EGFR and anti-MET therapies. J. Thorac. Oncol. 2016, 11, e78–e80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, L.; Allo, G.; John, T.; Li, M.; Tagawa, T.; Opitz, I.; Anraku, M.; Yun, Z.; Pintilie, M.; Pitcher, B.; et al. Patient-derived xenograft establishment from human malignant pleural mesothelioma. Clin. Cancer Res. 2016, 23, 1060–1067. [Google Scholar] [CrossRef] [Green Version]
- Chang, A.J.; De Silva, R.A.; Lapi, S.E. Development and characterization of 89Zr-labeled panitumumab for immuno–positron emission tomographic imaging of the epidermal growth factor receptor. Mol. Imaging 2013, 12, 17–27. [Google Scholar]
- Izquierdo-Sánchez, V.; Muñiz-Hernández, S.; Vázquez-Becerra, H.; Yepez, J.P.; Romero-Piña, M.E.; Arrieta, O.; Medina, L.A. Biodistribution and tumor uptake of 67Ga-nimotuzumab in a malignant pleural mesothelioma xenograft. Molecules 2018, 23, 3138. [Google Scholar] [CrossRef] [Green Version]
- Burvenich, I.; Parakh, S.; Gan, H.K.; Lee, F.-T.; Guo, N.; Rigopoulos, A.; Lee, S.-T.; Gong, S.; O’Keefe, G.; Tochon-Danguy, H.; et al. Molecular imaging and quantitation of EphA2 expression in xenograft models with 89Zr-DS-8895a. J. Nucl. Med. 2016, 57, 974–980. [Google Scholar] [CrossRef] [Green Version]
- Holland, J.P.; Divilov, V.; Bander, N.H.; Smith-Jones, P.M.; Larson, S.M.; Lewis, J.S. 89Zr-DFO-J591 for immune PET imaging of prostate-specific membrane antigen (PSMA) expression In Vivo. J. Nucl. Med. 2010, 51, 1293–1300. [Google Scholar] [CrossRef] [Green Version]
- Dijkers, E.C.; Kosterink, J.G.; Rademaker, A.P.; Perk, L.R.; van Dongen, G.A.; Bart, J.; de Jong, J.R.; de Vries, E.G.; Lub-de Hooge, M.N. Development and characterization of clinical-grade 89Zr-trastuzumab for HER2/neu immunoPET imaging. J. Nucl. Med. 2009, 50, 974–981. [Google Scholar] [CrossRef] [Green Version]
- Goss, G.D.; Vokes, E.E.; Gordon, M.S.; Gandhi, L.; Papadopoulos, K.P.; Rasco, D.W.; Fischer, J.S.; Chu, K.L.; Ames, W.W.; Mittapalli, R.K.; et al. Efficacy and safety results of depatuxizumab mafodotin (ABT-414) in patients with advanced solid tumors likely to overexpress epidermal growth factor receptor. Cancer 2018, 124, 2174–2183. [Google Scholar] [CrossRef]
- Scott, A.M.; Lee, F.-T.; Tebbutt, N.; Herbertson, R.; Gill, S.S.; Liu, Z.; Skrinos, E.; Murone, C.; Saunder, T.H.; Chappell, B.; et al. A phase I clinical trial with monoclonal antibody ch806 targeting transitional state and mutant epidermal growth factor receptors. Proc. Natl. Acad. Sci. USA 2007, 104, 4071–4076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blumenschein, G.R.; Hassan, R.; Moore, K.; Santin, A.; Kindler, H.L.; Nemunaitis, J.J.; Seward, S.M.; Rajagopalan, P.; Walter, A.; Sarapa, N.; et al. Phase I study of anti-mesothelin antibody drug conjugate anetumab ravtansine (AR). J. Clin. Oncol. 2016, 34, 2509. [Google Scholar] [CrossRef]
- Hassan, R.; Kindler, H.L.; Jahan, T.; Bazhenova, L.; Reck, M.; Thomas, A.; Pastan, I.; Parno, J.; O’Shannessy, D.J.; Fatato, P.; et al. Phase II clinical trial of amatuximab, a chimeric antimesothelin antibody with pemetrexed and cisplatin in advanced unresectable pleural mesothelioma. Clin. Cancer Res. 2014, 20, 5927–5936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kindler, H.; Novello, S.; Fennell, D.; Blumenschein, G.; Bearz, A.; Ceresoli, G.; Aerts, J.; Spicer, J.; Taylor, P.; Greystoke, A.; et al. OA 02.01 Randomized Phase II study of anetumab ravtansine or vinorelbine in patients with metastatic pleural mesothelioma. J. Thorac. Oncol. 2017, 12, S1746. [Google Scholar] [CrossRef]
- Aparicio, S.; Hidalgo, M.; Kung, A.L. Examining the utility of patient-derived xenograft mouse models. Nat. Rev. Cancer 2015, 15, 311–316. [Google Scholar] [CrossRef]
- Le Pimpec-Barthes, F.; Bernard, I.; Alsamad, I.A.; Renier, A.; Kheuang, L.; Fleury-Feith, J.; Devauchelle, P.; Colonna, F.Q.; Riquet, M.; Jaurand, M.-C. Pleuro-pulmonary tumours detected by clinical and chest X-ray analyses in rats transplanted with mesothelioma cells. Br. J. Cancer 1999, 81, 1344–1350. [Google Scholar] [CrossRef]
- Martarelli, D.; Catalano, A.; Procopio, A.; Orecchia, S.; Libener, R.; Santoni, G. Characterization of human malignant mesothelioma cell lines orthotopically implanted in the pleural cavity of immunodeficient mice for their ability to grow and form metastasis. BMC Cancer 2006, 6, 130. [Google Scholar] [CrossRef] [Green Version]
- Kelly, K.J.; Woo, Y.; Brader, P.; Yu, Z.; Riedl, C.; Lin, S.-F.; Chen, N.; Yu, Y.A.; Rusch, V.W.; Szalay, A.A.; et al. Novel oncolytic agent GLV-1h68 is effective against malignant pleural mesothelioma. Hum. Gene Ther. 2008, 19, 774–782. [Google Scholar] [CrossRef]
- Reilly, E.B.; Phillips, A.C.; Buchanan, F.G.; Kingsbury, G.; Zhang, Y.; Meulbroek, J.A.; Cole, T.B.; Devries, P.J.; Falls, H.D.; Beam, C.; et al. Characterization of ABT-806, a humanized tumor-specific anti-EGFR monoclonal antibody. Mol. Cancer Ther. 2015, 14, 1141–1151. [Google Scholar] [CrossRef] [Green Version]
- Nishikawa, R.; Ji, X.D.; Harmon, R.C.; Lazar, C.S.; Gill, G.N.; Cavenee, W.K.; Huang, H.J. A mutant epidermal growth factor receptor common in human glioma confers enhanced tumorigenicity. Proc. Natl. Acad. Sci. USA 1994, 91, 7727–7731. [Google Scholar] [CrossRef] [Green Version]
- Sato, J.D.; Kawamoto, T.; Le, A.D.; Mendelsohn, J.; Polikoff, J.; Sato, G.H. Biological effects In Vitro of monoclonal antibodies to human epidermal growth factor receptors. Mol. Boil. Med. 1983, 1, 511–529. [Google Scholar]
- Skehan, P.; Storeng, R.; Scudiero, D.; Monks, A.; McMahon, J.; Vistica, D.; Warren, J.T.; Bokesch, H.; Kenney, S.; Boyd, M.R. New colorimetric cytotoxicity assay for anticancer-drug screening. J. Natl. Cancer Inst. 1990, 82, 1107–1112. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, F.R.; Varella-Garcia, M.; Bunn, P.A.; Di Maria, M.V.; Veve, R.; Bremnes, R.M.; Barón, A.E.; Zeng, C.; Franklin, W.A. Epidermal growth factor receptor in non–small-cell lung carcinomas: Correlation between gene copy number and protein expression and impact on prognosis. J. Clin. Oncol. 2003, 21, 3798–3807. [Google Scholar] [CrossRef] [PubMed]
- Burvenich, I.; Parakh, S.; Lee, F.-T.; Guo, N.; Liu, Z.; Gan, H.K.; Rigopoulos, A.; O’Keefe, G.J.; Gong, S.J.; Goh, Y.W.; et al. Molecular imaging of T cell co-regulator factor B7-H3 with 89Zr-DS-5573a. Theranostics 2018, 8, 4199–4209. [Google Scholar] [CrossRef] [PubMed]
- Lindmo, T.; Boven, E.; Cuttitta, F.; Fedorko, J.; Bunn, P. Determination of the immunoreactive function of radiolabeled monoclonal antibodies by linear extrapolation to binding at infinite antigen excess. J. Immunol. Methods 1984, 72, 77–89. [Google Scholar] [CrossRef]
- Lee, F.T.; Rigopoulos, A.; Hall, C.; Clarke, K.; Cody, S.H.; Smyth, F.E.; Liu, Z.; Brechbiel, M.W.; Hanai, N.; Nice, E.C.; et al. Specific localization, gamma camera imaging, and intracellular trafficking of radiolabelled chimeric anti-G(D3) ganglioside monoclonal antibody KM871 in SK-MEL-28 melanoma xenografts. Cancer Res. 2001, 61, 4474–4482. [Google Scholar] [PubMed]






© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chia, P.-L.; Parakh, S.; Tsao, M.-S.; Pham, N.-A.; Gan, H.K.; Cao, D.; Burvenich, I.J.G.; Rigopoulos, A.; Reilly, E.B.; John, T.; et al. Targeting and Efficacy of Novel mAb806-Antibody-Drug Conjugates in Malignant Mesothelioma. Pharmaceuticals 2020, 13, 289. https://doi.org/10.3390/ph13100289
Chia P-L, Parakh S, Tsao M-S, Pham N-A, Gan HK, Cao D, Burvenich IJG, Rigopoulos A, Reilly EB, John T, et al. Targeting and Efficacy of Novel mAb806-Antibody-Drug Conjugates in Malignant Mesothelioma. Pharmaceuticals. 2020; 13(10):289. https://doi.org/10.3390/ph13100289
Chicago/Turabian StyleChia, Puey-Ling, Sagun Parakh, Ming-Sound Tsao, Nhu-An Pham, Hui K. Gan, Diana Cao, Ingrid J. G. Burvenich, Angela Rigopoulos, Edward B. Reilly, Thomas John, and et al. 2020. "Targeting and Efficacy of Novel mAb806-Antibody-Drug Conjugates in Malignant Mesothelioma" Pharmaceuticals 13, no. 10: 289. https://doi.org/10.3390/ph13100289
APA StyleChia, P. -L., Parakh, S., Tsao, M. -S., Pham, N. -A., Gan, H. K., Cao, D., Burvenich, I. J. G., Rigopoulos, A., Reilly, E. B., John, T., & Scott, A. M. (2020). Targeting and Efficacy of Novel mAb806-Antibody-Drug Conjugates in Malignant Mesothelioma. Pharmaceuticals, 13(10), 289. https://doi.org/10.3390/ph13100289