Prevalence and Determinants of Multimorbidity, Polypharmacy, and Potentially Inappropriate Medication Use in the Older Outpatients: Findings from EuroAgeism H2020 ESR7 Project in Ethiopia
Abstract
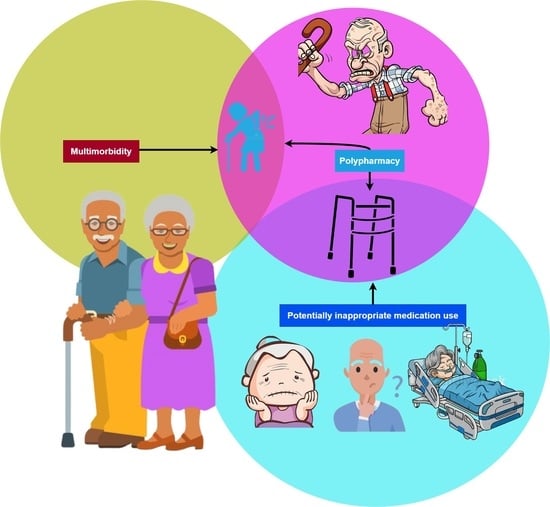
:1. Introduction
2. Results
2.1. Demographic Characteristics of Study Participants
2.2. Prevalence of Multimorbidity, Polypharmacy, and PIM Use
2.3. Determinants of Multimorbidity, Polypharmacy, and PIM Use
2.3.1. Multimorbidity
2.3.2. Polypharmacy
2.3.3. PIM Use
3. Discussion
Limitations
4. Materials and Methods
4.1. Sample Size and Sampling Technique
4.2. Data Collection
- Multimorbidity is defined as the presence of two or more long-term conditions that cannot be cured but can be controlled through medications or other treatments [1].
- Polypharmacy is considered if the patient is taking at least five medications regularly [3].
- PIM use is defined as drug therapy whose potential risks outweigh potential benefits, and identified PIMs were classified according to the 2019 AGS Beers criteria [14].
- Charlson comorbidity index (CCI) score is used to measure the severity of the comorbidity for each patient quantitatively [43]. Patients were divided into three groups: mild, with a CCI score of 1–2; moderate, with a CCI score of 3–4; and severe, with a CCI score of ≥5.
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mercer, S.; Furler, J.; Moffat, K.; Fischbacher-Smith, D.; Sanci, L.; World Health Organization. Multimorbidity: Technical Series on Safer Primary Care. 2016. Available online: https://eprints.gla.ac.uk/133210/1/133210.pdf (accessed on 25 June 2021).
- World Health Organization. Global Age-Friendly Cities Project; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- World Health Organization. Medication Safety in Polypharmacy: Technical Report; World Health Organization: Geneva, Switzerland, 2019; Available online: http://apps.who.int/iris (accessed on 10 August 2021).
- Beers, M.H.; Ouslander, J.G.; Rollingher, I.; Reuben, D.B.; Brooks, J.; Beck, J.C. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch. Intern. Med. 1991, 151, 1825–1832. [Google Scholar] [CrossRef] [PubMed]
- Krause, O.; Wiese, B.; Doyle, I.M.; Kirsch, C.; Thürmann, P.; Wilm, S.; Sparenberg, L.; Stolz, R.; Freytag, A.; Bleidorn, J.; et al. Multidisciplinary intervention to improve medication safety in nursing home residents: Protocol of a cluster randomised controlled trial (HIOPP-3-iTBX study). BMC Geriatr. 2019, 19, 24. [Google Scholar] [CrossRef] [PubMed]
- Dalton, K.; O’Mahony, D.; O’Sullivan, D.; O’Connor, M.N.; Byrne, S. Prescriber Implementation of STOPP/START Recommendations for Hospitalised Older Adults: A Comparison of a Pharmacist Approach and a Physician Approach. Drugs Aging 2019, 36, 279–288. [Google Scholar] [CrossRef] [PubMed]
- McNicholl, I.R.; Gandhi, M.; Hare, C.B.; Greene, M.; Pierluissi, E. A Pharmacist-Led Program to Evaluate and Reduce Polypharmacy and Potentially Inappropriate Prescribing in Older HIV-Positive Patients. Pharmacotherapy 2017, 37, 1498–1506. [Google Scholar] [CrossRef] [PubMed]
- Campins, L.; Serra-Prat, M.; Gózalo, I.; López, D.; Palomera, E.; Agustí, C.; Cabré, M.; REMEI Group. Randomized controlled trial of an intervention to improve drug appropriateness in community-dwelling polymedicated elderly people. Fam. Pract. 2017, 34, 36–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gillespie, U.; Alassaad, A.; Hammarlund-Udenaes, M.; Mörlin, C.; Henrohn, D.; Bertilsson, M.; Melhus, H. Effects of pharmacists’ interventions on appropriateness of prescribing and evaluation of the instruments’ (MAI, STOPP and STARTs’) ability to predict hospitalization--analyses from a randomized controlled trial. PLoS ONE 2013, 8, e62401. [Google Scholar] [CrossRef] [PubMed]
- American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc. 2015, 63, 2227–2246. [Google Scholar] [CrossRef] [PubMed]
- Topinkova, E.; Madlova, P.; Fialova, D.; Klan, J. New evidence-based criteria for evaluating the appropriateness of drug regimen in seniors Criteria STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert Doctors to Right Treatment). Vnitr. Lek. 2008, 54, 1161–1169. (In Czech) [Google Scholar] [PubMed]
- Renom-Guiteras, A.; Meyer, G.; Thürmann, P.A. The EU(7)-PIM list: A list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur. J. Clin. Pharmacol. 2015, 71, 861–875. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inocian, E.P.; Reynaldo, R.F.; Dillon, D.; Ignacio, E.H. Using Beers Criteria to Avoid Inappropriate Prescribing for Older Adults. Medsurg. Nurs. 2021, 30, 113–117. [Google Scholar]
- 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc. 2019, 67, 674–694. [Google Scholar] [CrossRef] [PubMed]
- The United Nations Population Fund. 2021. Available online: https://www.unfpa.org/publications/state-world-population-2021 (accessed on 23 May 2021).
- Mekonnen, A.B.; Bhagavathula, A.S. Inappropriate medication use in the elderly population attending Gondar University hospital: A preliminary assessment. Int. J. Pharm. Pharm. Sci. 2014, 6, 540–543. [Google Scholar]
- Tefera, Y.G.; Alemayehu, M.; Mekonnen, G.B. Prevalence and determinants of polypharmacy in cardiovascular patients attending outpatient clinic in Ethiopia University Hospital. PLoS ONE 2020, 15, e0234000. [Google Scholar] [CrossRef] [PubMed]
- Abegaz, T.M.; Birru, E.M.; Mekonnen, G.B. Potentially inappropriate prescribing in Ethiopian geriatric patients hospitalized with cardiovascular disorders using START/STOPP criteria. PLoS ONE 2018, 13, e0195949. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teka, F.; Teklay, G.; Ayalew, E.; Kassa, T.T. Prevalence of potentially inappropriate medications in Ayder referral hospital, Tigray region, Northern Ethiopia: Prospective study. J. Drug Deliv. Therap. 2016, 6, 16–21. [Google Scholar] [CrossRef]
- Getachew, H.; Bhagavathula, A.S.; Abebe, T.B.; Belachew, S.A. Inappropriate prescribing of antithrombotic therapy in Ethiopian elderly population using updated 2015 STOPP/START criteria: A cross-sectional study. Clin. Interv. Aging 2016, 11, 819–827. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geresu, G.D.; Yadesa, T.M.; Abebe, B.A. Polypharmacy and the Contributing Factors Among Elderly Patients in Shashemene Referral Hospital, West Arsi, Oromia Region, Ethiopia. J. Bioanal. Biomed. 2017, 9, 277–282. [Google Scholar] [CrossRef]
- Tegegn, H.G.; Erku, D.A.; Sebsibe, G.; Gizaw, B.; Seifu, D.; Tigabe, M.; Belachew, S.A.; Ayele, A.A. Medication-related quality of life among Ethiopian elderly patients with polypharmacy: A cross-sectional study in an Ethiopia university hospital. PLoS ONE 2019, 14, e0214191. [Google Scholar] [CrossRef] [PubMed]
- Bhagavathula, A.S.; Gebreyohannes, E.A.; Fialova, D. Prevalence of polypharmacy and risks of potentially inappropriate medication use in the older population in a developing country: A systematic review and meta-analysis. Gerontology 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Jirón, M.; Pate, V.; Hanson, L.C.; Lund, J.L.; Jonsson, F.M.; Stürmer, T. Trends in prevalence and determinants of potentially inappropriate prescribing in the United States: 2007 to 2012. J. Am. Geriatr. Soc. 2016, 64, 788–797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olusanya, A.; Ogunyemi, A.; Arikawe, A.; Megbuwawon, T.; Amao, O. Inappropriate drug use in the elderly outpatient population in a West-African metropolitan community. Int. J. Clin. Pharmacol. Ther. 2019, 57, 334–344. [Google Scholar] [CrossRef] [PubMed]
- Akande-Sholabi, W.; Ajilore, O.C.; Showande, S.J.; Adebusoye, L.A. Potential inappropriate prescribing among ambulatory elderly patients in a geriatric centre in southwestern Nigeria: Beers criteria versus STOPP/START criteria. Trop. J. Pharm. Res. 2020, 19, 1105–1111. [Google Scholar] [CrossRef]
- Abubakar, U.; Tangiisuran, B.; Kolo, M.; Yamma, A.I.; Hammad, M.A.; Sulaiman, S.A. Prevalence and predictors of potentially inappropriate medication use among ambulatory older adults in Northern Nigeria. Drugs Ther. Perspect. 2021, 37, 94–99. [Google Scholar] [CrossRef]
- Saka, S.A.; Oosthuizen, F.; Nlooto, M. Potential inappropriate prescribing and associated factors among older persons in Nigeria and South Africa. Int. J. Clin. Pharm. 2019, 41, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Lemma, W.; Islam, M.; Loha, E.; Mahalwal, V.S. Drug prescribing patterns in geriatric patients in selected health facilities of Addis Ababa, Ethiopia. J. Appl. Pharm. Sci. 2020, 10, 103–109. [Google Scholar] [CrossRef]
- Lemma, W.; Islam, M.; Loha, E. Potentially inappropriate medication prescribing patterns in geriatric patients in a health facility in Addis Ababa, Ethiopia. Trop. J. Pharm. Res. 2020, 19, 244–246. [Google Scholar] [CrossRef]
- Sada, O. Irrational use of medications among elderly patients in an Ethiopian referral hospital. Afr. J. Pharm. Pharmacol. 2017, 11, 191–194. [Google Scholar] [CrossRef]
- Zahwe, M.; Skouri, H.; Rachidi, S.; Khoury, M.; Noureddine, S.; Isma’eel, H.; Tamim, H.; Al-Hajje, A. Potentially inappropriate medications in elderly patients with heart failure: Beers Criteria-based study. Int. J. Pharm. Pract. 2020, 28, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Al-Dahshan, A.; Kehyayan, V. Prevalence and predictors of potentially inappropriate medication prescription among older adults: A cross-sectional study in the state of Qatar. Drugs Real. World Outcomes 2021, 8, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Chhabra, M.; Vidyasagar, K.; Rashid, M.; Fialova, D.; Bhagavathula, A.S. Potentially inappropriate medication use in older hospitalized patients with type 2 eiabetes: A cross-sectional study. Pharmacy 2020, 8, 219. [Google Scholar] [CrossRef] [PubMed]
- He, D.; Zhu, H.; Zhou, H.; Dong, N.; Zhang, H. Potentially inappropriate medications in Chinese older adults: A comparison of two updated Beers criteria. Int. J. Clin. Pharm. 2021, 43, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Tian, F.; Li, H.; Chen, Z.; Xu, T. Potentially inappropriate medications in Chinese older outpatients in tertiary hospitals according to Beers criteria: A cross-sectional study. Int. J. Clin. Pract. 2021, 75, e14348. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.N.; Laetsch, D.C.; Chen, L.J.; Holleczek, B.; Meid, A.D.; Brenner, H.; Schöttker, B. Comparison of five lists to identify potentially inappropriate use of non-steroidal anti-inflammatory drugs in older adults. Pain Med. 2021, pnaa480. [Google Scholar] [CrossRef] [PubMed]
- Brockmöller, J.; Stingl, J.C. Multimorbidity, polypharmacy and pharmacogenomics in old age. Pharmacogenomics 2017, 18, 515–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muhlack, D.C.; Hoppe, L.K.; Stock, C.; Haefeli, W.E.; Brenner, H.; Schöttker, B. The associations of geriatric syndromes and other patient characteristics with the current and future use of potentially inappropriate medications in a large cohort study. Eur. J. Clin. Pharmacol. 2018, 74, 1633–1644. [Google Scholar] [CrossRef] [PubMed]
- Manias, E.; Maier, A.; Krishnamurthy, G. Inappropriate medication use in hospitalised oldest old patients across transitions of care. Aging Clin. Exp. Res. 2019, 31, 1661–1673. [Google Scholar] [CrossRef] [PubMed]
- Damoiseaux-Volman, B.A.; Medlock, S.; Raven, K.; Sent, D.; Romijn, J.A.; van der Velde, N.; Abu-Hanna, A. Potentially inappropriate prescribing in older hospitalized Dutch patients according to the STOPP/START criteria v2: A longitudinal study. Eur. J. Clin. Pharmacol. 2021, 75, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Yarnall, A.J.; Sayer, A.A.; Clegg, A.; Rockwood, K.; Parker, S.; Hindle, J.V. New horizons in multimorbidity in older adults. Age Ageing 2017, 46, 882–888. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Prithviraj, G.K.; Koroukian, S.; Margevicius, S.; Berger, N.A.; Bagai, R.; Owusu, C. Patient characteristics associated with polypharmacy and inappropriate prescribing of medications among older adults with cancer. J. Geriatr. Oncol. 2012, 3, 228–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- González-González, A.I.; Meid, A.D.; Dinh, T.S.; Blom, J.W.; van den Akker, M.; Elders, P.J.M.; Thiem, U.; De Gaudry, D.K.; Swart, K.M.A.; Rudolf, H.; et al. A prognostic model predicted deterioration in health-related quality of life in older patients with multimorbidity and polypharmacy. J. Clin. Epidemiol. 2021, 130, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.P.B.; Leung, D.S.Y.; Chi, I. Social functioning, polypharmacy and depression in older Chinese primary care patients. Aging Mental Health 2011, 15, 732–741. [Google Scholar] [CrossRef] [PubMed]
- Pedrós, C.; Formiga, F.; Corbella, X.; Arnau, J.M. Adverse drug reactions leading to urgent hospital admission in an elderly population: Prevalence and main features. Eur. J. Clin. Pharmacol. 2016, 72, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Al-Busaidi, S.; Al-Kharusi, A.; Al-Hinai, M.; Al-Zakwani, I.; Al-Ghafri, F.; Rizvi, S.; Al-Balushi, K. Potentially inappropriate prescribing among elderly patients at a primary care clinic in Oman. J. Cross-Cult. Gerontol. 2020, 35, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Guaraldo, L.; Cano, F.G.; Damasceno, G.S.; Rozenfeld, S. Inappropriate medication use among the elderly: A systematic review of administrative databases. BMC Geriatr. 2011, 11, 79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jungo, K.T.; Streit, S.; Lauffenburger, J.C. Patient factors associated with new prescribing of potentially inappropriate medications in multimorbid US older adults using multiple medications. BMC Geriatr. 2021, 21, 163. [Google Scholar] [CrossRef] [PubMed]


| Variables | Overall | Multimorbidity (n = 189, 59.1%) | Polypharmacy (n = 77, 24.1%) | PIM † Use (n = 151, 47.2%) |
|---|---|---|---|---|
| Age (years) | 71.9 (SD: 6.07) | 71.6 (SD: 5.98) | 71.5 (SD: 6.24) | 72.8 (SD: 6.14) |
| 65–74 | 209 (65.3) | 124 (38.8) | 49 (15.3) | 93 (29.1) |
| ≥75 | 111 (34.7) | 65 (20.3) | 28 (8.8) | 58 (18.1) |
| Men | 189 (59) | 106 (33.1) | 48 (15) | 93 (29) |
| Women | 131 (41) | 83 (25.9) | 29 (9) | 58 (18.1) |
| Married | 225 (70.3) | 128 (40) | 58 (18.1) | 104 (32.5) |
| Illiterate | 208 (65) | 112 (35) | 25 (7.8) | 51 (15.9) |
| Overweight/Obese | 14 (4.4) | 9 (2.8) | 5 (1.6) | 6 (1.9) |
| Hospitalization previous year | 126 (39.4) | 80 (25) | 35 (10.9) | 64 (20) |
| Serum creatinine (micromol/L) (n = 188, 58.7%) | 69.6 (SD: 27.6) | 68.1 (SD: 28.2) | 66.0 (SD: 27.4) | 70.8 (SD: 28.8) |
| Creatine clearance < 30 mL/min | 42 (13.1) | 30 (9.4) | 13 (4.1) | 21 (6.6) |
| Charlson’s comorbidity index (score) | 2.53 (SD: 1.38) | 3.1 (SD: 1.36) | 2.54 (SD: 1.61) | 2.25 (SD: 1.40) |
| Mild (1–2 points) | 170 (53.1) | 57 (17.8) | 41 (12.8) | 85 (26.6) |
| Moderate (3–4 points) | 136 (42.5) | 120 (37.5) | 31 (9.7) | 59 (18.4) |
| Severe (≥ 5 points) | 14 (4.4) | 12 (0.6) | 5 (1.6) | 7 (2.2) |
| Comorbidities | ||||
| Hypertension | 213 (66.6) | 157 (49.1) | 54 (16.9) | 100 (31.3) |
| Diabetes | 118 (36.9) | 103 (32.2) | 27 (8.4) | 52 (16.3) |
| Dyslipidemia | 40 (12.5) | 38 (11.9) | 16 (5.0) | 23 (7.2) |
| Coronary heart disease | 31 (9.7) | 28 (8.8) | 5 (1.6) | 16 (5.0) |
| Peptic ulcer disease | 30 (9.4) | 28 (8.8) | 4 (1.3) | 10 (3.1) |
| Congestive heart failure | 11 (3.4) | 9 (2.8) | 2 (0.6) | 5 (1.6) |
| Pneumonia | 10 (3.1) | 9 (2.8) | 3 (0.9) | 6 (1.9) |
| HIV | 6 (1.9) | 5 (1.6) | 3 (0.9) | 3 (0.9) |
| Other diseases | 72 (22.5) | 58 (18.1) | 18 (5.6) | 31 (9.7) |
| Number of medications | 3.4 (SD: 1.69) | 3.5 (SD: 1.66) | 5.8 (SD: 1.24) | 3.4 (SD: 1.72) |
| Comprehensive geriatric assessment * | ||||
| Understand verbal and non-verbal communication | 233 (72.8) | 145 (45.3) | 63 (19.7) | 92 (28.8) |
| Physical fitness | 272 (85) | 159 (49.7) | 64 (20) | 120 (37.5) |
| Using walking assistance devices | 118 (36.9) | 72 (22.5) | 41 (12.8) | 72 (22.5) |
| Lack of interest in activities | 42 (13.1) | 22 (6.9) | 14 (4.4) | 25 (7.8) |
| Persistent anger with self/others | 51 (15.9) | 30 (9.4) | 22 (6.9) | 24 (7.5) |
| Cognitive impairment | 56 (17.5) | 31 (9.7) | 14 (4.4) | 35 (10.9) |
| Had repeated health complaints | 70 (21.9) | 43 (13.4) | 21 (6.6) | 34 (10.6) |
| Experienced fall in the past year | 44 (13.8) | 21 (6.6) | 11 (3.4) | 21 (6.6) |
| Flare-ups of pain | 56 (17.5) | 36 (11.3) | 20 (6.3) | 26 (8.1) |
| Health fluctuation/deterioration | 50 (15.6) | 26 (8.1) | 6 (1.9) | 30 (9.4) |
| Therapeutic Category | Drugs | Number of Patients (%) | Recommendation | Quality of Evidence | Strength of Recommendation |
|---|---|---|---|---|---|
| Antiparkinsonian agents | Trihexyphenidyl | 1 (0.3) | Avoid | Moderate | Strong |
| Central alpha-agonists | Methyldopa | 5 (1.6) | Avoid | Low | Strong |
| Antidepressants | Amitriptyline | 25 (7.8) | Avoid | High | Strong |
| Cardiovascular agents | Diuretics | 32 (10) | Use with caution | Moderate | Strong |
| Aspirin | 22 (6.9) | Use with caution in adults ≥ 70 years | Moderate | Strong | |
| RAS inhibitors or potassium-sparing diuretics | 17 (5.3) | Avoid use in those with CrCl < 30 mL/min | Moderate | Strong | |
| Nifedipine | 9 (2.8) | Avoid | High | Strong | |
| Chlorthalidone | 9 (2.8) | Use with caution | Moderate | Strong | |
| Digoxin | 5 (1.6) | Avoid dosages > 0.125 mg/day | Moderate | Strong | |
| Endocrine agents | Insulin, sliding scale | 28 (8.8) | Avoid | Moderate | Strong |
| Glimepiride | 15 (4.7) | Avoid | Moderate | Strong | |
| Anti-infective agents | Ciprofloxacin | 3 (0.9) | Avoid using when CrCl < 30 mL/min | Moderate | Strong |
| Gastrointestinal agents | Omeprazole | 6 (1.9) | Avoid scheduled use for >8 weeks unless for high-risk patients | High | Strong |
| Pantoprazole | 3 (0.9) | ||||
| Drug–drug interactions | Trimethoprim-sulfamethoxazole + ACE inhibitors | 11 (3.4) | Use with caution in patients on ACEI or ARB and decreasedCrCl | Low | Strong |
| Prazosin + Furosemide | 9 (2.8) | Avoid in older women | Moderate | Strong |
| Multimorbidity | Polypharmacy | PIM Use | ||||
|---|---|---|---|---|---|---|
| Ageing Characteristics | Crude OR | Adjusted OR | Crude OR | Adjusted OR | Crude OR | Adjusted OR |
| Understand verbal and non-verbal communication | 1.32 (1.02–1.71) * | 1.37 (0.97–1.94) | 2.04 (1.04–4.02) * | 2.06 (1.02–4.17) * | 0.47 (0.34–0.65) ** | 0.46 (0.33–0.65) ** |
| Physical fitness † | 0.87 (0.65–1.17) | 0.95 (0.65–1.39) | 0.85 (0.42–1.72) | 0.82 (0.39–1.70) | 0.68 (0.47–0.97) * | 0.69 (0.47–1.00) |
| Using walking assistance devices | 1.01 (0.80–1.27) | 1.15 (0.84–1.58) | 2.52 (1.47–4.32) ** | 2.41 (1.35–4.28) ** | 1.85 (1.36–2.51) ** | 1.83 (1.32–2.53) ** |
| Lack of interest in activities | 0.93 (0.67–1.28) | 0.90 (0.60–1.34) | 1.71 (0.84–3.47) | 1.68 (0.81–3.47) | 1.48 (1.02–2.15) * | 1.46 (1.00–2.14) * |
| Persistent anger with self/others | 1.08 (0.81–1.45) | 1.03 (0.70–1.50) | 2.91 (1.55–5.47) ** | 3.33 (1.71–6.47) ** | 1.18 (0.81–1.70) | 1.21 (0.83–1.78) |
| Cognitive impairment | 0.83 (0.46–1.48) | 0.98 (0.67–1.43) | 1.05 (0.53–2.09) | 1.00 (0.49–2.05) | 1.69 (1.21–2.37) ** | 1.65 (1.15–2.34) ** |
| Had repeated health complaints | 1.11 (0.86–1.44) | 1.07 (0.76–1.50) | 1.45 (0.80–2.63) | 1.45 (0.78–2.69) | 1.31 (0.95–1.80) | 1.32 (0.95–1.84) |
| Experienced fall in the past year | 0.71 (0.51–0.99) * | 0.71 (0.46–1.08) | 1.10 (0.52–2.31) | 1.10 (0.51–2.35) | 1.01 (0.67–1.51) | 0.98 (0.65–1.48) |
| Flare-ups of pain | 1.54 (1.16–2.04) ** | 1.64 (1.13–2.39) ** | 1.94 (1.03–3.67) * | 2.00 (1.03–3.89) * | 0.97 (0.66–1.42) | 0.96 (0.65–1.43) |
| Health fluctuation/deterioration | 0.89 (0.66–1.21) | 0.79 (0.53–1.17) | 0.37 (0.15–0.92) * | 0.40 (0.16–1.01) | 1.58 (1.11–2.24) * | 1.61 (1.11–2.32) ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bhagavathula, A.S.; Seid, M.A.; Adane, A.; Gebreyohannes, E.A.; Brkic, J.; Fialová, D. Prevalence and Determinants of Multimorbidity, Polypharmacy, and Potentially Inappropriate Medication Use in the Older Outpatients: Findings from EuroAgeism H2020 ESR7 Project in Ethiopia. Pharmaceuticals 2021, 14, 844. https://doi.org/10.3390/ph14090844
Bhagavathula AS, Seid MA, Adane A, Gebreyohannes EA, Brkic J, Fialová D. Prevalence and Determinants of Multimorbidity, Polypharmacy, and Potentially Inappropriate Medication Use in the Older Outpatients: Findings from EuroAgeism H2020 ESR7 Project in Ethiopia. Pharmaceuticals. 2021; 14(9):844. https://doi.org/10.3390/ph14090844
Chicago/Turabian StyleBhagavathula, Akshaya Srikanth, Mohammed Assen Seid, Aynishet Adane, Eyob Alemayehu Gebreyohannes, Jovana Brkic, and Daniela Fialová. 2021. "Prevalence and Determinants of Multimorbidity, Polypharmacy, and Potentially Inappropriate Medication Use in the Older Outpatients: Findings from EuroAgeism H2020 ESR7 Project in Ethiopia" Pharmaceuticals 14, no. 9: 844. https://doi.org/10.3390/ph14090844
APA StyleBhagavathula, A. S., Seid, M. A., Adane, A., Gebreyohannes, E. A., Brkic, J., & Fialová, D. (2021). Prevalence and Determinants of Multimorbidity, Polypharmacy, and Potentially Inappropriate Medication Use in the Older Outpatients: Findings from EuroAgeism H2020 ESR7 Project in Ethiopia. Pharmaceuticals, 14(9), 844. https://doi.org/10.3390/ph14090844