Health Benefits and Pharmacological Aspects of Chrysoeriol
Abstract
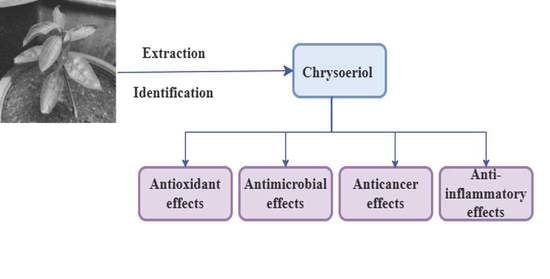
:1. Introduction
2. Sources of Chrysoeriol
3. Biological Properties
3.1. Anticancer Properties
3.2. Anti-Inflammatory Effects
3.3. Antidiabetic Effects
3.4. Anti-Hyperlipidemic Properties
3.5. Antioxidant Properties
3.6. Antimicrobial Activities
3.6.1. Antibacterial Activity
3.6.2. Antifungal Activity
3.7. Chrysoeriol Effect on Prevention and Treatment of Vascular Diseases
3.8. Anti-Osteoporosis Activity of Chrysoeriol
3.9. Neuroprotective Activity
3.10. Chrysoeriol Effect on the Cellular Models of Parkinson’s Disease
3.11. Anti-Insecticidal Activity
3.11.1. Anti Pea Alphid A. pisum Activity
3.11.2. Nodulation Genes Transcription Induction
3.11.3. Anti S. litura Activity
3.11.4. In Vivo Pharmacokinetic Investigations
4. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Prabhakar, K.R.; Srinivasan, K.K.; Rao, P.G.M. Chemical Investigation, Anti-Inflammatory and Wound Healing Properties of Coronopus Didymus. Pharm. Biol. 2002, 40, 490–493. [Google Scholar] [CrossRef]
- Mishra, B.; Priyadarsini, K.I.; Kumar, M.S.; Unnikrishnan, M.K.; Mohan, H. Effect of O-Glycosilation on the Antioxidant Activity and Free Radical Reactions of a Plant Flavonoid, Chrysoeriol. Bioorg. Med. Chem. 2003, 11, 2677–2685. [Google Scholar] [CrossRef]
- Nascimento, P.L.A.; Nascimento, T.C.E.S.; Ramos, N.S.M.; Silva, G.R.; Gomes, J.E.G.; Falcão, R.E.A.; Moreira, K.A.; Porto, A.L.F.; Silva, T.M.S. Quantification, Antioxidant and Antimicrobial Activity of Phenolics Isolated from Different Extracts of Capsicum Frutescens (Pimenta malagueta). Molecules 2014, 19, 5434–5447. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Jin, C.H. Inhibitory Activity of Flavonoids, Chrysoeriol and Luteolin-7-O-Glucopyranoside, on Soluble Epoxide Hydrolase from Capsicum Chinense. Biomolecules 2020, 10, 180. [Google Scholar] [CrossRef]
- Kim, Y.H.; Lee, Y.S.; Choi, E.M. Chrysoeriol Isolated from Eurya Cilliata Leaves Protects MC3T3-E1 Cells against Hydrogen Peroxide-Induced Inhibition of Osteoblastic Differentiation. J. Appl. Toxicol. 2010, 30, 666–673. [Google Scholar] [CrossRef]
- Tai, B.H.; Cuong, N.M.; Huong, T.T.; Choi, E.-M.; Kim, J.-A.; Kim, Y.H. Chrysoeriol Isolated from the Leaves of Eurya Ciliata Stimulates Proliferation and Differentiation of Osteoblastic MC3T3-E1 Cells. J. Asian Nat. Prod. Res. 2009, 11, 817–823. [Google Scholar] [CrossRef]
- Cha, B.-Y.; Shi, W.L.; Yonezawa, T.; Teruya, T.; Nagai, K.; Woo, J.-T. An Inhibitory Effect of Chrysoeriol on Platelet-Derived Growth Factor (PDGF)-Induced Proliferation and PDGF Receptor Signaling in Human Aortic Smooth Muscle Cells. J. Pharm. Sci. 2009, 110, 105–110. [Google Scholar] [CrossRef]
- Liu, G.; Ding, L.; Luo, C.; Yang, H.; Yang, D.; Liang, G.; Wang, L. Protection against DNA Damage and Inhibition of Lipid Peroxidation by Flavones from Eremosparton songoricum (Litv) Vass. Res. Chem. Intermediat. 2006, 32, 145–152. [Google Scholar] [CrossRef]
- Hartwig, U.A.; Maxwell, C.A.; Joseph, C.M.; Phillips, D.A. Chrysoeriol and Luteolin Released from Alfalfa Seeds Induce Nod Genes in Rhizobium Meliloti1. Plant Physiol. 1990, 92, 116–122. [Google Scholar] [CrossRef]
- Zeng, X.; Shi, J.; Zhao, M.; Chen, Q.; Wang, L.; Jiang, H.; Luo, F.; Zhu, L.; Lu, L.; Wang, X.; et al. Regioselective Glucuronidation of Diosmetin and Chrysoeriol by the Interplay of Glucuronidation and Transport in UGT1A9-Overexpressing HeLa Cells. PLoS ONE 2016, 11, e0166239. [Google Scholar] [CrossRef]
- Wei, W.; He, J.; Ruan, H.; Wang, Y. In Vitro and in Vivo Cytotoxic Effects of Chrysoeriol in Human Lung Carcinoma Are Facilitated through Activation of Autophagy, Sub-G1/G0 Cell Cycle Arrest, Cell Migration and Invasion Inhibition and Modulation of MAPK/ERK Signalling Pathway. J. BUON 2019, 24, 936–942. [Google Scholar] [PubMed]
- Carvalho, M.; Silva, B.M.; Silva, R.; Valentão, P.; Andrade, P.B.; Bastos, M.L. First Report on Cydonia Oblonga Miller Anticancer Potential: Differential Antiproliferative Effect against Human Kidney and Colon Cancer Cells. J. Agric. Food Chem. 2010, 58, 3366–3370. [Google Scholar] [CrossRef] [PubMed]
- Wongkularb, S.; Limboonreung, T.; Tuchinda, P.; Chongthammakun, S. Suppression of PI3K/Akt/MTOR Pathway in Chrysoeriol-Induced Apoptosis of Rat C6 Glioma Cells. Vitr. Cell. Dev. Biol. Anim. 2022, 58, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Manurung, K.; Sulastri, D.; Zubir, N.; Ilyas, S. In Silico Anticancer Activity and in Vitro Antioxidant of Flavonoids in Plectranthus Amboinicus. Pharmacogn. J. 2020, 12, 1573–1577. [Google Scholar] [CrossRef]
- Choi, D.-Y.; Lee, J.Y.; Kim, M.-R.; Woo, E.-R.; Kim, Y.G.; Kang, K.W. Chrysoeriol Potently Inhibits the Induction of Nitric Oxide Synthase by Blocking AP-1 Activation. J. Biomed. Sci. 2005, 12, 949–959. [Google Scholar] [CrossRef]
- Moscatelli, V.; Hnatyszyn, O.; Acevedo, C.; Megías, J.; Alcaraz, M.J.; Ferraro, G. Flavonoids from Artemisia Copa with Anti-Inflammatory Activity. Planta Med. 2006, 72, 72–74. [Google Scholar] [CrossRef]
- Xie, C.; Kang, J.; Li, Z.; Schauss, A.G.; Badger, T.M.; Nagarajan, S.; Wu, T.; Wu, X. The Açaí Flavonoid Velutin Is a Potent Anti-Inflammatory Agent: Blockade of LPS-Mediated TNF-α and IL-6 Production through Inhibiting NF-ΚB Activation and MAPK Pathway. J. Nutr. Biochem. 2012, 23, 1184–1191. [Google Scholar] [CrossRef]
- Oh, M.H.; Choe, K.I.; Cho, S.H.; Jeong, M.S.; Myung, S.C.; Seo, S.J.; Choi, S.E.; Lee, M.W. Anti-Oxidative and Anti-Inflammatory Effects of Flavonoids from the Silk of Zea Mays Linn. Asian J. Chem. 2013, 25, 4293–4297. [Google Scholar] [CrossRef]
- Nguyen, T.Y.; To, D.C.; Tran, M.H.; Lee, J.S.; Lee, J.H.; Kim, J.A.; Woo, M.H.; Min, B.S. Anti-Inflammatory Flavonoids Isolated from Passiflora Foetida. Nat. Prod. Commun. 2015, 10, 929–931. [Google Scholar] [CrossRef]
- Yoon, H.-S.; Park, C.M. Chrysoeriol Ameliorates COX-2 Expression through NF-ΚB, AP-1 and MAPK Regulation via the TLR4/MyD88 Signaling Pathway in LPS-Stimulated Murine Macrophages. Exp. Med. 2021, 22, 718. [Google Scholar] [CrossRef]
- Wu, J.-Y.; Chen, Y.-J.; Bai, L.; Liu, Y.-X.; Fu, X.-Q.; Zhu, P.-L.; Li, J.-K.; Chou, J.-Y.; Yin, C.-L.; Wang, Y.-P.; et al. Chrysoeriol Ameliorates TPA-Induced Acute Skin Inflammation in Mice and Inhibits NF-ΚB and STAT3 Pathways. Phytomedicine 2020, 68, 153173. [Google Scholar] [CrossRef] [PubMed]
- Qiu, C.; Xu, Y. Chrysoeriol Attenuates Cisplatin Induced Acute Kidney Injury in A Rat Model by Regulating PI3K/AKT and NF-[Kappa]B Pathways. Curr. Top. Nutraceutical Res. 2021, 19, 366–373. [Google Scholar]
- Ramirez, G.; Zamilpa, A.; Zavala, M.; Perez, J.; Morales, D.; Tortoriello, J. Chrysoeriol and Other Polyphenols from Tecoma Stans with Lipase Inhibitory Activity. J. Ethnopharmacol. 2016, 185, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Vinholes, J.; Grosso, C.; Andrade, P.B.; Gil-Izquierdo, A.; Valentão, P.; de Pinho, P.G.; Ferreres, F. In Vitro Studies to Assess the Antidiabetic, Anti-Cholinesterase and Antioxidant Potential of Spergularia rubra. Food Chem. 2011, 129, 454–462. [Google Scholar] [CrossRef]
- Purnomo, Y.; Soeatmadji, D.W.; Sumitro, S.B.; Widodo, M.A. Anti-Diabetic Potential of Urena Lobata Leaf Extract through Inhibition of Dipeptidyl Peptidase IV Activity. Asian Pac. J. Trop. Biomed. 2015, 5, 645–649. [Google Scholar] [CrossRef]
- Nickavar, B.; Abolhasani, L. Bioactivity-Guided Separation of an α-Amylase Inhibitor Flavonoid from Salvia virgata. Iran. J. Pharm. Res. 2013, 12, 57–61. [Google Scholar]
- Tofighi, Z.; Alipour, F.; Hadavinia, H.; Abdollahi, M.; Hadjiakhoondi, A.; Yassa, N. Effective Antidiabetic and Antioxidant Fractions of Otostegia Persica Extract and Their Constituents. Pharm. Biol. 2014, 52, 961–966. [Google Scholar] [CrossRef]
- Salib, J.Y.; Michael, H.N.; Eskande, E.F. Anti-Diabetic Properties of Flavonoid Compounds Isolated from Hyphaene Thebaica Epicarp on Alloxan Induced Diabetic Rats. Pharmacogn. Res. 2013, 5, 22–29. [Google Scholar] [CrossRef]
- Krishnan, B.; Ramu Ganesan, A.; Balasubramani, R.; Nguyen, D.D.; Chang, S.W.; Wang, S.; Xiao, J.; Balasubramanian, B. Chrysoeriol Ameliorates Hyperglycemia by Regulating the Carbohydrate Metabolic Enzymes in Streptozotocin-Induced Diabetic Rats. Food Sci. Hum. Wellness 2020, 9, 346–354. [Google Scholar] [CrossRef]
- Krishnan, B.; Pugalendi, K.V.; Saravanan, R. Ameliorative Potential of Chrysoeriol, a Bioactive Flavonoid on Oxidative Stress and Hepatic Marker Enzymes in STZ Induced Diabetic Rats. Available online: https://www.semanticscholar.org/paper/Ameliorative-potential-of-Chrysoeriol%2C-a-bioactive-Krishnan-Pugalendi/a57efa04660e33ed138000e08ee711845f982eb1 (accessed on 6 May 2022).
- Rauter, A.P.; Martins, A.; Borges, C.; Mota-Filipe, H.; Pinto, R.; Sepodes, B.; Justino, J. Antihyperglycaemic and Protective Effects of Flavonoids on Streptozotocin-Induced Diabetic Rats. Phytother. Res. 2010, 24 (Suppl. 2), S133–S138. [Google Scholar] [CrossRef]
- Elshamy, A.I.; El- Shazly, M.; Yassine, Y.M.; El- Bana, M.A.; Farrag, A.-R.; Nassar, M.I.; Singab, A.N.; Noji, M.; Umeyama, A. Phenolic Constituents, Anti-Inflammatory and Antidiabetic Activities of Cyperus laevigatus L. Pharmacogn. J. 2017, 9, 828–833. [Google Scholar] [CrossRef]
- Baskaran, K.; Pugalendi, K.V.; Saravanan, R. Antidiabetic and Antihyperlipidemic Activity of Chrysoeriol in Diabetic Rats, Role of HMG CoA Reductase, LCAT and LPL: In Vivo and in Silico Approaches. J. Pharm. Res. 2015, 9, 597–605. [Google Scholar]
- Bashyal, P.; Parajuli, P.; Pandey, R.P.; Sohng, J.K. Microbial Biosynthesis of Antibacterial Chrysoeriol in Recombinant Escherichia Coli and Bioactivity Assessment. Catalysts 2019, 9, 112. [Google Scholar] [CrossRef]
- Miski, M.; Ulubelen, A.; Johansson, C.; Mabry, T.J. Antibacterial Activity Studies of Flavonoids from Salvia Palaestina. J. Nat. Prod. 1983, 46, 874–875. [Google Scholar] [CrossRef]
- Shao, G.; Chen, S.; Sun, Y.; Xu, H.; Ge, F. Chrysoeriol Promotes Functional Neurological Recovery in a Rat Model of Cerebral Ischemia. Pharmacogn. Mag. 2021, 17, 802. [Google Scholar] [CrossRef]
- Limboonreung, T.; Tuchinda, P.; Chongthammakun, S. Chrysoeriol Mediates Mitochondrial Protection via PI3K/Akt Pathway in MPP+ Treated SH-SY5Y Cells. Neurosci. Lett. 2020, 714, 134545. [Google Scholar] [CrossRef]
- Liu, Z.; Song, X.; Xin, Y.; Wang, X.; Yu, H.; Bai, Y.; Liu, J.; Zhang, C.; Hui, R. Protective Effect of Chrysoeriol against Doxorubicin-Induced Cardiotoxicity in Vitro. Chin. Med. J. 2009, 122, 2652–2656. [Google Scholar]
- Khan, A.; Gilani, A.H. Selective Bronchodilatory Effect of Rooibos Tea (Aspalathus linearis) and Its Flavonoid, Chrysoeriol. Eur. J. Nutr. 2006, 45, 463–469. [Google Scholar] [CrossRef]
- Ruttanaphan, T.; Thitathan, W.; Piyasaengthong, N.; Nobsathian, S.; Bullangpoti, V. Chrysoeriol Isolated from Melientha Suavis Pierre with Activity against the Agricultural Pest Spodoptera litura. Chem. Biol. Technol. Agric. 2022, 9, 21. [Google Scholar] [CrossRef]
- Demirtas, I.; Erenler, R.; Elmastas, M.; Goktasoglu, A. Studies on the Antioxidant Potential of Flavones of Allium Vineale Isolated from Its Water-Soluble Fraction. Food Chem. 2013, 136, 34–40. [Google Scholar] [CrossRef]
- Park, C.M. Fortified Antioxidative Potential by Chrysoeriol through the Regulation of the Nrf2/MAPK-Mediated HO-1 Signaling Pathway in RAW 264.7 Cells. J. Life Sci. 2018, 28, 43–49. [Google Scholar] [CrossRef]
- Singh, D.; Gupta, R.S. Modulatory Influence of Abutilon Indicum Leaves on Hepatic Antioxidant Status and Lipid Peroxidation against Alcohol-Induced Liver Damage in Rats. Pharmacologyonline 2008, 1, 253–262. [Google Scholar]
- Liu, Y.; Han, C.; Lu, T.; Liu, Y.; Chen, H.; Yang, C.; Tu, Y.; Li, Y. Investigation of the Interaction between Chrysoeriol and Xanthine Oxidase Using Computational and in Vitro Approaches. Int. J. Biol. Macromol. 2021, 190, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Supriadin, A.; Juliani, H.; Tanyela, N. Isolation Flavonoid Compound Chrysoeriol from Ethyl Acetate Extract of Zaitun Leaves (Olea europaea). J. Phys. Conf. Ser. 2021, 1869, 012052. [Google Scholar] [CrossRef]
- Díaz, A.E.C.; Herfindal, L.; Rathe, B.A.; Sletta, K.Y.; Vedeler, A.; Haavik, S.; Fossen, T. Cytotoxic Saponins and Other Natural Products from Flowering Tops of Narthecium ossifragum L. Phytochemistry 2019, 164, 67–77. [Google Scholar] [CrossRef]
- Vestena, A.; Comerlato, L.; Bridi, H.; Guerini, L.; Ccana-Ccapatinta, G.V.; Vignoli-Silva, M.; Apel, M.A.; Fernandes, S.; Castro-Gamboa, I.; Zuanazzi, J.A.S. Chrysoeriol Derivatives and Other Constituents from Glandularia Selloi. Phytochem. Lett. 2019, 29, 30–34. [Google Scholar] [CrossRef]
- Khallouki, F.; Ricarte, I.; Breuer, A.; Owen, R.W. Characterization of Phenolic Compounds in Mature Moroccan Medjool Date Palm Fruits (Phoenix dactylifera) by HPLC-DAD-ESI-MS. J. Food Compos. Anal. 2018, 70, 63–71. [Google Scholar] [CrossRef]
- Tagousop, C.N.; Ngnokam, D.; Harakat, D.; Voutquenne-Nazabadioko, L. Three New Flavonoid Glycosides from the Aerial Parts of Graptophyllum Grandulosum Turril (Acanthaceae). Phytochem. Lett. 2017, 19, 172–175. [Google Scholar] [CrossRef]
- Farid, M.M.; Hussein, S.R.; Ibrahim, L.F.; El Desouky, M.A.; Elsayed, A.M.; El Oqlah, A.A.; Saker, M.M. Cytotoxic Activity and Phytochemical Analysis of Arum palaestinum Boiss. Asian Pac. J. Trop. Biomed. 2015, 5, 944–947. [Google Scholar] [CrossRef]
- Benyahia, S.; Benayache, F.; Benayache, S. Flavonoids from Artemisia Arborescens. Chem. Nat. Compd. 2014, 49, 1132–1133. [Google Scholar] [CrossRef]
- Goławska, S.; Łukasik, I.; Kapusta, I.; Janda, B. Do the Contents of Luteolin, Tricin, and Chrysoeriol Glycosides in Alfalfa (Medicago sativa L.) Affect the Behavior of Pea Aphid (Acyrthosiphon pisum)? Pol. J. Environ. Stud. 2012, 21, 1613–1619. [Google Scholar]
- Goławska, S.; Łukasik, I.; Kapusta, T.; Janda, B. Analysis of Flavonoids Content in Alfalfa. Ecol. Chem. Eng. A 2010, 17, 261–267. [Google Scholar]
- Iwashina, T.; Smirnov, S.V.; Damdinsuren, O.; Kondo, K. Saussurea Species from the Altai Mountains and Adjacent Area, and Their Flavonoid Diversity. Bull. Natl. Mus. Nat. Sci. Ser. B 2010, 36, 141–154. [Google Scholar]
- Iwashina, T.; Kokubugata, G. Flavonoids in the Leaves and Flowers of Myoporum Bontioides Native to Northernmost Region in the Myoporaceae. Bull. Natl. Sci. Mus. Ser. B 2010, 36, 117–125. [Google Scholar]
- Delazar, A.; Sabzevari, A.; Mojarrab, M.; Nazemiyeh, H.; Esnaashari, S.; Nahar, L.; Razavi, S.M.; Sarker, S.D. Free-Radical-Scavenging Principles from Phlomis Caucasica. J. Nat. Med. 2008, 62, 464–466. [Google Scholar] [CrossRef]
- Suzuki, R.; Iijima, M.; Okada, Y.; Okuyama, T. Chemical Constituents of the Style of Zea Mays L. with Glycation Inhibitory Activity. Chem. Pharm. Bull. 2007, 55, 153–155. [Google Scholar] [CrossRef]
- Marin, P.D.; Veitch, N.C.; Grayer, R.J.; Kite, G.C.; Soković, M.; Janaćković, P. Flavonoids from Phlomis Fruticosa (Lamiaceae) Growing in Montenegro. Biochem. Syst. Ecol. 2007, 35, 462–466. [Google Scholar] [CrossRef]
- Amani, S.A.; Maitland, D.J.; Soliman, G.A. Hepatoprotective Activity of Schouwia Thebica Webb. Bioorganic Med. Chem. Lett. 2006, 16, 4624–4628. [Google Scholar]
- Mericli, A.H.; Seyhan, G.V. Constituents of Cynara Syriaca. Leaves. Pharm. Biol. 2006, 44, 643–645. [Google Scholar] [CrossRef]
- Sarkhail, P.; Monsef-Esfehani, H.R.; Amin, G.; Surmaghi, M.H.S.; Shafiee, A. Phytochemical Study of Phlomis Olivieri Benth. and Phlomis persica Boiss. Daru J. Pharm. Sci. 2006, 14, 115–121. [Google Scholar]
- Şahin, F.P.; Ezer, N.; Çalış, İ. Three Acylated Flavone Glycosides from Sideritis Ozturkii Aytac & Aksoy. Phytochemistry 2004, 65, 2095–2099. [Google Scholar] [PubMed]
- Stochmal, A.; Simonet, A.M.; Macias, F.A.; Oleszek, W. Alfalfa (Medicago sativa L.) Flavonoids. 2. Tricin and Chrysoeriol Glycosides from Aerial Parts. J. Agric. Food Chem. 2001, 49, 5310–5314. [Google Scholar] [CrossRef] [PubMed]
- Bucar, F.; Ninov, S.; Ionkova, I.; Kartnig, T.; Schubert-Zsilavecz, M.; Asenov, I.; Konuklugil, B. Flavonoids from Phlomis Nissolii. Phytochemistry 1998, 48, 573–575. [Google Scholar] [CrossRef]
- Yamabe, N.; Kang, K.S.; Lee, A.Y.; Lee, D.; Choi, J.M.; Lee, S.; Park, J.Y.; Hwang, G.S.; Kim, H.Y.; Cho, E.-J.; et al. Identification of Anti-Cancer Active Components of Taraxacum Coreanum on Human Gastric Cancer AGS Cells. J. Korean Soc. Appl. Biol. Chem. 2014, 57, 187–190. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, Z.; Min, Q.; Palida, A.; Zhang, Y.; Tang, R.; Chen, L.; Li, H. 8-Chrysoeriol, as a Potential BCL-2 Inhibitor Triggers Apoptosis of SW1990 Pancreatic Cancer Cells. Bioorg. Chem. 2018, 77, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.-Y.; Hyun, C.-G. Chrysoeriol Enhances Melanogenesis in B16F10 Cells Through the Modulation of the MAPK, AKT, PKA, and Wnt/β-Catenin Signaling Pathways. Nat. Prod. Commun. 2022, 17, 1934578X211069204. [Google Scholar] [CrossRef]
- Min, D.Y.; Jung, E.; Ahn, S.S.; Lee, Y.H.; Lim, Y.; Shin, S.Y. Chrysoeriol Prevents TNFα-Induced CYP19 Gene Expression via EGR-1 Downregulation in MCF7 Breast Cancer Cells. Int. J. Mol. Sci. 2020, 21, 7523. [Google Scholar] [CrossRef] [PubMed]
- Zingue, S.; Gbaweng Yaya, A.J.; Michel, T.; Ndinteh, D.T.; Rutz, J.; Auberon, F.; Maxeiner, S.; Chun, F.K.-H.; Tchinda, A.T.; Njamen, D.; et al. Bioguided Identification of Daucosterol, a Compound That Contributes to the Cytotoxicity Effects of Crateva adansonii DC (Capparaceae) to Prostate Cancer Cells. J. Ethnopharmacol. 2020, 247, 112251. [Google Scholar] [CrossRef]
- Cui, M.-Y.; Lu, A.-R.; Li, J.-X.; Liu, J.; Fang, Y.-M.; Pei, T.-L.; Zhong, X.; Wei, Y.-K.; Kong, Y.; Qiu, W.-Q.; et al. Two Types of O-Methyltransferase Are Involved in Biosynthesis of Anticancer Methoxylated 4’-Deoxyflavones in Scutellaria Baicalensis Georgi. Plant Biotechnol. J. 2022, 20, 129–142. [Google Scholar] [CrossRef]
- Qiu, D.; Zhou, M.; Lin, T.; Chen, J.; Wang, G.; Huang, Y.; Jiang, X.; Tian, W.; Chen, H. Cytotoxic Components from Hypericum Elodeoides Targeting RXRα and Inducing HeLa Cell Apoptosis through Caspase-8 Activation and PARP Cleavage. J. Nat. Prod. 2019, 82, 1072–1080. [Google Scholar] [CrossRef]
- Singh, N.; Baby, D.; Rajguru, J.P.; Patil, P.B.; Thakkannavar, S.S.; Pujari, V.B. Inflammation and Cancer. Ann. Afr. Med. 2019, 18, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Csupor, D.; Widowitz, U.; Blazsó, G.; Laczkó-Zöld, E.; Tatsimo, J.S.N.; Balogh, A.; Boros, K.; Dankó, B.; Bauer, R.; Hohmann, J. Anti-Inflammatory Activities of Eleven Centaurea Species Occurring in the Carpathian Basin. Phytother. Res. 2013, 27, 540–544. [Google Scholar] [CrossRef]
- Hostetler, G.; Riedl, K.; Cardenas, H.; Diosa-Toro, M.; Arango, D.; Schwartz, S.; Doseff, A.I. Flavone Deglycosylation Increases Their Anti-Inflammatory Activity and Absorption. Mol. Nutr. Food Res. 2012, 56, 558–569. [Google Scholar] [CrossRef] [PubMed]
- Bolkent, S.; Yanardağ, R.; Tabakoğlu-Oğuz, A.; Ozsoy-Saçan, O. Effects of Chard (Beta vulgaris L. Var. Cicla) Extract on Pancreatic B Cells in Streptozotocin-Diabetic Rats: A Morphological and Biochemical Study. J. Ethnopharmacol. 2000, 73, 251–259. [Google Scholar] [CrossRef]
- Deacon, C.F. Dipeptidyl Peptidase 4 Inhibitors in the Treatment of Type 2 Diabetes Mellitus. Nat. Rev. Endocrinol. 2020, 16, 642–653. [Google Scholar] [CrossRef]
- Sivieri, K.; de Oliveira, S.M.; de Souza Marquez, A.; Pérez-Jiménez, J.; Diniz, S.N. Insights on β-glucan as a prebiotic coadjuvant in the treatment of Diabetes Mellitus: A review. Food Hydrocoll. Health 2022, 2, 100056. [Google Scholar] [CrossRef]
- Jang, Y.-H.; Park, J.-R.; Kim, K.-M. Antimicrobial Activity of Chrysoeriol 7 and Chochlioquinone 9, White-Backed Planthopper-Resistant Compounds, Against Rice Pathogenic Strains. Biology 2020, 9, 382. [Google Scholar] [CrossRef]
- Chen, Z.; Kong, S.; Song, F.; Li, L.; Jiang, H. Pharmacokinetic Study of Luteolin, Apigenin, Chrysoeriol and Diosmetin after Oral Administration of Flos Chrysanthemi Extract in Rats. Fitoterapia 2012, 83, 1616–1622. [Google Scholar] [CrossRef]



| Source | Country | Part | Extract | Extraction Methods | References |
|---|---|---|---|---|---|
| Melientha suavis Pierre | Thailand | Leaves and twigs | Dichloromethane | Maceration | [40] |
| Olea europaea L. | Indonesia | Leaves | Ethyl acetate | Maceration | [45] |
| Capsicum chinense Jacq. | Korea | Leaves | Methanol | Maceration | [4] |
| Narthecium ossifragum (L.) Huds. | Norway | Flowers | Methanol | Maceration | [46] |
| Glandularia selloi (Spreng.) Tronc. | Brazil | Aerial parts and roots | Methanol | Maceration | [47] |
| Phoenix dactylifera L. | Morocco | Fruit flesh and pits | Hexane and methanol | Soxhlet apparatus | [48] |
| Graptophyllum grandulosum Turill | Cameroon | Aerial parts | Methanol | Maceration | [49] |
| Cardiospermum halicacabum L. | India | Leaves | - | - | [33] |
| Arum palaestinum Boiss. | Jordan | Aerial parts | Diethyl ether | Maceration | [50] |
| Artemisia arborescens L. | Algeria | Aerial parts | n-butanol | Maceration | [51] |
| Capsicum frutescens L. | Brazil | Seeds, peel, and whole fruits | Hexane and acetonitrile | Ultrasonication | [3] |
| Allium vineale L. | Turkey | Leaves | Methanol and ethyl acetate | Decoction | [41] |
| Medicago sativa L. | Poland | Aerial parts | - | ASE 200 Accelerated Solvent Extractor | [52] |
| Medicago sativa L. | Poland | Aerial parts | - | ASE 200 Accelerated Solvent Extractor | [53] |
| Saussurea alpina L. | Russia and Mongolia | Aerial parts | Methanol | Maceration | [54] |
| Saussurea daurica L. | |||||
| Saussurea laciniata L. | |||||
| Saussurea pricei L. | |||||
| Saussurea pseudo-alpina L. | |||||
| Saussurea salicifolia L. | |||||
| Saussurea salsa L. | |||||
| Myoporum bontiodes spp. | Japan | Flowers and leaves | Methanol | Maceration | [55] |
| Eurya cilliata Merr. | Vietnam | Leaves | - | Maceration | [5] |
| Eurya ciliata Merr. | Vietnam | Leaves | Methanol | Maceration | [38] |
| Eremosparton Songoricum (Litv) Vass. | China | Leaves and caudexes | Methanol and ethyl acetate | Maceration | [38] |
| Phlomis caucasica Rech. | Iran | Aerial parts | Methanol | Soxhlet apparatus | [56] |
| Zea mays L. | Japan | Styles | Methanol and aqueous extracts | Maceration | [57] |
| Phlomis fruticosa L. | Balkans | Leaves | Methanol | Decoction | [58] |
| Schouwia thebica Webb | Egypt | Aerial parts | Ethanol | Maceration | [59] |
| Alhagi maurorum Medik. | Egypt | Aerial parts | Ether, chloroform, ethyl acetate, and n-butanol | Maceration | [59] |
| Aspalathus linearis (Burm.f.) R.Dahlgr. | South Africa | Leaves | aqueous extracts | Decoction | [39] |
| Cynara syriaca L. | Turkey | Leaves | Ethyl acetate | Soxhlet apparatus | [60] |
| Phlomis olivieri Benth. | Iran | Aerial parts | Ethyl acetate and n-butanol | Percolator | [61] |
| Phlomis persica Boiss. | |||||
| Sideritis ozturkii Aytac & Aksoy | Turkey | Aerial parts | Acetone | Maceration | [62] |
| Salix matsudana spp. | China | Leaves | Ethanol | Maceration | [2] |
| Coronopus didymus (L.) Sm. | India | Whole plant | Petrol ether, diethyl ether, ethyl acetate, and n-butanol | Soxhlet apparatus | [2] |
| Coronopus didymus (L.) Sm. | India | Whole plant | Petrol ether, diethyl ether, ethyl acetate, and n-butanol | Soxhlet apparatus | [1] |
| Medicago sativa L. | Poland | Aerial parts | Methanol | Maceration | [63] |
| Phlomis nissolii L. | Turkey | Aerial parts | Methanol | Maceration | [64] |
| Cell Lines | Key Results | References |
|---|---|---|
| Cell line A549 from lung cancer | IC50 = 16.95 Μm. Inhibited growth of A549 cells. Induced autophagy. Caused sub-G1/G0 arrest cells. Decreased cell migration and invasion. Inhibited tumor growth in vivo at the dosage of 50 mg/Kg. Inhibited the expression of p-p38 and p-ERK1/2 pathway. | [11] |
| Colon cancer cells HT-29, uterine cancer cells HeLa, and lymphoma cells HL-60 | Selectively killed leukemic cells. Up-regulated NFAT transcriptional pathways. Amplificated intracellular ROS in HL-60 cells. Exhibited cytotoxic potential and NF-κB p65 inhibition in HL-60 cells. | [5] |
| HeLa-UGT1A9 cells A549 and HepG2 cells Human-expressed UGT enzymes | Ko143 inhibited the efflux of glucuronides. Ko143 increased intracellular glucuronides. BCRP-mediated chrysoeriol glucuronide. Chrysoeriol with Ko143 decreased the A549 and HepG2 cell viability. | [10] |
| Human gastric cancer AGS cells | Exhibited a level of cytotoxicity against AGS cells that was moderate. Cleavage of poly (ADP-ribose) polymerase that is induced by an external stimulus (PARP). Caspase-3 and caspase-8 that have been activated. | [65] |
| SW1990 pancreatic cancer cells | IC50 = 56.35 ± 6.96 μM. Exhibited stronger pro-apoptosis effect against SW1990 cells. Targeted potentially to BCL-2. Identified as a BH3 mimetic. | [66] |
| C6 glioma cells | Decreased cell viability. Induced apoptosis. Bax/Bcl-2 ratio increased. Caspases-3/caspase-3 ratio cleaved. Reduced the phosphorylation of PI3K, Akt, and mTOR expression. | [13] |
| Renal carcinomas A-498 and 769-P, as well as colon cancers Caco-2 | Exhibited anti-proliferative effect. Inhibited cell growth of A-498 (91%) and 769-P cells (84%). Repressed cell growth of Caco-2 colon cancer cells (IC50 = 239.7 ± 43.2 μg/mL). | [12] |
| In silico against several cancer receptors | IC50 = 8.26 µg/Ml. P-Glycoprotein-1, cyclin-dependent kinase-2, and phosphoinositide-3-kinase receptors showed anticancer action. Induced antiproliferative activity for the Cyclooxygenase-2/phosphoenolpyruvate carboxykinase receptors. | [14] |
| Melanogenesis in B16F10 cells | Increased the expression of TRY/TRP-1/TRP-2. Up-regulated the expression of MITF. Suppressed the phosphorylation of ERK/AKT. Increased the phosphorylation of p38 MAPK/GSK-3β/β-catenin/PKA. Decreased the production of β-catenin. | [67] |
| MCF-7 breast cancer cells | Significantly inhibited TNFα-induced EGR-1 expression. Significantly inhibited TNFα-induced CYP19 expression. Suppressed ERK1/2-mediated EGR-1 expression. | [68] |
| HeLa cells | Inhibited the 9-cis-RA induced RXRα transcription. Exhibited concentration-dependent inhibitory effects (12.5–50 μmol/L). | [69] |
| Experimental Approaches | Key Results | References |
|---|---|---|
| TPA (12-O-tetradecanoylphorbol-13-acetate)—a mouse model of induced otitis media | Skin irritation was reduced to a more manageable level. Thinning of the earlobes. Reduced ear heaviness. Inflamed ear tissues had a lower number of inflammatory cells. Reduced protein levels of Ser536, Tyr705, iNOS, COX-2, IL-6, IL-1β, and TNF-α. | [21] |
| RAW264.7 cells activated with LPS | The synthesis of NO and prostaglandin E2 was reduced due to lower amounts of Ser536, Tyr705, iNOS, COX-2, IL-6, IL-1β, and TNF-β in the proteins. Inhibited the phosphorylation of inhibitor of κB (Ser32)/ p65 (Ser536)/Janus kinase 2 (Tyr1007/1008). Decreased nuclear localization of p50/p65/STAT3. Down-regulated mRNA levels of pro-inflammatory cytokines IL-6/IL-1β/ TNF-α. | |
| LPS-stimulated Raw264.7 cells | The cells treated with it were unable to release NO. Inhibited the LPS-induced inductions of iNOS gene. Suppressed AP-1 activation. | [15] |
| Carrageenan-induced hind paw edema model | Significantly reduced the edema volume at 2 h (ethanol extract). Significantly reduced the edema volume at 1 h and 3 h (aqueous extract). | [1] |
| LPS-stimulated RAW264.7 cells | Inhibited NO production (397.7 ± 16 ng/mL). Inhibited COX-1 activity (19.3 ± 0.7 ng/mL). Partially inhibited sPLA2 (2127.9 ± 64.5 ng/mL). Partially inhibited synovial phospholipase A2 activity. | [16] |
| RAW264.7 cells activated with LPS | IL-6 and TNF-α expression was only moderately reduced at 20 μM. Only slightly inhibited p38 phosphorylation. No inhibitory effect against JNK phosphorylation. | [17] |
| LPS-induced HaCaT human keratinocyte cells | Strongly inhibited LPS-induced iNOS and COX-2. | [18] |
| LPS-stimulated RAW264.7 cells | IC50 = 3.1 μM. Significantly inhibited NO production. | [19] |
| Induced Acute Kidney Injury in A Rat Model | Exhibited a reno-protection against cisplatin-induced acute kidney injury. Inactivated NF-κB pathway. Activated PI3K/AKT pathway. | [22] |
| RAW 264.7 cell line | Significantly inhibited LPS-induced PGE2 and COX-2. Activated transcription factors NF-κB and AP-1. Abolished LPS-induced phosphorylation levels of PI3K/Akt/MAPK. Inhibited the LPS-induced activation of TLR4/MyD88. | [20] |
| Experimental Approach | Key Results | References |
|---|---|---|
| Spectrophotometric analysis | IC50 = 158 µM. Inhibited pancreatic lipase activity. Exhibited mixed and non-competitive inhibition. | [23] |
| Streptozotocin (STZ)-induced diabetic rats | Showed an antidiabetic effect. Significantly decreased the levels of glucose. HbA1c levels were significantly reduced. Insulin levels were significantly raised. | [33] |
| Streptozotocin-induced diabetic mice | Exhibited antihyperglycemic effect. At dosages of 300 and 400 mg/kg, this drug reduces blood glucose levels. | [27] |
| Gly-pro-p-nitroanilide and vildagliptin | Inhibited dipeptidyl peptidase IV activity. | [25] |
| Streptozotocin (STZ)-induced diabetic rats | Reduced plasma glucose level. Reduced Hb and HbA1C level. Increased insulin sensitivity in the bloodstream. Glucose 6-phosphatase, fructose 1,6-bisphosphatase, and glycogen phosphorylase are among the enzymes that have been down-regulated. Hexokinase, glucose-6-phosphate dehydrogenase, pyruvate kinase, and hepatic glycogen levels were among the enzymes that were shown to have increased activity. Showed greatest ligand binding energy. Up-regulated the carbohydrate metabolic enzymes. Showed the turnover of pancreatic β cells. | [29] |
| α-Amylase inhibition test | IC50 = 1.27 (1.21–1.33) Mm. % of inhibition = 58.98 ± 1.20. Inhibited the α-amylase activity concentration dependently. | [26] |
| α-Glucosidase inhibitory assay | IC50 = 2.55 mg/mL. Showed α-glucosidase inhibition. | [24] |
| Rats were made diabetic with the drug streptozotocin (STZ). | Exhibited antidiabetic effects in rats that had STZ diabetes produced in them. Lowered concentrations of glucose, glucagon, and NO in the serum. An elevated insulin concentration prompted an increase in paraoxonase activity. | [32] |
| Streptozotocin (STZ) caused diabetic rats Oral glucose tolerance test | Significantly lowered the blood glucose levels (4 mg/kg b.w./day). Exerted an efficient protection on liver and kidney. Significantly enhanced oral glucose tolerance. | [31] |
| Molecule | Origin | Used Methods | Experimental Approaches | Key Results | References |
|---|---|---|---|---|---|
| Chrysoeriol Chrysoeriol-6-O-acetyl-40-b-d-glucoside | Coronopus didymus | Ethanol extract Diethyl ether extract Ethyl acetate n-butanol extract Methanol | DPPH. Lipid peroxidation brought about by exposure to g-radiation, iron (III), and iron (II). | Inhibit enzymatically produced superoxide anion by xanthine/xanthine oxidase system. Antioxidant activity is high in chrysoeriol. Inhibition of lipid peroxidation and peroxyl radical reactions are reduced by O-glycosylation of chrysoeriol. The glycoside is more effective than the aglycone at scavenging DPPH radicals and inhibiting xanthine/xanthine oxidase. | [2] |
| Chrysoeriol-7-O-[2′’-O-E-feruloyl]-b-D-glucoside chrysoeriol | Allium vineale L. (Leaves) | Water-soluble ethyl acetate Methanol in hexane (0–100% ethyl acetate and methanol) | The ferric thiocyanate method, ferric ion (Fe3+)-reducing antioxidant power assay (FRAP). Ferrous ion (Fe2+) metal chelating activity, DPPH. | Free hydroxyl groups were a source of hydrogen atom(s) in the neutralization of radical species of isolated flavonoids, affecting the stability of a flavonoid radical generated by the abstraction of a hydrogen atom from another hydroxyl group. The ability of crude extract, separated flavonoids, and standard compounds to scavenge free radicals resulted in a statistically significant (p < 0.01) reduction in the concentration of DPPH radical (BHT, BHA, and a-tocopherol). | [41] |
| Chrysoeriol | Eurya cilliata | Sirius Red-based colorimetric assay. ALP activity assay. Calcium deposition assay. Sandwich ELISA assay. B-glycerophosphate and 50 mg/ ml ascorbic acid. Buffer for the lysis of protein (50 mM Tris, pH 7.5; 10 mM EDTA, pH 8; 1 mM PMSF). Lipid peroxidation assay. | Chrysoeriol can protect osteoblasts from oxidative stress-induced toxicity. In the presence of H2O2, the cytotoxic impact that was caused by H2O2 was neutralized by chrysoeriol, which also led to an increase in the osteoblasts’ collagen content, alkaline phosphatase activity, and calcium deposition. The fact that the impact of chrysoeriol may be blocked by ICI182780 shows that it may be somewhat involved in the action of estrogen. H2O2-induced reduction of osteocalcin was recovered in the presence of chrysoeriol. In the presence of H2O2, the generation of receptor activator of nuclear factor-kB ligand, interleukin-6, protein carbonyl, and malondialdehyde was considerably reduced by chrysoeriol in MC3T3-E1 cells. | [5] | |
| Chrysoeriol | Capsicum frutescens | Hexane extract Acetonitrile extract | Assay for the Removal of Free Radicals Using the DPPH. Radical Cation Assay with ABTS. β-Carotene Bleaching Test. | The acetonitrile extract of the seeds, skin, and entire fruits contained capsaicin as the primary component, with dihydrocapsaicin and chrysoeriol also present in abundant amounts. The acetonitrile extract of seeds had a greater concentration of chrysoeriol (11.4 mg g−1) than the acetonitrile extract of peel. However, chrysoeriol exhibited a lower level of antioxidant activity in comparison to capsaicin and dihydrocapsaicin. | [3] |
| Chrysoeriol | Capsicum chinense (leaves) | Methanol extract Twice extraction | Epoxide hydrolase sEH assay. | IC50 values of 11.6 ± 2.9. Chrysoeriol was discovered to bind into the allosteric site of sE hydrolase in a non-competitive manner, with Ki values ranging from 10.5 ± 3.2. | [4] |
| Chrysoeriol | Purchased | Dulbecco’s modified Eagle medium (DMEM) containing fetal bovine serum (FBS) and glutamine was used for the cell culture. MTS assay Formazan product measure ROS-dependent oxidation of DCFH-DA to DCF in RAW 264.7 cells line. ROS generation. NE-PER Nuclear and Cytoplasmic Extraction. Western blot analysis RAW 264.7 cells line. | Through the modulation of the Nrf2/MAPK signaling pathway, chrysoeriol was able to improve the antioxidative potential that is mediated by HO-1. HO-1 overexpression caused by chrysoeriol, which was mediated via extracellular signal-regulated kinase, c-Jun NH2-terminal kinase, and phosphorylation of p38. Chrysoeriol. Scavenged intracellular ROS generation caused by lipopolysaccharide in a dose-dependent manner, without causing any cytotoxicity. Induction of nuclear factor-erythroid 2 p45-related factor 2 into the nucleus by chrysoeriol resulted in the production of the phase II enzyme known as heme oxygenase-1, which is responsible for antioxidative activity. Chrysoeriol also promoted the production of heme oxygenase-1. | [42] | |
| Chrysoeriol | Cardiospermum halicacabum leaves | Streptozotocin (STZ)-treated diabetic rats. Glucose oxidase method. Plasma insulin assay. Biochemical measurements. LPO in liver, kidney, and heart estimation. | In diabetic rats, the levels of non-enzymatic antioxidants such as vitamin C, vitamin E, and reduced glutathione, as well as the activities of the enzymatic antioxidants superoxide dismutase, catalase, and glutathione peroxidase, were reduced. | [30] | |
| Chrysoeriol | Eremosparton songoricum | Ethanol extract | PBMCs separation by lymphocyte separation medium. Comet assay. Lipid peroxidation induced by Fe2+/ascorbate in rat liver. Microsoma in rats’ liver. Single-cell gel electrophoresis to detect damaged cells. Thiobarbituric acid reactive substances (TBARS) were shown to be a lipid peroxidation product. | Oxidative activity on the protection of DNA damage and lipid peroxidation. IC50 = 11.9 µM. | [8] |
| Chrysoeriol Chrysoeriol-7-O-beta glucopyranoside | Abutilon indicum L. | Leaves shade dried and pulverized Ethanol (95% v/v) extract NMR and mass spectrometric evaluation | Up to 3g/kg of compound administration to rats in graded doses. By performing a heart puncture, blood samples were taken, and the serum was analyzed for a number of different antioxidant indicators. Lipid peroxidation monitoring in both serum and liver to evaluate unsaturated fatty acid formation in the hepatic cells. | Chrysoeriol and Chrysoeriol-7-O-beta glucopyranoside among other components show that peroxidative damage was minimal in both liver and serum decrease in liver and blood serum in the levels of enzymic and non-enzymic antioxidants such as superoxide dismutase, catalase, glutathione peroxidase, glutathione reductase, glutathione-S-transferase, glutathione, vitamin C, vitamin E, ceruloplasmin, and β-carotene, which are all important factors. | [43] |
| Origin | Used Methods | Tested Strains | Key Results | References |
|---|---|---|---|---|
| Escherichia coli cells by microbial biotransformation | Disc diffusion assay 40 µg per disc | Gram positive Staphylococcus aureus Bacillus subtilis Enterococcus faecalis Kocuria rhizophilla Gram negative Salmonella enterica Klebsiella pneumonia Escherichia coli Proteus hauseri | MIC = 1.25 µg/mL against Staphylococcus aureus. MIC= 30 µg/mL against Proteus hauseri. | [34] |
| Capsicum frutescens (Pimenta Malagueta) | Broth micro-dilution assay | Gram negative Escherichia coli Pseudomonas aeruginosa Klebsiella pneumonia Gram positive Enterococcus faecalis Bacillus subtillis Staphylococcus aureus | MIC = 0.06 µg/mL MIC = 0.12 µg/mL MIC = 0.25 µg/mL MIC = 1 µg/mL MIC = 1 µg/mL MIC = 0.25 µg/mL | [3] |
| Cynara syriaca Boiss | Disc diffusion method | Gram positive Streptococcus pyogenes Staphylococcus aureus Gram negative Pseudomonas aeruginosa Escherichia coli | Chrysoeriol, among other flavonoids, showed an inhibitory zone <12 mm. The leaf extract showed the maximum effectiveness against c. albicans, with a minimum inhibitory concentration (MIC) value of 250 g mL−1 and an inhibition zone width of 12.5 ± 0.7 mm inhibition zone diameter and 250 µg mL−1 MIC value. | [30] |
| Salvia palaestina | Disc diffusion method | Gram positive Staphylococcus aureus, Staphylococcus epidermidis Gram negative Escherichia coli Klebsiella pneumoniae Proteus vulgaris Pseudomonas aeruginosa | Chrysoeriol was isolated (18 mg from 500 g of dried leaves) but not tested on the cited bacterial stains. | [35] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aboulaghras, S.; Sahib, N.; Bakrim, S.; Benali, T.; Charfi, S.; Guaouguaou, F.-E.; Omari, N.E.; Gallo, M.; Montesano, D.; Zengin, G.; et al. Health Benefits and Pharmacological Aspects of Chrysoeriol. Pharmaceuticals 2022, 15, 973. https://doi.org/10.3390/ph15080973
Aboulaghras S, Sahib N, Bakrim S, Benali T, Charfi S, Guaouguaou F-E, Omari NE, Gallo M, Montesano D, Zengin G, et al. Health Benefits and Pharmacological Aspects of Chrysoeriol. Pharmaceuticals. 2022; 15(8):973. https://doi.org/10.3390/ph15080973
Chicago/Turabian StyleAboulaghras, Sara, Nargis Sahib, Saad Bakrim, Taoufiq Benali, Saoulajan Charfi, Fatima-Ezzahrae Guaouguaou, Nasreddine El Omari, Monica Gallo, Domenico Montesano, Gokhan Zengin, and et al. 2022. "Health Benefits and Pharmacological Aspects of Chrysoeriol" Pharmaceuticals 15, no. 8: 973. https://doi.org/10.3390/ph15080973
APA StyleAboulaghras, S., Sahib, N., Bakrim, S., Benali, T., Charfi, S., Guaouguaou, F. -E., Omari, N. E., Gallo, M., Montesano, D., Zengin, G., Taghzouti, K., & Bouyahya, A. (2022). Health Benefits and Pharmacological Aspects of Chrysoeriol. Pharmaceuticals, 15(8), 973. https://doi.org/10.3390/ph15080973