Uncommon Septic Arthritis of the Hip Joint in an Immunocompetent Adult Patient Due to Bacillus pumilus and Paenibacillus barengoltzii Managed with Long-Term Treatment with Linezolid: A Case Report and Short Literature Review
Abstract
:1. Introduction
2. Case Report
3. Discussion
3.1. Epidemiological and Clinical Considerations
3.2. Short Overview of Published Case Reports on Bacillus pumilus
3.3. Capabilities of Biofilm Formation
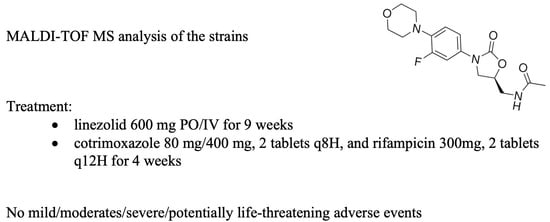
3.4. Long-Term Treatment with Linezolid
3.5. Limitations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ash, C.; Priest, F.G.; Collins, M.D. Molecular identification of rRNA group 3 bacilli (Ash, Farrow, Wallbanks and Collins) using a PCR probe test. Proposal for the creation of a new genus Paenibacillus. Antonie Van Leeuwenhoek 1993, 64, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.L. Control of bacterial spores. Br. Med. Bull. 2000, 56, 158–171. [Google Scholar] [CrossRef] [PubMed]
- Celandroni, F.; Salvetti, S.; Gueye, S.A.; Mazzantini, D.; Lupetti, A.; Senesi, S.; Ghelardi, E. Identification and Pathogenic Potential of Clinical Bacillus and Paenibacillus Isolates. PLoS ONE 2016, 11, e0152831. [Google Scholar] [CrossRef] [PubMed]
- Abrishami, M.; Hashemi, B.; Abrishami, M.; Abnous, K.; Razavi-Azarkhiavi, K.; Behravan, J. PCR detection and identification of bacterial contaminants in ocular samples from postoperative endophthalmitis. J. Clin. Diagn. Res. 2015, 9, NC01–NC03. [Google Scholar] [CrossRef] [PubMed]
- Ferrand, J.; Hadou, T.; Selton-Suty, C.; Goehringer, F.; Sadoul, N.; Alauzet, C.; Lozniewski, A. Cardiac device-related endocarditis caused by Paenibacillus glucanolyticus. J. Clin. Microbiol. 2013, 51, 3439–3442. [Google Scholar] [CrossRef] [PubMed]
- Idelevich, E.A.; Pogoda, C.A.; Ballhausen, B.; Wüllenweber, J.; Eckardt, L.; Baumgartner, H.; Waltenberger, J.; Peters, G.; Becker, K. Pacemaker lead infection and related bacteraemia caused by normal and small colony variant phenotypes of Bacillus licheniformis. J. Med. Microbiol. 2013, 62 Pt 6, 940–944. [Google Scholar] [CrossRef] [PubMed]
- Jeon, Y.L.; Yang, J.J.; Kim, M.J.; Lim, G.; Cho, S.Y.; Park, T.S.; Suh, J.-T.; Park, Y.H.; Lee, M.S.; Kim, S.C.; et al. Combined Bacillus licheniformis and Bacillus subtilis infection in a patient with esophageal perforation. J. Med. Microbiol. 2012, 61 Pt 12, 1766–1769. [Google Scholar] [CrossRef]
- Kimouli, M.; Vrioni, G.; Papadopoulou, M.; Koumaki, V.; Petropoulou, D.; Gounaris, A.; Friedrich, A.W.; Tsakris, A. Two cases of severe sepsis caused by Bacillus pumilus in neonatal infants. J. Med. Microbiol. 2012, 61 Pt 4, 596–599. [Google Scholar] [CrossRef]
- Padhi, S.; Dash, M.; Sahu, R.; Panda, P. Urinary tract infection due to Paenibacillus alvei in a chronic kidney disease: A rare case report. J. Lab. Phys. 2013, 5, 133–135. [Google Scholar] [CrossRef]
- Rieg, S.; Martin Bauer, T.; Peyerl-Hoffmann, G.; Held, J.; Ritter, W.; Wagner, D.; Kern, W.V.; Serr, A. Paenibacillus larvae bacteremia in injection drug users. Emerg. Infect. Dis. 2010, 16, 487–489. [Google Scholar] [CrossRef]
- Sahu, C.; Kumar, K.; Sinha, M.K.; Venkata, A.; Majji, A.B.; Jalali, S. Review of endogenous endophthalmitis during pregnancy including case series. Int. Ophthalmol. 2013, 33, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Tourasse, N.J.; Helgason, E.; Klevan, A.; Sylvestre, P.; Moya, M.; Haustant, M.; Økstad, O.A.; Fouet, A.; Mock, M.; Kolstø, A.-B. Extended and global phylogenetic view of the Bacillus cereus group population by combination of MLST, AFLP, and MLEE genotyping data. Food Microbiol. 2011, 28, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Rasko, D.A.; Altherr, M.R.; Han, C.S.; Ravel, J. Genomics of the Bacillus cereus group of organisms. FEMS Microbiol. Rev. 2005, 29, 303–329. [Google Scholar]
- Keller, P.M.; Rampini, S.K.; Büchler, A.C.; Eich, G.; Wanner, R.M.; Speck, R.F.; Böttger, E.C.; Bloemberg, G.V. Recognition of potentially novel human disease-associated pathogens by implementation of systematic 16S rRNA gene sequencing in the diagnostic laboratory. J. Clin. Microbiol. 2010, 48, 3397–3402. [Google Scholar] [CrossRef] [PubMed]
- Hua, K.; Yang, X.; Feng, J.; Wang, F.; Yang, L.; Zhang, H.; Hu, Y.-C. The efficacy and safety of core decompression for the treatment of femoral head necrosis: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2019, 14, 306. [Google Scholar] [CrossRef]
- Ravn, C.; Neyt, J.; Benito, N.; Abreu, M.A.; Achermann, Y.; Bozhkova, S.; Coorevits, L.; Ferrari, M.C.; Gammelsrud, K.W.; Gerlach, U.-J.; et al. Guideline for management of septic arthritis in native joints (SANJO). J. Bone Jt. Infect. 2023, 8, 29–37. [Google Scholar] [CrossRef]
- Clemett, D.; Markham, A. Linezolid. Drugs 2000, 59, 815–827. [Google Scholar] [CrossRef]
- Fusini, F.; Colò, G.; Massè, A.; Girardo, M. Uncommon cervical pain due by Bacillus pumilus spondylodiscitis in an immunocompetent patient: A case report. Acta Biomed. 2021, 92 (Suppl. S1), e2021136. [Google Scholar] [CrossRef]
- de Salazar, A.; Ferrer, F.; Vinuesa, D.; Chueca, N.; de Luis-Perez, C.; García, F. Unusual case report of skin infection by Paenibacillus timonensis. Rev. Esp. Quimioter. 2020, 33, 139–140. [Google Scholar] [CrossRef]
- Balato, G.; de Matteo, V.; Ascione, T.; de Giovanni, R.; Marano, E.; Rizzo, M.; Mariconda, M. Management of septic arthritis of the hip joint in adults. A systematic review of the literature. BMC Musculoskelet. Disord. 2021, 22 (Suppl. S2), 1006. [Google Scholar] [CrossRef]
- Jeßberger, N.; Krey, V.M.; Rademacher, C.; Böhm, M.E.; Mohr, A.-K.; Ehling-Schulz, M.; Scherer, S.; Märtlbauer, E. From genome to toxicity: A combinatory approach highlights the complexity of enterotoxin production in Bacillus cereus. Front. Microbiol. 2015, 6, 560. [Google Scholar] [CrossRef]
- Borsa, B.A.; Aldağ, M.E.; Tunalı, B.; Dinç, U.; Güngördü Dalar, Z.; Özalp, V.C. A sepsis case caused by a rare opportunistic pathogen: Bacillus pumilus. Mikrobiyol. Bul. 2016, 50, 466–470. [Google Scholar] [CrossRef] [PubMed]
- Farhat, H.; Chachaty, E.; Antoun, S.; Nitenberg, G.; Zahar, J.-R. Infections à Bacillus et immunodépression, à propos de deux cas. Méd. Mal. Infect. 2008, 38, 612–614. [Google Scholar] [CrossRef] [PubMed]
- McKillip, J.L. Prevalence and expression of enterotoxins in Bacillus cereus and other Bacillus spp., a literature review. Antonie Van Leeuwenhoek 2000, 77, 393–399. [Google Scholar] [CrossRef]
- Tena, D.; Martinez-Torres, J.A.; Perez-Pomata, M.T.; Saez-Nieto, J.A.; Rubio, V.; Bisquert, J. Cutaneous Infection Due to Bacillus pumilus: Report of 3 Cases. Clin. Infect. Dis. 2007, 44, e40–e42. [Google Scholar] [CrossRef] [PubMed]
- Grady, E.N.; MacDonald, J.; Liu, L.; Richman, A.; Yuan, Z.C. Current knowledge and perspectives of Paenibacillus: A review. Microb. Cell Fact. 2016, 15, 203. [Google Scholar] [CrossRef]
- Reboli, A.C.; Bryan, C.S.; Farrar, W.E. Bacteremia and infection of a hip prosthesis caused by Bacillus alvei. J. Clin. Microbiol. 1989, 27, 1395–1396. [Google Scholar] [CrossRef]
- DeLeon, S.D.; Welliver, R.C. Sr Paenibacillus alvei sepsis in a neonate. Pediatr. Infect. Dis. J. 2016, 35, 358. [Google Scholar] [CrossRef]
- Roux, V.; Fenner, L.; Raoult, D. Paenibacillus provencensis sp. nov., isolated from human cerebrospinal fluid, and Paenibacillus urinalis sp. nov., isolated from human urine. Int. J. Syst. Evol. Microbiol. 2008, 58, 682–687. [Google Scholar] [CrossRef]
- Bosshard, P.P.; Zbinden, R.; Altwegg, M. Paenibacillus turicensis sp. nov., a novel bacterium harbouring heterogeneities between 16S rRNA genes. Int. J. Syst. Evol. Microbiol. 2002, 52, 2241–2249. [Google Scholar]
- Roux, V.; Raoult, D. Paenibacillus massiliensis sp. nov. Paenibacillus sanguinis sp. nov. and Paenibacillus timonensis sp. nov., isolated from blood cultures. Int. J. Syst. Evol. Microbiol. 2004, 54, 1049–1054. [Google Scholar] [CrossRef] [PubMed]
- Birlutiu, R.M.; Roman, M.D.; Cismasiu, R.S.; Fleaca, S.R.; Popa, C.M.; Mihalache, M.; Birlutiu, V. Sonication contribution to identifying prosthetic joint infection with Ralstonia pickettii: A case report and review of the literature. BMC Musculoskelet. Disord. 2017, 18, 311. [Google Scholar] [CrossRef]
- Birlutiu, R.M.; Stoica, C.I.; Russu, O.; Cismasiu, R.S.; Birlutiu, V. Positivity Trends of Bacterial Cultures from Cases of Acute and Chronic Periprosthetic Joint Infections. J. Clin. Med. 2022, 11, 2238. [Google Scholar] [CrossRef] [PubMed]
- Roman, M.D.; Bocea, B.A.; Ion, N.I.; Vorovenci, A.E.; Dragomirescu, D.; Birlutiu, R.M.; Birlutiu, V.; Fleaca, S.R. Are There Any Changes in the Causative Microorganisms Isolated in the Last Years from Hip and Knee Periprosthetic Joint Infections? Antimicrobial Susceptibility Test Results Analysis. Microorganisms 2023, 11, 116. [Google Scholar] [CrossRef]
- Birlutiu, R.M.; Birlutiu, V.; Cismasiu, R.S.; Mihalache, M. bbFISH-ing in the sonication fluid. Medicine 2019, 98, e16501. [Google Scholar] [CrossRef] [PubMed]
- Birlutiu, R.M.; Mihalache, M.; Mihalache, P.; Cismasiu, R.S.; Birlutiu, V. Mid-term follow-up results after implementing a new strategy for the diagnosis and management of periprosthetic joint infections. BMC Infect. Dis. 2021, 21, 807. [Google Scholar] [CrossRef]
- Rondaan, C.; Maso, A.; Birlutiu, R.M.; Fernandez Sampedro, M.; Soriano, A.; Diaz de Brito, V.; Gómez Junyent, J.; Del Toro, M.D.; Hofstaetter, J.G.; Salles, M.J.; et al. Is an isolated positive sonication fluid culture in revision arthroplasties clinically relevant? Clin. Microbiol. Infect. 2023. [Google Scholar] [CrossRef]
- Nguyen, S.; Pasquet, A.; Legout, L.; Beltrand, E.; Dubreuil, L.; Migaud, H.; Yazdanpanah, Y.; Senneville, E. Efficacy and tolerance of rifampicin-linezolid compared with rifampicin-cotrimoxazole combinations in prolonged oral therapy for bone and joint infections. Clin. Microbiol. Infect. 2009, 15, 1163–1169. [Google Scholar] [CrossRef]
- Theil, C.; Schmidt-Braekling, T.; Gosheger, G.; Schwarze, J.; Dieckmann, R.; Schneider, K.N.; Möllenbeck, B. Clinical use of linezolid in periprosthetic joint infections—A systematic review. J. Bone Jt. Infect. 2020, 6, 7–16. [Google Scholar] [CrossRef]
- Soriano, A.; Gómez, J.; Gómez, L.; Azanza, J.; Pérez, R.; Romero, F.; Pons, M.; Bella, F.; Velasco, M.; Mensa, J. Efficacy and tolerability of prolonged linezolid therapy in the treatment of orthopedic implant infections. Eur. J. Clin. Microbiol. Infect. Dis. 2007, 26, 353–356. [Google Scholar] [CrossRef]
- Schwameis, R.; Syré, S.; Sarahrudi, K.; Appelt, A.; Marhofer, D.; Burau, D.; Kloft, C.; Zeitlinger, M. Penetration of linezolid into synovial fluid and muscle tissue after elective arthroscopy. J. Antimicrob. Chemother. 2017, 72, 2817–2822. [Google Scholar] [CrossRef] [PubMed]
- Vintila, B.I.; Arseniu, A.M.; Butuca, A.; Sava, M.; Bîrluțiu, V.; Rus, L.L.; Axente, D.D.; Morgovan, C.; Gligor, F.G. Adverse Drug Reactions Relevant to Drug Resistance and Ineffectiveness Associated with Meropenem, Linezolid, and Colistin: An Analysis Based on Spontaneous Reports from the European Pharmacovigilance Database. Antibiotics 2023, 12, 918. [Google Scholar] [CrossRef] [PubMed]
- Vintila, B.I.; Arseniu, A.M.; Morgovan, C.; Butuca, A.; Sava, M.; Bîrluțiu, V.; Rus, L.L.; Ghibu, S.; Bereanu, A.S.; Roxana Codru, I.; et al. A Pharmacovigilance Study Regarding the Risk of Antibiotic-Associated Clostridioides difficile Infection Based on Reports from the EudraVigilance Database: Analysis of Some of the Most Used Antibiotics in Intensive Care Units. Pharmaceuticals 2023, 16, 1585. [Google Scholar] [CrossRef] [PubMed]


| Date | Parameter | Values | Reference Value |
|---|---|---|---|
| On admission | C-reactive protein | 2.0 mg/L | 0–0.3 mg/L |
| Fibrinogen | 382 mg/dL | 180–350 mg/dL | |
| WBCs | 9.93 × 103/µL | 4–9 × 103/µL | |
| Differential blood count: | |||
| Neutrophils | 6.86 × 103/µL | 1.5–7.5 × 103/µL | |
| Lymphocytes | 2.22 × 103/µL | 1.2–3.5 × 103/µL | |
| Monocytes | 0.59 × 103/µL | 0.2–0.8 × 103/µL | |
| Basophils | 0.03 × 103/µL | 0.01–0.15 × 103/µL | |
| Eosinophils | 0.12 × 103/µL | 0.02–0.06 × 103/µL | |
| Red blood cells | 5.56 × 106/µL | 4.6–6.2 × 106/µL | |
| Hemoglobin | 16.1 g/dL | 14–18 g/dL | |
| Hematocrit | 47.2% | 40–52% | |
| Thrombocytes | 304 × 103/µL | 150–450 × 103/µL | |
| Coagulation tests | Prothrombin time (PT): 10.8 s | 9.8–12.1 s | |
| Activated partial thromboplastin time (aPTT): 22.6 s | 22.1–28.1 s | ||
| International normalized ratio (INR): 1.04 s | 0.86–1.2 s | ||
| ESR | 24 mm/h | 0–15 mm/h | |
| Urea | 28 mg/dL | 15–39 mg/dL | |
| Creatinine | 0.89 mg/dL | 0.7–1.3 mg/dL | |
| Blood glucose | 104 mg/dL | 74–106 mg/dL | |
| Urine culture | Negative < 1000 CFU/mL | ||
| Alanine transaminase | 38 U/L | 16–63 U/L | |
| Aspartate transferase | 117 U/L | 15–37 U/L |
| Antibiotic | MIC (μg/mL) | MIC Interpretation |
|---|---|---|
| Bacillus pumilus—beta-lactamases, ESBL-producing, carbapenemase, mannose-binding lectin, inducible resistance to clindamycin (negative) | ||
| Ciprofloxacin | =0.5 | Intermediate |
| Erythromycin | =1 | Resistant |
| Levofloxacin | ≤1 | Intermediate |
| Linezolid | ≤1 | Sensitive |
| Meropenem | ≤0.25 | Sensitive |
| Vancomycin | ≤1 | Sensitive |
| Paenibacillus barengoltzii—beta-lactamases, ESBL-producing, carbapenemase, mannose-binding lectin, inducible resistance to clindamycin (negative) | ||
| Ciprofloxacin | =0.5 | Intermediate |
| Erythromycin | =0.5 | Sensitive |
| Levofloxacin | ≤1 | Intermediate |
| Linezolid | ≤1 | Sensitive |
| Meropenem | ≤0.5 | Sensitive |
| Vancomycin | ≤1 | Sensitive |
| Date | Parameter | Values | Reference Value |
|---|---|---|---|
| Day 1 after surgery | C-reactive protein | - | 0–0.3 mg/L |
| Fibrinogen | 438 mg/dL | 180–350 mg/dL | |
| WBCs | 11.13 × 103/µL | 4–9 × 103/µL | |
| Red blood cells | 4.32 × 106/µL | 4.6–6.2 × 106/µL | |
| Hemoglobin | 12.5 g/dL | 14–18 g/dL | |
| Hematocrit | 36.5% | 40–52% | |
| Thrombocytes | 356 × 103/µL | 150–450 × 103/µL | |
| ESR | - | 0–15 mm/h | |
| Urea | 22 mg/dL | 15–39 mg/dL | |
| Creatinine | 0.8 mg/dL | 0.7–1.3 mg/dL | |
| Blood glucose | 134 mg/dL | 74–106 mg/dL | |
| Alanine transaminase | 81 U/L | 16–63 U/L | |
| Aspartate transferase | 51 U/L | 15–37 U/L | |
| Day 3 after surgery | C-reactive protein | 3.7 mg/L | 0–0.3 mg/L |
| Fibrinogen | 586 mg/dL | 180–350 mg/dL | |
| WBCs | 11.09 × 103/µL | 4–9 × 103/µL | |
| Red blood cells | 4.61 × 106/µL | 4.6–6.2 × 106/µL | |
| Hemoglobin | 13.2 g/dL | 14–18 g/dL | |
| Hematocrit | 40.0% | 40–52% | |
| Thrombocytes | 342 × 103/µL | 150–450 × 103/µL | |
| ESR | 50 mm/h | 0–15 mm/h | |
| Urea | 37 mg/dL | 15–39 mg/dL | |
| Creatinine | 0.81 mg/dL | 0.7–1.3 mg/dL | |
| Blood glucose | 99 mg/dL | 74–106 mg/dL | |
| Alanine transaminase | 86 U/L | 16–63 U/L | |
| Aspartate transferase | 53 U/L | 15–37 U/L | |
| At the time of discharge | C-reactive protein | 1.2 mg/L | 0–0.3 mg/L |
| Fibrinogen | 367 mg/dL | 180–350 mg/dL | |
| WBCs | 6.1 × 103/µL | 4–9 × 103/µL | |
| Red blood cells | 4.78 × 106/µL | 4.6–6.2 × 106/µL | |
| Hemoglobin | 14.2 g/dL | 14–18 g/dL | |
| Hematocrit | 42.3% | 40–52% | |
| Thrombocytes | 342 × 103/µL | 150–450 × 103/µL | |
| ESR | 24 mm/h | 0–15 mm/h | |
| Urea | 33 mg/dL | 15–39 mg/dL | |
| Creatinine | 0.83 mg/dL | 0.7–1.3 mg/dL | |
| Blood glucose | 102 mg/dL | 74–106 mg/dL | |
| Alanine transaminase | 233 U/L | 16–63 U/L | |
| Aspartate transferase | 86 U/L | 15–37 U/L |
| Author | Isolated Strain | Type of Infection | Antibiotic Susceptibility Test Results | Treatment |
|---|---|---|---|---|
| Fusini et al. [18] | Bacillus pumilus | C6–C7 intervertebral disc spondylodiscitis | Susceptible to ampicillin, amoxicillin, ciprofloxacin, clindamycin, erythromycin, imipenem, levofloxacin, teicoplanin, trimethoprim–sulfamethoxazole, and vancomycin | 6 weeks IV amoxicillin/clavulanic acid 2.2 g q8H plus ciprofloxacin 400 mg q12H, then oral therapy for 6 weeks with amoxicillin/clavulanic acid 875/125 mg q8H plus ciprofloxacin 500 mg q12H |
| Borsa et al. [22] | Bacillus pumilus | Sepsis | Resistant to penicillin Susceptible to vancomycin, erythromycin, clindamycin, levofloxacin, and trimethoprim–sulfamethoxazole | IV ceftriaxone (1000 mg q12H) in association with metronidazole (500 mg q12H for 7 days followed by IV ceftriaxone (1000 mg q12H) for 14 days |
| Kimouli et al. [8] | Bacillus pumilus (2 strains) | Neonatal sepsis | Susceptible to penicillin, ampicillin, imipenem, vancomycin, erythromycin, levofloxacin, and trimethoprim–sulfamethoxazole and just one strain was susceptible to clindamycin | Vancomycin for 10 days |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cismasiu, R.S.; Birlutiu, R.-M.; Preoțescu, L.L. Uncommon Septic Arthritis of the Hip Joint in an Immunocompetent Adult Patient Due to Bacillus pumilus and Paenibacillus barengoltzii Managed with Long-Term Treatment with Linezolid: A Case Report and Short Literature Review. Pharmaceuticals 2023, 16, 1743. https://doi.org/10.3390/ph16121743
Cismasiu RS, Birlutiu R-M, Preoțescu LL. Uncommon Septic Arthritis of the Hip Joint in an Immunocompetent Adult Patient Due to Bacillus pumilus and Paenibacillus barengoltzii Managed with Long-Term Treatment with Linezolid: A Case Report and Short Literature Review. Pharmaceuticals. 2023; 16(12):1743. https://doi.org/10.3390/ph16121743
Chicago/Turabian StyleCismasiu, Razvan Silviu, Rares-Mircea Birlutiu, and Liliana Lucia Preoțescu. 2023. "Uncommon Septic Arthritis of the Hip Joint in an Immunocompetent Adult Patient Due to Bacillus pumilus and Paenibacillus barengoltzii Managed with Long-Term Treatment with Linezolid: A Case Report and Short Literature Review" Pharmaceuticals 16, no. 12: 1743. https://doi.org/10.3390/ph16121743
APA StyleCismasiu, R. S., Birlutiu, R. -M., & Preoțescu, L. L. (2023). Uncommon Septic Arthritis of the Hip Joint in an Immunocompetent Adult Patient Due to Bacillus pumilus and Paenibacillus barengoltzii Managed with Long-Term Treatment with Linezolid: A Case Report and Short Literature Review. Pharmaceuticals, 16(12), 1743. https://doi.org/10.3390/ph16121743