Parenteral Ready-to-Use Fixed-Dose Combinations Including NSAIDs with Paracetamol or Metamizole for Multimodal Analgesia—Approved Products and Challenges
Abstract
:1. Introduction
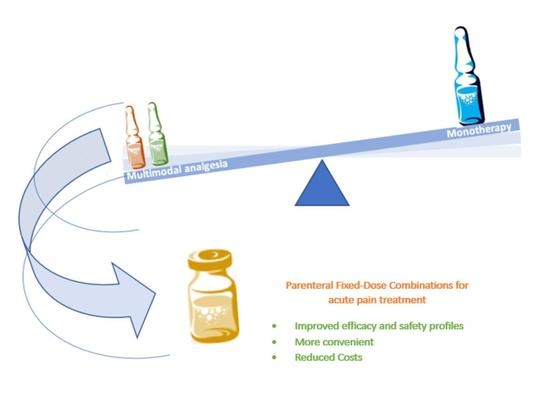
2. Multimodal and Parenteral Analgesia
2.1. Multimodal Analgesia
2.2. Parenteral Analgesia
2.2.1. Paracetamol-Based Parenteral Formulations
2.2.2. Metamizole-Based Parenteral Formulations
2.2.3. NSAID-Based Parenteral Formulations
| NSAID | Formulations | Route of Administration | Indications | Brands a | Countries with Marketing Authorization d |
|---|---|---|---|---|---|
| Ibuprofen | 800 mg/8 mL 800 mg/200 mL | IV | Management of mild-to-moderate pain and moderate-to-severe pain in adults. Also, it is indicated for the reduction of fever in adults [72]. | Caldolor® | US |
| Ketorolac | 15 mg/1 mL 30 mg/1 mL | IV/IM | Short-term management of moderate-to-severe acute pain, including pain following operative procedures [73]. | Toradol® b | US |
| Acetylsalicylate | 500 mg/5 mL (freeze-dried) | IM/IV | Symptomatic treatment of pain in rheumatology, traumatology, oncology, surgery and anaesthesiology, post-operatively, and in preparation for exams. Also used in the symptomatic treatment of fever [74]. | Aspegic® | BE, HU, and PT |
| Dexketoprofen | 50 mg/2 mL 25 mg/2 mL | IM/IV | Symptomatic treatment of acute pain of moderate-to-severe intensity when oral administration is not appropriate, such as post-operative pain, renal colic, and lower back pain [75,76]. | Ketesse® Keral® Auxilen® Dekenor® Morsadex® | DE, AT, SK, SI, ES, EE, FI, FR, GR, NL, HU, IE, LV, LT, MT, PL, CZ, and RW |
| 50 mg/100 mL | IV | Dexketoprofen B. Braun® | ES | ||
| Diclofenac | 75 mg/3 mL c 50 mg/1 mL 25 mg/1 mL | IV/IM | IM use is effective in acute forms of pain, including renal colic, exacerbations of osteo- and rheumatoid arthritis, acute back pain, acute gout, acute trauma and fractures, and post-operative pain. In IV use, it is indicated for the treatment or prevention of post-operative pain in the hospital setting [77]. | Voltaren® Voltarol® Fenil-V® Akis® plus Dicloin® Diclac® Almiral® | DE, AT, BE, BG, SK, SI, ES, EE, FR, FI, GR, NL, HU, IE, IT, LV, LT, MT, PL, PT, GB, CZ, RW, and SE |
| Etofenamate | 1000 mg/2 mL | IM | Indicated in painful and acute inflammatory situations in rheumatology, traumatology, and post-operatively [78]. | Rheumon® Traumon® | DE, AT, GR, HU, PT, and RW |
| Ibuprofen | 600 mg/100 mL c 400 mg/100 mL 200 mg/50 mL | IV | Indicated in adults for the short-term symptomatic treatment of acute moderate pain and fever. IV route is clinically justified when other routes of administration are not possible [79]. | Ibuprofen B. Braun® Solibu® | DE, AT, BE, BG, DK, SK, SI, ES, EE, FI, NL, HU, IE, LV, LT, PL, PT, GB, CZ, RW, and SE |
| Indomethacin | 50 mg/2 mL 25 mg/2 mL (freeze-dried) | IV | Indicated to reduce (acute) pain due to inflammation of the muscles and muscle joints (musculoskeletal system) [80]. | Liometacen® | IT |
| Ketoprofen | 100 mg/2 mL c | IM | Indicated for rheumatoid arthritis, osteoarthritis ankylosing spondylitis, and acute episodes of gout. The injectable form is especially indicated for the treatment of acute attacks with a predominance of pain [81]. | Profenid® Rofenid® Ketonal® Orudis® | BE, SK, SI, ES, FR, IT, LV, LT, PL, PT, CZ, and RW |
| Ketorolac | 50 mg/5 mL 30 mg/1 mL c 10 mg/1 mL | IM/IV | It is indicated for the short-term management of moderate-to-severe acute post-operative pain. Treatment should only be initiated in hospitals. The maximum duration of treatment is two days [82]. | Toradol® Taradyl® | BE, DK, ES, EE, FI, GR, IS, IT, LV, LT, PT, GB, RW, and SE |
| Lornoxicam | 8 mg/2 mL (freeze-dried) | IM/IV | Short-term relief of acute mild-to-moderate pain [83]. | Xefo® | SK, GR, HU, and RW |
| Meloxicam | 15 mg/1.5 mL | IM | Short-term treatment of symptomatic acute exacerbations of rheumatoid arthritis and ankylosing spondylitis when other routes of administration are not appropriate [68]. | Movalis® Melox® Mobic® | SK, EE, FR, GR, HU, IT, LV, LT, MT, PL, PT, and RW |
| Piroxicam | 20 mg/1 mL | IM | Symptomatic relief of osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis [67]. | Feldene® Flexase® | DE, BE, ES, FR, HU, PL, and PT |
| Tenoxicam | 20 mg/3 mL c (freeze-dried) | IM/IV | Indicated for patients considered unable to take oral tenoxicam for the relief of pain and inflammation in osteoarthritis and rheumatoid arthritis and for the short-term management of acute musculoskeletal disorders including strains, sprains, and other soft-tissue injuries [84]. | Neo-Indusix® | GR, GB, and RW |
3. Parenteral Fixed-Dose Combinations
3.1. Paracetamol-Based Parenteral Fixed-Dose Combinations
3.2. Metamizole-Based Parenteral Fixed-Dose Combinations
| Combination | Strengths | Route of Administration | Indications | Brands a | Countries with Marketing Authorization b |
|---|---|---|---|---|---|
| Paracetamol + Ibuprofen | 1000 mg + 300 mg/ 100 mL | IV | Short-term symptomatic treatment of moderate acute pain in adults when intravenous administration is considered clinically necessary and/or when other routes of administration are not possible [113]. | Combofusiv® Comboval® Combogesic® | AT, CZ, DE, EE, IE, HR, HU, LT, MT, NL, PT, SI, SE, and UK |
| Metamizole + Scopolamine (or Butylscopolamine) | 2500 mg + 20 mg/5 mL | IM/IV | Post-surgical pain, post-trauma pain, or colicky pain [114]. | Buscapina® compositum | AR, BR, CL, ES, and MX |
| Metamizole + Pitofenone | 2500 mg + 10 mg/5 mL | IM/IV | Treatment of painful conditions in the digestive tract and in the bile and urinary tract [115]. | Litalgin® | FI |
| Metamizole + Pitofenone + Fenpiverinium | 2500 mg + 10 mg + 0.1 mg/5 mL | IM/IV | Treatment of painful conditions in the digestive tract and in the bile and urinary tract and dysmenorrhea [116]. | Analgin® Spasmalgon® | CZ, LV, and PL |
| Metamizole + Adiphenine + Promethazine | 750 mg + 25 mg + 25 mg/2 mL | IM | General painful conditions [117]. | Dorilen® | BR |
| Metamizole + Hydroxocobalamin + Dexamethasone | 500 mg + 5 mg + 2 mg/1 mL | IM | Acute joint inflammation processes such as arthritis, periarthritis, bursitis, gout, ankylosing, and spondylitis; in degenerative processes that go along with pain, such as arthrosis and intervertebral disc disorders; in neuralgia; and in back and neck pain [118]. | Dexalgen® | BR |
| Metamizole + Pargeverine | 2000 mg + 5 mg/4 mL | IV | Treatment of all acute pain accompanied by muscle spasms in any portion of the digestive, hepatobiliary, or urinary tracts or the female genitals [119]. | Viadil® Compuesto | CL |
| Metamizole + Ampicillin + Guaifenesin + Lidocaine + Chlorphenamine | 500 mg + 500 mg + 100 mg + 30 mg + 4 mg/3 mL | IM | Unknown c | Ampigrin® | MX |
| Metamizole + Procaine Penicillin G | 400,000 U.I. + 500 mg/5 mL | IM | Unknown c | Respicil® | MX |
| Metamizole + Chlorphenamine | Unknown c | Unknown c | Unknown c | Singril® iny | MX |
3.3. Other NSAID-Based Combinations
- Justification and rationale for the combination.
- Demonstration of the contribution of all active substances to the desired therapeutic effect.
- The relevance of the evidence presented to the fixed-combination medicinal product.
| Author, Year | Trial Design (N) | Pain Model | Study Objectives | Treatment Details (Drug; Dosage; Regimen; Route; Frequency; Duration) | Primary Outcomes | Conclusions |
|---|---|---|---|---|---|---|
| Metamizole Combinations | ||||||
| Ibuprofen + Metamizole | ||||||
| Schneider et al., 2022 [112] | Randomized, crossover, double-blind, and controlled trial (35) | Lower third molar extraction | To compare the combination of ibuprofen/metamizole with either drug alone in relieving postoperative pain. | 1. MTZ 1000 mg 2. IBP 400 mg 3. MTZ 1000 mg + IBP Each patient received three applications and was assessed for 18 h. | Mean pain score | Efficacy: Combined use enables superior pain control compared to ibuprofen alone and tends to be superior to metamizole alone. Safety: Not addressed by the authors. |
| Paracetamol (or Propacetamol) Combinations | ||||||
| Diclofenac + Paracetamol (or Propacetamol) | ||||||
| Montgomery et al., 1996 [122] | Randomized, parallel, open-label, and controlled trial (60) | Elective abdominal gynecological surgery | Assess the analgesic efficacy of paracetamol alone and in combination with diclofenac. | 1. DCF 100 mg 2. APAP 1500 mg 3. DCF 100 mg + APAP 1500 mg Single rectal dose was given before the surgery with 24 h of observation. |
| Efficacy: Combination reduced the amount of morphine consumed. Safety: No difference in the incidence of side effects between the groups. |
| Breivik et al., 1999 [133] | Randomized, parallel, double-blind, and controlled trial (120) | Surgical removal of third molars | Assess the analgesic effect of combining diclofenac with paracetamol and with codeine. | 1. DCF 100 mg 2. APAP 1000 mg 3. DCF 100 mg + APAP 1000 mg 4. DCF 100 mg + APAP 1000 mg + CDN 60 mg 5. APAP 100 mg + CDN 60 mg Single oral dose was given after the surgery with 8 h of observation. |
| Efficacy: Combination of drugs is superior to diclofenac or paracetamol alone. Safety: No difference in the incidence of side effects between the groups. |
| Beck et al., 2000 [134] | Randomized, parallel, double-blind, and controlled trial (70) | Hysterectomy | Assess the pharmacokinetics of rectal paracetamol in women and compare their analgesic efficacy with a diclofenac combination. | 1. APAP 20 mg/kg (small-dose) 2. APAP 40 mg/kg (large-dose) 3. DCF 100 mg + APAP 20 mg/kg Single rectal dose was given before the surgery within 24 h of observation. |
| Efficacy: Only lower VAS scores after APAP + DCF at 4 h. Safety: Not addressed by the authors. |
| Siddik et al., 2001 [135] | Randomized, parallel, double-blind, and controlled trial (80) | Cesarean | Assess the postoperative analgesic effects of propacetamol in combination with diclofenac. | 1. Placebo 2. DCF 100 mg 3. PPCM 2 g 4. DCF 100 mg + PPCM 2 g Propacetamol intravenously q.i.d and diclofenac rectally t.i.d over 24 h following surgery. |
| Efficacy: No statistical difference between the groups. Safety: No difference in the incidence of side effects between the groups. |
| Man et al., 2004 [136] | Randomized, parallel, double-blind, and controlled trial (50) | Painful soft-tissue injuries | Asses the efficacy and safety of oral paracetamol compared with NSAIDs or combination therapy. | 1. DCF 25 mg 2. APAP 1000 mg 3. DCF 25 mg + APAP 1000 mg 4. IND 25 mg Oral administration of diclofenac t.i.d, paracetamol q.i.d, and indomethacin t.i.d with observation over 120 min (stage 1) and 3 days (stage 2). |
| Efficacy: No statistical difference between the groups. Safety: No difference in the incidence of side effects between the groups. |
| Hiller et al., 2004 [137] | Randomized, parallel, double-blind, and controlled trial (71) | Elective tonsillectomy | Assess the analgesic efficacy between the combination of paracetamol with diclofenac and either drug alone. | 1. DCF 75 mg 2. PPCM 2000 mg 3. DCF 75 mg + PPCM 2000 mg Single IV dose was administered after anesthetic induction and postoperatively; propacetamol was administered twice and diclofenac once. |
| Efficacy: No statistical difference between the groups. Safety: No difference in the incidence of side effects between the groups. |
| Woo et al., 2005 [138] | Randomized, parallel, double-blind, and controlled trial (300) | Musculoskeletal Injury | Assess the efficacy safety of oral paracetamol compared with oral nonsteroidal anti-inflammatory drugs or combination therapy. | 1. DCF 25 mg 2. APAP 1000 mg 3. DCF 25 mg + APAP 1000 mg 4. IND 25 mg Stage 1—single oral dose with 2 h of observation. Stage 2—outside the hospital, the same therapy with 3 days of observation (paracetamol q.i.d and diclofenac or indomethacin t.i.d) | Pain intensity (VAS) at rest and with limb movement | Efficacy: The analgesic benefits of oral combination were small and of doubtful clinical significance. Safety: No difference in the incidence of side effects between the groups. |
| Legeby et al., 2005 [139] | Randomized, parallel, double-blind, and controlled trial (50) | Mastectomy with immediate breast reconstruction | Assess the analgesic efficacy of diclofenac in combination with paracetamol and opioids. | 1. APAP 1000 mg 2. DCF 50 mg + APAP 1000 mg Diclofenac was administered rectally t.i.d and paracetamol was administered orally t.i.d with 64 h of observation. |
| Efficacy: The combination reduced opioid consumption and improved pain relief during the first 20 h. Safety: Post-operative bleeding was significantly higher with diclofenac than with a placebo (p < 0.01). |
| Munishankar et al., 2008 [140] | Randomized, parallel, double-blind, and controlled trial (78) | Elective cesarean section | Assess the efficacy of the combination of diclofenac and paracetamol used for pain relief after major surgery. | 1. DCF 100 mg 2. APAP 1000 mg 3. DCF 100 mg + APAP 1000 mg Study drugs were given as a suppository at the end of surgery and then orally for 24 h. Paracetamol q.i.d and diclofenac t.i.d with 24 h of observation. |
| Efficacy: Patients given a combination of diclofenac and paracetamol used 38% less morphine compared to patients given paracetamol. Safety: Not addressed by the authors. |
| Ridderikhof et al., 2018 [141] | Randomized, multicenter, parallel, double-blind, and controlled trial (547) | Acute musculoskeletal trauma | Assess the efficacy of paracetamol and diclofenac alone or in combination. | 1. DCF 50 mg 2. APAP 1000 mg 3. DCF 50 mg + APAP 1000 mg Diclofenac and paracetamol were administered orally t.i.d and q.i.d, respectively, with 3 days of observation. | Pain intensity (NRS pain score) at rest and with movement | Efficacy: No statistical difference between the groups. Safety: No difference in the incidence of side effects between the groups. |
| Ketoprofen + Paracetamol (or Propacetamol) | ||||||
| Fletcher et al., 1997 [142] | Randomized, parallel, double-blind, and controlled trial (60) | Disc surgery | Assess the effect of combining propacetamol with ketoprofen. | 1. KTPF 50 mg 2. PPCM 2000 mg 3. KTPF 50 mg + PPCM 2000 mg 4. Placebo All drugs were given q.i.d and intravenously for 2 days after the surgery. The observation occurred during the same period. | Pain intensity (VAS score) | Efficacy: The combination reduced pain scores both at rest and on movement. Safety: No difference in the incidence of side effects between the groups. |
| Aubrun et al., 2000 [143] | Randomized, parallel, double-blind, and controlled trial (50) | Spinal fusion surgery | Assess the efficacy of ketoprofen in patients receiving propacetamol. | 1. PPCM 2000 mg 2. KTPF 100 mg + PPCM 2000 mg Ketoprofen and propacetamol were administered intravenously t.i.d and q.i.d, respectively, over 24 h following surgery. The observation occurred during the same period. | Pain intensity (VAS score) | Efficacy: The combination reduced morphine requirements and improved postoperative analgesia. Safety: No difference in the incidence of side effects between the groups. |
| Fourcade et al., 2005 [144] | Randomized, parallel, double-blind, and controlled trial (97) | Thyroidectomy | Compare the efficacy of propacetamol and ketoprofen, alone or in combination. | 1. KTPF 100 mg 2. PPCM 2000 mg 3. KTPF 100 mg + PPCM 2000 mg Propacetamol and Ketoprofen were administered intravenously 30 min before the end of surgery and 6 and 12 h after the surgery. The observation occurred during the same period. | Pain intensity (VAS score) | Efficacy: No statistical difference between the groups. Safety: Not addressed by the authors. |
| Akural et al., 2009 [145] | Randomized, parallel, double-blind, and controlled trial (76) | Postoperative dental pain | Assess the efficacy of combining paracetamol with ketoprofen. | 1. KTPF 100 mg 2. APAP 1000 mg 3. KTPF 100 mg + APAP 1000 mg 4. Placebo Ketoprofen and paracetamol were administered orally in a single dose. The observation was performed every 15 min for 10 h. | Pain intensity difference (PID), sum of PID (SPID), and NRS score at rest and on dry swallowing | Efficacy: The combination provided a significantly more rapid onset of analgesia than either drug alone. Safety: No difference in the incidence of side effects between the groups. |
| Salonen et al., 2009 [146] | Randomized, parallel, double-blind, and controlled trial (116) | Tonsillectomy | Evaluate the efficacy of co-administration of intravenous paracetamol with ketoprofen. | 1. KTPF 1 mg/kg 2. KTPF 1 mg/kg + APAP 1000 mg 3. KTPF 1 mg/kg + APAP 2000 mg Both ketoprofen and paracetamol were administered intravenously in a single dose after the surgery. | The proportion of patients requiring rescue analgesia | Efficacy: In the combination groups, the number of opioid doses was reduced. Safety: No difference in the incidence of side effects between the groups. |
| Ketorolac + Paracetamol (or Propacetamol) | ||||||
| Romundstad et al., 2006 [123] | Randomized, crossover, double-blind, and controlled trial (16) | Pressure algometry | Evaluate the efficacy of propacetamol 2 g and ketorolac 30 mg, individually and in combination. | 1. KTLC 30 mg 2. PPCM 2000 mg 3. KTLC 30 mg + PPCM 2000 mg 4. Placebo The crossover study had a Latin square design. The drugs were administered intravenously in a single dose and the observation was performed for 165 min. | Pressure pain tolerance threshold (PPTT) | Efficacy: Combining paracetamol with ketorolac increased the PPTT. Safety: No difference in the incidence of side effects between the groups. |
| Iorno et al., 2013 [147] | Randomized, parallel, patient-blinded, and controlled trial (60) | Voluntary ambulatory abortion | Assess the efficacy and safety of oral paracetamol with IV ketorolac. | 1. KTLC 30 mg 2. KTLC 30 mg + APAP 1000 mg Ketorolac was administered intravenously o.d and paracetamol was administered orally t.i.d. The patients were observed until the following morning. | Pain intensity (NRS score) | Efficacy: The studied drugs were effective and well tolerated in the control of postoperative pain. Safety: No difference in the incidence of side effects between the groups. |
| Piroxicam + Paracetamol (or Propacetamol) | ||||||
| Msolli et al., 2021 [124] | Randomized, parallel, single-blinded, and controlled trial (1632) | Traumatic injury | Explore the possible benefits of combining piroxicam with paracetamol. | 1. APAP 1000 mg 2. PRX 20 mg 3. PRX 20 mg + APAP 1000 mg Paracetamol and piroxicam were administered orally t.i.d and b.i.d, respectively. Each patient was re-evaluated on the 3rd and 7th days. | Need for additional oral analgesics | Efficacy: The combination did not increase the analgesic effect compared to paracetamol alone. Safety: The occurrence of adverse events was significantly more frequent in the PRX alone and combination groups. |
3.3.1. Metamizole-Based Combinations with Ibuprofen
3.3.2. Paracetamol-Based Combinations with Diclofenac
3.3.3. Paracetamol-Based Combinations with Ketoprofen
3.3.4. Paracetamol-Based Combinations with Ketorolac
3.3.5. Paracetamol-Based Combinations with Piroxicam
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AAPM | American Academy of Pain Medicine |
| AM404 | N-(4-Hydroxyphenyl) arachidonylamide |
| API | Active pharmaceutical ingredient |
| ASA | American Society of Anaesthesiologists |
| ATP | Adenosine triphosphate |
| b.i.d | Two times a day |
| CB1 | Cannabinoid receptor type 1 |
| CHMP | Committee for Medicinal Products for Human Use |
| CNS | Central nervous system |
| COX | Cyclooxygenase |
| ERAS | Enhanced recovery after surgery |
| FDA | Food and Drugs Administration |
| FDC | Fixed-dose combination |
| IM | Intramuscular |
| IV | Intravenous |
| MSF | Doctors Without Borders |
| NAPQI | N-acetyl-p-benzoquinone imine |
| NMDA | N-Methyl-D-aspartic acid |
| NOA | Non-opioid analgesic |
| NRS | Numeric rating scale |
| NSAID | Non-steroidal anti-inflammatory drug |
| o.d | Once a day |
| OTA | Orthopaedic Trauma Association |
| OTC | Over-the-counter |
| PGE2 | Prostaglandin E2 |
| q.i.d | Four times a day |
| PID | Pain intensity difference |
| PPTT | Pressure pain tolerance threshold |
| SC | Subcutaneous |
| SPC | Summary of product characteristics |
| SPID | Sum of pain intensity difference |
| SSRI | Selective serotonin reuptake inhibitor |
| t.i.d | Three times a day |
| TRPV1 | Transient receptor potential vanilloid type 1 |
| US | United States |
| USA | United States of America |
| VAS | Visual analog scale |
| VRS | Verbal rating scale |
References
- Meissner, W.; Zaslansky, R. A survey of postoperative pain treatments and unmet needs. Best Pract. Res. Clin. Anaesthesiol. 2019, 33, 269–286. [Google Scholar] [CrossRef]
- Gabriel, R.A.; Swisher, M.W.; Sztain, J.F.; Furnish, T.; Ilfeld, B.; Said, E.T. State of the art opioid-sparing strategies for post-operative pain in adult surgical patients. Expert Opin. Pharmacother. 2019, 20, 949–961. [Google Scholar] [CrossRef] [Green Version]
- Smith, H.S. Perioperative Intravenous Acetaminophen and NSAIDs. Pain Med. 2011, 12, 961–981. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, D.; Lyons, M.; Montgomery, R.; Quinlan-Colwell, A. Exploring Opioid-Sparing Multimodal Analgesia Options in Trauma: A Nursing Perspective. J. Trauma Nurs. 2016, 23, 361–375. [Google Scholar] [CrossRef] [Green Version]
- Martinez, V.; Beloeil, H.; Marret, E.; Fletcher, D.; Ravaud, P.; Trinquart, L. Non-opioid analgesics in adults after major surgery: Systematic review with network meta-analysis of randomized trials. Br. J. Anaesth. 2016, 118, 22–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howard, M.L.; Isaacs, A.N.; Nisly, S. Continuous Infusion Nonsteroidal Anti-Inflammatory Drugs for Perioperative Pain Management. J. Pharm. Pract. 2016, 31, 66–81. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.A.; Black, L.K.; Sharma, D.; Bhagnani, T.; Jahr, J.S. Efficacy of non-opioid analgesics to control postoperative pain: A network meta-analysis. BMC Anesthesiol. 2020, 20, 272. [Google Scholar] [CrossRef]
- Mehraban, S.S.; Suddle, R.; Mehraban, S.; Petrucci, S.; Moretti, M.; Cabbad, M.; Lakhi, N. Opioid-freemultimodal analgesia pathway to decrease opioid utilization after cesarean delivery. J. Obstet. Gynaecol. Res. 2020, 47, 873–881. [Google Scholar] [CrossRef]
- Herbert, K.A.; Yurashevich, M.; Fuller, M.; Pedro, C.D.; Habib, A.S. Impact of a multimodal analgesic protocol modification on opioid consumption after cesarean delivery: A retrospective cohort study. J. Matern. Neonatal Med. 2021, 35, 4743–4749. [Google Scholar] [CrossRef]
- Nimmo, S.M.; Foo, I.T.; Paterson, H.M. Enhanced recovery after surgery: Pain management. J. Surg. Oncol. 2017, 116, 583–591. [Google Scholar] [CrossRef]
- Mercadante, S. The use of anti-inflammatory drugs in cancer pain. Cancer Treat. Rev. 2001, 27, 51–61. [Google Scholar] [CrossRef]
- Helander, E.M.; Menard, B.L.; Harmon, C.M.; Homra, B.K.; Allain, A.V.; Bordelon, G.J.; Wyche, M.Q.; Padnos, I.W.; Lavrova, A.; Kaye, A.D. Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. Curr. Pain Headache Rep. 2017, 21, 3. [Google Scholar] [CrossRef]
- Beverly, A.; Kaye, A.D.; Ljungqvist, O.; Urman, R.D. Essential Elements of Multimodal Analgesia in Enhanced Recovery after Surgery (ERAS) Guidelines. Anesthesiol. Clin. 2017, 35, e115–e143. [Google Scholar] [CrossRef]
- Mitra, S.; Carlyle, D.; Kodumudi, G.; Kodumudi, V.; Vadivelu, N. New Advances in Acute Postoperative Pain Management. Curr. Pain Headache Rep. 2018, 22, 35. [Google Scholar] [CrossRef] [PubMed]
- Martinez, L.; Ekman, E.; Nakhla, N. Perioperative Opioid-sparing Strategies: Utility of Conventional NSAIDs in Adults. Clin. Ther. 2019, 41, 2612–2628. [Google Scholar] [CrossRef]
- Janczura, M.; Kobus-Moryson, M.; Sip, S.; Żarowski, M.; Wareńczak, A.; Cielecka-P iontek, J. Fixed-Dose Combination of NSAIDs and Spasmolytic Agents in the Treatment of Different Types of Pain—A Practical Review. J. Clin. Med. 2021, 10, 3118. [Google Scholar] [CrossRef] [PubMed]
- Pitchon, D.N.; Dayan, A.C.; Schwenk, E.S.; Baratta, J.L.; Viscusi, E.R. Updates on Multimodal Analgesia for Orthopedic Surgery. Anesthesiol. Clin. 2018, 36, 361–373. [Google Scholar] [CrossRef] [PubMed]
- Manworren, R.C. Multimodal Pain Management and the Future of a Personalized Medicine Approach to Pain. AORN J. 2015, 101, 307–318. [Google Scholar] [CrossRef]
- Lee, G.I.; Neumeister, M.W. Pain: Pathways and Physiology. Clin. Plast. Surg. 2020, 47, 173–180. [Google Scholar] [CrossRef]
- Mariateresa, F.P.; Varrassi, G.G. The Routes of Administration for Acute Postoperative Pain Medication. Pain Ther. 2021, 10, 909–925. [Google Scholar] [CrossRef]
- Bookstaver, B.; Miller, A.D.; Norris, L.B.; Rudisill, C.N. Intravenous ibuprofen: The first injectable product for the treatment of pain and fever. J. Pain Res. 2010, 3, 67–79. [Google Scholar] [CrossRef] [Green Version]
- Lambert, W.J. Considerations in Developing a Target Product Profile for Parenteral Pharmaceutical Products. AAPS PharmSciTech 2010, 11, 1476–1481. [Google Scholar] [CrossRef] [Green Version]
- Singla, N.K.; Parulan, C.; Samson, R.; Hutchinson, J.; Bushnell, R.; Beja, E.G.; Ang, R.; Royal, M.A. Plasma and Cerebrospinal Fluid Pharmacokinetic Parameters After Single-Dose Administration of Intravenous, Oral, or Rectal Acetaminophen. Pain Pract. 2012, 12, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Raffa, R.B.; Pawasauskas, J.; Pergolizzi, J.V., Jr.; Lu, L.; Chen, Y.; Wu, S.; Jarrett, B.; Fain, R.; Hill, L.; Devarakonda, K. Pharmacokinetics of Oral and Intravenous Paracetamol (Acetaminophen) When Co-Administered with Intravenous Morphine in Healthy Adult Subjects. Clin. Drug Investig. 2017, 38, 259–268. [Google Scholar] [CrossRef] [Green Version]
- Yeh, Y.C.; Reddy, P. Clinical and economic evidence for intravenous acetaminophen. Pharmacotherapy 2012, 32, 559–579. [Google Scholar] [CrossRef] [PubMed]
- Irvine, J.; Afrose, A.; Islam, N. Formulation and delivery strategies of ibuprofen: Challenges and opportunities. Drug Dev. Ind. Pharm. 2018, 44, 173–183. [Google Scholar] [CrossRef]
- Panchal, N.; Kaur, M.; Tharmatt, A.; Thakur, S.; Jain, S.K. Development, Characterization and Evaluation of Parenteral Formulation of Diclofenac Sodium. AAPS PharmSciTech 2020, 21, 219. [Google Scholar] [CrossRef]
- Xiang, Q.; Niu, G.; Wu, X.-H.; Chen, G. Stability and Determination of Metamizole Sodium by Capillary Electrophoresis Analysis Combined with Infra-red Spectroscopy. Chem. Res. Chin. Univ. 2007, 23, 654–658. [Google Scholar] [CrossRef]
- Berkowitz, R.D.; Mack, R.J.; McCallum, S.W. Meloxicam for intravenous use: Review of its clinical efficacy and safety for management of postoperative pain. Pain Manag. 2021, 11, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Aitken, P.; Stanescu, I.; Playne, R.; Zhang, J.; Frampton, C.M.A.; Atkinson, H.C. An integrated safety analysis of combined acetaminophen and ibuprofen (Maxigesic®/Combogesic®) in adults. J. Pain Res. 2019, 12, 621–634. [Google Scholar] [CrossRef] [Green Version]
- Jibril, F.; Sharaby, S.; Mohamed, A.; Wilby, K. Intravenous versus Oral Acetaminophen for Pain: Systematic Review of Current Evidence to Support Clinical Decision-Making. Can. J. Hosp. Pharm. 2015, 68, 238–247. [Google Scholar] [CrossRef] [Green Version]
- The European Agency for the Evaluation of Medicinal Products Veterinary Medicines and Inspections Committee for Veterinary Medicinal Products Metamizole Summary Report (2), (2003). Available online: http://www.emea.eu.int (accessed on 29 June 2023).
- Lutz, M. Metamizole (Dipyrone) and the Liver: A Review of the Literature. J. Clin. Pharmacol. 2019, 59, 1433–1442. [Google Scholar] [CrossRef]
- Conaghan, P.G. A turbulent decade for NSAIDs: Update on current concepts of classification, epidemiology, comparative efficacy, and toxicity. Rheumatol. Int. 2011, 32, 1491–1502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tramŕr, D.R.; Williams, J.E.; Carroll, D.; Wiffen, P.J.; Moore, R.A.; McQuay, H.J. Comparing analgesic efficacy of non-steroidal anti-inflammatory drugs given by different routes in acute and chronic pain: A qualitative systematic review. Acta Anaesthesiol. Scand. 1998, 42, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Dwarica, D.S.; Pickett, S.D.; Zhao, Y.D.; Nihira, M.A.; Quiroz, L.H. Comparing Ketorolac with Ibuprofen for Postoperative Pain: A Randomized Clinical Trial. Urogynecology 2019, 26, 233–238. [Google Scholar] [CrossRef]
- Mazaleuskaya, L.L.; Theken, K.N.; Gong, L.; Thorn, C.F.; FitzGerald, G.A.; Altman, R.B.; Klein, T.E. PharmGKB summary: Ibuprofen pathways. Pharmacogenetics Genom. 2015, 25, 96–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pavliv, L.; Voss, B.; Rock, A. Pharmacokinetics, safety, and tolerability of a rapid infusion of i.v. ibuprofen in healthy adults. Am. J. Health Pharm. 2011, 68, 47–51. [Google Scholar] [CrossRef]
- Munsterhjelm, E.; Niemi, T.; Syrjälä, M.; Ylikorkala, O.; Rosenberg, P. Propacetamol augments inhibition of platelet function by diclofenac in volunteers. Br. J. Anaesth. 2003, 91, 357–362. [Google Scholar] [CrossRef] [Green Version]
- Freo, U.; Ruocco, C.; Valerio, A.; Scagnol, I.; Nisoli, E. Paracetamol: A Review of Guideline Recommendations. J. Clin. Med. 2021, 10, 3420. [Google Scholar] [CrossRef]
- Acetaminophen Intravenous Solution (Drugs@FDA: FDA-Approved Drugs), (n.d.). Available online: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=202605 (accessed on 25 May 2022).
- European Medicines Agency. Paracetamol (IV Formulation): List of Nationally Authorised Medicinal Products; PSUSA/00002311/201705, (n.d.). Available online: https://www.ema.europa.eu/en/documents/psusa/paracetamol-iv-formulation-list-nationally-authorised-medicinal-products-psusa/00002311/201705_en.pdf (accessed on 25 May 2022).
- Weinberg, L.; Chiam, E.; Weinberg, L.; Bellomo, R. Paracetamol: A Review with Specific Focus on the Haemodynamic Effects of Intravenous Administration. Heart Lung Vessel. 2015, 7, 121. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4476766/ (accessed on 25 May 2022).
- Hoffmann, F.; Bantel, C.; von Rosen, F.T.; Jobski, K. Regional Differences in Prescribing Patterns of Metamizole in Germany Based on Data from 70 Million Persons. Int. J. Environ. Res. Public Health 2020, 17, 3892. [Google Scholar] [CrossRef] [PubMed]
- Ungprasert, P.; Cheungpasitporn, W.; Crowson, C.S.; Matteson, E.L. Individual non-steroidal anti-inflammatory drugs and risk of acute kidney injury: A systematic review and meta-analysis of observational studies. Eur. J. Intern. Med. 2015, 26, 285–291. [Google Scholar] [CrossRef]
- Abdeena, A.; Abdelkader, A.; Elgazzar, D.; Aboubakr, M.; Abdulah, O.A.; Shoghy, K.; Abdel-Daim, M.; El-Serehy, H.A.; Najda, A.; El-Mleeh, A. Coenzyme Q10 supplementation mitigates piroxicam-induced oxidative injury and apoptotic pathways in the stomach, liver, and kidney. Biomed. Pharmacother. 2020, 130, 110627. [Google Scholar] [CrossRef]
- Gaertner, J.; Stamer, U.M.; Remi, C.; Voltz, R.; Bausewein, C.; Sabatowski, R.; Wirz, S.; Müller-Mundt, G.; Simon, S.T.; Pralong, A.; et al. Metamizole/dipyrone for the relief of cancer pain: A systematic review and evidence-based recommendations for clinical practice. Palliat. Med. 2016, 31, 26–34. [Google Scholar] [CrossRef] [Green Version]
- Rudin, D.; Schmutz, M.; Roos, N.J.; Bouitbir, J.; Krähenbühl, S. Reactive Metamizole Metabolites Enhance the Toxicity of Hemin on the ATP Pool in HL60 Cells by Inhibition of Glycolysis. Biomedicines 2020, 8, 212. [Google Scholar] [CrossRef] [PubMed]
- Cecílio, N.T.; Souza, G.R.; Alves-Filho, J.C.; Cunha, F.Q.; Cunha, T.M. The PI3Kγ/AKT signaling pathway mediates peripheral antinociceptive action of dipyrone. Fundam. Clin. Pharmacol. 2020, 35, 364–370. [Google Scholar] [CrossRef]
- Weber, S.; Benesic, A.; Gerbes, A.L. Further evidence for the hepatotoxic potential of metamizole. Br. J. Clin. Pharmacol. 2020, 87, 1587–1588. [Google Scholar] [CrossRef]
- Andrade, S.; Bartels, D.B.; Lange, R.; Sandford, L.; Gurwitz, J. Safety of metamizole: A systematic review of the literature. J. Clin. Pharm. Ther. 2016, 41, 459–477. [Google Scholar] [CrossRef] [PubMed]
- Klose, S.; Pflock, R.; König, I.R.; Linder, R.; Schwaninger, M. Metamizole and the risk of drug-induced agranulocytosis and neutropenia in statutory health insurance data. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2019, 393, 681–690. [Google Scholar] [CrossRef]
- Trautmann, A.; Brockow, K.; Stoevesandt, J. Metamizole-induced reactions as a paradigm of drug hypersensitivity: Non-allergic reactions, anaphylaxis, and delayed-type allergy. Clin. Exp. Allergy 2020, 50, 1103–1106. [Google Scholar] [CrossRef]
- Shah, R.R. Metamizole (dipyrone)-induced agranulocytosis: Does the risk vary according to ethnicity? J. Clin. Pharm. Ther. 2018, 44, 129–133. [Google Scholar] [CrossRef] [Green Version]
- Sarzi-Puttini, P.; Atzeni, F.; Lanata, L.; Bagnasco, M. Efficacy of Ketoprofen vs. Ibuprofen and Diclofenac: A Systematic Review of the Literature and Meta-Analysis. Clin. Exp. Rheumatol. 2013, 31, 731–738. Available online: https://www.ncbi.nlm.nih.gov/books/NBK190381/ (accessed on 22 March 2021).
- Gomes, F.I.F.; Cunha, F.Q.; Cunha, T.M. Peripheral nitric oxide signaling directly blocks inflammatory pain. Biochem. Pharmacol. 2020, 176, 113862. [Google Scholar] [CrossRef]
- dos Santos, G.G.; Vieira, W.F.; Vendramini, P.H.; da Silva, B.B.; Magalhães, S.F.; Tambeli, C.H.; Parada, C.A. Dipyrone is locally hydrolyzed to 4-methylaminoantipyrine and its antihyperalgesic effect depends on CB2 and kappa-opioid receptors activation. Eur. J. Pharmacol. 2020, 874, 173005. [Google Scholar] [CrossRef]
- Yamada, H.; Shimoyama, N.; Sora, I.; Uhl, G.R.; Fukuda, Y.; Moriya, H.; Shimoyama, M. Morphine can produce analgesia via spinal kappa opioid receptors in the absence of mu opioid receptors. Brain Res. 2006, 1083, 61–69. [Google Scholar] [CrossRef]
- Cunha, T.M.; Souza, G.R.; Domingues, A.C.; Carreira, E.U.; Lotufo, C.M.; Funez, M.I.; Verri, W.A.; Cunha, F.Q.; Ferreira, S.H.; Verri, J.W.A. Stimulation of Peripheral Kappa Opioid Receptors Inhibits Inflammatory Hyperalgesia via Activation of the PI3Kγ/AKT/nNOS/NO Signaling Pathway. Mol. Pain 2012, 8, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nikolova, I.; Tencheva, J.; Voinikov, J.; Petkova, V.; Benbasat, N.; Danchev, N. Metamizole: A Review Profile of a Well-Known “Forgotten” Drug. Part I: Pharmaceutical and Nonclinical Profile. Biotechnol. Biotechnol. Equip. 2012, 26, 3329–3337. [Google Scholar] [CrossRef]
- Salmeron-Garcia, A.; Navas, N.; Martin, A.; Roman, E.; Cabeza, J.; Capitan-Vallvey, L.F. Determination of tramadol, metamizole, ropivacaine, and bupivacaine in analgesic mixture samples by HPLC with DAD detection. J. Chromatogr. Sci. 2009, 47, 231–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grosser, T.; Ricciotti, E.; FitzGerald, G.A. The Cardiovascular Pharmacology of Nonsteroidal Anti-Inflammatory Drugs. Trends Pharmacol. Sci. 2017, 38, 733–748. [Google Scholar] [CrossRef]
- Jain, A.K. Solubilization of indomethacin using hydrotropes for aqueous injection. Eur. J. Pharm. Biopharm. 2008, 68, 701–714. [Google Scholar] [CrossRef]
- Ansari, K.K.; Sharma, N. Formulation and evaluation of orodispersible tablets of lornoxicam. J. Drug Deliv. Ther. 2018, 8, 225–228. [Google Scholar] [CrossRef]
- Yeh, M.-K.; Chang, L.-C.; Chiou, A.H.-J. Improving Tenoxicam Solubility and Bioavailability by Cosolvent System. AAPS PharmSciTech 2009, 10, 166–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bakar, S.K.; Niazi, S. Stability of Aspirin in Different Media. J. Pharm. Sci. 1983, 72, 1024–1026. [Google Scholar] [CrossRef]
- Feldene 20 mg/1 mL Injectable Solution—Summary of Product Characteristics (SmPC)—(Pfizer), (n.d.). Available online: https://labeling.pfizer.com/ShowLabeling.aspx?id=5277 (accessed on 23 May 2022).
- Movalis 15 mg/1,5 mL—Summary of Product Characteristics (SmPC)—(ADC.sk), (n.d.). Available online: https://www.adc.sk/databazy/produkty/pil/movalis-15-mg-1-5-ml-491875.html (accessed on 23 May 2022).
- Rainsford, K.D.; Bjarnason, I. NSAIDs: Take with food or after fasting? J. Pharm. Pharmacol. 2011, 64, 465–469. [Google Scholar] [CrossRef]
- Moore, R.A.; Derry, S.; Wiffen, P.J.; Straube, S. Effects of food on pharmacokinetics of immediate release oral formulations of aspirin, dipyrone, paracetamol and NSAIDs—A systematic review. Br. J. Clin. Pharmacol. 2015, 80, 381–388. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, N.A.; Turturro, M.A.; Istvan, D.J.; Larkin, G.L. Patients’ Perceptions of Route of Nonsteroidal Anti-inflammatory Drug Administration and Its Effect on Analgesia. Acad. Emerg. Med. 2000, 7, 857–861. [Google Scholar] [CrossRef] [PubMed]
- Fda, Cder, Caldolor (Ibuprofen) Injection-Summary of Product Characteristics (SmPC)—(FDA), (n.d.). Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/022348s018lbl.pdf (accessed on 27 June 2022).
- Ketorolac Tromethamine Solution for Injection (Hospira)—Summary of Product Characteristics (SmPC)—(FDA), (n.d.). Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/074802s038lbl.pdf (accessed on 27 June 2022).
- Aspegic InjecTable 1 g—Summary of Product Characteristics (SmPC)—(ANSM), (n.d.). Available online: http://agence-prd.ansm.sante.fr/php/ecodex/rcp/R0276307.htm (accessed on 23 May 2022).
- Dexketoprofen, B. Braun 50 MG/100 ML Solution for Perfusion-Summary of Product Characteristics (SmPC)—(Cima), (n.d.). Available online: https://cima.aemps.es/cima/dochtml/ft/83328/FT_83328.html (accessed on 23 May 2022).
- Morsadex 50 mg/2 mL Solution for Injection/Infusion—Summary of Product Characteristics (SmPC)—(hpra), (n.d.). Available online: https://www.hpra.ie/img/uploaded/swedocuments/f1bf49ef-2add-49ed-a136-c9289bb7d152.pdf (accessed on 23 May 2022).
- Voltarol Ampoules—Summary of Product Characteristics (SmPC)—(emc), (n.d.). Available online: https://www.medicines.org.uk/emc/medicine/1339#gref (accessed on 20 May 2022).
- REUMON I.M.—Summary of Product Characteristics (SmPC)—(indice.eu), (n.d.). Available online: https://www.indice.eu/pt/medicamentos/medicamentos/reumon-im/folheto-informativo (accessed on 23 May 2022).
- Ibuprofen, B. Braun 400 mg Solution for Infusion-Summary of Product Characteristics (SmPC)—(hpra), (n.d.). Available online: http://www.hpra.ie/img/uploaded/swedocuments/441ba0ac-92c2-4fdf-b35e-9ff01e4b77c1.pdf (accessed on 23 May 2022).
- Liometacin 50 mg/2 mL Injectable—Summary of Product Characteristics (SmPC)—(AIFA), (n.d.). Available online: https://farmaci.agenziafarmaco.gov.it/aifa/servlet/PdfDownloadServlet?pdfFileName=footer_007206_022559_FI.pdf&sys=m0b1l3 (accessed on 23 May 2022).
- ORUDIS 100 mg Injectable Solution—Summary of Product Characteristics (SmPC)—(Cima), (n.d.). Available online: https://cima.aemps.es/cima/dochtml/ft/55857/FT_55857.html (accessed on 23 May 2022).
- Ketorolac Trometamol 30 mg/mL Solution for Injection—Summary of Product Characteristics (SmPC)—(emc), (n.d.). Available online: https://www.medicines.org.uk/emc/product/11547/smpc#gref (accessed on 23 May 2022).
- Xefo 8 mg Solution for Injection-Summary of Product Characteristics (SmPC)—(hpra), (n.d.). Available online: http://www.hpra.ie/img/uploaded/swedocuments/LicenseSPC_PA1547-005-003_11032015142107.pdf (accessed on 23 May 2022).
- Tenoxicam 20 mg Lyophilisate for Solution for Injection (Drugs.com), (n.d.). Available online: https://www.drugs.com/uk/tenoxicam-20-mg-lyophilisate-for-solution-for-injection-leaflet.html (accessed on 23 May 2022).
- Schjerning, A.-M.; McGettigan, P.; Gislason, G. Cardiovascular effects and safety of (non-aspirin) NSAIDs. Nat. Rev. Cardiol. 2020, 17, 574–584. [Google Scholar] [CrossRef]
- García-Rayado, G.; Navarro, M.; Lanas, A. NSAID induced gastrointestinal damage and designing GI-sparing NSAIDs. Expert Rev. Clin. Pharmacol. 2018, 11, 1031–1043. [Google Scholar] [CrossRef] [PubMed]
- Miranda, H.F.; Puig, M.M.; Prieto, J.C.; Pinardi, G. Synergism between paracetamol and nonsteroidal anti-inflammatory drugs in experimental acute pain. Pain 2006, 121, 22–28. [Google Scholar] [CrossRef]
- Atkinson, H.C.; Stanescu, I.; Frampton, C.; Salem, I.I.; Beasley, C.P.H.; Robson, R. Pharmacokinetics and Bioavailability of a Fixed-Dose Combination of Ibuprofen and Paracetamol after Intravenous and Oral Administration. Clin. Drug Investig. 2015, 35, 625–632. [Google Scholar] [CrossRef] [Green Version]
- Assessment Report—Paracetamol/Ibuprofen 500 mg/150 mg Film Coated Tablets and Associated Names (EMEA/H/A-29(4)/1447-Annex II-Scientific Conclusions)—(EMA), (n.d.). Available online: https://www.ema.europa.eu/en/documents/referral/paracetamol/ibuprofen-500mg/150mg-article-294-referral-annex-ii_en.pdf (accessed on 15 June 2022).
- Paracetamol/Ibuprofen 500 mg/150 mg Film-Coated Tablets|European Medicines Agency, (n.d.). Available online: https://www.ema.europa.eu/en/medicines/human/referrals/paracetamolibuprofen-500-mg150-mg-film-coated-tablets (accessed on 1 April 2022).
- Public Assessment Report (SE/H/1948/01/DC)-EMA, (n.d.). Available online: https://docetp.mpa.se/LMF/Paracetamol_Ibuprofen%20Vale%20Pharma%20solution%20for%20infusion%20ENG%20PAR_09001bee811a4600.pdf (accessed on 28 June 2022).
- Public Assessment Report Scientific Discussion (SE/H/2093/001/DC)-(EMA), (n.d.). Available online: https://docetp.mpa.se/LMF/Comboval%20solution%20for%20infusion%20ENG%20PAR_09001bee825ee5b5.pdf (accessed on 14 June 2022).
- Abushanab, D.; Al-Badriyeh, D. Efficacy and Safety of Ibuprofen Plus Paracetamol in a Fixed-Dose Combination for Acute Postoperative Pain in Adults: Meta-Analysis and a Trial Sequential Analysis. CNS Drugs 2021, 35, 105–120. [Google Scholar] [CrossRef]
- US FDA Accepts Maxigesic IV® New Drug Application—NZX, New Zealand’s Exchange, (n.d.). Available online: https://www.nzx.com/announcements/381916 (accessed on 6 April 2022).
- Menhinick, K.A.; Gutmann, J.L.; Regan, J.D.; Taylor, S.E.; Buschang, P.H. The efficacy of pain control following nonsurgical root canal treatment using ibuprofen or a combination of ibuprofen and acetaminophen in a randomized, double-blind, placebo-controlled study. Int. Endod. J. 2004, 37, 531–541. [Google Scholar] [CrossRef] [PubMed]
- Mehlisch, D.R.; Aspley, S.; Daniels, S.E.; Bandy, D.P. Comparison of the analgesic efficacy of concurrent ibuprofen and paracetamol with ibuprofen or paracetamol alone in the management of moderate to severe acute postoperative dental pain in adolescents and adults: A randomized, double-blind, placebo-controlled, parallel-group, single-dose, two-center, modified factorial study. Clin. Ther. 2010, 32, 882–895. [Google Scholar] [CrossRef]
- Merry, A.; Gibbs, R.; Edwards, J.; Ting, G.; Frampton, C.; Davies, E.; Anderson, B. Combined acetaminophen and ibuprofen for pain relief after oral surgery in adults: A randomized controlled trial. Br. J. Anaesth. 2010, 104, 80–88. [Google Scholar] [CrossRef] [Green Version]
- Bondarsky, E.E.; Domingo, A.T.; Matuza, N.M.; Taylor, M.B.; Thode, H.C.; Singer, A.J. Ibuprofen vs acetaminophen vs their combination in the relief of musculoskeletal pain in the ED: A randomized, controlled trial. Am. J. Emerg. Med. 2013, 31, 1357–1360. [Google Scholar] [CrossRef] [PubMed]
- Ostojic, P.; Radunovic, G.; Lazovic, M.; Tomanovic-Vujadinovic, S. Ibuprofen plus paracetamol versus ibuprofen in acute low back pain: A randomized open label multicenter clinical study. Acta Reumatol. Port. 2017, 2017, 18–25. [Google Scholar]
- Daniels, S.E.; Atkinson, H.C.; Stanescu, I.; Frampton, C. Analgesic Efficacy of an Acetaminophen/Ibuprofen Fixed-dose Combination in Moderate to Severe Postoperative Dental Pain: A Randomized, Double-blind, Parallel-group, Placebo-controlled Trial. Clin. Ther. 2018, 40, 1765–1776. [Google Scholar] [CrossRef] [Green Version]
- Stamos, D.A.; Drum, D.M.; Al Reader, D.; Nusstein, D.J.; Fowler, D.S.; Beck, D.M. An Evaluation of Ibuprofen Versus Ibuprofen/Acetaminophen for Postoperative Endodontic Pain in Patients with Symptomatic Irreversible Pulpitis and Symptomatic Apical Periodontitis. Anesthesia Prog. 2019, 66, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.W.; Irizarry, E.; Chertoff, A.; Feliciano, C.; Solorzano, C.; Zias, E.; Gallagher, E.J. Ibuprofen Plus Acetaminophen Versus Ibuprofen Alone for Acute Low Back Pain: An Emergency Department–Based Randomized Study. Acad. Emerg. Med. 2019, 27, 229–235. [Google Scholar] [CrossRef]
- Dahl, V.; Dybvik, T.; Steen, T.; Aune, A.K.; Rosenlund, E.K.; Ræder, J.C. Ibuprofen vs. acetaminophen vs. ibuprofen and acetaminophen after arthroscopically assisted anterior cruciate ligament reconstruction. Eur. J. Anaesthesiol. 2004, 21, 471–475. [Google Scholar] [CrossRef]
- Thybo, K.H.; Hägi-Pedersen, D.; Dahl, J.B.; Wetterslev, J.; Nersesjan, M.; Jakobsen, J.C.; Pedersen, N.A.; Overgaard, S.; Schrøder, H.M.; Schmidt, H.; et al. Effect of Combination of Paracetamol (Acetaminophen) and Ibuprofen vs Either Alone on Patient-Controlled Morphine Consumption in the First 24 Hours After Total Hip Arthroplasty: The PANSAID Randomized Clinical Trial. JAMA 2019, 321, 562–571. [Google Scholar] [CrossRef] [Green Version]
- Doherty, M.; Hawkey, C.; Goulder, M.; Gibb, I.; Hill, N.; Aspley, S.; Reader, S. A randomised controlled trial of ibuprofen, paracetamol or a combination tablet of ibuprofen/paracetamol in community-derived people with knee pain. Ann. Rheum. Dis. 2011, 70, 1534–1541. [Google Scholar] [CrossRef] [PubMed]
- Kellstein, D.; Leyva, R. Evaluation of Fixed-Dose Combinations of Ibuprofen and Acetaminophen in the Treatment of Postsurgical Dental Pain: A Pilot, Dose-Ranging, Randomized Study. Drugs R D 2020, 20, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Wells, L.K.; Drum, M.; Nusstein, J.; Reader, A.; Beck, M. Efficacy of Ibuprofen and Ibuprofen/Acetaminophen on Postoperative Pain in Symptomatic Patients with a Pulpal Diagnosis of Necrosis. J. Endod. 2011, 37, 1608–1612. [Google Scholar] [CrossRef] [PubMed]
- Ianiro, S.R.; Jeansonne, B.G.; McNeal, S.F.; Eleazer, P.D. The Effect of Preoperative Acetaminophen or a Combination of Acetaminophen and Ibuprofen on the Success of Inferior Alveolar Nerve Block for Teeth with Irreversible Pulpitis. J. Endod. 2007, 33, 11–14. [Google Scholar] [CrossRef]
- Hung, K.K.; Graham, C.A.; Lo, R.; Leung, Y.K.; Leung, L.Y.; Man, S.Y.; Woo, W.K.; Cattermole, G.; Rainer, T.H. Oral paracetamol and/or ibuprofen for treating pain after soft tissue injuries: Single centre double-blind, randomised controlled clinical trial. PLoS ONE 2018, 13, e0192043. [Google Scholar] [CrossRef]
- Mallama, M.; Valencia, A.; Rijs, K.; Rietdijk, W.J.R.; Klimek, M.; Calvache, J.A. A systematic review and trial sequential analysis of intravenous vs. oral peri-operative paracetamol. Anaesthesia 2021, 76, 270–276. [Google Scholar] [CrossRef]
- Fux, D.; Metzner, M.; Brandl, J.; Feist, M.; Behrendt-Wippermann, M.; von Thaden, A.; Baumgartner, C. Pharmacokinetics of metamizole (dipyrone) as an add-on in calves undergoing umbilical surgery. PLoS ONE 2022, 17, e0265305. [Google Scholar] [CrossRef]
- Schneider, T.; Mauermann, E.; Ilgenstein, B.; Jaquiery, C.; Ruppen, W. Analgesic benefit of metamizole and ibuprofen vs. either medication alone: A randomized clinical trial. Minerva Anestesiol. 2022, 88, 448–456. [Google Scholar] [CrossRef]
- Comboval 10 mg/mL + 3 mg/mL Oplossing Voor Infusie | Geneesmiddeleninformatiebank | College ter Beoordeling van Geneesmiddelen, (n.d.). Available online: https://www.geneesmiddeleninformatiebank.nl/nl/rvg128889 (accessed on 28 November 2022).
- Buscapina Compositum 2500 mg/20 mg Injectable Solution-Summary of Product Characteristics (SmPC)—(CIMA), (n.d.). Available online: https://cima.aemps.es/cima/pdfs/es/ft/26791/FT_26791.pdf (accessed on 29 June 2022).
- Litalgin 500 mg/mL + 2 mg/mL Injectable Solution-Summary of Product Characteristics (SmPC)—(nam.fi), (n.d.). Available online: http://spc.nam.fi/indox/english/html/nam/humspc/3/23209023.pdf (accessed on 29 June 2022).
- Analgin Injectable Solution-Summary of Product Characteristics (SmPC)—(SUKL.eu), (n.d.). Available online: https://www.sukl.eu/modules/medication/detail.php?code=0107987&tab=texts (accessed on 29 June 2022).
- DORILEN—Summary of Product Characteristics (SmPC)—(bulas.med.br), (n.d.). Available online: https://www.bulas.med.br/p/bulas-de-medicamentos/bula/1330333/dorilen+solucao+injetavel.htm (accessed on 29 June 2022).
- Dexalgen—Summary of Product Characteristics (SmPC)—(Eurofarma), (n.d.). Available online: https://eurofarma.com.br/produtos/bulas/patient/bula-dexalgen.html (accessed on 29 June 2022).
- Viadil Compuesto Injectable Solution—Summary of Product Characteristics (SmPC)—(Vademecum), (n.d.). Available online: https://www.vademecum.es/equivalencia-lista-viadil+compuesto+solucion+inyectable-chile-a03da+p1-1289610-cl_1 (accessed on 29 June 2022).
- Daniels, S.E.; Playne, R.; Stanescu, I.; Zhang, J.; Gottlieb, I.J.; Atkinson, H.C. Efficacy and Safety of an Intravenous Acetaminophen/Ibuprofen Fixed-dose Combination After Bunionectomy: A Randomized, Double-blind, Factorial, Placebo-controlled Trial. Clin. Ther. 2019, 41, 1982–1995.e8. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.; Abubaker, H.; Demas, E.; Ahrendtsen, L. A randomized trial comparing the safety and efficacy of intravenous ibuprofen versus ibuprofen and acetaminophen in knee or hip arthroplasty. Pain Physician 2016, 19, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, J.E.; Sutherland, C.J.; Kestin, I.G.; Sneyd, J.R. Morphine consumption in patients receiving rectal paracetamol and diclofenac alone and in combination. Br. J. Anaesth. 1996, 77, 445–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romundstad, L.; Stubhaug, A.; Niemi, G.; Rosseland, L.A.; Breivik, H. Adding propacetamol to ketorolac increases the tolerance to painful pressure. Eur. J. Pain 2006, 10, 177. [Google Scholar] [CrossRef] [Green Version]
- Msolli, M.A.; Sekma, A.; Toumia, M.; Khalil, H.M.; Khalil, M.H.; Grissa, M.H.; Bouida, W.; Beltaief, K.; Zorgati, A.; Methamem, M.; et al. Acetaminophen, Nonsteroidal Anti-inflammatory Drugs, or Combination of Both Analgesics in Acute Posttrauma Pain: A Randomized Controlled Trial. Acad. Emerg. Med. 2020, 28, 155–163. [Google Scholar] [CrossRef]
- Kim, D.-W.; Weon, K.Y. Pharmaceutical application and development of fixed-dose combination: Dosage form review. J. Pharm. Investig. 2021, 51, 555–570. [Google Scholar] [CrossRef]
- Jayasheel, B. Regulatory requirements for marketing fixed dose combinations. Perspect. Clin. Res. 2010, 1, 120. [Google Scholar] [CrossRef]
- Desai, D.; Wang, J.; Wen, H.; Li, X.; Timmins, P. Formulation design, challenges, and development considerations for fixed dose combination (FDC) of oral solid dosage forms. Pharm. Dev. Technol. 2012, 18, 1265–1276. [Google Scholar] [CrossRef]
- Nøhr-Nielsen, A.; De Bruin, M.L.; Thomsen, M.; Pipper, C.B.; Lange, T.; Bjerrum, O.J.; Lund, T.M. Body of evidence and approaches applied in the clinical development programme of fixed-dose combinations in the European Union from 2010 to 2016. Br. J. Clin. Pharmacol. 2019, 85, 1829–1840. [Google Scholar] [CrossRef]
- Clinical Development of Fixed Combination Medicinal Products—Scientific Guideline | European Medicines Agency, (n.d.). Available online: https://www.ema.europa.eu/en/clinical-development-fixed-combination-medicinal-products-scientific-guideline (accessed on 1 July 2023).
- Kwon, K.C.; Lee, C. Implications for Designing a Regulatory Shortcut to New Drug Application. Ther. Innov. Regul. Sci. 2010, 51, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Fixed Dose Combinations, Co-Packaged Drug Products, and Single-Entity Versions of Previously Approved Antiretrovirals for the Treatment of HIV | FDA, (n.d.). Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/fixed-dose-combinations-co-packaged-drug-products-and-single-entity-versions-previously-approved (accessed on 1 July 2023).
- Codevelopment of Two or more New Investigational Drugs for Use in Combination | FDA, (n.d.). Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/codevelopment-two-or-more-new-investigational-drugs-use-combination (accessed on 1 July 2023).
- Breivik, E.K.; Barkvoll, P.; Skovlund, E. Combining diclofenac with acetaminophen or acetaminophen-codeine after oral surgery: A randomized, double-blind single-dose study. Clin. Pharmacol. Ther. 1999, 66, 625–635. [Google Scholar] [CrossRef]
- Beck, D.H.; Schenk, M.R.; Hagemann, K.; Doepfmer, U.R.; Kox, W.J. The Pharmacokinetics and Analgesic Efficacy of Larger Dose Rectal Acetaminophen (40 mg/kg) in Adults: A Double-Blinded, Randomized Study. Obstet. Anesthesia Dig. 2000, 90, 431–436. [Google Scholar] [CrossRef]
- Siddik, S.M.; Aouad, M.T.; Jalbout, M.I.; Rizk, L.B.; Kamar, G.H.; Baraka, A.S. Diclofenac and/or Propacetamol for Postoperative Pain Management After Cesarean Delivery in Patients Receiving Patient Controlled Analgesia Morphine. Reg. Anesth. Pain Med. 2001, 26, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Man, S.; Woo, W.; Lam, P.; Rainer, T.; Rainer, T.H.; Yan, M.S.; Keung, F.W.W.; Wai, L.K.; Phil, M. Feasibility study comparing oral paracetamol and oral non-steroidal anti-inflammatory drugs for treating pain after musculoskeletal injury: A randomised, double blind, controlled trial. Hong Kong J. Emerg. Med. 2004, 11, 78–84. [Google Scholar] [CrossRef]
- Hiller, A.; Silvanto, M.; Savolainen, S.; Tarkkila, P. Propacetamol and diclofenac alone and in combination for analgesia after elective tonsillectomy. Acta Anaesthesiol. Scand. 2004, 48, 1185–1189. [Google Scholar] [CrossRef]
- Woo, W.W.; Man, S.-Y.; Lam, P.K.; Rainer, T. Randomized Double-Blind Trial Comparing Oral Paracetamol and Oral Nonsteroidal Antiinflammatory Drugs for Treating Pain after Musculoskeletal Injury. Ann. Emerg. Med. 2005, 46, 352–361. [Google Scholar] [CrossRef]
- Legeby, M.; Sandelin, K.; Wickman, M.; Olofsson, C. Analgesic efficacy of diclofenac in combination with morphine and paracetamol after mastectomy and immediate breast reconstruction. Acta Anaesthesiol. Scand. 2005, 49, 1360–1366. [Google Scholar] [CrossRef]
- Munishankar, B.; Fettes, P.; Moore, C.; McLeod, G. A double-blind randomised controlled trial of paracetamol, diclofenac or the combination for pain relief after caesarean section. Int. J. Obstet. Anesthesia 2008, 17, 9–14. [Google Scholar] [CrossRef]
- Ridderikhof, M.L.; Lirk, P.; Goddijn, H.; Vandewalle, E.; Schinkel, E.; Van Dieren, S.; Kemper, E.M.; Hollmann, M.W.; Goslings, J.C. Acetaminophen or Nonsteroidal Anti-Inflammatory Drugs in Acute Musculoskeletal Trauma: A Multicenter, Double-Blind, Randomized, Clinical Trial. Ann. Emerg. Med. 2018, 71, 357–368.e8. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, D.; Nègre, I.; Barbin, C.; François, A.; Carreres, C.; Falgueirettes, C.; Barboteu, A.; Samii, K. Postoperative analgesia with iv propacetamol and ketoprofen combination after disc surgery. Can. J. Anaesth. 1997, 44, 479–485. [Google Scholar] [CrossRef] [Green Version]
- Aubrun, F.; Langeron, O.; Heitz, D.; Coriat, P.; Riou, B. Randomised, placebo-controlled study of the postoperative analgesic effects of ketoprofen after spinal fusion surgery. Acta Anaesthesiol. Scand. 2000, 44, 934–939. [Google Scholar] [CrossRef]
- Fourcade, O.; Sanchez, P.; Kern, D.; Mazoit, J.-X.; Minville, V.; Samii, K. Propacetamol and ketoprofen after thyroidectomy. Eur. J. Anaesthesiol. 2005, 22, 373–377. [Google Scholar] [CrossRef]
- Akural, E.I.; Järvimäki, V.; Länsineva, A.; Niinimaa, A.; Alahuhta, S. Effects of combination treatment with ketoprofen 100 mg + acetaminophen 1000 mg on postoperative dental pain: A single-dose, 10-hour, randomized, double-blind, active- and placebo-controlled clinical trial. Clin. Ther. 2009, 31, 560–568. [Google Scholar] [CrossRef]
- Salonen, A.; Silvola, J.; Kokki, H. Does 1 or 2 g paracetamol added to ketoprofen enhance analgesia in adult tonsillectomy patients? Acta Anaesthesiol. Scand. 2009, 53, 1200–1206. [Google Scholar] [CrossRef] [PubMed]
- Iorno, V.; Landi, L.; Di Pasquale, R.; Cicenia, S.; Moschini, V. Comparison of intravenous ketorolac with or without paracetamol in postoperative pain control following ambulatory surgery. Curr. Med Res. Opin. 2013, 29, 1685–1690. [Google Scholar] [CrossRef] [PubMed]
- Vadivelu, N.; Gowda, A.M.; Urman, R.D.; Jolly, S.; Kodumudi, V.; Maria, M.; Taylor, R.; Pergolizzi, J.V. Ketorolac Tromethamine—Routes and Clinical Implications. Pain Pract. 2014, 15, 175–193. [Google Scholar] [CrossRef]
- Ong, C.K.S.; Seymour, R.A.; Lirk, P.; Merry, A.F. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: A qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth. Analg. 2010, 110, 1170–1179. [Google Scholar] [CrossRef]
- Lipscomb, G.R.; Wallis, N.; Armstrong, G.; Rees, W.D.W. Gastrointestinal tolerability of meloxicam and piroxicam: A double-blind placebo-controlled study. Br. J. Clin. Pharmacol. 1998, 46, 133–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Public Assessment Report (SE/H/1945/01/DC)-EMA, (n.d.). Available online: https://docetp.mpa.se/LMF/Paracetamol_Ibuprofen%20Vale%20solution%20for%20infusion%20ENG%20PAR_09001bee811a45fd.pdf (accessed on 6 April 2022).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, F.; Costa, G.; Veiga, F.; Cardoso, C.; Paiva-Santos, A.C. Parenteral Ready-to-Use Fixed-Dose Combinations Including NSAIDs with Paracetamol or Metamizole for Multimodal Analgesia—Approved Products and Challenges. Pharmaceuticals 2023, 16, 1084. https://doi.org/10.3390/ph16081084
Silva F, Costa G, Veiga F, Cardoso C, Paiva-Santos AC. Parenteral Ready-to-Use Fixed-Dose Combinations Including NSAIDs with Paracetamol or Metamizole for Multimodal Analgesia—Approved Products and Challenges. Pharmaceuticals. 2023; 16(8):1084. https://doi.org/10.3390/ph16081084
Chicago/Turabian StyleSilva, Fernando, Gustavo Costa, Francisco Veiga, Catarina Cardoso, and Ana Cláudia Paiva-Santos. 2023. "Parenteral Ready-to-Use Fixed-Dose Combinations Including NSAIDs with Paracetamol or Metamizole for Multimodal Analgesia—Approved Products and Challenges" Pharmaceuticals 16, no. 8: 1084. https://doi.org/10.3390/ph16081084
APA StyleSilva, F., Costa, G., Veiga, F., Cardoso, C., & Paiva-Santos, A. C. (2023). Parenteral Ready-to-Use Fixed-Dose Combinations Including NSAIDs with Paracetamol or Metamizole for Multimodal Analgesia—Approved Products and Challenges. Pharmaceuticals, 16(8), 1084. https://doi.org/10.3390/ph16081084