Health Insurance, Socio-Economic Position and Racial Disparities in Preventive Dental Visits in South Africa
Abstract
:1. Introduction
2. Methods
2.1. Data Source and Study Design
2.2. Data Collection Procedure and Measures
2.3. Measures
2.3.1. Socio-Demographic Characteristics
2.3.2. Material Wealth Index
2.3.3. Household Member Per Room (Crowding)
2.3.4. Nutritional Status (Food Security)
2.3.5. Tobacco Use Status
2.3.6. Self-Reported Dental Problems
2.3.7. Health Insurance Status
2.3.8. Preventive Dental Service Utilization
2.4. Data Analysis
2.5. Results
| % Privately Insured (n) | p-value | % visiting yearly (n) | p-value | |||
|---|---|---|---|---|---|---|
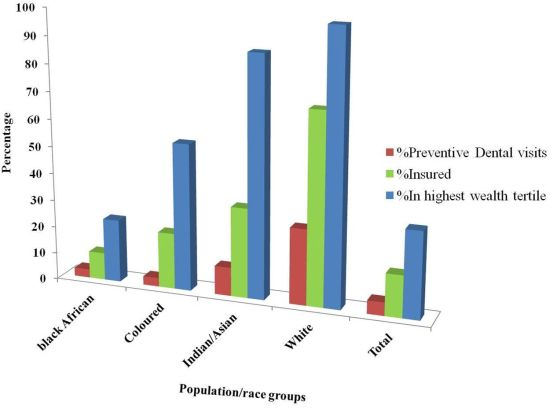
| Ethnicity/Race | <0.001 | <0.001 | ||||
| Black African | 10.1 (427) | 3.1 (123) | ||||
| Coloured | 21.6 (126) | 3.2 (19) | ||||
| Indian/Asian | 32.9 (195) | 10.5 (54) | ||||
| White | 70.0 (163) | 27.8 (74) | ||||
| Location | <0.001 | 0.001 | ||||
| Urban | 19.9 (744) | 5.7 (208) | ||||
| Rural | 6.2 (167) | 3.2 (62) | ||||
| Education | <0.001 | <0.001 | ||||
| <High school | 8.3 (400) | 2.3 (100) | ||||
| High School | 23.5 (248) | 7.9 (92) | ||||
| >High School | 56.5 (263) | 19.2 (78) | ||||
| Gender | 0.958 | 0.303 | ||||
| Male | 15.4 (383) | 4.5 (109) | ||||
| Female | 15.4 (528) | 5.2 (161) | ||||
| Nutritional status | <0.001 | <0.001 | ||||
| Poorest | 7.4 (262) | 2.2 (60) | ||||
| Middle | 20.8 (402) | 6.7 (122) | ||||
| Highest | 19.9 (247) | 6.4 (88) | ||||
| Tobacco use | <0.001 | 0.002 | ||||
| Never | 16.2 (650) | 5.4 (204) | ||||
| Ever snuff user | 4.4 (17) | 0.7 (4) | ||||
| Ever smoker | 16.2 (244) | 4.5 (62) | ||||
| Dental problem | 0.400 | 0.009 | ||||
| No | 15.6 (966) | 5.2 (235) | ||||
| Yes | 14.2 (145) | 2.8 (35) | ||||
| Privately insured | <0.001 | |||||
| No | - | 2.5 (112) | ||||
| Yes | - | 17.7 (156) | ||||
| Material wealth index | <0.001 | <0.001 | ||||
| Lowest | 2.2 (40) | 1.9 (24) | ||||
| Middle | 7.2 (181) | 2.2 (48) | ||||
| Highest | 36.4 (659) | 10.9 (195) | ||||
| Total population | 15.4 (13.4–17.7) | 4.9 (4.0–6.0) |
| Characteristics | Odds Ratio (95% Confidence Interval) | p-value | |
|---|---|---|---|
| Age | |||
| per year increase | 1.01 (1.00–1.02) | 0.049 | |
| Ethnicity/race | |||
| Black African | 1 | ||
| Coloured | 0.77 (0.42–1.40) | 0.390 | |
| Indian/Asian | 1.60 (0.95–2.70) | 0.077 | |
| White | 4.24 (2.54–7.09) | <0.001 | |
| Education | |||
| <High School | 1 | ||
| High school | 2.36 (1.66–3.36) | <0.001 | |
| >High school | 2.12 (1.40–3.23) | <0.001 | |
| Material wealth index | |||
| Lowest | 1 | ||
| Middle | 1.00 (0.59–1.72) | 0.992 | |
| Highest | 1.89 (1.08–3.31) | 0.026 | |
| Tobacco use | |||
| Never user | 1 | ||
| Ever snuff users | 0.32 (0.10–1.04) | 0.059 | |
| Ever smokers | 0.68 (0.48–0.96) | 0.029 | |
| Nutritional status | |||
| (food security) | Poorest | 1 | |
| Middle | 1.65 (1.15–2.37) | 0.007 | |
| Highest | 2.43 (1.61–3.65) | <0.001 | |
| Privately insured | |||
| No | 1 | ||
| Yes | 4.32 (3.04–6.14) | <0.001 | |
| Characteristics | Odds Ratio (95% Confidence Interval) | p-value | |
|---|---|---|---|
| Race | |||
| Black African | 1 | ||
| Coloured | 0.80 (0.42–1.53) | 0.505 | |
| Indian/Asian | 1.35 (0.79–2.32) | 0.276 | |
| White | 3.82 (2.21–6.60) | <0.001 | |
| Education | |||
| <High school | 1 | ||
| High school | 2.84 (1.89–4.26) | <0.001 | |
| >High school | 2.70 (1.71–4.27) | <0.001 | |
| Material wealth index | |||
| Lowest | 1 | ||
| Middle | 1.26 (0.49–3.21) | 0.633 | |
| Highest | 2.79 (1.12–6.97) | 0.028 | |
| Privately insured | |||
| No | 1 | ||
| Yes | 5.26 (3.55–7.80) | <0.001 | |
| Characteristics | Odd Ratio (95% Confidence Interval) | p-value | |
|---|---|---|---|
| Age | |||
| Per year increase | 1.02 (1.00–1.03) | 0.045 | |
| Nutritional status (food security) | |||
| Poorest | 1 | ||
| Middle | 5.22 (2.12–12.84) | <0.001 | |
| Highest | 16.48 (6.78–40.05) | <0.001 | |
| Privately insured | |||
| No | 1 | ||
| Yes | 4.64 (2.12–10.14) | <0.001 | |
| Tobacco use | |||
| Never | 1 | ||
| Ever snuff user | 0.35 (0.09–1.30) | 0.118 | |
| Ever smoker | 0.38 (0.14–1.02) | 0.056 | |
| Observed characteristics | Size of indirect effect relative to total effect (95% CI) | Predicted PDV among non-Whites * (compared to actual of 3.2%) |
|---|---|---|
| Health insurance | 40.3% (31.2–49.3) | 8.5% |
| Educational attainment | 27.8% (20.9–34.8) | 6.5% |
| Material wealth | 27.6% (21.3–33.9) | 6.2% |
| Nutritional status | 10.3% (6.9–13.6) | 4.2% |
| Location | 7.4% (3.1–11.6) | 3.9% |
| Domains combined | 55.9% (44.9–67.8) | 12.8% |
3. Discussion
4. Conclusions
Conflict of Interest
Acknowledgements
References
- Shisana, O.; Rehle, T.; Louw, J.; Zungu-Dirwayi, N.; Dana, P.; Rispel, L. Public perceptions on national health insurance: Moving towards universal health coverage in South Africa. S. Afr. Med. J. 2006, 96, 814–818. [Google Scholar]
- Coovadia, H.; Jewkes, R.; Barron, P.; Sanders, D.; McIntyre, D. The health and health system of South Africa: Historical roots of current public health challenges. Lancet 2009, 374, 817–834. [Google Scholar] [CrossRef]
- Gilson, L.; McIntyre, D. Post-apartheid challenges: Household access and use of health care in South Africa. Int. J. Health Serv. 2007, 37, 673–691. [Google Scholar] [CrossRef]
- Booysen, F.R. Urban-rural inequality in health care delivery in South Africa. Dev. S. Afr. 2003, 20, 659–673. [Google Scholar] [CrossRef]
- Shisana, O.; Louw, J. Financing healthcare in South Africa, new agenda. S. Afr. J. Soc. Econ. Pol. 2005, 17, 39–44. [Google Scholar]
- McIntyre, D.; Doherty, J.; Gilson, L. A tale of two visions: The changing fortunes of social health insurance in South Africa. Health Pol. Plann. 2003, 18, 47–58. [Google Scholar] [CrossRef]
- Benefits, Exclusions and imitations. Available online: http://www.medicalaid.co.za/MedicalAid/Benefitsexclusionsandlimitations.aspx (assessed on 24 December 2012).
- Council for Medical Schemes Prescribed Minimum Benefit (PMB) Review consultation document. Available online: http://www.medicalschemes.com/files/PMB%20Review/3rd_Draft_PMB_20090325.pdf (assessed on 24 December 2012).
- Andersen, R.M. Revisiting the behavioural model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Wang, H.; Norton, E.C.; Rozier, R.G. Effects of the statechildren’s healthinsuranceprogram on access to dental care and use of dental services. Health Serv. Res. 2007, 42, 1544–1563. [Google Scholar] [CrossRef]
- Pizarro, V.; Ferrer, M.; Domingo-Salvany, A.; Benach, J.; Borrell, C.; Pont, A.; Schiaffino, A.; Alamnza, J.; Tresserras, R.; Alonso, J. The utilization of dental care services according to health insurance coverage in Catalonia. Community Dent. Oral Epidemiol. 2009, 37, 78–84. [Google Scholar] [CrossRef]
- Veugelers, P.J.; Yip, A.M. Socioeconomic disparities in health care use: Does universal coverage reduce inequalities in health? J. Epidemiol. Community Health 2003, 57, 424–428. [Google Scholar] [CrossRef]
- Harkinson, B.N.; Cleaton-Jones, P.E. Analysis of attendance at Soweto dental clinics 1995–2002. SADJ 2004, 59, 147–149. [Google Scholar]
- Fisher, M.A.; Mascarenhas, A.K. Does Medicaid improve utilization of medical and dental services and health outcomes for Medicaid-eligible children in the United States? Community Dent. Oral Epidemiol. 2007, 35, 263–271. [Google Scholar] [CrossRef]
- Somokotra, T.; Detsomboonrat, P. Is there equity in oral healthcare utilization: Experience after achieving universal coverage? Community Dent. Oral Epidemiol. 2009, 37, 85–96. [Google Scholar] [CrossRef]
- Suraratdecha, C.; Saithanu, S.; Tangcharoensathien, V. Is universal coverage a solution for disparities in health care? Findings from low-income provinces of Thailand. Health Pol. 2005, 73, 272–284. [Google Scholar] [CrossRef]
- Brothwell, D.J.; Jutai, D.K.; Hawkins, R.J. An update of mechanical oral hygiene practices: Evidence-based recommendations for disease prevention. J. Can. Dent. Assoc. 1998, 64, 295–306. [Google Scholar]
- Peer, N.; Bradshaw, D.; Laubscher, R.; Steyn, K. Trends in adult tobacco use from two South African demographic and health surveys conducted in 1998 and 2003. S. Afr. Med. J. 2009, 99, 744–749. [Google Scholar]
- Galobardes, B.; Shaw, M.; Lawlor, D.A.; Lynch, J.W.; Davey, S.G. Indicators of socioeconomic position (Part 1). J. Epidemiol. Community Health 2006, 60, 7–12. [Google Scholar] [CrossRef]
- Muirhead, V.; Quinonez, C.; Figueiredo, R.; Locker, D. Oral health disparities and food insecurity in working poor Canadians. Community Dent. Oral Epidemiol. 2009, 37, 294–304. [Google Scholar] [CrossRef]
- Nel, J.H.; Steyn, N.P. Report on South African Food Consumption Studies Undertaken Amongst Different Population Groups (1983–2000): Average Intakes of Foods Most Commonly Consumed; Department of Health: Pretoria, South Africa, 2002; p. 16. [Google Scholar]
- South African Demographic and Health Survey 2003. Available online: http:/www.doh.gov.za/docs/misc/sadhs-f.html (accessed on 20 October 2012).
- Drilea, S.K.; Reid, B.C.; Li, C.-H.; Hyman, J.J.; Manski, R.J. Dental visits among smoking and non-smoking US adults in 2000. Am. J. Health Behav. 2005, 29, 462–471. [Google Scholar] [CrossRef]
- Merlo, J.; Yang, M.; Chaix, B.; Lynch, J.; Råstam, L.A. brief conceptual tutorial on multilevel analysis in social epidemiology: Linking the statistical concept of clustering to the idea of contextual phenomenon. J. Epidemiol. Community Health 2005, 59, 443–449. [Google Scholar] [CrossRef]
- Rossouw, L. Dentists, the oral health team, their numbers, distribution and income profiles in South Africa: 1995–2010. J. Dent. Assoc. S. Afr. 1996, 51, 247–260. [Google Scholar]
- Buis, M.L. Direct and indirect effects in a logit model. Stata J. 2010, 10, 11–29. [Google Scholar]
- Lopez, R.; Baelum, V. Factors associated with dental attendance among adolescents in Santiago, Chile. BMC Oral Health 2007, 7. [Google Scholar] [CrossRef]
- Watt, R.G. Emerging theories into the social determinants of health: Implications for oral health promotion. Community Dent. Oral Epidemiol. 2002, 30, 241–247. [Google Scholar] [CrossRef]
- Pegon-Machat, E.; Tubert-Jeann, S.; Loignon, C.; Landry, A.; Bedos, C. Dentists’ experience with low-income patients benefitting from a public insurance program. Eur. J. Oral Sci. 2009, 117, 398–406. [Google Scholar] [CrossRef]
- Mickenautch, S.; van’t Hof, M.A.; Frencken, J.E. Oral health service systems in Gauteng Province, South Africa. East. Afr. Med. J. 2007, 84, 178–182. [Google Scholar]
- Doty, H.E.; Weech-Maldonado, R. Racial/ethnic disparities in adult preventive dental care use. JHCPU 2003, 14, 516–534. [Google Scholar]
- Scheppers, E.; van Dongen, E.; Dekker, J.; Geertzen, J.; Dekker, J. Potential barriers to the use of health services among ethnic minorities: A review. Fam. Pract. 2006, 23, 325–348. [Google Scholar] [CrossRef]
- Rosen, M. Dental treatment: Utilisation, motivation and prevention. A behavioural study of why people seek dental care. J. Dent. Assoc. S. Afr. 1990, 45, 319–321. [Google Scholar]
- Van Wyk, C.; van Wyk, P.J. Trends in dental caries prevalence, severity and unmet treatment need levels in South Africa between 1983 and 2002. SADJ 2010, 65, 312–314. [Google Scholar]
- Friedling, L.J.; Morris, A.G. The frequency of culturally derived dental modification practices on the Cape Flats in the Western Cape. SADJ 2005, 60, 99–102. [Google Scholar]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Ayo-Yusuf, I.J.; Ayo-Yusuf, O.A.; Olutola, B.G. Health Insurance, Socio-Economic Position and Racial Disparities in Preventive Dental Visits in South Africa. Int. J. Environ. Res. Public Health 2013, 10, 178-191. https://doi.org/10.3390/ijerph10010178
Ayo-Yusuf IJ, Ayo-Yusuf OA, Olutola BG. Health Insurance, Socio-Economic Position and Racial Disparities in Preventive Dental Visits in South Africa. International Journal of Environmental Research and Public Health. 2013; 10(1):178-191. https://doi.org/10.3390/ijerph10010178
Chicago/Turabian StyleAyo-Yusuf, Imade J., Olalekan A. Ayo-Yusuf, and Bukola G. Olutola. 2013. "Health Insurance, Socio-Economic Position and Racial Disparities in Preventive Dental Visits in South Africa" International Journal of Environmental Research and Public Health 10, no. 1: 178-191. https://doi.org/10.3390/ijerph10010178
APA StyleAyo-Yusuf, I. J., Ayo-Yusuf, O. A., & Olutola, B. G. (2013). Health Insurance, Socio-Economic Position and Racial Disparities in Preventive Dental Visits in South Africa. International Journal of Environmental Research and Public Health, 10(1), 178-191. https://doi.org/10.3390/ijerph10010178