Field Survey of Health Perception and Complaints of Pennsylvania Residents in the Marcellus Shale Region
Abstract
:1. Introduction
2. Methods
| Symptom | |
|---|---|
| Rashes/skin irritation | Chest pain/tightness |
| Hair loss | Palpitations |
| Irritated eyes | Dizziness |
| Headaches | Trembling of hands |
| Muscle aches | Balance difficulty |
| Joint pain | Numbness/tingling/burning in hands/feet |
| Dental problems | Blood in stool |
| Bleeding from gums | Diarrhea |
| Nosebleeds | Vomiting or nausea |
| Burning of the nose and throat | Abdominal pain |
| Ringing in ear | Blood in urine |
| Frequent sinus problems | Anxiety |
| Ear pain | Sadness |
| Wheezing | Sleep difficulties |
| Shortness of breath | |
| Natural Gas Activity | Antibiotics in Food | Aging from Free Radicals | High Tension Power lines | Living Near Highways | Other Causes | |
|---|---|---|---|---|---|---|
| N | 16 | 11 | 6 | 2 | 1 | 20 |
| % | 28.6 | 19.6 | 10.7 | 3.6 | 1.8 | 35.7 |
3. Results
3.1. Perceptions of Causation
| Organ System | Symptom | Number of Positive Responses |
|---|---|---|
| Mental health | Sleeping difficulty | 2 |
| Anxiety | 1 | |
| Head, ears, throat | Ringing in ear(s) | 1 |
| Sinus problems/infection | 2 | |
| Headaches | 1 | |
| Neurological | Balance difficulty | 1 |
| Trembling of hands | 1 | |
| Tingling of hands and feet | 1 | |
| Dizziness | 1 | |
| Seizures | 1 | |
| Gastro-intestinal | Nausea | 2 |
| Vomiting | 1 | |
| Diarrhea | 1 | |
| Stomach pain | 1 | |
| Cardiovascular | Palpitations | 1 |
3.2. Medical Record Review
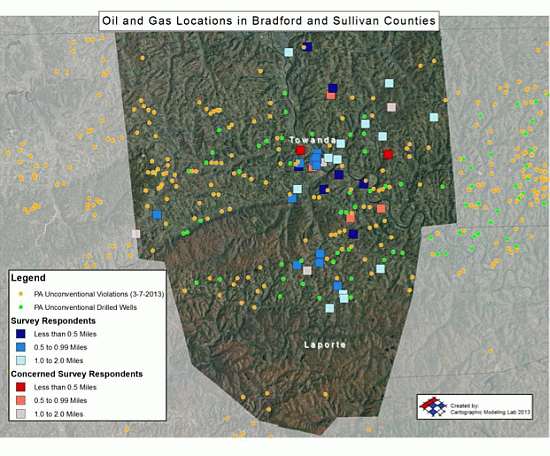
3.3. Mapping
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Howarth, R.W.; Ingraffea, A.; Engelder, T. Natural gas: Should fracking stop? Nature 2011, 477, 271–275. [Google Scholar] [CrossRef]
- Jackson, R.B.; Vengosha, A.; Darraha, T.H.; Warnera, N.R. Increased stray gas abundance in a subset of drinking water wells near Marcellus shale gas extraction. Proc. Natl. Acad. Sci. 2013, 110, 11250–11255. [Google Scholar]
- Boyer, E.W.; Swistock, B.R.; Clark, J.; Madden, M.; Rizzo, D.E. The Impact of Marcellus Gas Drilling on Rural Drinking Water Supplies. Available online: http://www.marcellus.psu.edu/resources/PDFs/swistock_water.pdf (accessed on 27 January 2014).
- Pring, M.O.; Wilhelmi, J. Fort Worth Natural Gas Air Quality Study. Available online: http://www.epa.gov/ttnchie1/conference/ei20/session6/mpring.pdf (accessed 15 May 2014).
- McKenzie, L.M.; Witter, R.Z.; Newman, L.S.; Adgate, J.L. Human health risk assessment of air emissions from development of unconventional natural gas resources. Sci. Total Environ. 2012, 424, 79–87. [Google Scholar] [CrossRef]
- Paleontological Research Institute. Beyond Water: A Discussion of the Non-Water Related Environmental Issues Associated with Drilling for Natural Gas in the Marcellus Shale. Available online: http://www.museumoftheearth.org/files/marcellus/Marcellus_issue9.pdf (accessed on 27 January 2014).
- Pennsylvania Department of Environmental Protection Agency (PADEP), Sampling and Analysis Plan, Part 1–Field Sampling Plan. April 2013. Available online: http://files.dep.state.pa.us/OilGas/BOGM/BOGMPortalFiles/RadiationProtection/Sampling_and_Analysis_Plan-Part-I-Field_Sampling_Plan.pdf (accessed on 6 June 2014).
- Multi-State Shale Research Collaborative- Case Studies: Assesing the Costs and Benefits and Natural Gas Development. Available online: http://www.multistateshale.org/case-studies (accessed on 5 June 2014).
- Perry, S. It’s Like We’re Losing Our Love: Documenting and Evaluating Social Change in Bradford County, PA during the Marcellus Shale Gas Boom. In Proceedings of the 2nd Annual Health Effects of Shale Gas Extraction Conference, Pittsburgh, PA, USA, 18 November 2012.
- Pennsylvania Department of Environmental Protection. Marcellus Shale. Available online: http://www.portal.state.pa.us/portal/server.pt/community/marcellus_shale/20296 (accessed on 27 January 2014).
- Rebecca Roter. 575 Turnpike Road, Kingsley, PA 18826, USA. Email: [email protected].
- Rowan, E.L.; Engle, M.A.; Kirby, C.S.; Kraemer, T.F.U.S. Geological Survey: Radium Content of Oil- and Gas-Field Produced Waters in the Northern Appalachian Basin (USA)—Summary and Discussion of Data: U.S. Geological Survey Scientific Investigations Report 2011–5135. Available online: http://pubs.usgs.gov/sir/2011/5135/pdf/sir2011–5135.pdf (accessed on 27 January 2014).
- Agency for Toxic Substances and Disease Registry (ATSDR). Health Consultation: Chesapeake ATGAS 2H Well Site, Leroy Township, Bradford County, Pennsylvania. October 2013. Available online: http://www.atsdr.cdc.gov/HAC/pha/ChesapeakeATGASWellSite/ChesapeakeATGASWellSiteHC10282013_508.pdf (accessed on 6 June 2014).
- Phillips, S. A Link Between Heavy Drilling and Illness? Doctors Search for Solid Answers. Available online: http://stateimpact.npr.org/pennsylvania/2012/04/27/doctors-in-shale-country-search-for-answers-but-come-up-short/ (accessed on 27 January 2014).
- Witter, R.; McKenzie, L.; Towle, M.; Stinson, K.; Scott, K.; Newman, L.; Adgate, J. Health Impact Assessment for Battlement Mesa, Garfield County, Colorado. Available online: http://www.garfield-county.com/public-health/documents/1%20%20%20Complete%20HIA%20without%20Appendix%20D.pdf (accessed on 24 January 2014).
- Goldstein, B.D.; Kriesky, J.; Pavliakova, B. Missing from the table: Role of the environmental public health community in governmental advisory commissions related to Marcellus Shale drilling. Environ. Health Perspect. 2012, 120, 483–486. [Google Scholar] [CrossRef]
- Bamberger, M.; Oswald, R.E. Impacts of gas drilling on human and animal health. New Solut. 2012, 22, 51–77. [Google Scholar] [CrossRef]
- Ferrar, K.; Kriesky, J.; Christen, L.; Marshall, L.; Malone, S.; Sharma, R.; Michanowicz, D.; Goldstein, B.D. Assessment and longitudinal analysis of health impacts and stressors perceived to result from unconventional shale gas development in the Marcellus Shale region. Int. J. Occup. Environ. Med. 2013, 19, 104–112. [Google Scholar] [CrossRef]
- Research Electronic Data Capture (REDCap) Hosted at University of Pennsylvania. Available online: http://www.project-redcap.org/cite.php (accessed on 31 March 2014).
- StataCorp. 2013. In Stata Statistical Software: Release 13; StataCorp LP: College Station, TX, USA.
- ESRI 2013. In ArcGIS Desktop: Release 10.2; Environmental Systems Research Institute: Redlands, CA, USA.
- Unconventional Oil and Gas Permits, Drilled Wells, Violations, Pits, and Compressor Stations in Pennsylvania. Available online: http://www.arcgis.com/home/item.html?id=4edd854fdda74ed7bf4709034a4dad24 (accessed 27 January 2014).
- Schreier, N.; Huss, A.; Röösli, M. The prevalence of symptoms attributed to electromagnetic field exposure: A cross-sectional representative survey in Switzerland. Soz. Praventivmed. 2006, 51, 202–209. [Google Scholar] [CrossRef]
- Vrijheid, M. Health effects of residence near hazardous waste landfill sites: A review of epidemiologic literature. Environ. Health Perspect. 2000, 108, 101–112. [Google Scholar]
- Steinzor, N.; Subra, W.; Sumi, L. Investigating links between Shale gas development and health impacts through a community survey project in Pennsylvania. New Solut. 2013, 23, 55–83. [Google Scholar] [CrossRef]
- Colburn, T.; Kwiatkowski, C.; Schultz, K.; Bachran, M. Natural gas operations from a public health perspective. Hum. Ecol. Risk Assess. 2011, 17, 1039–1056. [Google Scholar] [CrossRef]
- Resick, L.K.; Knestrick, J.M.; Counts, M.M.; Pizzuto, L.K. The meaning of health among mid-Appalachian women within the context of the environment. J. Environ. Stud. Sci. 2013, 3, 290–296. [Google Scholar] [CrossRef]
- Merkel, L.; Bicking, C.; Sekhar, D. Parents’ perceptions of water safety and quality. J. Commun. Health 2012, 37, 195–201. [Google Scholar] [CrossRef]
- Ha, J.F.; Longnecker, N. Doctor-patient communication: A review. Ochsner J. 2010, 10, 38–43. [Google Scholar]
- Pakhomov, S.V.; Jacobsen, S.J.; Chute, C.G.; Roger, V.L. Agreement between patient-reported symptoms and their documentation in the medical record. Am. J. Manag. Care 2008, 14, 530–539. [Google Scholar]
- Sikorskii, A.; Wyatt, G.; Tamkus, D.; Victorson, D.; Rahbar, M.H.; Ahn, S. Concordance between patient reports of cancer-related symptoms and medical records documentation. J. Pain Symptom Manag. 2012, 44, 362–372. [Google Scholar] [CrossRef]
- Concerned Health Professionals of NY. Call for a Comprehensive Health Impact Assessment. Available online: http://concernedhealthny.org/call-for-a-comprehensive-health-impact-assessment/ (accessed on 5 June 2014).
- Pennsylvania Department of Health. Available online: http://www.health.state.pa.us/ (accessed on 4 June 2014).
- Lustgarten, A.; Kusnetz, N. Science Lags as Health Problems Emerge Near Gas Fields. Available online: http://www.propublica.org/article/science-lags-as-health-problems-emerge-near-gas-fields (accessed on 4 June 2014).
- Saberi, P. Navigating medical issues in Shale territory. New Solut. 2013, 23, 209–221. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Saberi, P.; Propert, K.J.; Powers, M.; Emmett, E.; Green-McKenzie, J. Field Survey of Health Perception and Complaints of Pennsylvania Residents in the Marcellus Shale Region. Int. J. Environ. Res. Public Health 2014, 11, 6517-6527. https://doi.org/10.3390/ijerph110606517
Saberi P, Propert KJ, Powers M, Emmett E, Green-McKenzie J. Field Survey of Health Perception and Complaints of Pennsylvania Residents in the Marcellus Shale Region. International Journal of Environmental Research and Public Health. 2014; 11(6):6517-6527. https://doi.org/10.3390/ijerph110606517
Chicago/Turabian StyleSaberi, Pouné, Kathleen Joy Propert, Martha Powers, Edward Emmett, and Judith Green-McKenzie. 2014. "Field Survey of Health Perception and Complaints of Pennsylvania Residents in the Marcellus Shale Region" International Journal of Environmental Research and Public Health 11, no. 6: 6517-6527. https://doi.org/10.3390/ijerph110606517
APA StyleSaberi, P., Propert, K. J., Powers, M., Emmett, E., & Green-McKenzie, J. (2014). Field Survey of Health Perception and Complaints of Pennsylvania Residents in the Marcellus Shale Region. International Journal of Environmental Research and Public Health, 11(6), 6517-6527. https://doi.org/10.3390/ijerph110606517