The Communication, Awareness, Relationships and Empowerment (C.A.R.E.) Model: An Effective Tool for Engaging Urban Communities in Community-Based Participatory Research
Abstract
:1. Introduction
2. Materials and Methods
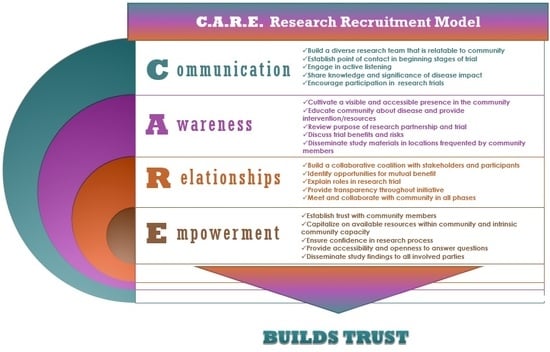
2.1. Using the C.A.R.E. Model
2.2. Communication
2.3. Awareness
2.4. Relationships
2.4.1. Church Partnerships
2.4.2. Community Partnerships—Community Advisory Board
2.5. Empowerment
2.5.1. Study Design and Implementation in Collaboration with CAB
2.5.2. Mobile Health Technology
3. Results
4. Discussion
4.1. The C.A.R.E. Model Addresses Difficulty with Recruitment and Retention
4.2. Implementation of C.A.R.E. Model May Be Especially Helpful When Launching Use of mHealth Technology
4.3. Consideration of C.A.R.E. Model Employment in Future CBPR-Based Interventions
4.4. Limitations
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Go, A.S.; Mozaffarian, D.; Roger, V.L. Heart disease and stroke statistics—2013 update: A report from the American Heart Association. Circulation 2013, 27, e6–e245. [Google Scholar] [CrossRef] [PubMed]
- De Berrington, G.A.; Hartge, P.; Cerhan, J.R.; Flint, A.J.; Hannan, L.; MacInnis, R.J.; Moore, S.C.; Tobias, G.S.; Anton-Culver, H.; Freeman, L.B.; et al. Body-mass index and mortality among 1.46 million white adults. N. Engl. J. Med. 2010, 363, 2211–2219. [Google Scholar] [CrossRef] [PubMed]
- Boggs, D.A.; Rosenberg, L.; Cozier, Y.C. General and abdominal obesity and risk of death among black women. N. Engl. J. Med. 2011, 365, 901–908. [Google Scholar] [CrossRef] [PubMed]
- Bibbins-Domingo, K.; Coxson, P.; Pletcher, M.J.; Lightwood, J.; Goldman, L. Adolescent overweight and future adult coronary heart disease. N. Engl. J. Med. 2007, 357, 2371–2379. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American heart association’s strategic impact goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef] [PubMed]
- Artinian, N.T.; Fletcher, G.F.; Mozaffarian, D. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: A scientific statement from the American heart association. Circulation 2010, 122, 406–441. [Google Scholar] [CrossRef] [PubMed]
- Poirier, P.; Giles, T.D.; Bray, G.A. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss. Arterioscler Thromb. Vasc. Biol. 2006, 26, 968–976. [Google Scholar] [CrossRef] [PubMed]
- Skolarus, L.E.; Cowdery, J.; Dome, M. Reach out churches: A community-based participatory research pilot trial to assess the feasibility of a mobile health technology intervention to reduce blood pressure among African Americans. Health Promot Pract. 2017. [CrossRef] [PubMed]
- Greiner, K.A.; Daniela, B.F.; Swann, A.A.; Clement, K.G.; Paula, C.; Kimberly, K.; Engelman, C.D.; Meader, J.R.H. Effective recruitment strategies and community-based participatory research: Community networks program centers’ recruitment in cancer prevention studies. Cancer Epidemiol. Biomarkers Prev. 2014, 23, 416–423. [Google Scholar] [CrossRef] [PubMed]
- Salimi, Y.; Shahandeh, K.; Malekafzali, H. Is Community-based participatory research (CBPR) useful? A systematic review on papers in a decade. Int. J. Prev. Med. 2012, 3, 386–393. [Google Scholar] [PubMed]
- Wallen, G.R.; Saygbe, J.N.; Brooks, A.T.; McClurkin, M.; Thomas, S.; Powell-Wiley, T.M. Engaging community leaders in the development of a cardiovascular health behavior survey using focus group-based cognitive interviewing. Health Serv. Insights 2017. [CrossRef] [PubMed]
- Ralston, P.A.; Young-Clark, I.; Coccia, C. The development of health for hearts united: A longitudinal church-based intervention to reduce cardiovascular risk in mid-life and older African Americans. Ethn. Dis. 2017, 27, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Yingling, L.R.; Brooks, A.T.; Wallen, G.R. Community engagement to optimize the use of web-based and wearable technology in a cardiovascular health and needs assessment study: A mixed methods approach. JMIR mHealth uHealth 2016, 4, e38. [Google Scholar] [CrossRef] [PubMed]
- Yingling, L.R.; Mitchell, V.; Ayers, C.R. Adherence with physical activity monitoring wearable devices in a community-based population: Observations from the Washington, D.C., cardiovzascular health and needs assessment. Transl. Behav. Med. 2017, 7, 719–730. [Google Scholar] [CrossRef] [PubMed]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Review of community-based research: Assessing partnership approaches to improve public health. Annu. Rev. Public Health 1998, 19, 173–202. [Google Scholar] [CrossRef] [PubMed]
- Gamble, V.N. Under the shadow of Tuskegee: African Americans and health care. Am. J. Public Health 1997, 87, 1773–1778. [Google Scholar] [CrossRef] [PubMed]
- Darcell, P.S.; Katherine, J.M.; Pamela, J.; Jonathan, H.; Emeobong, M.; Dorothy, E. More than Tuskegee: Understanding mistrust about research participation. J. Health Care Poor Underserved 2010, 21, 879–897. [Google Scholar] [CrossRef] [PubMed]
- George, S.; Duran, N.; Norris, K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans and Pacific Islanders. Am. J. Public Health 2014, 104, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.K.; Hudson, M.A.; Resnicow, K.; Blakeney, N.; Paxton, A.; Baskin, M. Church-based health promotion interventions: Evidence and lessons learned. Annu. Rev. Public Health 2007, 28, 213–234. [Google Scholar] [CrossRef] [PubMed]
- Martin, T. Assessing mHealth: Opportunities and barriers to patient engagement. J. Health Care Poor Underserved 2012, 23, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, V.; Johnson, E.; Gonzalez, C.; Ramirez, V.; Rubino, B.; Rossetti, G. Assessing the use of mobile health technology by patients: An observational study in primary care clinics. JMIR mHealth uHealth 2016, 4, e41. [Google Scholar] [CrossRef] [PubMed]
- Nebeker, C.; Murray, K.; Holub, C.; Haughton, J.; Arredondo, E.M. Acceptance of mobile health in communities underrepresented in biomedical research: Barriers and ethical considerations for scientists. JMIR mHealth uHealth 2017, 5, e87. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, S.; Hanlon, P.; O’Donnell, C.A.; Garcia, S.; Glanville, J.; Mair, F.S. Understanding factors affecting patient and public engagement and recruitment to digital health interventions: A systematic review of qualitative studies. BMC Med. Inform. Decis. Mak. 2016, 16, 120. [Google Scholar] [CrossRef] [PubMed]
- Lorenda, B.; Lucero, J.E.; Duran, B.; Tafoya, G.; Baker, E.A.; Chan, D.; Chang, C.; Green-Moton, E.; Kelley, M.; Wallerstein, N. Community-based participatory research conceptual model: Community partner consultation and face validity. Qual. Health Res. 2016, 26, 117–135. [Google Scholar]
- Jones, R.A.; Steeves, R.; Williams, I. Strategies for recruiting African American men into prostate cancer screening studies. Nurs. Res. 2009, 58, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Unertl, K.M.; Schaefbauer, C.L.; Campbell, T.R. Integrating community-based participatory research and informatics approaches to improve the engagement and health of underserved populations. J. Am. Med. Inform. Assoc. 2016, 23, 60–73. [Google Scholar] [CrossRef] [PubMed]


| Communication, Awareness, Relationship, Empowerment (C.A.R.E.) in Action: Recruitment Strategies | ||
|---|---|---|
| Communication | Outreach | Participants recruited at community events such as:
|
| Awareness | Referrals (word of mouth and community partners) | Participants referred to the study by:
|
| Relationships | Churches | Participants recruited via:
|
| Empowerment | NIH Website | Participants searched independently and discovered the study from the Healthy volunteer opportunity posted on the NIH Website. |
| Participant Involvement and Engagement | Communication | Awareness | Relationships | Empowerment |
|---|---|---|---|---|
| Initial Involvement |
|
|
|
|
| Maintaining Engagement |
|
|
|
|
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceasar, J.; Peters-Lawrence, M.H.; Mitchell, V.; Powell-Wiley, T.M. The Communication, Awareness, Relationships and Empowerment (C.A.R.E.) Model: An Effective Tool for Engaging Urban Communities in Community-Based Participatory Research. Int. J. Environ. Res. Public Health 2017, 14, 1422. https://doi.org/10.3390/ijerph14111422
Ceasar J, Peters-Lawrence MH, Mitchell V, Powell-Wiley TM. The Communication, Awareness, Relationships and Empowerment (C.A.R.E.) Model: An Effective Tool for Engaging Urban Communities in Community-Based Participatory Research. International Journal of Environmental Research and Public Health. 2017; 14(11):1422. https://doi.org/10.3390/ijerph14111422
Chicago/Turabian StyleCeasar, Joniqua, Marlene H. Peters-Lawrence, Valerie Mitchell, and Tiffany M. Powell-Wiley. 2017. "The Communication, Awareness, Relationships and Empowerment (C.A.R.E.) Model: An Effective Tool for Engaging Urban Communities in Community-Based Participatory Research" International Journal of Environmental Research and Public Health 14, no. 11: 1422. https://doi.org/10.3390/ijerph14111422
APA StyleCeasar, J., Peters-Lawrence, M. H., Mitchell, V., & Powell-Wiley, T. M. (2017). The Communication, Awareness, Relationships and Empowerment (C.A.R.E.) Model: An Effective Tool for Engaging Urban Communities in Community-Based Participatory Research. International Journal of Environmental Research and Public Health, 14(11), 1422. https://doi.org/10.3390/ijerph14111422