Network Analysis: A Novel Approach to Understand Suicidal Behaviour
Abstract
:1. Introduction
1.1. The Complexity of Suicidal Behaviour
1.2. A Network Approach to Psychopathology
2. Application of Network Analysis within the Field of Suicide Prevention
2.1. Validating Complex Explanatory Models of Suicidal Behaviour
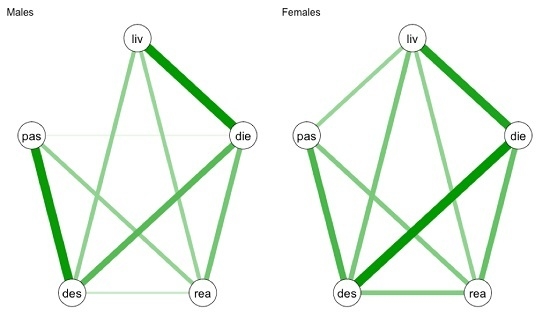
2.2. Understanding the Differences between Subgroups of Patients
2.3. Personalized Treatment Using Networks Based on Individual Data
3. Discussion
3.1. Social Networks and Suicidal Behaviour
3.2. Future Studies
4. Conclusions
Acknowledgments
Conflicts of Interest
References
- World Health Organization Public Health Action for the Prevention of Suicide. WHO, 2012. Available online: http://www.who.int/m (accessed on 12 December 2016).
- Oyesanya, M.; Lopez-Morinigo, J.; Dutta, R. Systematic review of suicide in economic recession. World J. Psychiatry 2015, 5, 243–254. [Google Scholar] [PubMed]
- Hawton, K.; van Heeringen, K. Suicide. Lancet 2009, 373, 1372–1381. [Google Scholar] [CrossRef]
- O’Connor, R.C.; Nock, M.K. The psychology of suicidal behaviour. Lancet Psychiatry 2014, 1, 73–85. [Google Scholar] [CrossRef]
- O’connor, R.C. Towards an Integrated Motivational-Volitional Model of Suicidal Behaviour. In International Handbook of Suicide Prevention: Research, Policy and Practice; Wiley-Blackwell: Hoboken, NJ, USA, 2011; pp. 181–198. [Google Scholar]
- O’Connor, R.C.; Smyth, R.; Williams, J.M.G. Intrapersonal positive future thinking predicts repeat suicide attempts in hospital-treated suicide attempters. J. Consult. Clin. Psychol. 2015, 83, 169–176. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, R.C.; Rasmussen, S.; Hawton, K. Distinguishing adolescents who think about self-harm from those who engage in self-harm. Br. J. Psychiatry 2012, 200, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Borsboom, D.; Cramer, A.O.J. Network Analysis: An Integrative Approach to the Structure of Psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef] [PubMed]
- Fried, E.I.; van Borkulo, C.D.; Cramer, A.O.J.; Boschloo, L.; Schoevers, R.A.; Borsboom, D. Mental disorders as networks of problems: A review of recent insights. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 58, 7250–7257. [Google Scholar] [CrossRef] [PubMed]
- Oquendo, M.A.; Baca-Garcia, E. Suicidal behavior disorder as a diagnostic entity in the DSM-5 classification system: Advantages outweigh limitations. World Psychiatry 2014, 13, 128–130. [Google Scholar] [CrossRef] [PubMed]
- Epskamp, S.; Cramer, A.O.J.; Waldrop, L.J.; Schmittmann, V.D.; Borsboom, D. Qgraph: Network visualizations of relationships in psychometric data. J. Stat. Soft. 2012, 48, 1–18. [Google Scholar] [CrossRef]
- Costantini, G.; Epskamp, S.; Borsboom, D.; Perugini, M.; Mõttus, R.; Waldorp, L.J.; Cramer, A.O.J. State of the aRt personality research: A tutorial on network analysis of personality data in R. J. Res. Personal. 2015, 54, 13–29. [Google Scholar] [CrossRef]
- Van Borkulo, C.D.; Borsboom, D.; Epskamp, S.; Blanken, T.F.; Boschloo, L.; Schoevers, R.A.; Waldorp, L.J. A new method for constructing networks from binary data. Sci. Rep. 2014, 4, 5918. [Google Scholar] [CrossRef] [PubMed]
- Epskamp, S.; Rhemtulla, M.; Borsboom, D. Generalized Network Psychometrics: Combining Network and Latent Variable Models. arXiv:1605.09288.
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating Psychological Networks and their Stability: A Tutorial Paper. arXiv:1604.08462.
- De Beurs, D.P.; Hooiveld, M.; Kerkhof, A.J.F.M.; Korevaar, J.C.; Donker, G.A. Trends in suicidal behaviour in Dutch general practice 1983–2013: A retrospective observational study. BMJ Open 2016, 6, e010868. [Google Scholar] [CrossRef] [PubMed]
- Fried, E.I.; Nesse, R.M.; Zivin, K.; Guille, C.; Sen, S. Depression is more than the sum score of its parts: Individual DSM symptoms have different risk factors. Psychol. Med. 2013, 44, 2067–2076. [Google Scholar] [CrossRef] [PubMed]
- De Beurs, D.P.; de Groot, M.H.; de Keijser, J.; van Duijn, E.; de Winter, R.F.P.; Kerkhof, A.J.F.M. Evaluation of benefit to patients of training mental health professionals in suicide guidelines: Cluster randomised trial. Br. J. Psychiatry 2015, 208, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Dhingra, K.; Boduszek, D.; O’Connor, R.C. A structural test of the Integrated Motivational-Volitional model of suicidal behaviour. Psychiatry Res. 2016, 239, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Van Borkulo, C.; Boschloo, L.; Borsboom, D.; Penninx, B.W.J.H.; Waldorp, L.J.; Schoevers, R.A. Association of Symptom Network Structure with the Course of Longitudinal Depression. JAMA Psychiatry 2015, 72, 1219–1226. [Google Scholar] [CrossRef] [PubMed]
- R package Network Comparison Test. Available online: https://cran.r-project.org/web/packages/NetworkComparisonTest/NetworkComparisonTest.pdf (accessed on 12 December 2016).
- De Beurs, D.; Kirtley, O.; Kerkhof, A.; Portzky, G.; O’Connor, R.C. The role of mobile phone technology in understanding and preventing suicidal behavior. Crisis J. Crisis Interv. Suicide Prev. 2015, 36, 79–82. [Google Scholar] [CrossRef]
- Bak, M.; Drukker, M.; Hasmi, L.; Van Jim, O.S. An n=1 Clinical network analysis of symptoms and treatment in psychosis. PLoS ONE 2016, 11, e0162811. [Google Scholar]
- Isvoranu, A.M.; van Borkulo, C.D.; Boyette, L.L.; Wigman, J.T.W.; Vinkers, C.H.; Borsboom, D. A Network Approach to Psychosis: Pathways between Childhood Trauma and Psychotic Symptoms. Schizophr. Bull. 2016, 43, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Pescosolido, B.A.; Georgianna, S. Durkheim, Suicide, and Religion: Toward a Network Theory of Suicide. Am. Sociol. Rev. 1989, 54, 33–48. [Google Scholar] [CrossRef] [PubMed]
- Stack, S. Suicide: A 15 Year Review of the Sociological Literature: Part II: Modernization and Social Integration Perspectives. Suicide Life Threat. Behav. 2000, 30, 163–176. [Google Scholar] [PubMed]
- Penninx, B.W.J.H.; Beekman, A.T.F.; Smit, J.H.; Zitman, F.G.; Nolen, W.A.; Spinhoven, P.; Cuijpers, P.; De Jong, P.J.; Van Marwijk, H.W.J.; Assendelft, W.J.J.; et al. The Netherlands Study of Depression and Anxiety (NESDA): Rationale, objectives and methods. Int. J. Methods Psychiatr. Res. 2008, 17, 121–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vancayseele, N.; Portzky, G.; Van Heeringen, K. Increase in self-injury as a method of self-harm in Ghent, Belgium: 1987–2013. PLoS ONE 2016, 11, e0156711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terluin, B.; De Boer, M.R.; De Vet, H.C.W. Differences in connection strength between mental symptoms might be explained by differences in variance: Reanalysis of network data did not confirm staging. PLoS ONE 2016, 11, e0155205. [Google Scholar] [CrossRef] [PubMed]
- Chekroud, A.M.; Zotti, R.J.; Shehzad, Z.; Gueorguieva, R.; Johnson, M.K.; Trivedi, M.H.; Cannon, T.D.; Krystal, J.H.; Corlett, P.R. Cross-trial prediction of treatment outcome in depression: A machine learning approach. Lancet Psychiatry 2016, 3, 243–250. [Google Scholar] [CrossRef]



© 2017 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Beurs, D. Network Analysis: A Novel Approach to Understand Suicidal Behaviour. Int. J. Environ. Res. Public Health 2017, 14, 219. https://doi.org/10.3390/ijerph14030219
De Beurs D. Network Analysis: A Novel Approach to Understand Suicidal Behaviour. International Journal of Environmental Research and Public Health. 2017; 14(3):219. https://doi.org/10.3390/ijerph14030219
Chicago/Turabian StyleDe Beurs, Derek. 2017. "Network Analysis: A Novel Approach to Understand Suicidal Behaviour" International Journal of Environmental Research and Public Health 14, no. 3: 219. https://doi.org/10.3390/ijerph14030219
APA StyleDe Beurs, D. (2017). Network Analysis: A Novel Approach to Understand Suicidal Behaviour. International Journal of Environmental Research and Public Health, 14(3), 219. https://doi.org/10.3390/ijerph14030219