A Comparative Study of the Physiological and Socio-Economic Vulnerabilities to Heat Waves of the Population of the Metropolis of Lyon (France) in a Climate Change Context
Abstract
:1. Introduction
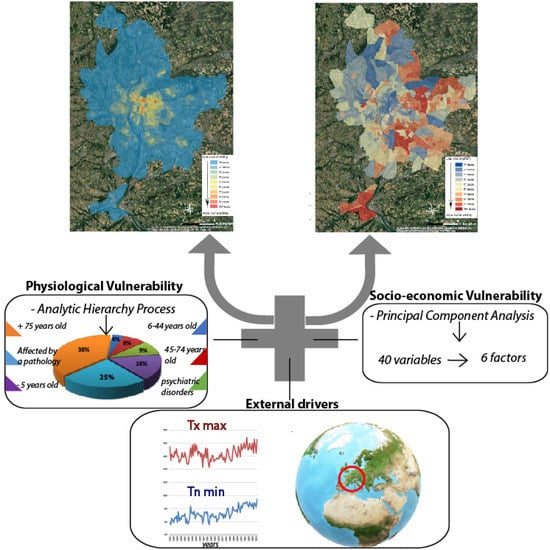
2. Vulnerabilities: Differences in Approaches and Concepts Applied to the Greater Lyon Area
2.1. Physiological Vulnerability
2.2. Socio-Economic Vulnerability
2.3. Study Area: the Metropolis of the Greater Lyon Area
3. Methodologies
3.1. The Application of AHP to Assess Physiological Vulnerability
- detailed description of the 8 vulnerability factors of the population to characterize, synthesize and decompose the complex situation;
- series of semi-directed interviews with the expert panel where they make binary comparisons of vulnerability factors they appear to have a higher vulnerability to heat waves than other experts.
- validation of the consistency of the experts’ responses and calculation of the weighting of vulnerability factors
- aggregation of responses and calculation of physiological vulnerability to heat waves
3.2. Treatment of Socio-Economic Vulnerability Using PCA
3.2.1. Initial Statistical Tests and Realization of PCA with Varimax Rotation
3.2.2. The weighting of the Final Variables Selected
4. Results
4.1. The Physiological Vulnerability
4.2. The Socio-Economic Vulnerability
- Factor No. 1 groups together variables representative of the socio-economic defaults of the metropolis: people with low-skilled jobs, people without higher education, people with higher education, unemployment rate, percentage of social housing, average annual household wage, percentage of children under 5 years old and poverty rate.
- Factor No. 2 tends to include characteristics of physical defaults with the number of persons undergoing psychotropic drug treatment per capita, the percentage of persons receiving the disabled adult allowance and the percentage of the population who died before the age of 65, supplemented by the number of births per capita.
- Factor No. 3 highlights the vulnerability of the elderly with the variables relating to the percentage of retired persons and the percentage of persons aged 65 and over and the percentage of persons without a diploma.
- Factor No. 4 is considered an indicator of territorial development since it includes the mortality rate, the distance from the nearest home to the nearest hospital, and the number of beds available per hospital.
- Factor No. 5 focuses on the vulnerability of the female population by grouping together the percentage of women in the total population of metropolitan Lyon and the percentage of working women.
- Finally, the last factor gathers the health-related variables, with the number of medical professions per inhabitant and the number of health establishments (public or private) per inhabitant.
5. Discussion
5.1. A Global Socio-Economic Vulnerability to Be Enhanced Using the Factors
5.2. Physiological and Socioeconomic Vulnerabilities That Are Spatially very Divergent
5.3. A Perception of Physiological Vulnerability That Differs According to the Training of Experts
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jouzel, J. Scénarios régionalisés. In Le climat de la France au XXIe Siècle, 2014 ed.; pour la métropole et les régions d’outre-mer; Ministère de l’Ecologie, du Développement durable et de l’Energie: Paris, France, 2014; Volume 4. [Google Scholar]
- Stocker, T.F.; Intergovernmental Panel on Climate Change (Eds.) Climate Change 2013: The Physical Science Basis; Summary, a Report of Working Group I of the IPCC; Intergovernmental Panel on Climate Change: New York, NY, USA, 2013; ISBN 978-92-9169-138-8. [Google Scholar]
- Hartmann, D.L.; Tank, A.M.G.K.; Rusticucci, M. Climatie Change 2013: Observations: Atmosphere and Surface; IPCC Fifth Assessment Report; Intergovernmental Panel on Climate Change: New York, NY, USA, 2013; pp. 31–39. [Google Scholar]
- Meehl, G.A.; Tebaldi, C. More Intense, More Frequent, and Longer Lasting Heat Waves in the 21st Century. Science 2004, 305, 994–997. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beniston, M. The 2003 heat wave in Europe: A shape of things to come? An analysis based on Swiss climatological data and model simulations. Geophys. Res. Lett. 2004, 31. [Google Scholar] [CrossRef] [Green Version]
- Schär, C.; Vidale, P.L.; Lüthi, D.; Frei, C.; Häberli, C.; Liniger, M.A.; Appenzeller, C. The role of increasing temperature variability in European summer heatwaves. Nature 2004, 427, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Golden, J.S. The Built Environment Induced Urban Heat Island Effect in Rapidly Urbanizing Arid Regions—A Sustainable Urban Engineering Complexity. Environ. Sci. 2004, 1, 321–349. [Google Scholar] [CrossRef]
- Kosaka, E.; Iida, A.; Vanos, J.; Middel, A.; Yokohari, M.; Brown, R. Microclimate Variation and Estimated Heat Stress of Runners in the 2020 Tokyo Olympic Marathon. Atmosphere 2018, 9, 192. [Google Scholar] [CrossRef] [Green Version]
- Oke, T. City Size and the Urban Heat Island. Atmos. Env. 1973, 7, 769–779. [Google Scholar] [CrossRef]
- Oke, T.R. Boundary Layer Climates, Londres. GPQ 1978, 32, 290–291. [Google Scholar]
- Patz, J.A.; Campbell-Lendrum, D.; Holloway, T.; Foley, J.A. Impact of regional climate change on human health. Nature 2005, 438, 310–317. [Google Scholar] [CrossRef]
- Tan, J.; Zheng, Y.; Tang, X.; Guo, C.; Li, L.; Song, G.; Zhen, X.; Yuan, D.; Kalkstein, A.J.; Li, F.; et al. The urban heat island and its impact on heat waves and human health in Shanghai. Int. J. Biometeorol. 2010, 54, 75–84. [Google Scholar] [CrossRef]
- Bobb, J.F.; Peng, R.D.; Bell, M.L.; Dominici, F. Heat-Related Mortality and Adaptation to Heat in the United States. Env. Health Perspect. 2014, 122, 811–816. [Google Scholar] [CrossRef]
- Besancenot, J.-P. Heat waves and mortality in large urban areas. Env. Risques Sante 2002, 1, 229–240. [Google Scholar]
- Gabriel, K.M.A.; Endlicher, W.R. Urban and rural mortality rates during heat waves in Berlin and Brandenburg, Germany. Env. Pollut. 2011, 159, 2044–2050. [Google Scholar] [CrossRef] [PubMed]
- Jenerette, G.D.; Harlan, S.L.; Buyantuev, A.; Stefanov, W.L.; Declet-Barreto, J.; Ruddell, B.L.; Myint, S.W.; Kaplan, S.; Li, X. Micro-scale urban surface temperatures are related to land-cover features and residential heat related health impacts in Phoenix, AZ USA. Landsc. Ecol. 2016, 31, 745–760. [Google Scholar] [CrossRef]
- Barreca, A.; Clay, K.; Deschenes, O.; Greenstone, M.; Shapiro, J.S. Adapting to Climate Change: The Remarkable Decline in the US Temperature-Mortality Relationship over the Twentieth Century. J. Political Econ. 2016, 124, 105–159. [Google Scholar] [CrossRef] [Green Version]
- Hajat, S.; Kosatky, T. Heat-related mortality: A review and exploration of heterogeneity. J. Epidemiol. Community Health 2010, 64, 753–760. [Google Scholar] [CrossRef]
- Kosatsky, T. The 2003 European heat waves. Eurosurveillance 2005, 10, 3–4. [Google Scholar] [CrossRef]
- Robine, J.-M.; Cheung, S.L.K.; Le Roy, S.; Van Oyen, H.; Griffiths, C.; Michel, J.-P.; Herrmann, F.R. Death toll exceeded 70,000 in Europe during the summer of 2003. C. R. Biol. 2008, 331, 171–178. [Google Scholar] [CrossRef]
- Pirard, P.; Vandentorren, S.; Pascal, M.; Laaidi, K.; Le Tertre, A.; Cassadou, S.; Ledrans, M. Summary of the mortality impact assessment of the 2003 heat wave in France. Euro Surveill. 2005, 10, 153–156. [Google Scholar] [CrossRef]
- Centre for Research on the Epidemiology of Disasters—CRED. Database|EM-DAT. Available online: https://www.emdat.be/database (accessed on 11 August 2019).
- Pascal, M.; Wagner, V.; Corso, M.; Laiidi, K.; Le Tertre, A. Évolutions de L’exposition Aux Canicules et de la Mortalité Associée en France Métropolitaine Entre 1970 et 2013. Available online: https://www.santepubliquefrance.fr/determinants-de-sante/climat/fortes-chaleurs-canicule/documents/rapport-synthese/evolutions-de-l-exposition-aux-canicules-et-de-la-mortalite-associee-en-france-metropolitaine-entre-1970-et-2013 (accessed on 10 December 2019).
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019: Highlights; ST/ESA/SER.A/42; United Nations, Department of Economic and Social Affairs, Population Division: New York, NY, USA, 2019. [Google Scholar]
- UNDESA. World Population Prospects: The 2012 Revision; Population division of the department of economic and social affairs of the United Nations Secretariat: New York, NY, USA, 2013; Volume 18. [Google Scholar]
- United Nation, Department of Economic and Social Affairs. World Urbanization Prospects: The 2018 Revision: Key facts; United Nation, Department of Economic and Social Affairs: New York, NY, USA, 2018. [Google Scholar]
- Intergovernmental Panel on Climate Change Emergent Risks and Key Vulnerabilities. Climate Change 2014—Impacts, Adaptation and Vulnerability; Part A: Global and Sectoral Aspects; IPCC: New York, NY, USA, 2014. [Google Scholar]
- Akerlof, K.L.; Delamater, P.L.; Boules, C.R.; Upperman, C.R.; Mitchell, C.S. Vulnerable Populations Perceive Their Health as at Risk from Climate Change. Int. J. Env. Res. Public Health 2015, 12, 15419–15433. [Google Scholar] [CrossRef]
- IPCC AR5. Climate Change 2014: Impacts, Adaptation, and Vulnerability; IPCC: New York, NY, USA, 2014. [Google Scholar]
- Wolf, T.; McGregor, G. The development of a heat wave vulnerability index for London, United Kingdom. Weather Clim. Extrem. 2013, 1, 59–68. [Google Scholar] [CrossRef] [Green Version]
- Cutter, S.L. Vulnerability to environmental hazards. Prog. Hum. Geogr. 1996, 20, 529–539. [Google Scholar] [CrossRef]
- Ebi, K.L.; Kovats, R.S.; Menne, B. An Approach for Assessing Human Health Vulnerability and Public Health Interventions to Adapt to Climate Change. Environ. Health Perspect. 2006, 114, 1930–1934. [Google Scholar]
- EPSON Climate—Climate Change and Territorial Effects on Regions and Local Economies; ESPON Monitoring Committee: Berlin, Germany, 2019.
- Cutter, S.L.; Boruff, B.J.; Shirley, W.L. Social Vulnerability to Environmental Hazards*. Soc. Sci. Q. 2003, 84, 242–261. [Google Scholar] [CrossRef]
- Reid Colleen, E.; O’Neill Marie, S.; Gronlund Carina, J.; Brines Shannon, J.; Brown Daniel, G.; Diez-Roux Ana, V.; Joel, S. Mapping Community Determinants of Heat Vulnerability. Environ. Health Perspect. 2009, 117, 1730–1736. [Google Scholar] [CrossRef]
- Uejio, C.K.; Wilhelmi, O.V.; Golden, J.S.; Mills, D.M.; Gulino, S.P.; Samenow, J.P. Intra-urban societal vulnerability to extreme heat: The role of heat exposure and the built environment, socioeconomics, and neighborhood stability. Health Place 2011, 17, 498–507. [Google Scholar] [CrossRef]
- Wolf, T.; McGregor, G.; Analitis, A. Assessing Vulnerability to Heat Stress in Urban Areas. The Example of Greater London. Epidemiology 2009, 20, S24. [Google Scholar] [CrossRef]
- Nayak, S.G.; Shrestha, S.; Kinney, P.L.; Ross, Z.; Sheridan, S.C.; Pantea, C.I.; Hsu, W.H.; Muscatiello, N.; Hwang, S.A. Development of a heat vulnerability index for New York State. Public Health 2018, 161, 127–137. [Google Scholar] [CrossRef]
- Bao, J.; Li, X.; Yu, C. The Construction and Validation of the Heat Vulnerability Index, a Review. Int. J. Environ. Res. Public Health 2015, 12, 7220–7234. [Google Scholar] [CrossRef] [Green Version]
- Inostroza, L.; Palme, M.; Barrera, F. de la A Heat Vulnerability Index: Spatial Patterns of Exposure, Sensitivity and Adaptive Capacity for Santiago de Chile. PLoS ONE 2016, 11, e0162464. [Google Scholar] [CrossRef] [Green Version]
- Borden, K.A.; Schmidtlein, M.C.; Emrich, C.T.; Piegorsch, W.W.; Cutter, S.L. Vulnerability of U.S. Cities to Environmental Hazards. J. Homel. Secur. Emerg. Manag. 2007, 4. [Google Scholar] [CrossRef]
- Cutter, S.L.; Finch, C. Temporal and spatial changes in social vulnerability to natural hazards. Proc. Natl. Acad. Sci. USA 2008, 105, 2301–2306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holand, I.S.; Lujala, P. Replicating and Adapting an Index of Social Vulnerability to a New Context: A Comparison Study for Norway. Prof. Geogr. 2013, 65, 312–328. [Google Scholar] [CrossRef]
- Johnson, D.P.; Stanforth, A.; Lulla, V.; Luber, G. Developing an applied extreme heat vulnerability index utilizing socioeconomic and environmental data. Appl. Geogr. 2012, 35, 23–31. [Google Scholar] [CrossRef]
- Koks, E.E.; Jongman, B.; Husby, T.G.; Botzen, W.J.W. Combining hazard, exposure and social vulnerability to provide lessons for flood risk management. Environ. Sci. Policy 2015, 47, 42–52. [Google Scholar] [CrossRef]
- Lee, Y.-J. Social vulnerability indicators as a sustainable planning tool. Environ. Impact Assess. Rev. 2014, 44, 31–42. [Google Scholar] [CrossRef]
- Rinner, C.; Patychuk, D.; Bassil, K.; Nasr, S.; Gower, S.; Campbell, M. The Role of Maps in Neighborhood-level Heat Vulnerability Assessment for the City of Toronto. Cartogr. Geogr. Inf. Sci. 2010, 37, 31–44. [Google Scholar] [CrossRef]
- Su, S.; Pi, J.; Wan, C.; Li, H.; Xiao, R.; Li, B. Categorizing social vulnerability patterns in Chinese coastal cities. Ocean Coast. Manag. 2015, 116, 1–8. [Google Scholar] [CrossRef]
- El-Zein, A.; Tonmoy, F.N. Assessment of vulnerability to climate change using a multi-criteria outranking approach with application to heat stress in Sydney. Ecol. Indic. 2015, 48, 207–217. [Google Scholar] [CrossRef] [Green Version]
- Hémon, D.; Jougla, E. Surmortalité Liée à la Canicule D’août 2003—Rapport D’étape; Institut National de la Santé et la Recherche Médicale (ISERM): Paris, France, 2003; p. 57. [Google Scholar]
- Hondula, D.M.; Davis, R.E.; Leisten, M.J.; Saha, M.V.; Veazey, L.M.; Wegner, C.R. Fine-scale spatial variability of heat-related mortality in Philadelphia County, USA, from 1983–2008: A case-series analysis. Environ. Health 2012, 11, 16. [Google Scholar] [CrossRef] [Green Version]
- Laiidi, K. Synthèse Des Études de L’INVS Sur Les Facteurs de Risques/Impacts Sanitaires Des Vagues de Chaleur en Milieu Urbain Utilisant Des Données Satellitaires; Institut de Veillle Sanitaire (INVS): Saint-Maurice, France, 2012.
- Tomlinson, C.J.; Chapman, L.; Thornes, J.E.; Baker, C.J. Including the urban heat island in spatial heat health risk assessment strategies: A case study for Birmingham, UK. Int. J. Health Geogr. 2011, 10, 42. [Google Scholar] [CrossRef] [Green Version]
- Vescovi, L.; Rebetez, M.; Rong, F. Assessing public health risk due to extremely high temperature events: Climate and social parameters. Clim. Res. 2005, 30, 71–78. [Google Scholar] [CrossRef]
- Rød, J.K.; Berthling, I.; Lein, H.; Lujala, P.; Vatne, G.; Bye, L.M. Integrated vulnerability mapping for wards in Mid-Norway. Local Environ. 2012, 17, 695–716. [Google Scholar] [CrossRef]
- Fouillet, A.; Rey, G.; Laurent, F.; Pavillon, G.; Bellec, S.; Guihenneuc-Jouyaux, C.; Clavel, J.; Jougla, E.; Hémon, D. Excess mortality related to the August 2003 heat wave in France. Int. Arch. Occup. Environ. Health 2006, 80, 16–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holand, I.S.; Lujala, P.; Rød, J.K. Social vulnerability assessment for Norway: A quantitative approach. Nor. Geogr. Tidsskr. Nor. J. Geogr. 2011, 65, 1–17. [Google Scholar] [CrossRef]
- Patt, A.G.; Schröter, D.; de la Vega-Leinert, A.; Klein, R. Vulnerability research and assessment to support adaptation and mitigation: Common themes from the diversity of approaches. In Assessing Vulnerability to Global Environmental Change; Richard, J.T., Klein, A.G., London, P., Eds.; Routledge: Abingdon-on-Thames, UK, 2009; pp. 1–25. ISBN 978-1-84407-697-0. [Google Scholar]
- Luers, A.; Lobell, D.; Sklar, L.; Addams, C.; Matson, P. A Method for Quantifying Vulnerability, Applied to the Agricultural System of the Yaqui Valley, Mexico. Glob. Environ. Chang. 2003, 13, 255–267. [Google Scholar] [CrossRef]
- Andrade, M.; Szlafsztein, C.; Pedro, W.M.S. A socioeconomic and natural vulnerability index for oil spills in an Amazonian harbor: A case study using GIS and remote sensing. J. Environ. Manag. 2010, 91, 1972–1980. [Google Scholar] [CrossRef]
- Huang, Y.; Li, F.; Bai, X.; Cui, S. Comparing vulnerability of coastal communities to land use change: Analytical framework and a case study in China. Environ. Sci. Policy 2012, 23, 133–143. [Google Scholar] [CrossRef]
- Voelkel, J.; Hellman, D.; Sakuma, R.; Shandas, V. Assessing Vulnerability to Urban Heat: A Study of Disproportionate Heat Exposure and Access to Refuge by Socio-Demographic Status in Portland, Oregon. Int. J. Environ. Res. Public Health 2018, 15, 640. [Google Scholar] [CrossRef] [Green Version]
- Sen, P.K. Estimates of the Regression Coefficient Based on Kendall’s Tau. J. Am. Stat. Assoc. 1968, 63, 1379–1389. [Google Scholar] [CrossRef]
- Renard, F.; Alonso, L.; Fitts, Y.; Hadjiosif, A.; Comby, J. Evaluation of the Effect of Urban Redevelopment on Surface Urban Heat Islands. Remote Sens. 2019, 11, 299. [Google Scholar] [CrossRef] [Green Version]
- ORECC. Fiche Indicateur—Climat: Changement climatique en Auvergne Rhône-Alpes—Températures Moyennes Annuelles et Saisonnières; ORECC, Direction Régionale de l’Environnement de l’Aménagement et du Logement (DREAL) Auvergne-Rhône-Alpes: Lyon, France, 2017. [Google Scholar]
- Bastin, J.-F.; Clark, E.; Elliott, T.; Hart, S.; van den Hoogen, J.; Hordijk, I.; Ma, H.; Majumder, S.; Manoli, G.; Maschler, J.; et al. Understanding climate change from a global analysis of city analogues. PLoS ONE 2019, 14, e0217592. [Google Scholar]
- Foissard, X.; Dubreuil, V.; Quénol, H. Defining scales of the land use effect to map the urban heat island in a mid-size European city: Rennes (France). Urban Clim. 2019, 29, 100490. [Google Scholar] [CrossRef]
- Karl, T.R.; Nicholls, N.; Ghazi, A. Clivar/GCOS/WMO Workshop on Indices and Indicators for Climate Extremes Workshop Summary. Clim. Chang. 1999, 42, 3–7. [Google Scholar] [CrossRef]
- Nairn, J.R.; Fawcett, R.J.B. The Excess Heat Factor: A Metric for Heatwave Intensity and Its Use in Classifying Heatwave Severity. Int. J. Environ. Res. Public Health 2015, 12, 227–253. [Google Scholar] [CrossRef] [Green Version]
- Renard, F. Flood risk management centred on clusters of territorial vulnerability. Geomat. Nat. Hazards Risk 2017, 8, 525–543. [Google Scholar] [CrossRef] [Green Version]
- Saaty, R.W. The analytic hierarchy process—What it is and how it is used. Math. Model. 1987, 9, 161–176. [Google Scholar] [CrossRef] [Green Version]
- Kendrick, D.J.; Saaty, D. Use Analytic Hierarchy Process for Project Selection. Inf. Manag. 2007, 18, 87–95. [Google Scholar]
- Saaty, T.L. How to Make a Decision: The Analytic Hierarchy Process. Inf. J. Appl. Anal. 1994, 24, 19–43. [Google Scholar] [CrossRef]
- Saaty, T.L. How to make a decision: The analytic hierarchy process. Eur. J. Oper. Res. 1990, 48, 9–26. [Google Scholar] [CrossRef]
- OCDE. Handbook on Constructing Composite Indicators: Methodology and User Guide; OCDE. Joint Research Centre (JRC) of the European Commission in Ispra, Italy, 2008. Available online: http://www.oecd.org/fr/els/soc/handbookonconstructingcompositeindicatorsmethodologyanduserguide.htm (accessed on 17 April 2019).
- Shapiro, S.S.; Wilk, M.B. An analysis of variance test for normality (complete samples). Biometrika 1965, 52, 591–611. [Google Scholar] [CrossRef]
- Kaiser, H.F. An index of factorial simplicity. Psychometrika 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Brown, M.B.; Forsythe, A.B. Robust Tests for the Equality of Variances. J. Am. Stat. Assoc. 1974, 69, 364–367. [Google Scholar] [CrossRef]
- Cureton, E.E.; Mulaik, S.A. The weighted varimax rotation and the promax rotation. Psychometrika 1975, 40, 183–195. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef] [Green Version]
- Jaime, M.; Kazuhiko, I.; Sarah, J.; Kinney Patrick, L.; Thomas, M. A Case-Only Study of Vulnerability to Heat Wave–Related Mortality in New York City (2000–2011). Environ. Health Perspect. 2015, 123, 672–678. [Google Scholar]
- O’Brien, K.; Sygna, L.; Haugen, J.E. Vulnerable or Resilient? A Multi-Scale Assessment of Climate Impacts and Vulnerability in Norway. Clim. Chang. 2004, 64, 193–225. [Google Scholar] [CrossRef]
- Saaty, T. Decision making with the Analytic Hierarchy Process. Int. J. Serv. Sci. 2008, 1, 83–98. [Google Scholar] [CrossRef] [Green Version]
- Lin, W.-Y.; Hung, C.-T. Applying spatial clustering analysis to a township-level social vulnerability assessment in Taiwan. Geomat. Nat. Hazards Risk 2016, 7, 1659–1676. [Google Scholar] [CrossRef] [Green Version]
- Forman, E.; Peniwati, K. Aggregating individual judgments and priorities with the analytic hierarchy process. Eur. J. Oper. Res. 1998, 108, 165–169. [Google Scholar] [CrossRef]
- Ramanathan, R.; Ganesh, L.S. Group preference aggregation methods employed in AHP: An evaluation and an intrinsic process for deriving members’ weightages. Eur. J. Oper. Res. 1994, 79, 249–265. [Google Scholar] [CrossRef]
- Zhao, Q.; Yang, J.; Wang, Z.-H.; Wentz, E.A. Assessing the Cooling Benefits of Tree Shade by an Outdoor Urban Physical Scale Model at Tempe, AZ. Urban Sci. 2018, 2, 4. [Google Scholar] [CrossRef] [Green Version]









| Selected Variables | Effect on the Vulnerability | References |
|---|---|---|
| Children under 5 years old | Increase | [44,47] |
| Person aged 6 to 44 years old | Decrease | [49,50] |
| Person aged 45 to 74 years old | Decrease | [50] |
| Person 75 years old or older | Increase | [35,44,47,49,50,51,52,53,54] |
| Sex for 45–74 years olds | The greater the number of women, the more vulnerable they are | [44] |
| Sex for over 75 years olds | The greater the number of women, the more vulnerable they are | [44] |
| Person affected by chronic or acute pathology | Increase | [35,47,52,53] |
| Person with psychiatric disorders | Increase | [50,52] |
| Children Under 5 Years Old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person Aged 6 to 44 Years Old |
| Children under 5 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person aged 45 to 74 years old |
| Children under 5 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person 75 years of age or older |
| Children under 5 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person affected by chronic or acute pathology |
| Children under 5 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person with psychiatric disorders |
| Person aged 6 to 44 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person aged 45 to 74 years old |
| Person aged 6 to 44 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person 75 years of age or older |
| Person aged 6 to 44 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person affected by chronic or acute pathology |
| Person aged 6 to 44 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person with psychiatric disorders |
| Person aged 6 to 44 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person 75 years of age or older |
| Person aged 45 to 74 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person affected by chronic or acute pathology |
| Person aged 45 to 74 years old | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person with psychiatric disorders |
| Person 75 years of age or older | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person affected by chronic or acute pathology |
| Person 75 years of age or older | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person with psychiatric disorders |
| Person affected by chronic or acute pathology | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Person with psychiatric disorders |
| Person aged 45 to 74 years old | ||||||||||||||||||
| Male | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Female |
| Person 75 years of age or older | ||||||||||||||||||
| Male | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Female |
| Selected Variables | Author |
|---|---|
| Ratio of the number of births domiciled at the mother’s home | [34,41,42,43,46] |
| Average age of the population | [41,42,43] |
| % of the population between the ages of 18 and 64 | [55] |
| % of population under 5 years old | [34,41,43,45,48,57] |
| % of population over 65 years old | [30,34,41,43,45] |
| Ratio of females to males | [43,57] |
| % of female population | [34,41,43,46] |
| number of employed persons with low-skilled jobs between 15–64 years old | [34,43,57] |
| Poverty rate of the entire population | [34,41,42] |
| Average age of principal residences over the period 1900 to 2009, | [41,43,46] |
| % of apartment type principal residents built between 1990 and 2009 | [57] |
| % population living in low-rent housing | [43] |
| % population in main residence occupied free of charge | [34] |
| % of precarious housing | [34] |
| % of employed women between 15–64 years old | [34,41,42] |
| % of employment in the population between 15 and 64 years old | [34,41] |
| % of the employed population between 15–64 years old working in farming | [41,55,57] |
| Unemployment rate of the employed population between 15 and 64 years old | [34,41,48,57] |
| Unemployment rate of employed women between 15 and 64 years old | / |
| % employed population with low-skilled jobs | [34,43,57] |
| % of retired people in 2012 | / |
| % out-of-school population over 15 with no higher education qualification | [34,41,42,46,57] |
| % population over 15 years out of school with no certificate or diploma | / |
| % out-of-school population over 15 years old with long-term education at tertiary institutions | [57] |
| % out-of-school population over 15 years old with higher education | / |
| Number of medical professions in 2014 per capita | [41,43,57] |
| Number of health institutions of all types (private or public) | [34,41,42] |
| Average annual salary in euros | [34,41,42,43,45,55,57] |
| Mortality rate (all causes) per 1000 inhabitants | [55] |
| Number of premature deaths from all causes (before the 65 years old) per capita | [43,55] |
| Number of new long-term care (LTC) admissions per capita | [30,55] |
| Number of people receiving adult disabled benefit (ADB) per inhabitant | [43,57] |
| Median household income in euros | [55,57] |
| Number of people on psychotropic treatment per capita | [46] |
| Number of hospital places (short or long hospitalisation) per 1000 inhabitants | [41,46] |
| % of people suffering from psychiatric disorders (Full-time inpatient active file) in 2012 | [46] |
| Number of psychiatric hospital places per 1000 inhabitants | / |
| Number of care places per 1000 inhabitants | [30] |
| Proportion of social housing (%) | [30] |
| Length in kilometres from a hospital by isochrones | [43,57] |
| Factors after PCA with Varimax Rotating | Variables | Increases (+) or Decreases (−) Socio-Economic Vulnerability | Details | Weighting | |
|---|---|---|---|---|---|
| Socio-economic disadvantages (+) | Low-skilled worker | High concentration (+); low concentration (−) | People working in low-skilled jobs can be severely impacted by a heat wave, often working in extreme conditions. | 0.92 | |
| No graduate student | High concentration (+); low concentration (−) | People without higher education may not be aware of preventive actions against heat waves. | 0.87 | ||
| Person with university education | High concentration (−); low concentration (+) | People with higher education may have a greater knowledge of preventive measures to be taken in the event of heat waves. | 0.79 | ||
| Unemployment rate | High (+); Low (−) | People affected by unemployment do not necessarily have the financial means and appropriate housing to protect themselves from these extreme climatic conditions. | 0.76 | ||
| Person in social housing | High concentration (+); low concentration (−) | Social housing is more obsolete, often poorly insulated and without centralized air conditioning. | 0.73 | ||
| Average annual income | High (−); Low (+) | The higher a household’s average annual income, the more it will have the financial means to protect itself from these unpredicted and extreme weather conditions. | 0.69 | ||
| Person 5 years old or younger | High concentration (+); low concentration (−) | Children under 5 years of age are less physically resistant to extreme heat (more rapidly dehydrated). | 0.66 | ||
| Poverty rate | High (+); Low (−) | People living below the poverty level do not have sufficient income funds to be able to cope with rising temperatures or to protect themselves from a heat wave. | 0.60 | ||
| The economic disadvantages of a population, household or individual contribute to increasing their vulnerability to a heat wave. | |||||
| Physical disadvantages (+) | Birth rate | High (+); Low (−) | Many births may represent increasing family size and thus financial limitations, often with the outsourcing of care for newborns, requiring families to combine their responsibilities with the needs of the family. | 0.92 | |
| Number of treatments with psychotropic medications | High concentration (+); low concentration (−) | People taking psychotropic medications are less physically resistant to extreme heat. | 0.92 | ||
| Number of people receiving an Adult Disability Benefit (ADB) | High contribution (+); Low contribution (−) | People receiving an ADB who are dependent on services | 0.87 | ||
| Number of premature deaths | High concentration (+); low concentration (−) | The number of premature deaths is associated with poor health and often low income and therefore low physical resistance during a heat wave. | 0.84 | ||
| People with physical disavantages are therefore more vulnerable to heat waves. | |||||
| Elderly people (+) | Pensioners | High contribution (+); Low contribution (−) | Pensioners are people of advanced age, physically less resistant to high temperatures. | 0.83 | |
| People over 65 years old | High contribution (+); Low contribution (−) | People over the age of 65 are less physically resistant to extreme heat (more rapidly dehydrated). | 0.79 | ||
| Person without a certificate | High contribution (+); Low contribution (−) | People without certificates may not be aware of preventive measures to cope with heat waves. | 0.66 | ||
| Elderly people are less physically resistant to extreme heat (more rapidly dehydrated). | |||||
| Territorial development indicator (−) | Mortality rate | High (+); Low (−) | A high mortality rate is associated with deteriorated health and therefore low physical resistance of the populations living within this space during a heat wave. | 0.73 | |
| Distance to hospital | High (+); Low (−) | A high distance reduces the ability to mobilize sufficient resources in a reasonable amount of time. | 0.71 | ||
| Number of beds in hospital | High (−); Low (+) | A low number of hospital beds reduces the ability to mobilize sufficient resources in a reasonable period of time to help people cope with the impact of a heat wave. | 0.68 | ||
| High territorial development can help reduce the vulnerability of the population to heat waves. | |||||
| Female population (+) | Female person | High contribution (+); Low contribution (−) | Women have more physical defaults to cope with the effects of high heat. | 0.77 | |
| Non-working woman | High contribution (+); Low contribution (−) | Working women may be less vulnerable than non-working women because they will have more financial resources to prevent heat waves. | 0.33 | ||
| Women are generally more vulnerable to the effects of a heat wave. | |||||
| Health (−) | Number of medical professions | Numerous (−); not many (+) | A high number of medical professions contributes to increasing the capacity to mobilize sufficient resources in a reasonable time to help populations cope with the effects of a heat wave. | 0.77 | |
| Number of health establishments | Numerous (−); not many (+) | A high number of health establishments contributes to increasing the capacity to mobilize sufficient resources in a reasonable time to help populations cope with the effects of a heat wave. | 0.76 | ||
| Rapid and dense health interventions can help reduce people’s vulnerability to heat waves. | |||||
| Physio | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Factor 6 | Res. Density | |
|---|---|---|---|---|---|---|---|---|
| Socio-eco | −0.015 | 0.886 | 0.554 | 0.327 | 0.445 | 0.266 | 0.056 | −0.036 |
| Physio | 1 | −0.036 | 0.338 | −0.302 | −0.397 | 0.084 | −0.469 | 0.970 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alonso, L.; Renard, F. A Comparative Study of the Physiological and Socio-Economic Vulnerabilities to Heat Waves of the Population of the Metropolis of Lyon (France) in a Climate Change Context. Int. J. Environ. Res. Public Health 2020, 17, 1004. https://doi.org/10.3390/ijerph17031004
Alonso L, Renard F. A Comparative Study of the Physiological and Socio-Economic Vulnerabilities to Heat Waves of the Population of the Metropolis of Lyon (France) in a Climate Change Context. International Journal of Environmental Research and Public Health. 2020; 17(3):1004. https://doi.org/10.3390/ijerph17031004
Chicago/Turabian StyleAlonso, Lucille, and Florent Renard. 2020. "A Comparative Study of the Physiological and Socio-Economic Vulnerabilities to Heat Waves of the Population of the Metropolis of Lyon (France) in a Climate Change Context" International Journal of Environmental Research and Public Health 17, no. 3: 1004. https://doi.org/10.3390/ijerph17031004
APA StyleAlonso, L., & Renard, F. (2020). A Comparative Study of the Physiological and Socio-Economic Vulnerabilities to Heat Waves of the Population of the Metropolis of Lyon (France) in a Climate Change Context. International Journal of Environmental Research and Public Health, 17(3), 1004. https://doi.org/10.3390/ijerph17031004