Effect of Natural Disaster-Related Prenatal Maternal Stress on Child Development and Health: A Meta-Analytic Review
Abstract
:1. Introduction
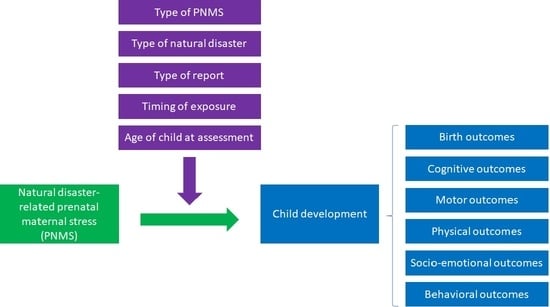
Study Aims
2. Materials and Methods
2.1. Protocol
2.2. Search Strategy
2.3. Study Eligibility Criteria
2.4. Study Selection
2.5. Data Extraction
2.6. Quality Assessment
2.7. Statistical Analysis
3. Results
3.1. Database Search Process
3.2. Data Extraction
3.3. Child Development Outcomes
3.3.1. Birth Outcomes
3.3.2. Cognitive Outcomes
3.3.3. Motor Outcomes
3.3.4. Physical Outcomes
3.3.5. Socio-Emotional Outcomes
3.3.6. Behavioral Outcomes
4. Discussion
4.1. Limitations
4.2. Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van den Bergh, B.R.; van den Heuvel, M.I.; Lahti, M.; Braeken, M.; de Rooij, S.R.; Entringer, S.; Hoyer, D.; Roseboom, T.; Räikkönen, K.; King, S. Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci. Biobehav. Rev. 2020, 117, 26–64. [Google Scholar] [CrossRef] [Green Version]
- Madigan, S.; Oatley, H.; Racine, N.; Fearon, R.P.; Schumacher, L.; Akbari, E.; Cooke, J.E.; Tarabulsy, G.M. A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. J. Am. Acad. Child. Adolesc. Psychiatry 2018, 57, 645–657.e648. [Google Scholar] [CrossRef]
- Camacho, A. Stress and birth weight: Evidence from terrorist attacks. Am. Econ. Rev. 2008, 98, 511–515. [Google Scholar] [CrossRef]
- Ritchie, H.; Roser, M. Natural Disasters. 2014. Available online: https://ourworldindata.org/natural-disasters (accessed on 20 June 2020).
- Patz, J.A.; Campbell-Lendrum, D.; Holloway, T.; Foley, J.A. Impact of regional climate change on human health. Nature 2005, 438, 310–317. [Google Scholar] [CrossRef]
- Van Aalst, M.K. The impacts of climate change on the risk of natural disasters. Disasters 2006, 30, 5–18. [Google Scholar] [CrossRef]
- Doocy, S.; Daniels, A.; Dick, A.; Kirsch, T.D. The human impact of tsunamis: A historical review of events 1900–2009 and systematic literature review. PLoS Curr. 2013, 5. [Google Scholar] [CrossRef] [PubMed]
- Doocy, S.; Daniels, A.; Dooling, S.; Gorokhovich, Y. The human impact of volcanoes: A historical review of events 1900–2009 and systematic literature review. PLoS Curr. 2013, 5. [Google Scholar] [CrossRef]
- Doocy, S.; Daniels, A.; Murray, S.; Kirsch, T.D. The human impact of floods: A historical review of events 1980–2009 and systematic literature review. PLoS Curr. 2013, 5. [Google Scholar] [CrossRef] [PubMed]
- Doocy, S.; Daniels, A.; Packer, C.; Dick, A.; Kirsch, T.D. The human impact of earthquakes: A historical review of events 1980–2009 and systematic literature review. PLoS Curr. 2013, 5. [Google Scholar] [CrossRef]
- Doocy, S.; Dick, A.; Daniels, A.; Kirsch, T.D. The human impact of tropical cyclones: A historical review of events 1980–2009 and systematic literature review. PLoS Curr. 2013, 5. [Google Scholar] [CrossRef]
- Assar, M. Guide to Sanitation in Natural Disasters; WHO: Geneva, Switzerland, 1971. [Google Scholar]
- Alexander, D. Natural Disasters; Routledge: London, UK, 2018. [Google Scholar]
- Neumayer, E.; Plümper, T. The gendered nature of natural disasters: The impact of catastrophic events on the gender gap in life expectancy, 1981–2002. Ann. Am. Assoc. Geogr. 2007, 97, 551–566. [Google Scholar] [CrossRef] [Green Version]
- Thurston, A.M.; Stöckl, H.; Ranganathan, M. Natural hazards, disasters and violence against women and girls: A global mixed-methods systematic review. BMJ Glob. Health 2021, 6, e004377. [Google Scholar] [CrossRef]
- Bateson, P.; Gluckman, P.; Hanson, M. The biology of developmental plasticity and the Predictive Adaptive Response hypothesis. J. Physiol. 2014, 592, 2357–2368. [Google Scholar] [CrossRef] [PubMed]
- Gluckman, P.D.; Hanson, M.A. The developmental origins of health and disease. In Early Life Origins of Health and Disease; Springer: Boston, MA, USA, 2006; pp. 1–7. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- King, S.; Mancini-Marie, A.; Brunet, A.; Walker, E.; Meaney, M.J.; Laplante, D.P. Prenatal maternal stress from a natural disaster predicts dermatoglyphic asymmetry in humans. Dev. Psychopathol. 2009, 21, 343–353. [Google Scholar] [CrossRef] [Green Version]
- Glover, V.; Hill, J. Sex differences in the programming effects of prenatal stress on psychopathology and stress responses: An evolutionary perspective. Physiol. Behav. 2012, 106, 736–740. [Google Scholar] [CrossRef] [PubMed]
- Charil, A.; Laplante, D.P.; Vaillancourt, C.; King, S. Prenatal stress and brain development. Brain Res. Rev. 2010, 65, 56–79. [Google Scholar] [CrossRef]
- Veru, F.; Laplante, D.P.; Luheshi, G.; King, S. Prenatal maternal stress exposure and immune function in the offspring. Stress 2014, 17, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Van Os, J.; Reininghaus, U. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry 2016, 15, 118–124. [Google Scholar] [CrossRef] [Green Version]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dancause, K.N.; Veru, F.; Andersen, R.E.; Laplante, D.P.; King, S. Prenatal stress due to a natural disaster predicts insulin secretion in adolescence. Early Hum. Dev. 2013, 89, 773–776. [Google Scholar] [CrossRef] [Green Version]
- Jones, S.L.; Dufoix, R.; Laplante, D.P.; Elgbeili, G.; Patel, R.; Chakravarty, M.M.; King, S.; Pruessner, J.C. Larger amygdala volume mediates the association between prenatal maternal stress and higher levels of externalizing behaviors: Sex specific effects in project ice storm. Front. Hum. Neurosci. 2019, 13, 144. [Google Scholar] [CrossRef] [PubMed]
- Cao-Lei, L.; Elgbeili, G.; Massart, R.; Laplante, D.P.; Szyf, M.; King, S. Pregnant women’s cognitive appraisal of a natural disaster affects DNA methylation in their children 13 years later: Project Ice Storm. Transl. Psychiatry 2015, 5, e515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bero, L.; Chartres, N.; Diong, J.; Fabbri, A.; Ghersi, D.; Lam, J.; Lau, A.; McDonald, S.; Mintzes, B.; Sutton, P.; et al. The risk of bias in observational studies of exposures (ROBINS-E) tool: Concerns arising from application to observational studies of exposures. Syst. Rev. 2018, 7, 242. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G.; Group, C.S.M. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2019; Available online: www.training.cochrane.org/handbook (accessed on 15 July 2020).
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: Chichester, UK, 2011. [Google Scholar]
- United Nations Children’s Fund (UNICEF). Adolescence, an Age of Opportunity: The State of the World’s Children 2011; Anthony, D., Ed.; UNICEF: New York, NY, USA, 2011; ISBN 978-92-806-4555-2. Available online: https://www.refworld.org/docid/4d6cfa162.html (accessed on 21 July 2020).
- Austin, M.P.; Christl, B.; McMahon, C.; Kildea, S.; Reilly, N.; Yin, C.; Simcock, G.; Elgbeili, G.; Laplante, D.P.; King, S. Moderating effects of maternal emotional availability on language and cognitive development in toddlers of mothers exposed to a natural disaster in pregnancy: The QF2011 Queensland Flood Study. Infant Behav. Dev. 2017, 49, 296–309. [Google Scholar] [CrossRef]
- Cai, D.; Zhu, Z.; Sun, H.; Qi, Y.; Xing, L.; Zhao, X.; Wan, Q.; Su, Q.; Li, H. Maternal PTSD following exposure to the Wenchuan earthquake is associated with impaired mental development of children. PLoS ONE 2017, 12, e0168747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, X.; Laplante, D.P.; Brunet, A.; Ciampi, A.; King, S. Prenatal maternal stress affects motor function in 5(1/2)-year-old children: Project ice storm. Dev. Psychobiol. 2014, 56, 117–125. [Google Scholar] [CrossRef]
- Cao-Lei, L.; Dancause, K.N.; Elgbeili, G.; Laplante, D.P.; Szyf, M.; King, S. DNA methylation mediates the effect of maternal cognitive appraisal of a disaster in pregnancy on the child’s C-peptide secretion in adolescence: Project Ice Storm. PLoS ONE 2018, 13, e0192199. [Google Scholar] [CrossRef] [PubMed]
- Dancause, K.N.; Laplante, D.P.; Hart, K.J.; O’Hara, M.W.; Elgbeili, G.; Brunet, A.; King, S. Prenatal stress due to a natural disaster predicts adiposity in childhood: The Iowa Flood Study. J. Obes. 2015, 2015, 570541. [Google Scholar] [CrossRef] [Green Version]
- Dancause, K.N.; Mutran, D.; Elgbeili, G.; Laplante, D.P.; Kildea, S.; Stapleton, H.; McIntyre, D.; King, S. Dietary change mediates relationships between stress during pregnancy and infant head circumference measures: The QF2011 study. Matern. Child. Nutr. 2017, 13, e12359. [Google Scholar] [CrossRef]
- Harville, E.W.; Do, M. Reproductive and birth outcomes in Haiti before and after the 2010 earthquake. Disaster Med. Public Health Prep. 2016, 10, 59–66. [Google Scholar] [CrossRef]
- Hilmert, C.J.; Kvasnicka-Gates, L.; Teoh, A.N.; Bresin, K.; Fiebiger, S. Major flood related strains and pregnancy outcomes. Health Psychol. 2016, 35, 1189–1196. [Google Scholar] [CrossRef]
- Kroska, E.B.; O’Hara, M.W.; Elgbeili, G.; Hart, K.J.; Laplante, D.P.; Dancause, K.N.; King, S. The impact of maternal flood-related stress and social support on offspring weight in early childhood. Arch. Womens Ment. Health 2018, 21, 225–233. [Google Scholar] [CrossRef]
- Laplante, D.P.; Barr, R.G.; Brunet, A.; Galbaud du Fort, G.; Meaney, M.L.; Saucier, J.F.; Zelazo, P.R.; King, S. Stress during pregnancy affects general intellectual and language functioning in human toddlers. Pediatric Res. 2004, 56, 400–410. [Google Scholar] [CrossRef] [Green Version]
- Laplante, D.P.; Zelazo, P.R.; Brunet, A.; King, S. Functional play at 2 years of age: Effects of prenatal maternal stress. Infancy 2007, 12, 69–93. [Google Scholar] [CrossRef]
- Laplante, D.P.; Brunet, A.; Schmitz, N.; Ciampi, A.; King, S. Project Ice Storm: Prenatal maternal stress affects cognitive and linguistic functioning in 5 1/2-year-old children. J. Am. Acad. Child. Adolesc. Psychiatry 2008, 47, 1063–1072. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laplante, D.P.; Brunet, A.; King, S. The effects of maternal stress and illness during pregnancy on infant temperament: Project Ice Storm. Pediatric Res. 2016, 79, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Laplante, D.P.; Hart, K.J.; O’Hara, M.W.; Brunet, A.; King, S. Prenatal maternal stress is associated with toddler cognitive functioning: The Iowa Flood Study. Early Hum. Dev. 2018, 116, 84. [Google Scholar] [CrossRef]
- Laplante, D.P.; Simcock, G.; Cao-Lei, L.; Mouallem, M.; Elgbeili, G.; Brunet, A.; Cobham, V.; Kildea, S.; King, S. The 5-HTTLPR polymorphism of the serotonin transporter gene and child’s sex moderate the relationship between disaster-related prenatal maternal stress and autism spectrum disorder traits: The QF2011 Queensland flood study. Dev. Psychopathol. 2019, 31, 1395–1409. [Google Scholar] [CrossRef] [PubMed]
- Lequertier, B.; Simcock, G.; Cobham, V.E.; Kildea, S.; King, S. Infant behavior and competence following prenatal exposure to a natural disaster: The QF 2011 Queensland Flood Study. Infancy 2019, 24, 411–432. [Google Scholar] [CrossRef]
- Liu, G.T.; Dancause, K.N.; Elgbeili, G.; Laplante, D.P.; King, S. Disaster-related prenatal maternal stress explains increasing amounts of variance in body composition through childhood and adolescence: Project Ice Storm. Environ. Res. 2016, 150, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McLean, M.A.; Cobham, V.E.; Simcock, G.; Elgbeili, G.; Kildea, S.; King, S. The role of prenatal maternal stress in the development of childhood anxiety symptomatology: The QF2011 Queensland Flood Study. Dev. Psychopathol. 2018, 30, 995–1007. [Google Scholar] [CrossRef] [PubMed]
- McLean, M.A.; Cobham, V.E.; Simcock, G.; Kildea, S.; King, S. Toddler Temperament Mediates the Effect of Prenatal Maternal Stress on Childhood Anxiety Symptomatology: The QF2011 Queensland Flood Study. Int. J. Environ. Res. Public Health 2019, 16, 1998. [Google Scholar] [CrossRef] [Green Version]
- McLean, M.A.; Simcock, G.; Elgbeili, G.; Laplante, D.P.; Kildea, S.; Hurrion, E.; Lequertier, B.; Cobham, V.E.; King, S. Disaster-related prenatal maternal stress, and childhood HPA-axis regulation and anxiety: The QF2011 Queensland Flood Study. Psychoneuroendocrinology 2020, 118, 104716. [Google Scholar] [CrossRef] [PubMed]
- Moss, K.M.; Simcock, G.; Cobham, V.; Kildea, S.; Elgbeili, G.; Laplante, D.P.; King, S. A potential psychological mechanism linking disaster-related prenatal maternal stress with child cognitive and motor development at 16 months: The QF2011 Queensland Flood Study. Dev. Psychol. 2017, 53, 629. [Google Scholar] [CrossRef] [PubMed]
- Moss, K.M.; Simcock, G.; Cobham, V.E.; Kildea, S.; Laplante, D.P.; King, S. Continuous, emerging, and dissipating associations between prenatal maternal stress and child cognitive and motor development: The QF2011 Queensland Flood Study. Early Hum. Dev. 2018, 119, 29–37. [Google Scholar] [CrossRef]
- Nguyen, T.V.; Jones, S.L.; Elgbeili, G.; Monnier, P.; Yu, C.; Laplante, D.P.; King, S. Testosterone-cortisol dissociation in children exposed to prenatal maternal stress, and relationship with aggression: Project Ice Storm. Dev. Psychopathol. 2018, 30, 981–994. [Google Scholar] [CrossRef]
- Yong Ping, E.; Laplante, D.P.; Elgbeili, G.; Hillerer, K.M.; Brunet, A.; O’Hara, M.W.; King, S. Prenatal maternal stress predicts stress reactivity at 2½ years of age: The Iowa Flood Study. Psychoneuroendocrinology 2015, 56, 62–78. [Google Scholar] [CrossRef]
- Yong Ping, E.; Laplante, D.P.; Elgbeili, G.; Jones, S.L.; Brunet, A.; King, S.J.P. Disaster-related prenatal maternal stress predicts HPA reactivity and psychopathology in adolescent offspring: Project Ice Storm. Psychoneuroendocrinology 2020, 117, 104697. [Google Scholar] [CrossRef]
- Pomer, A.; Buffa, G.; Taleo, F.; Sizemore, J.H.; Tokon, A.; Taleo, G.; Tarivonda, L.; Chan, C.W.; Kaneko, A.; Dancause, K.N. Relationships between psychosocial distress and diet during pregnancy and infant birthweight in a lower-middle income country:‘Healthy mothers, healthy communities’ study in Vanuatu. Ann. Hum. Biol. 2018, 45, 220–228. [Google Scholar] [CrossRef]
- Sanguanklin, N.; McFarlin, B.L.; Park, C.G.; Giurgescu, C.; Finnegan, L.; White-Traut, R.; Engstrom, J.L. Effects of the 2011 flood in Thailand on birth outcomes and perceived social support. J. Obstet. Gynecol. Neonatal. Nurs. 2014, 43, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Simcock, G.; Kildea, S.; Elgbeili, G.; Laplante, D.P.; Stapleton, H.; Cobham, V.; King, S. Age-related changes in the effects of stress in pregnancy on infant motor development by maternal report: The Queensland Flood Study. Dev. Psychobiol. 2016, 58, 640–659. [Google Scholar] [CrossRef]
- Simcock, G.; Laplante, D.P.; Elgbeili, G.; Kildea, S.; Cobham, V.; Stapleton, H.; King, S. Infant neurodevelopment is affected by prenatal maternal stress: The QF 2011 Queensland Flood Study. Infancy 2017, 22, 282–302. [Google Scholar] [CrossRef]
- Simcock, G.; Elgbeili, G.; Laplante, D.P.; Kildea, S.; Cobham, V.; Stapleton, H.; Austin, M.P.; Brunet, A.; King, S. The effects of prenatal maternal stress on early temperament: The 2011 Queensland Flood Study. J. Dev. Behav. Pediatr. 2017, 38, 310–321. [Google Scholar] [CrossRef]
- Simcock, G.; Laplante, D.P.; Elgbeili, G.; Kildea, S.; King, S. A trajectory analysis of childhood motor development following stress in pregnancy: The QF2011 Flood Study. Dev. Psychobiol. 2018, 60, 836–848. [Google Scholar] [CrossRef] [PubMed]
- Simcock, G.; Cobham, V.E.; Laplante, D.P.; Elgbeili, G.; Gruber, R.; Kildea, S.; King, S. A cross-lagged panel analysis of children’s sleep, attention, and mood in a prenatally stressed cohort: The QF2011 Queensland Flood Study. J. Affect. Disord. 2019, 255, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Strahm, A.M.; Bagne, A.G.; Rued, H.A.; Larson, K.J.; Roemmich, J.N.; Hilmert, C.J. Prenatal traumatic stress and offspring hair cortisol concentration: A nine year follow up to the Red River flood pregnancy study. Psychoneuroendocrinology 2020, 113, 104579. [Google Scholar] [CrossRef] [PubMed]
- Veru, F.; Dancause, K.; Laplante, D.P.; King, S.; Luheshi, G. Prenatal maternal stress predicts reductions in CD4+ lymphocytes, increases in innate-derived cytokines, and a Th2 shift in adolescents: Project Ice Storm. Physiol. Behav. 2015, 144, 137–145. [Google Scholar] [CrossRef]
- Walder, D.J.; Laplante, D.P.; Sousa-Pires, A.; Veru, F.; Brunet, A.; King, S. Prenatal maternal stress predicts autism traits in 6½ year-old children: Project Ice Storm. Psychiatry Res. 2014, 219, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Berghella, V.; Boelig, R.; Roman, A.; Burd, J.; Anderson, K. Decreased incidence of preterm birth during coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. MFM 2020, 2, 100258. [Google Scholar] [CrossRef] [PubMed]
- Been, J.V.; Ochoa, L.B.; Bertens, L.C.; Schoenmakers, S.; Steegers, E.A.; Reiss, I.K. Impact of COVID-19 mitigation measures on the incidence of preterm birth: A national quasi-experimental study. Lancet Public Health 2020, 5, e604–e611. [Google Scholar] [CrossRef]
- Paquin, V.; Elgbeili, G.; Laplante, D.P.; Kildea, S.; King, S. Positive cognitive appraisal “buffers” the long-term effect of peritraumatic distress on maternal anxiety: The Queensland Flood Study. J. Affect. Disord. 2021, 278, 5–12. [Google Scholar] [CrossRef]
- Khoury, J.E.; Atkinson, L.; Bennett, T.; Jack, S.M.; Gonzalez, A. COVID-19 and mental health during pregnancy: The importance of cognitive appraisal and social support. J. Affect. Disord. 2021, 282, 1161–1169. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhou, X.; Jia, X.; Song, C.; Luo, X.; Zhang, H.; Wu, H.; Ye, J. Emotional exhaustion in front-line healthcare workers during the COVID-19 pandemic in Wuhan, China: The effects of time pressure, social sharing and cognitive appraisal. BMC Public Health 2021, 21, 829. [Google Scholar] [CrossRef]
- Xiaoyun, Y.; Hongai, Y.; Qifa, L. The research on the reliability and validity of PCL-C and influence factors. China J. Health Psychol. 2007, 15, 6–9. [Google Scholar]
- Weiss, D.S. The impact of event scale: Revised. In Cross-Cultural Assessment of Psychological Trauma and PTSD; Springer: New York, NY, USA, 2007; pp. 219–238. [Google Scholar]
- Brunet, A.; Weiss, D.S.; Metzler, T.J.; Best, S.R.; Neylan, T.C.; Rogers, C.; Fagan, J.; Marmar, C.R. The Peritraumatic Distress Inventory: A proposed measure of PTSD criterion A2. Am. J. Psychiatry 2001, 158, 1480–1485. [Google Scholar] [CrossRef] [Green Version]
- Marmar, C.R.; Metzler, T.J.; Otte, C.; McCaslin, S.; Inslicht, S.; Haase, C.H. The Peritraumatic Dissociative Experiences Questionnaire: An international perspective. In Cross-Cultural Assessment of Psychological Trauma and PTSD; Wilson, J.P., Tang, C.S.-K., Eds.; Springer: Boston, MA, USA, 2007; pp. 197–217. [Google Scholar]
- Bradshaw, S. Socio-Economic Impacts of Natural Disasters: A Gender Analysis; United Nations Economic Commission for Latin America and the Caribbean: Santiago, Chile, 2004. [Google Scholar]
- Cheung, M.W.-L. A guide to conducting a meta-analysis with non-independent effect sizes. Neuropsychol. Rev. 2019, 29, 387–396. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Castilla, B.; Maes, M.; Declercq, L.; Jamshidi, L.; Beretvas, S.N.; Onghena, P.; Van den Noortgate, W. A demonstration and evaluation of the use of cross-classified random-effects models for meta-analysis. Behav. Res. Methods. 2019, 51, 1286–1304. [Google Scholar] [CrossRef] [Green Version]
- Hedges, L.V.; Tipton, E.; Johnson, M.C. Robust variance estimation in meta-regression with dependent effect size estimates. Res. Synth. Methods 2010, 1, 39–65. [Google Scholar] [CrossRef]
- Janssen, I. Unpublished manuscript for the Public Health Agency of Canada; Based on Analysis of the 1994/95 and 1996/97 National Population Health Surveys; 2000/01, 2003, 2004, 2005, 2007 and 2008 Canadian Community Health Surveys (Statistics Canada); and Economic Burden of Illness 2000 Database. 2011. Available online: https://www.canada.ca/en/public-health/services/health-promotion/healthy-living/obesity-canada/health-economic-implications.html (accessed on 20 July 2021).



















| Author | Year of Publication | Country | Type of Outcomes (Specific Outcome [Type of Report]) | Natural Disaster | Type of PNMS | Timing of Exposure | Age of Assessment | Sample Size |
|---|---|---|---|---|---|---|---|---|
| Austin | 2017 | Australia | Cognitive (language abilities [maternal], cognitive functioning [third-party observer]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 30 months | 131 |
| Cai | 2017 | China | Cognitive (developmental quotient, mental index [third-party observer]) | 2008 Sichuan Earthquake | Psychological | Preconception included (3 years) | 0–4 years | 86 |
| Cao | 2014 | Canada | Motor (balance, bilateral coordination, visual motor integration [third-party observer]) | 1998 Quebec Ice Storm | Objective; psychological | No preconception | 5 ½ years | 89 |
| Cao-Lei | 2018 | Canada | Physiological (c-peptide [medical]) | 1998 Quebec Ice Storm | Objective; cognitive appraisal | Preconception included (3 months) | 13 ½ years | 30 |
| Dancause | 2013 | Canada | Physiological (insulin [medical]) | 1998 Quebec Ice Storm | Objective; psychological | Preconception included (1 month) | 13 ½ years | 32 |
| Dancause | 2015 | United States | Physical (body mass index, total adiposity, central adiposity [third-party observer]) | 2008 Iowa Flood | Objective; psychological | No preconception | 2 ½ and 4 years | 106 |
| Dancause | 2017 | Australia | Birth (birth weight, birth length, head circumference, head circumference to birth length ratio, ponderal index [medical]) | 2011 Queensland Flood | Diet | No preconception | Birth | 222 |
| Harville | 2016 | Haiti | Birth (birth weight [medical]) | 2010 Haiti Earthquake | Objective | Preconception included (20 ½ months) | Birth | 857 |
| Hilmert | 2016 | United States | Birth (birth weight, gestational age [medical]) | 2009 Red River Flood | Objective | No preconception | Birth | 136 |
| King | 2009 | Canada | Physical (dermatoglyphic asymmetry [third-party observer]) | 1998 Quebec Ice Storm | Objective; psychological; maternal cortisol | Preconception included (3 months) | 4; 5; 5 ½ years | 97 |
| Kroska | 2018 | United States | Physical (body mass index [third-party observer]) | 2008 Iowa Flood | Objective; psychological; cognitive appraisal | No preconception | 30 months | 103 |
| Laplante | 2004 | Canada | Cognitive (mental development index [third-party observer], productive and receptive language [maternal]) | 1998 Quebec Ice Storm | Objective; psychological | No preconception | 2 years | 58 |
| Laplante | 2007 | Canada | Cognitive (length of session, nonplay activity, functional play, stereotypical play, displayed hypotheses [third-party observer]) | 1998 Quebec Ice Storm | Objective; psychological | No preconception | 2 years | 52 |
| Laplante | 2008 | Canada | Cognitive (IQ, vocabulary [third-party observer]) | 1998 Quebec Ice Storm | Objective; psychological | No preconception | 5 ½ years | 89 |
| Laplante | 2016 | Canada | Socio-emotional (temperament: fussy/difficult, unadaptable, dull, needs attention [third-party observer]) | 1998 Quebec Ice Storm | Objective; psychological | No preconception | 6 months | 121 |
| Laplante | 2018 | United States | Cognitive (cognitive functioning [third-party observer], productive and receptive language [maternal]) | 2008 Iowa Flood | Objective; psychological | No preconception | 30 months | 132 |
| Laplante | 2019 | Australia | Behavioral (autistic spectrum disorder symptoms [maternal]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 30 months | 105 |
| Lequertier | 2019 | Australia | Socio-emotional (socio-emotional problems and competence [maternal]) | 2011 Queensland Flood | Objective; psychological | No preconception | 16 months | 125 |
| Liu | 2016 | Canada | Physical (body mass index, central adiposity [third-party observer]) | 1998 Quebec Ice Storm | Objective; psychological; cognitive appraisal | Preconception included (3 months) | 5 ½; 8 ½; 11 ½; 13 ½; 15 ½ years | 111 |
| McLean | 2018 | Australia | Behavioral (internalizing behavior [maternal and third-party observer], anxiety symptoms [maternal] | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 4 years | 115 |
| McLean | 2019 | Australia | Socio-emotional (temperament: negative reactivity, shy-inhibition (approach-withdrawal), attentional control (persistence) [maternal]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 16 months | 104 |
| McLean | 2020 | Australia | Physiological (cortisol [medical]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 16 months | 111 |
| Moss | 2017 | Australia | Cognitive (cognitive development); motor (fine and gross motor development [third-party observer]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 16 months | 145 |
| Moss | 2018 | Australia | Cognitive (cognitive development [third-party observer]); motor (fine and gross motor development [third-party observer]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 30 months | 150 |
| Nguyen | 2018 | Canada | Physiological (testosterone [medical], cortisol [medical]; behavioral (aggressive behavior [maternal]) | 1998 Quebec Ice Storm | Objective; psychological | Preconception included (3 months) | 11 ½ years | 59 |
| Pomer | 2018 | Vanuatu | Birth (birth weight [medical]) | 2015 Cyclone Pam | Objective; psychological; diet | Preconception included (3 months) | Birth | 70 |
| Sanguanklin | 2014 | Thailand | Birth (gestational age [medical]) | 2011 Thailand Flood | Objective | No preconception (third trimester only) | Birth | 175 |
| Simcock | 2016 | Australia | Motor (fine and gross motor development [maternal]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 2 months; 6 months; 16 months | 2 months (106); 6 months (115); 16 months (130) |
| Simcock | 2017a | Australia | Socio-emotional (personal-social skills [maternal]); cognitive (communication; problem-solving skills [maternal]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 6 months | 115 |
| Simcock | 2017b | Australia | Socio-emotional (temperament: approach, rhythmicity, cooperation-manageability, activity-reactivity, irritability [maternal]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 6 months | 121 |
| Simcock | 2018 | Australia | Motor (fine and gross motor development [maternal]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 2 ½ and 4 years | 2 ½ years (124) and 4 years (113) |
| Simcock | 2019 | Australia | Behavioral (sleep problems, attention problems, anxious/depressed symptoms [maternal]) | 2011 Queensland Flood | Objective; psychological; cognitive appraisal | No preconception | 2 ½ and 4 years | 2 ½ (134); 4 (118) |
| Strahm | 2020 | United States | Physiological (cortisol [medical]) | 2009 Red River Flood | Objective; maternal cortisol | No preconception | 9 years | 56 |
| Veru | 2015 | Canada | Physiological (lymphocytes, cytokines [medical]) | 1998 Quebec Ice Storm | Objective; psychological | Preconception included (3 months) | 13 years | 37 |
| Walder | 2014 | Canada | Behavioral (autistic traits [maternal]) | 1998 Quebec Ice Storm | Objective; psychological | No preconception | 6 ½ years | 89 |
| Yong Ping | 2015 | United States | Physiological (cortisol [medical]) | 2008 Iowa Flood | Objective; psychological | No preconception | 2 ½ years | 94 |
| Yong Ping | 2020 | Canada | Behavioral (internalizing and externalizing behavior [maternal]); physiological (cortisol [medical]) | 1998 Quebec Ice Storm | Objective; psychological | No preconception | 13 years | 45 |
| Factors/Type of Outcomes | Birth | Cognitive | Motor | Physical | Socio-Emotional | Behavioral |
|---|---|---|---|---|---|---|
| Type of PNMS | ||||||
| Objective hardship | 0.0618 ** | 0.1682 *** | 0.0994 ** | 0.1539 *** | 0.0679 * | 0.1225 *** |
| Psychological distress | 0.1178 *** | 0.0827 *** | 0.1532 *** | 0.0681 *** | 0.1118 *** | |
| Cognitive appraisal | 0.0082 | 0.0650 | −0.0674 | 0.0091 | 0.0318 | |
| Diet | 0.0555 * | |||||
| Type of natural disaster | ||||||
| Ice storm | 0.2389 *** | 0.1978 *** | 0.1316 *** | 0.1299 *** | 0.2643 *** | |
| Flood | 0.0329 | 0.0741 *** | 0.0597 | 0.0467 ** | 0.0752 *** | |
| Type of report | ||||||
| Maternal | 0.0633 | 0.0809 *** | 0.1040 *** | |||
| Third-party observer | 0.1607 *** | 0.0865 *** | 0.0236 | |||
| Timing of exposure | ||||||
| No preconception | 0.0480 ** | 0.0597 | ||||
| With preconception | 0.0737 * | 0.1316 *** | ||||
| Age | ||||||
| Under 10 | 0.0715 * | 0.0923 *** | ||||
| 10 or older | 0.1600 *** | 0.1449 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lafortune, S.; Laplante, D.P.; Elgbeili, G.; Li, X.; Lebel, S.; Dagenais, C.; King, S. Effect of Natural Disaster-Related Prenatal Maternal Stress on Child Development and Health: A Meta-Analytic Review. Int. J. Environ. Res. Public Health 2021, 18, 8332. https://doi.org/10.3390/ijerph18168332
Lafortune S, Laplante DP, Elgbeili G, Li X, Lebel S, Dagenais C, King S. Effect of Natural Disaster-Related Prenatal Maternal Stress on Child Development and Health: A Meta-Analytic Review. International Journal of Environmental Research and Public Health. 2021; 18(16):8332. https://doi.org/10.3390/ijerph18168332
Chicago/Turabian StyleLafortune, Sandra, David P. Laplante, Guillaume Elgbeili, Xinyuan Li, Stéphanie Lebel, Christian Dagenais, and Suzanne King. 2021. "Effect of Natural Disaster-Related Prenatal Maternal Stress on Child Development and Health: A Meta-Analytic Review" International Journal of Environmental Research and Public Health 18, no. 16: 8332. https://doi.org/10.3390/ijerph18168332
APA StyleLafortune, S., Laplante, D. P., Elgbeili, G., Li, X., Lebel, S., Dagenais, C., & King, S. (2021). Effect of Natural Disaster-Related Prenatal Maternal Stress on Child Development and Health: A Meta-Analytic Review. International Journal of Environmental Research and Public Health, 18(16), 8332. https://doi.org/10.3390/ijerph18168332