Population Response to Air Pollution and the Risk of Coronavirus Disease in Chinese Cities during the Early Pandemic Period
Abstract
:1. Introduction
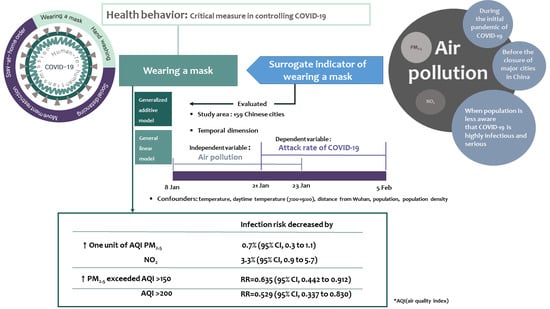
2. Materials and Methods
2.1. Study Area and Design
2.2. Data Collection
2.3. Data Analysis
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Gorbalenya, A.E.; Baker, S.C.; Baric, R.; Groot, R.J.D.; Drosten, C.; Gulyaeva, A.A.; Haagmans, B.L.; Lauber, C.; Leontovich, A.M.; Neuman, B.W.; et al. Severe acute respiratory syndrome-related coronavirus: The species and its viruses—A statement of the Coronavirus Study Group. bioRxiv 2020. [CrossRef] [Green Version]
- European Centre for Disease Prevention and Control. Outbreak of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): Increased Transmission beyond China—Fourth Update. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/SARS-CoV-2-risk-assessment-14-feb-2020.pdf (accessed on 8 March 2020).
- Johns Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE). Available online: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 (accessed on 21 October 2020).
- WHO. Coronavirus Disease (COVID-19): Masks. Available online: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-masks (accessed on 22 January 2021).
- IQAir. 2019 World Air Quality Report, Region & City PM2.5 Ranking. Available online: https://www.iqair.com/world-most-polluted-cities/world-air-quality-report-2019-en.pdf (accessed on 21 October 2020).
- Yang, Q.; Wu, S. Air pollution in China: Health information seeking and protective behaviors. Health Promot. Int. 2020, 35, 1495–1506. [Google Scholar] [CrossRef]
- Park, J.H.; Cheong, H.K.; Son, D.Y.; Kim, S.U.; Ha, C.M. Perceptions and behaviors related to hand hygiene for the prevention of H1N1 influenza transmission among Korean university students during the peak pandemic period. BMC Infect. Dis. 2010, 10, 222. [Google Scholar] [CrossRef] [Green Version]
- Sun, C.; Kahn, M.E.; Zheng, S. Self-protection investment exacerbates air pollution exposure inequality in urban China. Ecol. Econ. 2017, 131, 468–474. [Google Scholar] [CrossRef] [Green Version]
- Liu, T.; He, G.; Lau, A. Avoidance behavior against air pollution: Evidence from online search indices for anti-PM2.5 masks and air filters in Chinese cities. Environ. Econ. Policy Stud. 2017, 20, 325–363. [Google Scholar] [CrossRef]
- Zhang, J.; Mu, Q. Air pollution and defensive expenditures: Evidence from particulate-filtering facemask. J. Environ. Econ. Manag. 2018, 92, 517–536. [Google Scholar] [CrossRef]
- WHO. Timeline of WHO’s Response to COVID-19. Available online: https://www.who.int/news-room/detail/29-06-2020-covidtimeline (accessed on 21 October 2020).
- Lau, H.; Khosrawipour, V.; Kocbach, P.; Mikolajczyk, A.; Schubert, J.; Bania, J.; Khosrawipour, T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Travel Med. 2020, 27, taaa037. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ji, T.; Chen, H.L.; Xu, J.; Wu, L.N.; Li, J.J.; Chen, K.; Qin, G. Lockdown contained the spread of 2019 novel coronavirus disease in Huangshi City, China: Early epidemiological findings. Clin. Infect. Dis. 2020, 71, 1454–1460. [Google Scholar] [CrossRef] [PubMed]
- Backer, J.A.; Klinkenberg, D.; Wallinga, J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance 2020, 25, 2000062. [Google Scholar] [CrossRef] [Green Version]
- WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Available online: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf (accessed on 21 October 2020).
- DXY·DY Doctor. COVID-19 Global Pandemic Real-time Report. Available online: https://ncov.dxy.cn/ncovh5/view/pneumonia (accessed on 5 February 2020).
- Free Meteo. Available online: https://freemeteo.kr (accessed on 18 May 2020).
- World Air Quality Indicator Project Team. Air Quality Index. Available online: http://aqicn.org (accessed on 23 June 2020).
- National Bureau of Statistics of China. Available online: http://www.stats.gov.cn/English (accessed on 16 September 2020).
- Kang, D.; Choi, H.; Kim, J.H.; Choi, J. Spatial epidemic dynamics of the COVID-19 outbreak in China. Int. J. Infect. Dis. 2020, 94, 96–102. [Google Scholar] [CrossRef]
- Zhao, S.; Zhuang, Z.; Ran, J.; Lin, J.; Yang, G.; Yang, L.; He, D. The association between domestic train transportation and novel coronavirus (2019-nCoV) outbreak in China from 2019 to 2020: A data-driven correlational report. Travel Med. Infect. Dis. 2020, 33, 101568. [Google Scholar] [CrossRef]
- Dominici, F.; McDermott, A.; Zeger, S.L.; Samet, J.M. On the use of generalized additive models in time-series studies of air pollution and health. Am. J. Epidemiol. 2002, 156, 193–203. [Google Scholar] [CrossRef]
- Muggeo, V.M. Regression Models with Break-Points/Change-Points Estimation. Available online: https://cran.r-project.org/web/packages/segmented/segmented.pdf (accessed on 21 October 2020).
- Wu, X.; Nethery, R.C.; Sabath, B.M.; Braun, D.; Dominici, F. Exposure to air pollution and COVID-19 mortality in the United States: A nationwide cross-sectional study. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Liang, D.; Shi, L.; Zhao, J.; Liu, P.; Schwartz, J.; Gao, S.; Sarnat, J.; Liu, Y.; Ebelt, S.; Scovronick, N.; et al. Urban air pollution may enhance COVID-19 case-fatality and mortality rates in the United States. Innovation 2020, 1, 100047. [Google Scholar] [CrossRef]
- Yao, Y.; Pan, J.; Liu, Z.; Meng, X.; Wang, W.; Kan, H.; Wang, W. Temporal association between particulate matter pollution and case fatality rate of COVID-19 in Wuhan. Environ. Res. 2020, 189, 109941. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zhao, G.; Luo, L.; Li, Y.; Shi, W. Associations between ambient air pollutants exposure and case fatality rate of COVID-19: A multi-city ecological study in China. medRxiv 2020. [Google Scholar] [CrossRef]
- Chen, K.; Wang, M.; Huang, C.; Kinney, P.L.; Anastas, P.T. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet. Health 2020, 4, e210–e212. [Google Scholar] [CrossRef]
- He, G.; Pan, Y.; Tanaka, T. The short-term impacts of COVID-19 lockdown on urban air pollution in China. Nat. Sustain. 2020, 3, 1005–1011. [Google Scholar] [CrossRef]
- Setti, L.; Passarini, F.; De Gennaro, G.; Barbieri, P.; Licen, S.; Perrone, M.G.; Piazzalunga, A.; Borelli, M.; Palmisani, J.; Di Gilio, A.; et al. Potential role of particulate matter in the spreading of COVID-19 in Northern Italy: First observational study based on initial epidemic diffusion. BMJ Open 2020, 10, e039338. [Google Scholar] [CrossRef]
- Setti, L.; Passarini, F.; De Gennaro, G.; Barbieri, P.; Perrone, M.G.; Borelli, M.; Palmisani, J.; Di Gilio, A.; Piscitelli, P.; Miani, A. Airborne Transmission Route of COVID-19: Why 2 Meters/6 Feet of Inter-Personal Distance Could Not Be Enough. Int. J. Environ. Res. Public Health 2020, 17, 2932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stadnytskyi, V.; Bax, C.E.; Bax, A.; Anfinrud, P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc. Natl. Acad. Sci. USA 2020, 117, 11875–11877. [Google Scholar] [CrossRef] [PubMed]
- Cha, W.J. Hand Washing and Wearing Mask Prevention of Infectious Diseases Great Effect. Mecical Newspaper. Available online: http://m.healthcaren.com/news/news_article_yong.jsp?mn_idx=361421 (accessed on 26 October 2020).
- Rotko, T.; Oglesby, L.; Künzli, N.; Carrer, P.; Nieuwenhuijsen, M.J.; Jantunen, M. Determinants of perceived air pollution annoyance and association between annoyance scores and air pollution (PM2.5, NO2) concentrations in the European EXPOLIS study. Atmos. Environ. 2002, 36, 4593–4602. [Google Scholar] [CrossRef]
- Leung, N.H.; Chu, D.K.; Shiu, E.Y.; Chan, K.H.; McDevitt, J.J.; Hau, B.J.; Yen, H.L.; Li, Y.; Ip, D.K.; Peiris, J.M.; et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020, 26, 676–680. [Google Scholar] [CrossRef] [PubMed] [Green Version]







| Variable | Number of Cities 9 | Mean | Standard Deviation | Percentile | |||||
|---|---|---|---|---|---|---|---|---|---|
| Minimum | 25th | Median | 75th | Maximum | Inter-Quartile Range | ||||
| Cumulative cases | 159 | 42.90 | 57.06 | 10.00 | 15.00 | 24.00 | 45.00 | 376.00 | 30.00 |
| Attack rate/100,000 persons | 159 | 0.79 | 0.79 | 0.14 | 0.36 | 0.56 | 0.94 | 6.06 | 0.58 |
| PM2.5 (AQI) 1 | 159 | 145.93 | 41.85 | 56.44 | 112.94 | 146.06 | 177.63 | 244.31 | 64.69 |
| PM2.5 AQI level 2 | 159 | 3.38 | 0.90 | 2.00 | 3.00 | 3.00 | 4.00 | 5.00 | 1.00 |
| PM2.5 ≥ 150 AQI Days 3 | 159 | 7.52 | 5.35 | 0.00 | 2.00 | 8.00 | 12.00 | 16.00 | 10.00 |
| PM2.5 ≥ 100 AQI Days 4 | 159 | 12.19 | 4.28 | 0.00 | 9.00 | 14.00 | 16.00 | 16.00 | 7.00 |
| PM10 (AQI) 5 | 154 | 68.42 | 28.95 | 24.19 | 45.56 | 59.81 | 92.50 | 147.00 | 46.94 |
| NO2 (AQI) 6 | 154 | 17.65 | 7.45 | 2.75 | 12.44 | 17.22 | 22.69 | 37.06 | 10.25 |
| SO2 (AQI) 7 | 154 | 6.00 | 4.70 | 0.81 | 2.94 | 4.16 | 7.50 | 25.44 | 4.56 |
| O3 (AQI) 8 | 141 | 25.54 | 7.31 | 9.94 | 20.56 | 24.38 | 29.38 | 47.81 | 8.81 |
| Temperature (℃) | 159 | 4.32 | 8.47 | −18.10 | 0.80 | 4.05 | 8.77 | 24.00 | 7.96 |
| Day time temperature (7:00–19:00, ℃) | 159 | 5.45 | 8.25 | −16.65 | 2.45 | 4.91 | 9.39 | 25.79 | 6.94 |
| Population (1,000,000 persons) | 159 | 5.65 | 3.95 | 0.69 | 3.26 | 4.81 | 7.20 | 32.35 | 3.93 |
| Population density (persons/km2) | 158 | 621.15 | 672.83 | 23.00 | 270.00 | 508.00 | 700.00 | 6100.00 | 430.00 |
| Distance from Wuhan (km) | 159 | 784.64 | 449.66 | 172.00 | 527.00 | 705.00 | 927.00 | 2768.00 | 400.00 |
| Number of high-speed railway routes | 159 | 0.49 | 0.69 | 0.00 | 0.00 | 0.00 | 1.00 | 3.00 | 1.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoon, M.; Kim, J.-H.; Sung, J.; Lim, A.-Y.; Hwang, M.-J.; Kim, E.-H.; Cheong, H.-K. Population Response to Air Pollution and the Risk of Coronavirus Disease in Chinese Cities during the Early Pandemic Period. Int. J. Environ. Res. Public Health 2021, 18, 2248. https://doi.org/10.3390/ijerph18052248
Yoon M, Kim J-H, Sung J, Lim A-Y, Hwang M-J, Kim E-H, Cheong H-K. Population Response to Air Pollution and the Risk of Coronavirus Disease in Chinese Cities during the Early Pandemic Period. International Journal of Environmental Research and Public Health. 2021; 18(5):2248. https://doi.org/10.3390/ijerph18052248
Chicago/Turabian StyleYoon, Miryoung, Jong-Hun Kim, Jisun Sung, Ah-Young Lim, Myung-Jae Hwang, Eun-Hye Kim, and Hae-Kwan Cheong. 2021. "Population Response to Air Pollution and the Risk of Coronavirus Disease in Chinese Cities during the Early Pandemic Period" International Journal of Environmental Research and Public Health 18, no. 5: 2248. https://doi.org/10.3390/ijerph18052248
APA StyleYoon, M., Kim, J. -H., Sung, J., Lim, A. -Y., Hwang, M. -J., Kim, E. -H., & Cheong, H. -K. (2021). Population Response to Air Pollution and the Risk of Coronavirus Disease in Chinese Cities during the Early Pandemic Period. International Journal of Environmental Research and Public Health, 18(5), 2248. https://doi.org/10.3390/ijerph18052248