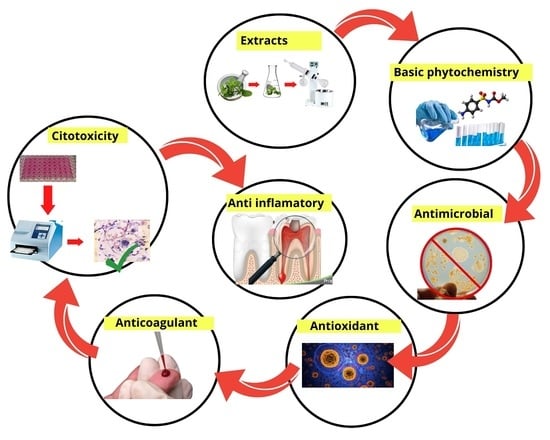
Preliminary Study of the Antimicrobial, Anticoagulant, Antioxidant, Cytotoxic, and Anti-Inflammatory Activity of Five Selected Plants with Therapeutic Application in Dentistry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals and Reagents
2.2. Cell Culture
2.3. Plant Material, Extraction, and Phytochemical Tests
2.4. Antimicrobial Assays
2.5. In Vitro Anticoagulant Assays
2.6. Antioxidant Activity Tests
2.7. Cytotoxic Activity Assays
2.8. Anti-Inflammatory Assays
2.9. Statistical Analysis
3. Results and Discussion
3.1. Phytochemical Tests
3.2. Antimicrobial Activity of Extracts
3.3. Anticoagulant Activity of Extracts
3.4. Antioxidant Activity of Extracts
3.5. Cytotoxic Activity of Extracts
3.6. Anti-Inflammatory Activity of Extracts
4. Conclusions
5. Future Perspectives
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murakami, S.; Mealey, B.L.; Mariotti, A.; Chapple, I.L.C. Dental plaque–induced gingival conditions. J. Clin. Periodontol. 2018, 45, S17–S27. [Google Scholar] [CrossRef] [PubMed]
- Loyola-Rodriguez, J.P.; Martinez-Martinez, R.E.; Flores-Ferreyra, B.I.; Patiño-Marin, N.; Alpuche-Solis, A.G.; Reyes-Macias, J.F. Distribution of Streptococcus mutans and Streptococcus sobrinus in saliva of Mexican preschool caries-free and caries-active children by microbial and molecular (PCR) assays. J. Clin. Pediatr. Dent. 2008, 32, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Li, J.W.; Wyllie, R.M.; Jensen, P.A. A Novel Competence Pathway in the Oral Pathogen Streptococcus sobrinus. J. Dent. Res. 2021, 100, 542–548. [Google Scholar] [CrossRef]
- Pitts, N.B.; Zero, D.T.; Marsh, P.D.; Ekstrand, K.; Weintraub, J.A.; Ramos-Gomez, F.; Tagami, J.; Twetman, S.; Tsakos, G.; Ismail, A. Dental caries. Nat. Rev. Dis. Prim. 2017, 3, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Smaïl-Faugeron, V.; Glenny, A.-M.; Courson, F.; Durieux, P.; Muller-Bolla, M.; Fron Chabouis, H. Pulp treatment for extensive decay in primary teeth. Cochrane Database Syst. Rev. 2018, 5, CD003220. [Google Scholar] [CrossRef]
- Calatayud, J.; Casado, I.; Álvarez, C. Análisis de los estudios clínicos sobre la eficacia de las técnicas alternatives al formocresol en las pulpotomías de dientes temporales. Av. Odontoestomatol. 2006, 22, 229–239. [Google Scholar] [CrossRef] [Green Version]
- Lewis, B. The obsolescence of formocresol. Br. Dent. J. 2009, 207, 525–528. [Google Scholar] [CrossRef] [Green Version]
- Elizondo-Luévano, J.H.; Hernández-García, M.E.; Pérez-Narváez, O.A.; Castro-Ríos, R.; Chávez-Montes, A. Berberina, curcumina y quercetina como potenciales agentes con capacidad antiparasitaria. Rev. Biol. Trop. 2020, 68, 1241–1249. [Google Scholar] [CrossRef]
- Elizondo-Luévano, J.H.; Castro-Ríos, R.; Sánchez-García, E.; Hernández-García, M.E.; Vargas-Villarreal, J.; Rodríguez-Luis, O.E.; Chávez-Montes, A. In Vitro Study of Antiamoebic Activity of Methanol Extracts of Argemone mexicana on Trophozoites of Entamoeba histolytica HM1-IMSS. Can. J. Infect. Dis. Med. Microbiol. 2018, 2018, 7453787. [Google Scholar] [CrossRef]
- Hernández-Martinez, H.C.; Gómez-Flores, R.; Tamez-Guerra, P.; Quintanilla-Licea, R.; Samaniego-Escamilla, M.A.; Monreal-Cuevas, E.; Tamez-Guerra, R.; Rodriguez-Padilla, C. Antitumor activity of Pachycereus marginatus (DC.) Britton Rose extracts against murine lymphoma L5178Y-R and skin melanoma B16F10 cells. J. Med. Plants Res. 2016, 10, 635–639. [Google Scholar] [CrossRef] [Green Version]
- Cárdenas Garza, G.R.; Elizondo Luévano, J.H.; Bazaldúa Rodríguez, A.F.; Chávez Montes, A.; Pérez Hernández, R.A.; Martínez Delgado, A.J.; López Villarreal, S.M.; Rodríguez Rodríguez, J.; Sánchez Casas, R.M.; Castillo Velázquez, U.; et al. Benefits of Cardamom (Elettaria cardamomum (L.) Maton) and Turmeric (Curcuma longa L.) Extracts for Their Applications as Natural Anti-Inflammatory Adjuvants. Plants 2021, 10, 1908. [Google Scholar] [CrossRef]
- Rai, P.K.; Lalramnghinglova, H. Ethnomedicinal Plant Resources of Mizoram, India: Implication of Traditional Knowledge in Health Care System. Ethnobot. Leafl. 2010, 14, 274–305. [Google Scholar]
- Mahomoodally, M.F. Traditional Medicines in Africa: An Appraisal of Ten Potent African Medicinal Plants. Evid. Based Complement Altern. Med. 2013, 2013, 617459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamath, N.P.; Tandon, S.; Nayak, R.; Naidu, S.; Anand, P.S.; Kamath, Y.S. The effect of Aloe vera and tea tree oil mouthwashes on the oral health of school children. Eur. Arch. Paediatr. Dent. Off. J. Eur. Acad. Paediatr. Dent. 2020, 21, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Dragos, D.; Gilca, M.; Gaman, L.; Vlad, A.; Iosif, L.; Stoian, I.; Lupescu, O. Phytomedicine in joint disorders. Nutrients 2017, 9, 70. [Google Scholar] [CrossRef]
- Ferreira, T.L.; Evangelista, A.J.J. Mimosa tenuiflora’s antimicrobial activity on bacteria and fungi from medical importance: An integrative review. Arch. Microbiol. 2021, 203, 3399–3406. [Google Scholar] [CrossRef]
- Miller, A.B.; Cates, R.G.; Lawrence, M.; Soria, J.A.F.; Espinoza, L.V.; Martinez, J.V.; Arbizú, D.A. The antibacterial and antifungal activity of essential oils extracted from Guatemalan medicinal plants. Pharm. Biol. 2015, 53, 548–554. [Google Scholar] [CrossRef] [Green Version]
- Marchese, A.; Barbieri, R.; Coppo, E.; Orhan, I.E.; Daglia, M.; Nabavi, S.F.; Izadi, M.; Abdollahi, M.; Nabavi, S.M.; Ajami, M. Antimicrobial activity of eugenol and essential oils containing eugenol: A mechanistic viewpoint. Crit. Rev. Microbiol. 2017, 43, 668–689. [Google Scholar] [CrossRef]
- Del Angel-Mosqueda, C.; Hernandez-Delgadillo, R.; Rodríguez-Luis, O.E.; Ramírez-Rodríguez, M.T.; Munguía-Moreno, S.; Zavala-Alonso, N.V.; Solís-Soto, J.M.; Nakagoshi-Cepeda, M.A.A.; Sánchez-Nájera, R.I.; Nakagoshi-Cepeda, S.E.; et al. Hydroxyapatite decreases cytotoxicity of a glass ionomer cement by calcium fluoride uptake in vitro. J. Appl. Biomater. Funct. Mater. 2018, 16, 42–46. [Google Scholar] [CrossRef] [Green Version]
- Bazaldúa-Rodríguez, A.F.; Quintanilla-Licea, R.; Verde-Star, M.J.; Hernández-García, M.E.; Vargas-Villarreal, J.; Garza-González, J.N. Furanocoumarins from Ruta chalepensis with amebicide activity. Molecules 2021, 26, 3684. [Google Scholar] [CrossRef]
- Sanabria-Galindo, A.; López, S.I.; Gualdrón, R. Estudio fitoquimico preliminar y letalidad sobre Artemia salina de plantas colombianas. Rev. Col. Cienc. Quím. Farm. 1997, 26, 15–19. [Google Scholar]
- Coe, F.G.; Anderson, G.J. Screening of medicinal plants used by the Garífuna of Eastern Nicaragua for bioactive compounds. J. Ethnopharmacol. 1996, 53, 29–50. [Google Scholar] [CrossRef] [Green Version]
- Farnsworth, N.R. Biological and phytochemical screening of plants. J. Pharm. Sci. 1966, 55, 225–276. [Google Scholar] [CrossRef] [PubMed]
- Boiss, B.; Sadaf, H.M.; Bibi, Y.; Ishaque, M.; Nisa, S.; Qayyum, A.; Safdar, N.; Shah, Z.H.; Alsamadany, H.; Chung, G. Determination of ROS Scavenging, Antibacterial and Antifungal Potential of Methanolic Extract of Otostegia limbata (Benth.) Boiss. Plants 2021, 10, 2360. [Google Scholar] [CrossRef]
- Mira, A.; Alkhiary, W.; Shimizu, K. Antiplatelet and Anticoagulant Activities of Angelica shikokiana Extract and Its Isolated Compounds. Clin. Appl. Thromb. 2017, 23, 91–99. [Google Scholar] [CrossRef] [Green Version]
- Elizondo-Luévano, J.H.; Pérez-Narváez, O.A.; Sánchez-García, E.; Castro-Ríos, R.; Hernández-García, M.E.; Chávez-Montes, A. In-vitro effect of Kalanchoe daigremontiana and its main component, quercetin against Entamoeba histolytica and Trichomonas vaginalis. Iran. J. Parasitol. 2021, 16, 394–401. [Google Scholar] [CrossRef]
- Lindhagen, E.; Nygren, P.; Larsson, R. The fluorometric microculture cytotoxicity assay. Nat. Protoc. 2008, 3, 1364–1369. [Google Scholar] [CrossRef]
- Ramírez-Villalobos, J.M.; Romo-Sáenz, C.I.; Morán-Santibañez, K.S.; Tamez-Guerra, P.; Quintanilla-Licea, R.; Orozco-Flores, A.A.; Romero-Arguelles, R.; Tamez-Guerra, R.; Rodríguez-Padilla, C.; Gomez-Flores, R. In vitro tumor cell growth inhibition induced by Lophocereus marginatus (Dc.) S. Arias and terrazas endophytic fungi extracts. Int. J. Environ. Res. Public Health 2021, 18, 9917. [Google Scholar] [CrossRef]
- Nigenda, G.; Mora-Flores, G.; Aldama-López, S.; Orozco-Núñez, E. La práctica de la medicina tradicional en América Latina y el Caribe: El dilema entre regulación y tolerancia. Salud Publica Mex. 2001, 43, 41–51. [Google Scholar] [CrossRef] [Green Version]
- Pérez, K.C.; Galaviz, L.; Iracheta, J.M.; Lucero, E.A.; Molina, Z.J. Actividad contra Trypanosoma cruzi (Kinetoplastida: Trypanosomatidae) de extractos metanólicos de plantas de uso medicinal en México. Rev. Biol. Trop. 2017, 65, 1459–1469. [Google Scholar] [CrossRef] [Green Version]
- Jacobo-Herrera, N.J.; Jacobo-Herrera, F.E.; Zentella-Dehesa, A.; Andrade-Cetto, A.; Heinrich, M.; Pérez-Plasencia, C. Medicinal plants used in Mexican traditional medicine for the treatment of colorectal cancer. J. Ethnopharmacol. 2016, 179, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Pacheco-ordaz, A.; Sánchez-García, E.; Quintanilla-Licea, R.; Bazaldúa-Rodríguez, A.F.; Pérez-Hernández, R.A.; Hernández-García, M.E.; Báez-González, J.G.; Castro-Ríos, R.; Elizondo-Luévano, J.H.; Chávez-Montes, A. Amoebicidal and trichomonicidal capacity of polymeric nanoparticles loaded with extracts of the plants Curcuma longa (Zingiberaceae) and Berberis vulgaris (Berberidaceae). Rev. Biol. Trop. 2022, 70, 319–331. [Google Scholar] [CrossRef]
- Elizondo-Luévano, J.H.; Castro-Ríos, R.; Vicente, B.; Fernández-Soto, P.; López-Aban, J.; Muro, A.; Chávez-Montes, A. In vitro antischistosomal activity of the Argemone mexicana methanolic extract and its main component berberine. Iran. J. Parasitol. 2021, 16, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Pina-Barrera, A.M.; Alvarez-Roman, R.; Baez-Gonzalez, J.G.; Amaya-Guerra, C.A.; Rivas-Morales, C.; Gallardo-Rivera, C.T.; Galindo-Rodriguez, S.A. Application of a Multisystem Coating Based on Polymeric Nanocapsules Containing Essential Oil of Thymus vulgaris L. To Increase the Shelf Life of Table Grapes (Vitis vinifera L.). IEEE Trans. Nanobiosci. 2019, 18, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Luis, O.; Verde-Star, J.; González-Horta, A.; Báez-González, G.; Castro-Ríos, R.; Sánchez-García, E.; Chávez-Montes, A. Preparation of polymer nanoparticles loaded with Syzygium aromaticum essential oil: An oral potential application. Bol. Latinoam. Caribe Plantas Med. Aromat. 2020, 19, 65–76. [Google Scholar]
- Le Bourvellec, C.; Bureau, S.; Renard, C.M.G.C.; Plenet, D.; Gautier, H.; Touloumet, L.; Girard, T.; Simon, S. Cultivar and year rather than agricultural practices affect primary and secondary metabolites in apple fruit. PLoS ONE 2015, 10, e0141916. [Google Scholar] [CrossRef]
- Figuero, E.; Nóbrega, D.F.; García-Gargallo, M.; Tenuta, L.M.A.; Herrera, D.; Carvalho, J.C. Mechanical and chemical plaque control in the simultaneous management of gingivitis and caries: A systematic review. J. Clin. Periodontol. 2017, 44, S116–S134. [Google Scholar] [CrossRef] [Green Version]
- Delgado, A.J.M.; Velázquez, U.C.; González, J.G.B.; Montes, A.C.; Villarreal, S.M.L.; García, L.E.V.; Casas, R.M.S.; Luis, O.E.R. Evaluation of the Essential Oil of Citrus paradisi as an Alternative Treatment against Candida albicans. Open J. Stomatol. 2020, 10, 258–270. [Google Scholar] [CrossRef]
- Bhavikatti, S.K.; Karobari, M.I.; Zainuddin, S.L.A.; Marya, A.; Nadaf, S.J.; Sawant, V.J.; Patil, S.B.; Venugopal, A.; Messina, P.; Scardina, G.A. Investigating the Antioxidant and Cytocompatibility of Mimusops elengi Linn Extract over Human Gingival Fibroblast Cells. Int. J. Environ. Res. Public Health 2021, 18, 7162. [Google Scholar] [CrossRef]
- Elizondo-Luévano, J.H.; Castro-Ríos, R.; López-Abán, J.; Gorgojo-Galindo, O.; Fernández-Soto, P.; Vicente, B.; Muro, A.; Chávez-Montes, A. Berberine: A nematocidal alkaloid from Argemone mexicana against Strongyloides venezuelensis. Exp. Parasitol. 2021, 220, 108043. [Google Scholar] [CrossRef]
- Mekhfi, H.; El Haouari, M.; Legssyer, A.; Bnouham, M.; Aziz, M.; Atmani, F.; Remmal, A.; Ziyyat, A. Platelet anti-aggregant property of some Moroccan medicinal plants. J. Ethnopharmacol. 2004, 94, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Asghar, M.A.; Yousuf, R.I.; Shoaib, M.H.; Asghar, M.A. Antibacterial, anticoagulant and cytotoxic evaluation of biocompatible nanocomposite of chitosan loaded green synthesized bioinspired silver nanoparticles. Int. J. Biol. Macromol. 2020, 160, 934–943. [Google Scholar] [CrossRef] [PubMed]
- Mahdi-Pour, B.; Jothy, S.L.; Latha, L.Y.; Chen, Y.; Sasidharan, S. Antioxidant activity of methanol extracts of different parts of Lantana Camara Asian Pac. J. Trop. Biomed. 2012, 2, 960–965. [Google Scholar] [CrossRef] [Green Version]
- Baby, B.; Antony, P.; Vijayan, R. Antioxidant and anticancer properties of berries. Crit. Rev. Food Sci. Nutr. 2018, 58, 2491–2507. [Google Scholar] [CrossRef] [PubMed]
- Tufinio-Miranda, K.; Ames-Canchaya, H.; Vergara-Sotomayor, A.; Fukusaki-Yoshizawa, A.; Paucar-Cuba, K. Determination of the antioxidant activity of Buddleja inkana, Oreocallis grandiflora and Chuquiraga spinosa. Rev. la Soc. Química del Perú. 2021, 87, 107–119. [Google Scholar] [CrossRef]
- Aberoumand, A.; Deokule, S.S. Comparison of phenolic compounds of some edible plants of Iran and India. Pak. J. Nutr. 2008, 7, 582–585. [Google Scholar] [CrossRef] [Green Version]
- Romero-Arguelles, R.; Morán-Santibáñez, K.; Tamez-guerra, P.; Quintanilla-Licea, R.; Orozco-Flores, A.A.; Ramírez-Villalobos, J.M.; Tamez-guerra, R.; Rodríguez-Padilla, C.; Gomez-Flores, R. In Vitro Antitumor Activity of Endophytic and Rhizosphere Gram-Positive Bacteria from Ibervillea sonorae (S. Watson) Greene against L5178Y-R Lymphoma Cells. Int. J. Environ. Res. Public Health 2022, 19, 894. [Google Scholar] [CrossRef]
- Alonso-Castro, A.J.; Villarreal, M.L.; Salazar-Olivo, L.A.; Gomez-Sanchez, M.; Dominguez, F.; Garcia-Carranca, A. Mexican medicinal plants used for cancer treatment: Pharmacological, phytochemical and ethnobotanical studies. J. Ethnopharmacol. 2011, 133, 945–972. [Google Scholar] [CrossRef]
- Wang, Y.; Che, M.; Xin, J.; Zheng, Z.; Li, J.; Zhang, S. The role of IL-1β and TNF-α in intervertebral disc degeneration. Biomed. Pharmacother. 2020, 131, 110660. [Google Scholar] [CrossRef]
- Ramírez Alvarado, M.M.; Sánchez Roitz, C. El factor de necrosis tumoral-α, la resistencia a la insulina, el metabolismo de lipoproteínas y la obesidad en humanos. Nutr. Hosp. 2012, 27, 1751–1757. [Google Scholar] [CrossRef]
- Locksley, R.M.; Killeen, N.; Lenardo, M.J. The TNF and TNF Receptor Superfamilies: Integrating Mammalian Biology. Cell 2001, 104, 487–501. [Google Scholar] [CrossRef] [Green Version]
- Komakech, R.; Kim, Y.-G.; Matsabisa, G.M.; Kang, Y. Anti-inflammatory and analgesic potential of Tamarindus indica Linn. (Fabaceae): A narrative review. Integr. Med. Res. 2019, 8, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Marzanna, H.; Dziedzic, K. Aloe vera (L.) Webb.: Natural Sources of Antioxidants—A Review. Plant Foods Hum. Nutr. 2019, 74, 255–265. [Google Scholar]
- Lima Bezerra, J.J.; Vieira Pinheiro, A.A.; Barbosa Lucena, R. Phytochemistry and teratogenic potential of Mimosa tenuiflora (willd.) poir. (Fabaceae) in ruminants: A systematic review. Toxicon 2021, 195, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Bent, R.; Moll, L.; Grabbe, S.; Bros, M. Interleukin-1 beta—A friend or foe in malignancies? Int. J. Mol. Sci. 2018, 19, 2155. [Google Scholar] [CrossRef] [Green Version]
- Massaro, H.; Zambelli, L.F.A.; de Britto, A.A.; Vieira, R.P.; Ligeiro-de-Oliveira, A.P.; Andia, D.C.; Oliveira, M.T.; Lima, A.F. Solvent and HEMA Increase Adhesive Toxicity and Cytokine Release from Dental Pulp Cells. Materials 2019, 12, 2750. [Google Scholar] [CrossRef] [Green Version]
- Yuan, L.; You, H.; Qin, N.; Zuo, W. Interleukin-10 Modulates the Metabolism and Osteogenesis of Human Dental Pulp Stem Cells. Cell. Reprogram. 2021, 23, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Fonseca-Camarillo, G.; Furuzawa-Carballedab, J.; Martínez-Benítezc, B.; Barreto-Zúñigad, R.; Yamamoto-Furushoa, K. Expresión de la interleucina (IL-10) con función inmunorreguladora en mucosa de pacientes con colitis ulcerosa crónica idiopática. Rev. Gastroenterol. Mex. 2011, 76, 113–119. [Google Scholar]
- Sandner, G.; Heckmann, M.; Weghuber, J. Immunomodulatory activities of selected essential oils. Biomolecules 2020, 10, 1139. [Google Scholar] [CrossRef]
- Batiha, G.E.S.; Alkazmi, L.M.; Wasef, L.G.; Beshbishy, A.M.; Nadwa, E.H.; Rashwan, E.K. Syzygium aromaticum L. (Myrtaceae): Traditional uses, bioactive chemical constituents, pharmacological and toxicological activities. Biomolecules 2020, 10, 202. [Google Scholar] [CrossRef] [Green Version]


| Family | Plant Species | Common Name | Part Used |
|---|---|---|---|
| Xanthorrhoeaceae | Aloe vera (L.) Burm.f. | Aloe or Sabila | Leaves |
| Equisetaceae | Equisetum arvense L. | Horsetail | Aerial part |
| Leguminosae | Mimosa tenuiflora (Willd.) Poir. | Tepezcohuite | Bark |
| Verbenaceae | Lippia graveolens Kunth. | Mexican oregano | Leaves |
| Myrtaceae | Syzygium aromaticum (L.) Merr. and L.M.Perry. | Clove | Buttons |
| Test | Chemical Groups | A. vera | E. arvense | M. tenuiflora | L. graveolens | S. aromaticum |
|---|---|---|---|---|---|---|
| KMnO4 | Unsaturations | + | + | + | + | + |
| Antrone | Carbohydrates | + | + | + | + | − |
| Lieberman–Burchard | Sterols, triterpenes | − | + | + | + | + |
| Shinoda | Flavonoids | + | − | + | + | + |
| NaOH | Coumarins | − | + | − | + | + |
| Baljet | Sesquiterpene lactones | − | − | + | + | + |
| Sulfuric acid | Quinones | − | − | + | + | + |
| NaHCO3 | Carboxyl group | + | − | − | − | − |
| Ferric chloride | Tannins | − | − | + | + | + |
| Dragendorff | Alkaloids | − | − | + | − | − |
| Yield % | 11.16 | 5.23 | 17.84 | 8.81 | 7.20 |
| Plant Extracts vs. S. mutans (Zone of Inhibition in mm) | |||||
|---|---|---|---|---|---|
| Concentration (µg/mL) | A. vera | E. arvense | M. tenuiflora | L. graveolens | S. aromaticum |
| 250 | 10.67 ± 0.88 | 15.33 ± 1.53 | 15.52 ± 0.33 | 25.33 ± 1.05 ** | 16.33 ± 0.58 |
| 500 | 13.67 ± 0.58 | 16.67 ± 3.06 | 16.00 ± 2.65 | 26.00 ± 0.41 ** | 17.00 ± 1.00 |
| 1000 | 16.00 ± 1.00 | 20.00 ± 2.00 * | 17.67 ± 0.80 * | 26.33 ± 1.15 ** | 18.00 ± 1.34 * |
| 2000 | 16.33 ± 0.85 | 22.67 ± 1.58 ** | 18.00 ± 1.00 * | 27.67 ± 1.85 ** | 19.67 ± 0.58 * |
| 3000 | 18.67 ± 1.15 * | 26.00 ± 2.04 ** | 18.33 ± 2.08 * | 28.48 ± 1.33 ** | 28.67 ± 0.98 ** |
| C+ | 15.10 ± 0.77 | 15.79 ± 0.58 | 15.00 ± 1.00 | 15.00 ± 1.67 | 16.00 ± 0.81 |
| p-ANOVA | >0.05 | >0.01 | >0.05 | >0.01 | >0.01 |
| Plant Extracts vs. S. sorbinus (Zone of Inhibition in mm) | |||||
|---|---|---|---|---|---|
| Concentration (µg/mL) | A. vera | E. arvense | M. tenuiflora | L. graveolens | S. aromaticum |
| 250 | 11.00 ± 1.05 | 8.77 ± 0.41 | 10.52 ± 1.80 | 15.67 ± 0.08 | 10.52 ± 0.05 |
| 500 | 16.67 ± 1.08 | 12.00 ± 0.89 | 14.00 ± 0.37 | 18.00 ± 1.03 * | 15.67 ± 0.50 |
| 1000 | 18.00 ± 1.11 * | 13.67 ± 1.58 | 15.67 ± 1.18 | 19.33 ± 1.53 * | 16.00 ± 0.46 |
| 2000 | 18.67 ± 1.53 * | 15.76 ± 0.85 | 16.33 ± 0.58 | 23.67 ± 2.33 ** | 19.41 ± 0.58 * |
| 3000 | 19.67 ± 0.58 * | 16.00 ± 1.14 | 19.67 ± 0.13 * | 25.67 ± 0.82 ** | 23.67 ± 1.53 ** |
| C+ | 15.10 ± 0.77 | 15.79 ± 0.58 | 15.00 ± 1.00 | 15.00 ± 1.67 | 16.00 ± 0.81 |
| p-ANOVA | >0.05 | >0.05 | >0.05 | >0.01 | >0.01 |
| Plant extract | DPPH Scavenging (IC50 in μg/mL) |
|---|---|
| A. vera | 8.66 ± 1.42 b |
| E. arvense | 2.73 ± 0.87 a |
| M. tenuiflora | 464.06 ± 8.58 e |
| L. graveolens | 19.80 ± 1.37 c |
| S. aromaticum | 37.20 ± 2.88 d |
| C+ (Vitamin C) | 2.23 ± 0.42 a |
| Plant Extracts | |||||
|---|---|---|---|---|---|
| Concentration (µg/mL) | A. vera | E. arvense | M. tenuiflora | L. graveolens | S. aromaticum |
| 125 | 99.00 ± 0.11 a | 89.42 ± 3.52 d | 91.11 ± 3.71 b | 84.60 ± 3.21 b | 88.04 ± 1.36 d |
| 250 | 99.00 ± 2.28 a | 81.68 ± 4.34 c | 86..99 ± 5.69 b | 79.53 ± 3.50 b | 75.89 ± 0.42 c |
| 500 | 99.04 ± 3.29 a | 61.12 ± 1.40 b | 58.07 ± 3.72 a | 72.31 ± 0.81 ab | 50.71 ± 0.34 b |
| 1000 | 96.71 ± 3.90 a | 8.03 ± 1.08 a | 55.95 ± 4.52 a | 62.50 ± 2.26 a | 6.10 ± 1.02 a |
| C− | 100.00 ± 0.00 a | 100.00 ± 0.00 e | 99.32 ± 0.65 c | 100.00 ± 0.00 c | 97.26 ± 0.92 e |
| IC50 (μg/mL) | >3000 | 560.62 | 1037.43 | 1384.70 | 497.51 |
| LL | ND | 510.51 | 953.25 | 1217.02 | 449.46 |
| UL | ND | 590.42 | 1161.09 | 1552.65 | 550.93 |
| IL Levels (pg/mL) | ||||
|---|---|---|---|---|
| Extract | Hr | TNF-α | IL-1 β | IL-10 |
| A. vera | 0 | 128.35 | 303.17 | 85.40 |
| 24 | 0.00 | 154.83 | 19.40 | |
| 48 | 0.00 | 219.83 | 0.00 | |
| 72 | 0.00 | 251.50 | 0.00 | |
| p-ANOVA | >0.001 | >0.05 | >0.001 | |
| E. arvense | 0 | 39.10 | 105.67 | 62.90 |
| 24 | 0.00 | 156.36 | 20.90 | |
| 48 | 68.60 | 181.08 | 85.40 | |
| 72 | 222.62 | 410.25 | 138.40 | |
| p-ANOVA | >0.001 | >0.01 | >0.01 | |
| M. tenuiflora | 0 | 378.63 | 21.92 | 0.00 |
| 24 | 376.10 | 64.42 | 0.00 | |
| 48 | 156.60 | 100.25 | 24.90 | |
| 72 | 7.66 | 189.00 | 60.40 | |
| p-ANOVA | >0.05 | >0.05 | >0.01 | |
| L. graveolens | 0 | 0.00 | 251.50 | 17.40 |
| 24 | 0.00 | 236.92 | 28.90 | |
| 48 | 19.11 | 117.33 | 76.40 | |
| 72 | 116.10 | 112.33 | 97.40 | |
| p-ANOVA | >0.01 | >0.01 | >0.05 | |
| S. aromaticum | 0 | 354.61 | 179.83 | 5.90 |
| 24 | 327.10 | 156.08 | 0.00 | |
| 48 | 304.35 | 132.75 | 26.40 | |
| 72 | 239.60 | 110.25 | 0.00 | |
| p-ANOVA | >0.05 | >0.05 | >0.01 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López Villarreal, S.M.; Elizondo Luévano, J.H.; Pérez Hernández, R.A.; Sánchez García, E.; Verde Star, M.J.; Castro Ríos, R.; Garza Tapia, M.; Rodríguez Luis, O.E.; Chávez Montes, A. Preliminary Study of the Antimicrobial, Anticoagulant, Antioxidant, Cytotoxic, and Anti-Inflammatory Activity of Five Selected Plants with Therapeutic Application in Dentistry. Int. J. Environ. Res. Public Health 2022, 19, 7927. https://doi.org/10.3390/ijerph19137927
López Villarreal SM, Elizondo Luévano JH, Pérez Hernández RA, Sánchez García E, Verde Star MJ, Castro Ríos R, Garza Tapia M, Rodríguez Luis OE, Chávez Montes A. Preliminary Study of the Antimicrobial, Anticoagulant, Antioxidant, Cytotoxic, and Anti-Inflammatory Activity of Five Selected Plants with Therapeutic Application in Dentistry. International Journal of Environmental Research and Public Health. 2022; 19(13):7927. https://doi.org/10.3390/ijerph19137927
Chicago/Turabian StyleLópez Villarreal, Sonia M., Joel H. Elizondo Luévano, Raymundo A. Pérez Hernández, Eduardo Sánchez García, María J. Verde Star, Roció Castro Ríos, Marsela Garza Tapia, Osvelia E. Rodríguez Luis, and Abelardo Chávez Montes. 2022. "Preliminary Study of the Antimicrobial, Anticoagulant, Antioxidant, Cytotoxic, and Anti-Inflammatory Activity of Five Selected Plants with Therapeutic Application in Dentistry" International Journal of Environmental Research and Public Health 19, no. 13: 7927. https://doi.org/10.3390/ijerph19137927
APA StyleLópez Villarreal, S. M., Elizondo Luévano, J. H., Pérez Hernández, R. A., Sánchez García, E., Verde Star, M. J., Castro Ríos, R., Garza Tapia, M., Rodríguez Luis, O. E., & Chávez Montes, A. (2022). Preliminary Study of the Antimicrobial, Anticoagulant, Antioxidant, Cytotoxic, and Anti-Inflammatory Activity of Five Selected Plants with Therapeutic Application in Dentistry. International Journal of Environmental Research and Public Health, 19(13), 7927. https://doi.org/10.3390/ijerph19137927