Epidemiological Characteristics of COVID-19 Cases in Non-Italian Nationals in Sicily: Identifying Vulnerable Groups in the Context of the COVID-19 Pandemic in Sicily, Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
- Non-severe clinical outcome (NSCO);
- Severe clinical outcome (SCO).
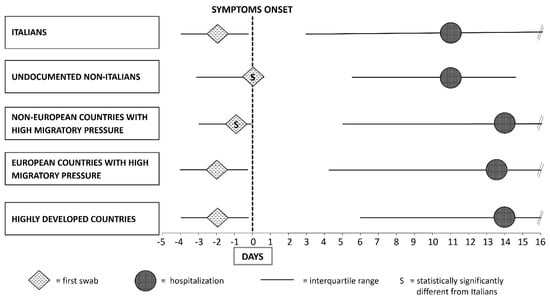
- Highly developed countries (European countries except those of Central–Eastern Europe, North America, Israel, Japan and Oceania);
- European countries with High Migratory Pressure (Central and Eastern Europe);
- Non-European countries with High Migratory Pressure (Africa, Asia, Central and South America).
2.2. Statistical Analysis
3. Results
3.1. Socio-Demographic Characteristics and Time of Diagnosis
3.2. Univariable Analyses
3.3. Multivariable Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. COVID-19 Epi Summary. 2021. Available online: https://covid19.who.int (accessed on 29 December 2021).
- World Health Organization Regional Office for Europe. Interim Guidance for Refugee and Migrant Health in Relation to COVID-19 in the WHO European Region. 2020. Available online: https://www.euro.who.int/__data/assets/pdf_file/0008/434978/Interim-guidance-refugee-and-migrant-health-COVID-19.pdf (accessed on 28 January 2022).
- Office of the High Commissioner for Human Rights. The Rights and Health of Refugees, Migrants and Stateless Must Be Protected in COVID-19 Response. Joint Press Release. 2020. Available online: https://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx (accessed on 28 January 2022).
- World Health Organization Regional Office for Europe. A Review of the Evidence on Health Status for Undocumented Migrants in the European Region. 2015. Available online: http://www.euro.who.int/__data/assets/pdf_file/0004/289255/WHO-HEN-Report-A5-3-Undocumented_FINAL-rev1.pdf?ua=1 (accessed on 28 January 2022).
- United Nations. COVID-19 and Human Rights: We Are All in This Together. Policy Brief. 76y. 2020. Available online: https://www.un.org/sites/un2.un.org/files/un_policy_brief_on_human_rights_and_covid_23_april_2020.pdf (accessed on 28 January 2022).
- World Health Organization. Considerations in Adjusting Public Health and Social Measures in the Context of COVID-19. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/331773/WHO-2019-nCoV-Adjusting_PH_measures-2020.1-eng.pdf (accessed on 28 January 2022).
- International Labour Organization. COVID-19 and the World of Work: Impacts and Responses. 2020. Available online: https://www.ilo.org/wcmsp5/groups/public/---dgreports/---dcomm/documents/briefingnote/wcms_738753.pdf (accessed on 28 January 2022).
- United Nation Women. In Focus: Gender Equality Matters in COVID-19 Response. 2020. Available online: https://www.unwomen.org/en/news/in-focus/in-focus-gender-equality-in-covid-19-response (accessed on 28 January 2022).
- Frontex. Situation at EU External Borders—Detections Down Because of Drop in Eastern Mediterranean. 2021. Available online: https://frontex.europa.eu/media-centre/news/news-release/situation-at-eu-external-borders-detections-down-because-of-drop-in-eastern-mediterranean-DLPwqm (accessed on 28 January 2022).
- European Commision. Migration Statistics Update: The Impact of COVID-19. 2021. Available online: https://ec.europa.eu/commission/presscorner/detail/en/ip_21_232 (accessed on 28 January 2022).
- Organisation for Economic Co-Operation and Development. Stocks of Foreign-Born Population in OECD Countries. 2020. Available online: https://data.oecd.org/migration/stocks-of-foreign-born-population-in-oecd-countries.htm (accessed on 28 January 2022).
- Centers for Disease Control and Prevention. Reducing Stigma. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/reducing-stigma.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fsymptoms-testing%2Freducing-stigma.html (accessed on 28 January 2022).
- Istituto Superiore di Sanita’. Dati Della Sorveglianza Integrata COVID-19 in Italia. 2022. Available online: https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard (accessed on 28 January 2022).
- Amodio, E.; Battisti, M.; Maida, C.M.; Zarcone, M.; Casuccio, A.; Vitale, F. Socio-Demographic Factors Involved in a Low-Incidence Phase of SARS-CoV-2 Spread in Sicily, Italy. Healthcare 2021, 9, 867. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, S.; Kidd, M.P.; McDonald, J.T.; Biddle, N. The Healthy Immigrant Effect: Patterns and Evidence from Four Countries. J. Int. Migr. Integr. 2014, 16, 317–332. [Google Scholar] [CrossRef]
- Fabiani, M.; Mateo-Urdiales, A.; Andrianou, X.; Bella, A.; Del Manso, M.; Bellino, S.; Rota, M.C.; Boros, S.; Vescio, M.F.; D’Ancona, F.P.; et al. Epidemiological characteristics of COVID-19 cases in non-Italian nationals notified to the Italian surveillance system. Eur. J. Public Health 2021, 31, 37–44. [Google Scholar] [CrossRef] [PubMed]
- United Nations High Commissioner for Refugees. Operational Data Portal Refugee Situation. 2022. Available online: https://data2.unhcr.org/en/documents/details/90072 (accessed on 28 January 2022).
- Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA 2020, 323, 1775–1776. [Google Scholar] [CrossRef] [PubMed]
- Sisti, L.G.; Di Napoli, A.; Petrelli, A.; Rossi, A.; Diodati, A.; Menghini, M.; Mirisola, C.; Costanzo, G. COVID-19 Impact in the Italian Reception System for Migrants during the Nationwide Lockdown: A National Observational Study. Int. J. Environ. Res. Public Health 2021, 18, 12380. [Google Scholar] [CrossRef] [PubMed]
- Hintermeier, M.; Gencer, H.; Kajikhina, K.; Rohleder, S.; Hövener, C.; Tallarek, M.; Spallek, J.; Bozorgmehr, K. SARS-CoV-2 among migrants and forcibly displaced populations: A rapid systematic review. J. Migr. Health 2021, 4, 100056. [Google Scholar] [CrossRef] [PubMed]
- Statens Serum Institut. COVID-19 in Denmark. 2020. Available online: https://files.ssi.dk/COVID19-og-herkomst-oktober-2020 (accessed on 28 January 2022).
- Kondilis, E.; Papamichail, D.; McCann, S.; Carruthers, E.; Veizis, A.; Orcutt, M.; Hargreaves, S. The impact of the COVID-19 pandemic on refugees and asylum seekers in Greece: A retrospective analysis of national surveillance data from 2020. eClinicalMedicine 2021, 37, 100958. [Google Scholar] [CrossRef] [PubMed]
- Khunti, K.; Singh, A.K.; Pareek, M.; Hanif, W. Is ethnicity linked to incidence or outcomes of COVID-19? BMJ 2020, 369, m1548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canevelli, M.; Palmieri, L.; Raparelli, V.; Punzo, O.; Donfrancesco, C.; Lo Noce, C.; Vanacore, N.; Brusaferro, S.; Onder, G.; The Italian National Institute of Health COVID-19 Mortality Group. COVID-19 mortality among migrants living in Italy. Ann. Ist. Super Sanita. 2020, 56, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Drefahl, S.; Wallace, M.; Mussino, E.; Aradhya, S.; Kolk, M.; Brandén, M.; Malmberg, B.; Andersson, G. A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat. Commun. 2020, 11, 5097. [Google Scholar] [CrossRef] [PubMed]
- Garcini, L.M.; Pham, T.T.; Ambriz, A.M.; Lill, S.; Tsevat, J. COVID-19 diagnostic testing among underserved Latino communities: Barriers and facilitators. Health Soc. Care Community 2021. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Cui, C.; Zhang, K.; Liu, J.; Xu, J.; Nisenbaum, E.; Huang, Y.; Qin, G.; Chen, B.; Hoffer, M.; et al. COVID19: A Systematic Approach to Early Identification and Healthcare Worker Protection. Front. Public Health 2020, 8, 205. [Google Scholar] [CrossRef] [PubMed]
- International Organization for Migration. Migration Data Portal. 2020. Available online: https://www.migrationdataportal.org/blog/national-preparedness-and-response-plans-covid-19-and-other-diseases-why-migrants-should-be (accessed on 28 January 2022).
- Jakab, Z.; Severoni, S.; Alderslade, R.; Kaojaroen, K.; Hossain, R.; Melki, S. Health and migration: Will migrants share the road to recovery from COVID-19? eClinicalMedicine 2021, 36, 100932. [Google Scholar] [CrossRef] [PubMed]


| Italians N = 155,441 (95.8%) | Undocumented Non-Italians N = 531 (0.3%) | Non-Italians from N = 6288 (3.9%) | |||
|---|---|---|---|---|---|
| nE-HMP 2964 (1.8%) | E-HMP 1159 (0.7%) | HDCs 2165 (1.3%) | |||
| Sex, N (%) | |||||
| - F | 79,754 (51.3%) | 140 (26.4%) | 1105 (37.3%) | 810 (69.9%) | 1261 (58.2%) |
| - M | 75,687 (48.7%) | 391 (73.6%) | 1859 (62.7%) | 349 (30.1%) | 904 (41.8%) |
| Age, Median (IQR) | 46.4 (27.8–45.6) | 25.4 (18.1–29.8) | 36.9 (25.2–39.3) | 38.9 (28.9–39.3) | 47.7 (39.2–45.7) |
| Stratification per Trimester, N (%) 1 | |||||
| - Jan–Mar 2020 | 1717 (1.1%) | 1 (0.2%) | 6 (0.5%) | 13 (0.4%) | 17 (0.8%) |
| - Apr–Jun 2020 | 1223 (0.8%) | 9 (1.7%) | 4 (0.3%) | 25 (0.8%) | 13 (0.6%) |
| - Jul–Sep 2020 | 3502 (2.3%) | 182 (34.3%) | 65 (5.6%) | 339 (11.5%) | 74 (3.4%) |
| - Oct–Dec 2020 | 86,645 (55.9%) | 162 (30.6%) | 480 (41.6%) | 1342 (45.4%) | 1256 (58.1%) |
| - Jan–Mar 2021 | 61,874 (39.9%) | 176 (33.2%) | 600 (51.9%) | 1240 (41.9%) | 800 (37.0%) |
| Worst Clinical Outcome, N (%) 1 | |||||
| - Non-hospitalized | 140,199 (90.4%) | 446 (84.5%) | 2621 (88.8%) | 1090 (94.2%) | 2044 (94.6%) |
| - Hospitalized | 9987 (6.4%) | 71 (13.4%) | 279 (9.5%) | 60 (5.2%) | 98 (4.5%) |
| - Intubation | 113 (0.1%) | 2 (0.4%) | 1 (0%) | 0 (0%) | 2 (0.1%) |
| - Death | 4820 (3.1%) | 9 (1.7%) | 50 (1.7%) | 7 (0.6%) | 16 (0.7%) |
| Non-Severe Clinical Outcome | Severe Clinical Outcome | p-Value | |
|---|---|---|---|
| Sex, N (%) | |||
| - F | 76,258 (92.0%) | 6643 (8.0%) | <0.001 |
| - M | 70,142 (88.8%) | 8872 (11.2%) | |
| Age, Median (IQR) | 43.51 (26.1–58.2) | 70.77 (57.3–81.6) | <0.001 |
| ISTAT classification, N (%) | |||
| - Italians | 140,199 (90.4%) | 14,920 (9.6%) | <0.001 |
| - Undocumented Non-Italians | 446 (84.5%) | 82 (15.5%) | |
| - Non-Italians from non-European countries with High Migratory Pressure | 2621 (88.8%) | 330 (11.2%) | |
| - Non-Italians from European countries with High Migratory Pressure | 1090 (94.2%) | 67 (5.8%) | |
| - Non-Italians from highly developed countries | 2044 (94.6%) | 116 (5.4%) | |
| Stratification per Trimester, N (%) | |||
| - Jan–Mar 2020 | 1018 (58.0%) | 736 (42.0%) | <0.001 |
| - Apr–Jun 2020 | 866 (68.0%) | 408 (32.0%) | |
| - Jul–Sep 2020 | 3487 (83.8%) | 675 (16.2%) | |
| - Oct–Dec 2020 | 81,579 (90.8%) | 8271 (9.2%) | |
| - Jan–Mar 2021 | 59,260 (92.0%) | 5140 (8.0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Immordino, P.; Genovese, D.; Morales, F.; Casuccio, A.; Amodio, E. Epidemiological Characteristics of COVID-19 Cases in Non-Italian Nationals in Sicily: Identifying Vulnerable Groups in the Context of the COVID-19 Pandemic in Sicily, Italy. Int. J. Environ. Res. Public Health 2022, 19, 5767. https://doi.org/10.3390/ijerph19095767
Immordino P, Genovese D, Morales F, Casuccio A, Amodio E. Epidemiological Characteristics of COVID-19 Cases in Non-Italian Nationals in Sicily: Identifying Vulnerable Groups in the Context of the COVID-19 Pandemic in Sicily, Italy. International Journal of Environmental Research and Public Health. 2022; 19(9):5767. https://doi.org/10.3390/ijerph19095767
Chicago/Turabian StyleImmordino, Palmira, Dario Genovese, Fatima Morales, Alessandra Casuccio, and Emanuele Amodio. 2022. "Epidemiological Characteristics of COVID-19 Cases in Non-Italian Nationals in Sicily: Identifying Vulnerable Groups in the Context of the COVID-19 Pandemic in Sicily, Italy" International Journal of Environmental Research and Public Health 19, no. 9: 5767. https://doi.org/10.3390/ijerph19095767
APA StyleImmordino, P., Genovese, D., Morales, F., Casuccio, A., & Amodio, E. (2022). Epidemiological Characteristics of COVID-19 Cases in Non-Italian Nationals in Sicily: Identifying Vulnerable Groups in the Context of the COVID-19 Pandemic in Sicily, Italy. International Journal of Environmental Research and Public Health, 19(9), 5767. https://doi.org/10.3390/ijerph19095767