Analysis of Diabetic Foot Deformation and Plantar Pressure Distribution of Women at Different Walking Speeds
Abstract
:Highlights
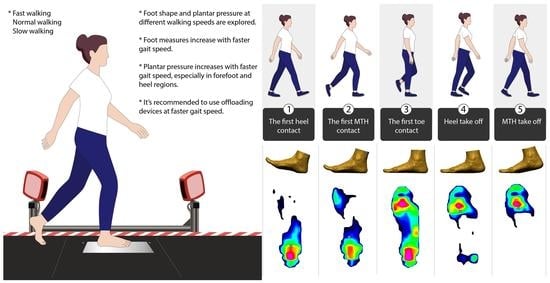
- Foot measurements show an insignificant increase at a more rapid walking speed.
- Faster walking speed results in higher mean peak plantar pressure in the forefoot and heel areas, along with a lower pressure time integral in all foot regions.
- Suitable offloading devices are recommended for people with diabetes during exercise at higher walking speeds.
- An insole with a different structure and material for each specific area contributes to plantar pressure offloading.
Abstract
1. Introduction
- (1)
- to analyze the effect of walking speed on plantar pressure distribution in dynamic situations;
- (2)
- to investigate the effect of walking speed on the deformation of the foot geometry.
2. Materials and Methods
2.1. Participants
2.2. Experiment Protocols
- (1)
- First, the subjects walked on the walkway 10 times at their natural pace to determine their normal speed and calculate the slow and fast walking speeds. Scanning and plantar pressure measurement trials that exceeded 5% of the predetermined speeds were rejected to minimize the effect of speed on foot deformation and plantar pressure distribution.
- (2)
- Then, both the left and right feet were scanned 3 times at the three walking speeds defined in the first step.
- (3)
- The plantar pressure of the subjects in their bare feet at the 3 defined walking speeds was recorded 3 times, and the subjects wore standard cotton socks to secure Pedar sensors onto the plantar of their feet.
2.3. Foot Image Analysis
2.4. Plantar Pressure Analysis
2.5. Data Analysis
3. Results and Discussion
3.1. Participant Information
3.2. Effect of Walking Speed on Foot Deformation
3.3. Effect of Walking Speed on Plantar Pressure Distribution
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- IDF. Diabetes Facts & Figures. 2022. Available online: https://idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html (accessed on 11 March 2022).
- Atosona, A.; Larbie, C. Prevalence and determinants of diabetic foot ulcers and lower extremity amputations in three selected tertiary hospitals in Ghana. J. Diabetes Res. 2019, 2019, 7132861. [Google Scholar] [CrossRef] [PubMed]
- Lavery, L.A.; Boulton, A.J.; Niezgoda, J.A.; Sheehan, P. A comparison of diabetic foot ulcer outcomes using negative pressure wound therapy versus historical standard of care. Int. Wound J. 2007, 4, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Mariam, T.G.; Alemayehu, A.; Tesfaye, E.; Mequannt, W.; Temesgen, K.; Yetwale, F.; Limenih, M.A. Prevalence of diabetic foot ulcer and associated factors among adult diabetic patients who attend the diabetic follow-up clinic at the University of Gondar Referral Hospital, North West Ethiopia, 2016: Institutional-based cross-sectional study. J. Diabetes Res. 2017, 2017, 2879249. [Google Scholar] [CrossRef] [Green Version]
- Raghav, A.; Khan, Z.A.; Labala, R.K.; Ahmad, J.; Noor, S.; Mishra, B.K. Financial burden of diabetic foot ulcers to world: A progressive topic to discuss always. Adv. Endocrinol. Metab. 2018, 9, 29–31. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Boulton, A.J.M.; Bus, S.A. Diabetic Foot Ulcers and Their Recurrence. N. Engl. J. Med. 2017, 376, 2367–2375. [Google Scholar] [CrossRef]
- Nazar, C.M.; Bojerenu, M.M.; Safdar, M.; Marwat, J. Effectiveness of diabetes education and awareness of diabetes mellitus in combating diabetes in the United Kigdom; a literature review. J. Nephropharmacol. 2016, 5, 110–115. [Google Scholar]
- Holt, P. Blood glucose monitoring in diabetes. Nurs. Stand. 2014, 28, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Collings, R.; Freeman, J.; Latour, J.M.; Paton, J. Footwear and insole design features for offloading the diabetic at risk foot-A systematic review and meta-analyses. Endocrinol. Diabetes Metab. 2020, 4, e00132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogrin, R.; Sands, A. Foot assessment in patients with diabetes. Aust. Fam. Physician 2006, 35, 419–421. [Google Scholar] [PubMed]
- Cannata, F.; Vadalà, G.; Russo, F.; Papalia, R.; Napoli, N.; Pozzilli, P. Beneficial Effects of Physical Activity in Diabetic Patients. J. Funct. Morphol. Kinesiol. 2020, 5, 70. [Google Scholar] [CrossRef] [PubMed]
- Church, T.S.; Cheng, Y.J.; Earnest, C.P.; Barlow, C.E.; Gibbons, L.W.; Priest, E.L.; Blair, S.N. Exercise capacity and body composition as predictors of mortality among men with diabetes. Diabetes Care 2004, 27, 83–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seidu, S.; Khunti, K.; Yates, T.; Almaqhawi, A.; Davies, M.J.; Sargeant, J. The importance of physical activity in management of type 2 diabetes and COVID-19. Ther. Adv. Endocrinol. Metab. 2021, 12, 20420188211054686. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Kudo, A.; Asahi, K.; Machii, N.; Iseki, K.; Satoh, H.; Moriyama, T.; Yamagata, K.; Tsuruya, K.; Fujimoto, S.; et al. Fast walking is a preventive factor against new-onset diabetes mellitus in a large cohort from a Japanese general population. Sci. Rep. 2021, 11, 716. [Google Scholar] [CrossRef] [PubMed]
- Lakhdar, D.; Mustapha, D.; Khaled, M.B. Effectiveness of Brisk Walking Exercise on Glycaemic Control and Cardio-Vascular Risk Factors in Patients with Type 2 Diabetes. J. Drug Deliv. Ther. 2020, 10, 53–62. [Google Scholar] [CrossRef]
- Negri, C.; Bacchi, E.; Morgante, S.; Soave, D.; Marques, A.; Menghini, E.; Muggeo, M.; Bonora, E.; Moghetti, P. Supervised Walking Groups to Increase Physical Activity in Type 2 Diabetic Patients. Diabetes Care 2010, 33, 2333–2335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qiu, S.; Cai, X.; Schumann, U.; Velders, M.; Sun, Z.; Steinacker, J.M. Impact of walking on glycemic control and other cardiovascular risk factors in type 2 diabetes: A meta-analysis. PLoS ONE 2014, 9, e109767. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lung, C.-W.; Mo, P.-C.; Cao, C.; Zhang, K.; Wu, F.-L.; Liau, B.-Y.; Jan, Y.-K. Effects of walking speeds and durations on the plantar pressure gradient and pressure gradient angle. BMC Musculoskelet. Disord. 2022, 23, 823. [Google Scholar] [CrossRef]
- Segal, A.; Rohr, E.; Orendurff, M.; Shofer, J.; O’Brien, M.; Sangeorzan, B. The Effect of Walking Speed on Peak Plantar Pressure. Foot Ankle Int. 2005, 25, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Bisiaux, M.; Moretto, P. The effects of fatigue on plantar pressure distribution in walking. Gait Posture 2008, 28, 693–698. [Google Scholar] [CrossRef]
- Weist, R.; Eils, E.; Rosenbaum, D. The influence of muscle fatigue on electromyogram and plantar pressure patterns as an explanation for the incidence of metatarsal stress fractures. Am. J. Sport. Med. 2004, 32, 1893–1898. [Google Scholar] [CrossRef]
- Cheung, J.T.; Zhang, M. Parametric design of pressure-relieving foot orthosis using statistics-based finite element method. Med. Eng. Phys. 2008, 30, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Schmeltzpfenning, T.; Brauner, T. 2—Foot biomechanics and gait. In Handbook of Footwear Design and Manufacture; Luximon, A., Ed.; Woodhead Publishing: Sawston, UK, 2013; pp. 27–48. [Google Scholar] [CrossRef]
- Xiong, S.; Goonetilleke, R.; Zhao, J.; Li, W.; Witana, C. Foot deformations under different load-bearing conditions and their relationships to stature and body weight. Anthropol. Sci. 2009, 117, 77–88. [Google Scholar] [CrossRef] [Green Version]
- Barisch-Fritz, B.; Schmeltzpfenning, T.; Plank, C.; Grau, S. Foot deformation during walking: Differences between static and dynamic 3D foot morphology in developing feet. Ergonomics 2014, 57, 921–933. [Google Scholar] [CrossRef] [PubMed]
- Grau, S.; Barisch-Fritz, B. Improvement of safety shoe fit—Evaluation of dynamic foot structure. Footwear Sci. 2018, 10, 179–187. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Yick, K.-L.; Li, P.-L.; Yip, J.; Ng, S.-P. Foot deformation analysis with different load-bearing conditions to enhance diabetic footwear designs. PLoS ONE 2022, 17, e0264233. [Google Scholar] [CrossRef] [PubMed]
- Ohuchi, H.; Chavez, J.; Alvarez, C. Changes in calcaneal pitch and heel fat pad thickness in static weight bearing radiographs while wearing shoes with arch support and heel cup orthotics. Asia-Pac. J. Sport. Med. Arthrosc. Rehabil. Technol. 2019, 17, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Cui, C.; Wan, X.; Zheng, Z.; Yan, S.; Liu, H.; Qu, F.; Zhang, K. Design feature combinations effects of running shoe on plantar pressure during heel landing: A finite element analysis with Taguchi optimization approach. Front. Bioeng. Biotechnol. 2022, 10, 959842. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ma, Y.; Hou, B.Y.; Lam, W.-K. Influence of Gait Speeds on Contact Forces of Lower Limbs. J. Healthc. Eng. 2017, 2017, 6375976. [Google Scholar] [CrossRef] [Green Version]
- Sun, D.; Fekete, G.; Mei, Q.; Gu, Y. The effect of walking speed on the foot inter-segment kinematics, ground reaction forces and lower limb joint moments. PeerJ 2018, 6, e5517. [Google Scholar] [CrossRef] [Green Version]
- Koo, S.; Park, M.S.; Chung, C.Y.; Yoon, J.S.; Park, C.; Lee, K.M. Effects of walking speed and slope on pedobarographic findings in young healthy adults. PLoS ONE 2019, 14, e0220073. [Google Scholar] [CrossRef]
- Ma, X.; Luximon, A. 9—Design and manufacture of shoe lasts. In Handbook of Footwear Design and Manufacture; Luximon, A., Ed.; Woodhead Publishing: Sawston, UK, 2013; pp. 177–196. [Google Scholar] [CrossRef]
- D’AoÛt, K.; Pataky, T.C.; De Clercq, D.; Aerts, P. The effects of habitual footwear use: Foot shape and function in native barefoot walkers. Footwear Sci. 2009, 1, 81–94. [Google Scholar] [CrossRef]
- Chiles, N.S.; Phillips, C.L.; Volpato, S.; Bandinelli, S.; Ferrucci, L.; Guralnik, J.M.; Patel, K.V. Diabetes, peripheral neuropathy, and lower-extremity function. J. Diabetes Its Complicat. 2014, 28, 91–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sacco, I.C.; Hamamoto, A.N.; Tonicelli, L.M.; Watari, R.; Ortega, N.R.; Sartor, C.D. Abnormalities of plantar pressure distribution in early, intermediate, and late stages of diabetic neuropathy. Gait Posture 2014, 40, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Bus, S.A.; van Deursen, R.W.; Kanade, R.V.; Wissink, M.; Manning, E.A.; van Baal, J.G.; Harding, K.G. Plantar pressure relief in the diabetic foot using forefoot offloading shoes. Gait Posture 2009, 29, 618–622. [Google Scholar] [CrossRef] [PubMed]
- Woo, Y.; Ko, S.; Ahn, S.; Nguyen, H.T.P.; Shin, C.; Jeong, H.; Noh, B.; Lee, M.; Park, H.; Youm, C. Classification of Diabetic Walking for Senior Citizens and Personal Home Training System Using Single RGB Camera through Machine Learning. Appl. Sci. 2021, 11, 9029. [Google Scholar] [CrossRef]
- Nilsson, J.; Thorstensson, A. Ground reaction forces at different speeds of human walking and running. Acta Physiol. Scand. 1989, 136, 217–227. [Google Scholar] [CrossRef]
- Caravaggi, P.; Pataky, T.; Günther, M.; Savage, R.; Crompton, R. Dynamics of longitudinal arch support in relation to walking speed: Contribution of the plantar aponeurosis. J. Anat. 2010, 217, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-W.; Hung, W.; Wu, H.-W.; Chiu, Y.-C.; Hsu, H.-C. Measurements of Foot Arch in Standing, Level Walking, Vertical Jump and Sprint Start. Int. J. Sport Exerc. Sci. 2010, 2, 31–38. [Google Scholar]
- Peng, Y.; Wang, Y.; Wong, D.W.-C.; Chen, T.L.-W.; Chen, S.F.; Zhang, G.; Tan, Q.; Zhang, M. Different Design Feature Combinations of Flatfoot Orthosis on Plantar Fascia Strain and Plantar Pressure: A Muscle-Driven Finite Element Analysis With Taguchi Method. Front. Bioeng. Biotechnol. 2022, 10, 853085. [Google Scholar] [CrossRef] [PubMed]
- Zelik, K.E.; Adamczyk, P.G. A unified perspective on ankle push-off in human walking. J. Exp. Biol. 2016, 219, 3676–3683. [Google Scholar] [CrossRef] [Green Version]
- Hulshof, C.M.; van Netten, J.J.; Dekker, M.G.; Pijnappels, M.; Bus, S.A. In-shoe plantar pressure depends on walking speed and type of weight-bearing activity in people with diabetes at high risk of ulceration. bioRxiv 2022, 479511. [Google Scholar] [CrossRef]
- Hebenstreit, F.; Leibold, A.; Krinner, S.; Welsch, G.; Lochmann, M.; Eskofier, B.M. Effect of walking speed on gait sub phase durations. Hum. Mov. Sci. 2015, 43, 118–124. [Google Scholar] [CrossRef]
- Haris, F.; Liau, B.-Y.; Jan, Y.-K.; Akbari, V.; Primanda, Y.; Lin, K.-H.; Lung, C.-W. A Review of the Plantar Pressure Distribution Effects from Insole Materials and at Different Walking Speeds. Appl. Sci. 2021, 11, 11851. [Google Scholar] [CrossRef]
- Leung, M.S.-H.; Yick, K.-L.; Sun, Y.; Chow, L.; Ng, S.-P. 3D printed auxetic heel pads for patients with diabetic mellitus. Comput. Biol. Med. 2022, 146, 105582. [Google Scholar] [CrossRef]
- Chen, T.; Tian, M.; Wang, X. A Novel Porous Structural Design of the Orthotic Insole for Diabetic Foot. In Proceedings of the 2021 International Conference on Computer, Control and Robotics (ICCCR), Shanghai, China, 8–10 January 2021; pp. 188–192. [Google Scholar]
- Lemaster, J.W.; Reiber, G.E.; Smith, D.G.; Heagerty, P.J.; Wallace, C. Daily weight-bearing activity does not increase the risk of diabetic foot ulcers. Med. Sci. Sport. Exerc. 2003, 35, 1093–1099. [Google Scholar] [CrossRef]
- Lemaster, J.W.; Mueller, M.J.; Reiber, G.E.; Mehr, D.R.; Madsen, R.W.; Conn, V.S. Effect of weight-bearing activity on foot ulcer incidence in people with diabetic peripheral neuropathy: Feet first randomized controlled trial. Phys. Ther. 2008, 88, 1385–1398. [Google Scholar] [CrossRef] [Green Version]
- Honert, E.C.; Bastas, G.; Zelik, K.E. Effect of toe joint stiffness and toe shape on walking biomechanics. Bioinspir. Biomim. 2018, 13, 066007. [Google Scholar] [CrossRef]
- Day, E.M.; Hahn, M.E. Dynamic angular stiffness about the metatarsophalangeal joint increases with running speed. Hum. Mov. Sci. 2019, 67, 102501. [Google Scholar] [CrossRef] [PubMed]
- Pamela, D.; Ritzline, A.Z.-L. Foot and ankle exercises in patients with diabetes. Lower Extremity Review Magazine. January 2011. Available online: https://lermagazine.com/article/foot-and-ankle-exercises-in-patients-with-diabetes (accessed on 29 December 2022).
- Wu, G.; Millon, D.J.C.B. Joint kinetics during Tai Chi gait and normal walking gait in young and elderly Tai Chi Chuan practitioners. Clin. Biomech. 2008, 23, 787–795. [Google Scholar] [CrossRef]






| Variable | Mean | Standard Deviation | Maximum | Minimum |
|---|---|---|---|---|
| Female (n = 19) | ||||
| Age (years old) | 66 | 5 | 75 | 57 |
| BMI (kg/m2) | 22.3 | 3.2 | 30.8 | 18.2 |
| Foot size (EUR) | 38 | 1 | 41 | 37 |
| Years since diagnosis (DM) | 13 | 1 | 31 | 10 |
| Foot Measurement (mm) | Mean (Standard Deviation) | Fast vs. Slow (%) | Normal vs. Slow (%) | Fast vs. Normal (%) | ||
|---|---|---|---|---|---|---|
| Slow | Normal | Fast | ||||
| Foot length (FL) | 237.0 (9.3) | 237.2 (8.5) | 237.5 (9.0) | 0.2% | 0.1% | 0.2% |
| Medial ball length (MBL) | 177.1 (4.3) | 177.1 (4.8) | 178.5 (5.5) | 0.8% | 0.0% | 0.8% |
| Lateral ball length (LBL) | 152.4 (4.8) | 152.4 (3.7) | 153.8 (4.2) | 0.9% | 0.0% | 0.9% |
| Anatomical ball width (ABW) | 98.8 (4.9) | 98.9 (5.3) | 99.4 (4.8) | 0.6% | 0.1% | 0.5% |
| Orthogonal ball width (OBW) | 92.8 (4.3) | 92.8 (4.8) | 93.5 (4.5) | 0.7% | 0.0% | 0.7% |
| Orthogonal heel width (OHW) | 52.0 (4.4) | 52.1 (4.2) | 53.0 (5.8) | 1.8% | 0.2% | 1.6% |
| Instep height (IH) | 61.8 (3.3) | 61.9 (3.7) | 61.9 (2.8) | 0.2% | 0.1% | 0.1% |
| Ball height (BH) | 47.8 (3.7) | 47.9 (3.8) | 47.9 (2.3) | 0.3% | 0.3% | 0.0% |
| Ball angle (BA) | 78.4 (9.1) | 79.0 (9.7) | 79.1 (9.6) | 0.8% | 0.7% | 0.1% |
| Toe1 angle (T1A) | 17.2 (5.4) | 17.3 (5.9) | 17.7 (5.3) | 3.3% | 0.6% | 2.7% |
| Toe5 angle (T5A) | 13.6 (3.1) | 13.7 (3.5) | 14.7 (2.3) | 8.2% | 0.9% | 7.2% |
| Anatomical ball girth (ABG) | 225.6 (11.5) | 226.0 (13.1) | 226.2 (13.3) | 0.3% | 0.2% | 0.1% |
| Instep girth (IG) | 238.3 (11.9) | 238.4 (13.0) | 239.1 (14.7) | 0.3% | 0.1% | 0.3% |
| Area of Pressure Measurement | Mean (Standard Deviation) | Fast vs. Slow (%) | Normal vs. Slow (%) | Fast vs. Normal (%) | ||
|---|---|---|---|---|---|---|
| Slow | Normal | Fast | ||||
| Mean peak pressure (kPa) | ||||||
| Toes | 191.8 (80.9) | 216.6 (85.6) | 230.2 (77.9) | 20.0% | 13.0% | 6.3% |
| Metatarsal heads | 295.4 (70.4) | 316.4 (83.6) | 338.1 (82.1) | 14.5% | 7.1% | 6.9% |
| Medial midfoot | 32.5 (21.4) | 30.9 (20.6) | 28.7 (17.3) | −11.7% | −4.7% | −7.3% |
| Lateral midfoot | 94.9 (55.1) | 86.0 (50.7) | 85.5 (40.4) | −9.9% | −9.4% | −0.6% |
| Heel | 243.5 (63.9) | 249.2 (62.7) | 276.4 (88.0) | 13.5% | 2.4% | 10.9% |
| Whole | 316.1 (75.3) | 334.4 (84.7) | 365.9 (89.4) | 15.8% | 5.8% | 9.4% |
| Pressure time integral (kPa*s) | ||||||
| Toes | 72.7 (38.4) | 67.4 (27.3) | 60.2 (18.6) | −17.2% | −7.2% | −10.8% |
| Metatarsal heads | 118.3 (32.6) | 111.9 (28.7) | 101.5 (21.6) | −14.2% | −5.4% | −9.3% |
| Medial midfoot | 14.4 (6.1) | 12.5 (5.1) | 8.3 (4.2) | −42.6% | −12.9% | −34.1% |
| Lateral midfoot | 43.6 (28.1) | 36.5 (23.3) | 30.6 (14.5) | −29.9% | −16.4% | −16.1% |
| Heel | 86.7 (20.8) | 83.7 (26.4) | 71.2 (19.3) | −17.8% | −3.5% | −14.9% |
| Whole | 168.3 (42.8) | 161.1 (34.0) | 143.6 (24.4) | −14.7% | −4.3% | −10.8% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, L.-Y.; Liu, Q.-L.; Yick, K.-L.; Yip, J.; Ng, S.-P. Analysis of Diabetic Foot Deformation and Plantar Pressure Distribution of Women at Different Walking Speeds. Int. J. Environ. Res. Public Health 2023, 20, 3688. https://doi.org/10.3390/ijerph20043688
Zhang L-Y, Liu Q-L, Yick K-L, Yip J, Ng S-P. Analysis of Diabetic Foot Deformation and Plantar Pressure Distribution of Women at Different Walking Speeds. International Journal of Environmental Research and Public Health. 2023; 20(4):3688. https://doi.org/10.3390/ijerph20043688
Chicago/Turabian StyleZhang, Li-Ying, Qi-Long Liu, Kit-Lun Yick, Joanne Yip, and Sun-Pui Ng. 2023. "Analysis of Diabetic Foot Deformation and Plantar Pressure Distribution of Women at Different Walking Speeds" International Journal of Environmental Research and Public Health 20, no. 4: 3688. https://doi.org/10.3390/ijerph20043688
APA StyleZhang, L. -Y., Liu, Q. -L., Yick, K. -L., Yip, J., & Ng, S. -P. (2023). Analysis of Diabetic Foot Deformation and Plantar Pressure Distribution of Women at Different Walking Speeds. International Journal of Environmental Research and Public Health, 20(4), 3688. https://doi.org/10.3390/ijerph20043688