In Situ-Based Gels for Nose to Brain Delivery for the Treatment of Neurological Diseases
Abstract
:1. Introduction
2. Anatomy of the Nose
2.1. Mechanism of Nose-to-Brain Drug Delivery
2.2. Anatomical Structures Involved in Nose-to-Brain Transport
3. Neurological Diseases and Challenges in Treatment
4. Nasal Delivery for the Treatment of Neurological Diseases Such as Alzheimer’s Diseases, Parkinson’s Diseases, Epilepsy, etc.
4.1. Hydrogels
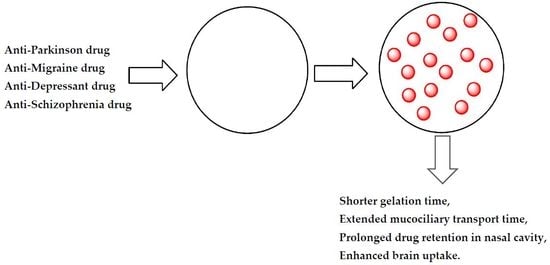
4.1.1. In Situ Gels
In Situ-Based Gels for the Delivery of Anti-Parkinson Drugs
In Situ Gels for the Delivery of Anti-Migraine Drug
In Situ Hydrogels for the Delivery of Anti-Alzheimer’s Drug
In Situ Gels for the Delivery of Anti-Depressant Drug
In Situ Gels for the Delivery of Anti-Schizophrenia Drug
5. Challenges and Future Perspective
Acknowledgments
Author Contribution
Conflicts of Interest
References
- What Are Neurological Disorders? Available online:. Available online: http://www.who.int/features/qa/55/en (accessed on 29 December 2017).
- Neurological Problem Symptoms, Causes and Effects. Available online: https://www.psychguides.com/guides/neurological-problem-symptoms-causes-and-effects (accessed on 29 December 2017).
- Choi, S.; Krishnan, J.; Ruckmani, K. Cigarette smoke and related risk factors in neurological disorders: An update. Biomed. Pharmacother. 2017, 85, 79–86. [Google Scholar]
- Kumar, R.; Bhave, A.; Bhargava, R.; Agarwal, G.G. Prevalence and risk factors for neurological disorders in children aged 6 months to 2 years in northern India. Dev. Med. Child Neurol. 2013, 55, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Yu, S.; Wu, Z.; Tang, B. Genetics of hereditary neurological disorders in children. Transl. Pediatr. 2014, 3, 108–119. [Google Scholar] [PubMed]
- Silberberg, D.; Anand, N.P.; Michels, K.; Kalaria, R.N. Brain and other nervous system disorders across the lifespan—Global challenges and opportunities. Nature 2015, 527, S151–S154. [Google Scholar] [CrossRef] [PubMed]
- Kanwar, J.R.; Sriramoju, B.; Kanwar, R.K. Neurological disorders and therapeutics targeted to surmount the blood-brain barrier. Int. J. Nanomed. 2012, 7, 3259–3278. [Google Scholar] [CrossRef] [PubMed]
- Neurological Testing and Treatment. Available online: http://www.mountsinai.org/patient-care/service-areas/neurology/treatment (accessed on 29 December 2017).
- Upadhyay, R.K. Drug delivery systems, CNS protection, and the blood brain barrier. BioMed. Res. Int. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, M.S. Treatment of neurological and psychiatric disorders with deep brain stimulation; Raising hopes and future challenges. Basic. Clin. Neurosci. 2013, 4, 266–270. [Google Scholar] [PubMed]
- Xu, X.; Warrington, A.E.; Bieber, A.J.; Rodriguez, M. Enhancing CNS repair in neurological disease. CNS Drugs. 2011, 25, 555–573. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, B. Nose to brain drug delivery: A recent update. J. Formul. Sci. Bioavailab. 2017, 1. [Google Scholar]
- Archer, S.M. Nasal Physiology. 26 February 2016. Available online: https://emedicine.medscape.com/article/874771-overview (accessed on 2 January 2018).
- Nose Sinuses and Smell. Available online: http://www.innerbody.com/anim/nasal.html (accessed on 2 January 2018).
- Ghori, M.U.; Mahdi, M.H.; Smith, A.M.; Conway, B.R. Nasal drug delivery systems: An overview. Am. J. Pharmacol. Sci. 2015, 3, 110–119. [Google Scholar]
- Alagusundaram, M. Nasal drug delivery system-an overview. Int. J. Res. Pharm. Sci. 2010, 1, 454–465. [Google Scholar]
- Ozsoy, Y.; Gungor, S.; Cevher, E. Nasal delivery of high molecular weight drugs. Molecules 2009, 14, 3754–3779. [Google Scholar] [CrossRef] [PubMed]
- Mittal, D.; Ali, A.; Md, S.; Baboota, S.; Sahni, J.K.; Ali, J. Insights into direct nose to brain delivery: Current status and future perspective. Drug Deliv. 2014, 21, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Dhuria, S.V.; Hanson, L.R.; Frey, W.H. Intranasal delivery to the central nervous system: Mechanisms and experimental considerations. J. Pharm. Sci. 2010, 99, 1654–1673. [Google Scholar] [CrossRef] [PubMed]
- Rassu, G.; Soddu, E.; Cossu, M.; Gavini, E.; Giunchedi, P.; Dalpiaz, A. Particulate formulations based on chitosan for nose-to-brain delivery of drugs. A review. J. Drug Deliv. Sci. Technol. 2016, 32, 77–87. [Google Scholar] [CrossRef]
- Anatomy and Physiology of the Nose: Key Points Relating to Nasal Drug Delivery. Available online: http://intranasal.net/AnatomyPhysiology/default.htm. (accessed on 14 February 2018).
- Van Woensel, M.; Wauthoz, N.; Rosière, R.; Amighi, K.; Mathieu, V.; Lefranc, F.; Van Gool, S.W.; De Vleeschouwer, S. Formulations for intranasal delivery of pharmacological agents to combat brain disease: A new opportunity to tackle GBM? Cancers 2013, 5, 1020–1048. [Google Scholar] [CrossRef] [PubMed]
- Van Itallie, C.M.; Anderson, J.M. Claudins and epithelial paracellular transport. Annu. Rev. Physiol. 2006, 68, 403–429. [Google Scholar] [CrossRef] [PubMed]
- Doty, R.L. The olfactory vector hypothesis of neurodegenerative disease: Is it viable? Ann. Neurol. 2008, 63, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Hadaczek, P.; Yamashita, Y.; Mirek, H.; Tamas, L.; Bohn, M.C.; Noble, C.; Park, J.W.; Bankiewicz, K. The “perivascular pump” driven by arterial pulsation is a powerful mechanism for the distribution of therapeutic molecules within the brain. Mol. Ther. 2006, 14, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Enna, S.J.; Williams, M. Challenges in the search for drugs to treat central nervous system disorders. J. Pharmacol. Exp. Ther. 2009, 329, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Forum on Neuroscience and Nervous System Disorders; Board on Health Sciences Policy; Institute of Medicine. Drug Development Challenges. In Improving and Accelerating Therapeutic Development for Nervous System Disorders: Workshop Summary; National Academies Press: Washington, DC, USA, 2014. [Google Scholar]
- Pankevich, D.E.; Altevogt, B.M.; Dunlop, J.; Gage, F.H.; Hyman, S.E. Improving and accelerating drug development for nervous system disorders. Neuron. 2014, 84, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Kvq, L.; Nguyen, L.T. Environmental factors in Alzheimer’s and Parkinson’s diseases. J. Alzheimers Dis. Parkinsonism 2013, 3. [Google Scholar]
- Fleminger, S.; Oliver, D.L.; Lovestone, S.; Rabe-Hesketh, S.; Giora, A. Head injury as a risk factor for Alzheimer’s disease: The evidence 10 years on; a partial replication. J. Neurol. Neurosurg. Psychiatr. 2003, 74, 857–862. [Google Scholar] [CrossRef]
- Evatt, M.L.; Delong, M.R.; Khazai, N.; Rosen, A.; Triche, S.; Tangpicha, V. Prevalence of vitamin D insufficiency in patients with Parkinson disease and Alzheimer’s disease. Arch. Neurol. 2008, 65, 1348–1352. [Google Scholar] [CrossRef] [PubMed]
- Sudduth, T.L.; Powell, D.K.; Smith, C.D.; Greenstein, A.; Wilcock, D.M. Induction of hyperhomocysteinemia models vascular dementia by induction of cerebral microhemorrhages and neuroinflammation. J. Cereb. Blood Flow Metab. 2013, 33, 708–715. [Google Scholar] [CrossRef] [PubMed]
- FDA-Approved Treatments for Alzheimer’s. Available online: https://www.alz.org/dementia/downloads/topicsheet_treatments.pdf (accessed on 14 February 2018).
- Fan, X.; Sun, D.; Tang, X.; Cai, Y.; Yin, Z.Q.; Xu, H. Stem-cell challenges in the treatment of Alzheimer’s disease: A long way from bench to bedside. Med. Res. Rev. 2014, 34, 957–978. [Google Scholar] [PubMed]
- Piehl, F. A changing treatment landscape for multiple sclerosis: Challenges and opportunities. J. Intern. Med. 2014, 275, 364–381. [Google Scholar] [CrossRef] [PubMed]
- Racke, M.K. Challenges in developing new multiple sclerosis therapies. Ther. Adv. Neurol. Disord. 2008, 1, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Compston, A.; Coles, A. Multiple sclerosis. Lancet. 2008, 372, 1502–1517. [Google Scholar] [PubMed]
- Patel, K.R.; Cherian, J.; Gohil, K.; Atkinson, D. Schizophrenia: Overview and treatment options. Pharm. Ther. 2014, 39, 638–645. [Google Scholar]
- FDA-approved drugs to treat schizophrenia. J. Psychosoc. Nurs. Ment. Health Serv. 2014, 52, 11–12. [CrossRef]
- Epilepsy. Available online: http://www.who.int/mediacentre/factsheets/fs999/en (accessed on 2 January 2018).
- Wahab, A. Difficulties in treatment and management of epilepsy and challenges in new drug development. Pharmaceuticals 2010, 3, 2090–2110. [Google Scholar] [CrossRef] [PubMed]
- Remy, S.; Beck, H. Molecular and cellular mechanisms of pharmacoresistance in epilepsy. Brain 2006, 129, 18–35. [Google Scholar] [CrossRef] [PubMed]
- Oertel, WH. Recent advances in treating Parkinson’s disease. F1000Res. 2017, 6. [Google Scholar] [CrossRef] [PubMed]
- Seinbart, E.; Patterson, M. Parkinson’s disease: Challenges, progress and hope. Available online: https://nursece.com/courses/120-parkinson-s-disease-challenges-progress-and-hope (accessed on 15 February 2018).
- Smith, Y.; Wichmann, T.; Factor, S.A.; DeLong, M.R. Parkinson’s disease therapeutics: New developments and challenges since the introduction of levodopa. Neuropsychopharmacology 2012, 37, 213–246. [Google Scholar] [CrossRef] [PubMed]
- Understanding brain tumors. Available online: http://braintumor.org/brain-tumor-information/understanding-brain-tumors/ (accessed on 2 January 2018).
- Rajesh, Y.; Pal, I.; Banik, P.; Chakraborty, S.; Borkar, S.A.; Dey, G.; Mukherjee, A.; Mandal, M. Insights into molecular therapy of glioma: Current challenges and next generation blueprint. Acta Pharmacol. Sin. 2017, 38, 591–613. [Google Scholar] [CrossRef] [PubMed]
- Sosnik, A.; Seremeta, K.P. Polymeric hydrogels as technology platform for drug delivery applications. Gels 2017, 3. [Google Scholar] [CrossRef]
- Hoare, T.R.; Kohane, D.S. Hydrogels in drug delivery: Progress and challenges. Polymer 2008, 49, 1993–2007. [Google Scholar] [CrossRef]
- Chassenieux, C.; Tsitsilianis, C. Recent trends in pH/thermo-responsive self-assembling hydrogels: From polyions to peptide-based polymeric gelators. Soft Matter 2016, 12, 1344–1359. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; HariKumar, S.L. Injectable in-situ gelling controlled release drug delivery system. Int. J. Drug Dev. Res. 2012, 4, 56–69. [Google Scholar]
- Djaldetti, R.; Baron, J.; Ziv, I.; Melamed, E. Gastric emptying in Parkinson’s disease patients with and without response fluctuations. Neurology 1996, 46, 1051–1054. [Google Scholar] [CrossRef] [PubMed]
- LeWitt, P.A. Levodopa for the treatment of Parkinson’s disease. N. Engl. J. Med. 2008, 359, 2468–2476. [Google Scholar] [CrossRef] [PubMed]
- Kurlan, R.; Rothfield, K.; Woodward, W.; Nutt, J.; Miller, C.; Lichter, D.; Shoulson, I. Erratic gastric emptying of levodopa may cause random fluctuations of Parkinsonian mobility. Neurology 1988, 38, 585–595. [Google Scholar] [CrossRef]
- Haddad, F.; Sawalha, M.; Khawaja, Y.; Najjar, A.; Karaman, R. Dopamine and levodopa prodrugs for the treatment of Parkinson’s disease. Molecules 2017, 23. [Google Scholar]
- Sharma, S.; Lohan, S.; Murthy, R.S. Formulation and characterization of intranasal mucoadhesive nanoparticulates and thermo-reversible gel of levodopa for brain delivery. Drug Dev. Ind. Pharm. 2014, 40, 869–878. [Google Scholar] [CrossRef] [PubMed]
- Lungare, S.; Bowen, J.; Badhan, R.K. Overcoming Parkinson’s disease: Direct nose-to-brain delivery of amantadine. In Proceedings of the UK & Ireland Controlled Release Society Annual Symposium, Reading, UK, 16 April 2013. [Google Scholar]
- Lungare, S.; Bowen, J.; Badhan, R. Development and evaluation of a novel intranasal spray for the delivery of amantadine. J. Pharm. Sci. 2016, 105, 1209–1220. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Patil, K.; Bobade, N.; Yeole, P.; Gaikwad, R. Formulation of intranasal mucoadhesive temperature-mediated in situ gel containing ropinirole and evaluation of brain targeting efficiency in rats. J. Drug Target 2010, 18, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Ravi, P.R.; Aditya, N.; Patil, S.; Cherian, L. Nasal in-situ gels for delivery of rasagiline mesylate: Improvement in bioavailability and brain localization. Drug Deliv. 2015, 22, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Rao, M.; Agrawal, D.K.; Shirsath, C. Thermoreversible mucoadhesive in situ nasal gel for treatment of Parkinson’s disease. Drug Dev. Ind. Pharm. 2017, 43, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Galgatte, U.C.; Kumbhar, A.B.; Chaudhari, P.D. Development of in situ gel for nasal delivery: Design, optimization, in vitro and in vivo evaluation. Drug Deliv. 2014, 21, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Tao, T.; Zhao, Y.; Yue, P.; Dong, W.X.; Chen, Q.H. Preparation of huperzine A nasal in situ gel and evaluation of its brain targeting following intranasal administration. Yao Xue Xue Bao 2006, 41, 1104–1110. [Google Scholar] [PubMed]
- Chen, X.; Zhi, F.; Jia, X.; Zhang, X.; Ambardekar, R.; Meng, Z.; Paradkar, A.R.; Hu, Y.; Yang, Y. Enhanced brain targeting of curcumin by intranasal administration of a thermosensitive poloxamer hydrogel. J. Pharm. Pharmacol. 2013, 65, 807–816. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Jiang, S.; Wang, H.; Bie, H. A mucoadhesive, thermoreversible in situ nasal gel of geniposide for neurodegenerative diseases. PLoS ONE 2017, 12, e0189478. [Google Scholar] [CrossRef] [PubMed]
- Salatin, S.; Barar, J.; Barzegar-Jalali, M.; Adibkia, K.; Jelvehgari, M. Thermosensitive in situ nanocomposite of rivastigmine hydrogen tartrate as an intranasal delivery system: Development, characterization, ex vivo permeation and cellular studies. Colloids Surf. B 2017, 159, 629–638. [Google Scholar] [CrossRef] [PubMed]
- Abouhussein, D.M.; Khattab, A.; Bayoumi, N.A.; Mahmoud, A.F.; Sakr, T.M. Brain targeted rivastigmine mucoadhesive thermosensitive In situ gel: Optimization, in vitro evaluation, radiolabeling, in vivo pharmacokinetics and biodistribution. J. Drug Deliv. Sci. Technol. 2018, 43, 129–140. [Google Scholar] [CrossRef]
- Naik, A.; Naik, H. Formulation and evaluation of thermosensitive biogels for nose to brain delivery of doxepin. Biomed Res. Int. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Fatouh, A.M.; Elshafeey, A.H.; Abdelbary, A. Agomelatine-based in situ gels for brain targeting via the nasal route: Statistical optimization, in vitro, and in vivo evaluation. Drug Deliv. 2017, 24, 1077–1085. [Google Scholar] [CrossRef] [PubMed]
- Pathan, I.B.; Mene, H.; Bairagi, S. Quality by design (QbD) approach to formulate in situ gelling system for nose to brain delivery of Fluoxetine hydrochloride: Ex-vivo and In-vivo study. Ars. Pharm. 2017, 58, 107–114. [Google Scholar]
- Kaur, P.; Garg, T.; Vaidya, B.; Prakash, A.; Rath, G.; Goyal, A.K. Brain delivery of intranasal in situ gel of nanoparticulated polymeric carriers containing antidepressant drug: Behavioral and biochemical assessment. J. Drug Target 2015, 23, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Pathan, I.B.; More, B. Formulation and characterization of intra nasal delivery of nortriptyline hydrochloride thermoreversible gelling system in treatment of depression. Acta Pharm. Sci. 2017, 55, 35–44. [Google Scholar] [CrossRef]
- Haque, S.; Md, S.; Sahni, J.K.; Ali, J.; Baboota, S. Development and evaluation of brain targeted intranasal alginate nanoparticles for treatment of depression. J. Psychiatr. Res. 2014, 48, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Sherje, A.P.; Londhe, V. Development and evaluation of pH-responsive cyclodextrin-based in situ gel of paliperidone for intranasal delivery. AAPS Pharm. Sci. Tech. 2018, 19, 384–394. [Google Scholar] [CrossRef] [PubMed]
- Krol, S. Challenges in drug delivery to the brain: Nature is against us. J. Control. Release 2012, 164, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Illum, L. Transport of drugs from the nasal cavity to the central nervous system. Eur. J. Pharm. Sci. 2000, 11, 1–18. [Google Scholar] [CrossRef]
- Reese, T.S.; Karnovsky, M.J. Fine structural localization of a blood-brain barrier to exogenous peroxidase. J. Cell Biol. 1967, 34, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Wong, H.L.; Wu, X.Y.; Bendayan, R. Nanotechnological advances for the delivery of CNS therapeutics. Adv. Drug Deliv. Rev. 2012, 64, 686–700. [Google Scholar] [CrossRef] [PubMed]



| Drugs | Application | Route of Administration | Side Effects |
|---|---|---|---|
| Donepezil | All stages of Alzheimer’s disease | Oral | Nausea, increased bowel movements, loss of appetite |
| Galantamine | Mild to moderate Alzheimer’s disease | Oral | Nausea, increased bowel movements, loss of appetite |
| Rivastigmine | Mild to moderate Alzheimer’s disease | Orally and transdermally | Dizziness, constipation, headache |
| Memantine | Moderate to severe Alzheimer’s disease | Oral | Dizziness, constipation, headache |
| Donepezil and memantine | Moderate to severe Alzheimer’s disease | Oral | Nausea, increased bowel movements, loss of appetite, dizziness, constipation, headache. |
| Beta interferon | Relapsing-remitting multiple sclerosis | Subcutaneous and intramuscular | Myalgia, headache, anemia, nausea |
| Glatiramer acetate | First clinical episode of multiple sclerosis | Subcutaneous | Nausea, vomiting, body ache |
| Fingolimod | Relapsing form of multiple sclerosis | Oral | Headache, diarrhea, cough |
| Teriflunomide | Relapsing form of multiple sclerosis | Oral | Liver problems, influenza, nausea, diarrhea |
| Dimethyl fumarate | Relapsing form of multiple sclerosis | Oral | Burning feeling of the skin, itching, nausea, abdominal pain, vomiting |
| Mitoxantrone | Worsening relapsing remitting multiple sclerosis | Intravenous | Nausea, diarrhea, constipation, flu-like symptoms, cardiac toxicity and risk of leukemia |
| Natalizumab | Relapsing progressive form of multiple sclerosis | Intravenous | Headache, stomach pain, diarrhea, depression |
| Quetiapine | To treat depression associated with schizophrenia | Oral | Risk of diabetes, weight gain, constipation, dizziness |
| Risperidone | Schizophrenia | Oral, intramuscular | Risk of diabetes, weight gain, constipation, dizziness |
| Paliperidone | Schizophrenia | Oral, intramuscular | Risk of diabetes, weight gain, headache. |
| Aripiprazole | Schizophrenia | Oral, intramuscular | Dizziness, nausea, vomiting, sedation |
| Asenapine | Schizophrenia | Oral | Weight gain, risk of diabetes, sedation, akathisia |
| Clozapine | Suicidal behavior associated with schizophrenia | Oral | Weight gain, sweating, seizures, sedation, risk of diabetes |
| Felbamate | Severe and refractory epilepsies | Oral | Weight loss, insomnia, dizziness, headache, ataxia, skin rashes, hepatotoxicity |
| Gabapentin | Partial seizures | Oral | Dizziness, fatigue, hyperactivity and weight gain |
| Lamotrigine | Partial seizures | Oral, intravenous | Dizziness, headache, diplopia, ataxia, skin rash |
| Vigabatrin | Partial seizures | Oral | Drowsiness, insomnia, Irritability psychosis, depression, weight gain, blindness |
| Levetiracetam | Partial seizures | Oral | Leucopenia, fatigue, dizziness, headache, anorexia, psychiatric disturbances |
| Oxcarbazepine | Partial seizures | Oral | Drowsiness, diplopia, headache, GI distress, hyponatremia, skin rash, Stevens–Johnson syndrome |
| Phenytoin | Partial seizure | Intravenous | Diplopia, nystagmus, coarsening of facial features gingival hyperplasia, hirsutism, skin rashes, Stevens–Johnson syndrome, agranulocytosis, aplastic anemia, hepatotoxicity |
| Levodopa | It is used to treat symptoms of Parkinson’s syndrome such as slow movements and stiff, rigid body parts | Oral, intravenous | Nausea, vomiting, and irregular heart rhythms |
| Sinemet | Treat nausea, vomiting, and irregular heart rhythms, which are side effect associated with levodopa | Oral | Dyskinesias |
| Pramipexole | It mimic dopamine, thus helping to produce smooth voluntary movement | Oral | Nausea, drowsiness, sleep attacks, hypotension, and hallucinations |
| Selegiline hydrochloride | It increase the amount of dopamine in the brain and reduces the motor symptoms of Parkinson’s disease | Oral | Nausea, headache, confusion, postural hypotension, hallucinations and insomnia |
| Tolcapone | It increase the amount of dopamine in the brain and reduce the motor symptoms of Parkinson’s disease | Oral | Dyskinesias, nausea, diarrhea, sleep disturbance, urine dis-coloration and hallucinations |
| Biperiden hydrochloride | It reduces tremors and muscle rigidity | Oral | Blurred vision, constipation, urinary retention, heat stroke, nervousness, anxiety, confusion, depression, delusions |
| Bioactive Agents | Formulation Composition | Neurological Disorder | Efficacy | References |
|---|---|---|---|---|
| Levodopa | Pluronic F127, chitosan | Parkinson’s syndrome | Delayed mucociliary clearance | [56] |
| Amantadine | Pluronic F127, carboxymethylcellulose | Parkinson’s syndrome | No cellular toxicity to human nasal epithelial cells | [57,58] |
| Ropinirole | Chitosan, hydroxyl propyl methyl cellulose | Parkinson’s syndrome | Enhanced brain uptake of drug in vivo | [59] |
| Rasagiline mesylate | Poloxamer 407, poloxamer 188, carbopol 934 P and chitosan | Parkinson’s syndrome | 6-fold higher drug bioavailability | [60] |
| Ropinirole | Pluronic F-127 and hydroxy methyl propyl cellulose | Parkinson’s syndrome | Five-fold brain uptake of the drug | [61] |
| Sumatriptan | Gellan gum | Migraine | High drug concentration in plasma and brain tissues | [62] |
| Huperzine A | Gellan gum | Alzheimer’s | Increased drug distributions in the rat brain tissues: the cerebrum and hippocampus | [63] |
| Curcumin | Pluronic F127, Poloxamer | Alzheimer’s | Improved drug-targeting efficiencies in the cerebrum, cerebellum, hippocampus and olfactory bulb | [64] |
| Geniposide | Poloxamers (P407, P188) and hydroxypropyl methylcellulose | Alzheimer’s | In vitro release profile of the drug was zero-order, and the ex vivo release mechanism was the Weibull model | [65] |
| Rivastigmine | Poloxamer 407®, poly(lactic-co-glycolic acid) nanoparticles | Alzheimer’s | Enhanced drug permeability and sustained drug release profile; the cellular uptake of the drug from the formulation was time dependent | [66] |
| Rivastigmine tartrate | Pluronic F127, HPMC Chitosan, Carbopol 934 and sodium carboxymethyl cellulose | Alzheimer’s | Good distribution to the brain (0.54% ID/g) when compared to intravenous administration | [67] |
| Doxepin | Chitosan and glycerophosphate, poly(ethylene) glycol | Depression | In vivo studies in Swiss albino mice showed a good increase in activity count and a decrease in immobility time | [68] |
| Agomelatine | Pluronic F127, Carbopol, chitosan, sodium carboxymethylcellulose, sodium alginate, and hydroxypropyl methylcellulose | Depression | Significantly enhanced brain uptake in vivo | [69] |
| Fluoxetine hydrochloride | Gellan gum and HPMC (hydroxypropyl methylcellulose) | Depression | Reduced immobility, increased climbing and swimming behavior | [70] |
| Tramadol hydrochloride | Chitosan, Pluronic, HPMC | Depression | Increased locomotor activity and body weight of the rat model in vivo | [71] |
| Nortriptyline hydrochloride | Poloxamer 188 and HPMC | Depression | Enhanced drug release profile | [72] |
| Venlafaxine | Sodium alginate | Depression | Brain uptake was 742.5 ng/mL, tmax 60 min; improved swimming and climbing and reduced immobility in vivo | [73] |
| Paliperidone | Carbopol 934 and hydroxypropyl methyl cellulose | Schizophrenia | High rate of drug permeation via sheep nasal mucosa | [74] |
© 2018 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aderibigbe, B.A. In Situ-Based Gels for Nose to Brain Delivery for the Treatment of Neurological Diseases. Pharmaceutics 2018, 10, 40. https://doi.org/10.3390/pharmaceutics10020040
Aderibigbe BA. In Situ-Based Gels for Nose to Brain Delivery for the Treatment of Neurological Diseases. Pharmaceutics. 2018; 10(2):40. https://doi.org/10.3390/pharmaceutics10020040
Chicago/Turabian StyleAderibigbe, Blessing Atim. 2018. "In Situ-Based Gels for Nose to Brain Delivery for the Treatment of Neurological Diseases" Pharmaceutics 10, no. 2: 40. https://doi.org/10.3390/pharmaceutics10020040
APA StyleAderibigbe, B. A. (2018). In Situ-Based Gels for Nose to Brain Delivery for the Treatment of Neurological Diseases. Pharmaceutics, 10(2), 40. https://doi.org/10.3390/pharmaceutics10020040