One-Pot Synthesis of Epirubicin-Capped Silver Nanoparticles and Their Anticancer Activity against Hep G2 Cells
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals and Reagents
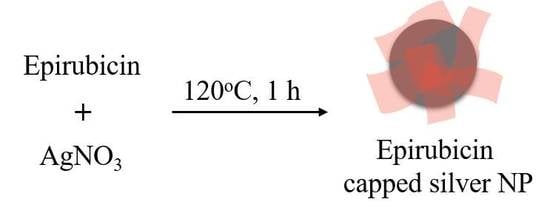
2.2. Preparation of Epirubicin-Capped Silver NPs
2.3. Characterization of Epirubicin-Capped Silver NPs
2.4. Cytotoxicity Assay
3. Results and Discussion
3.1. Characterization
3.2. Evaluation of Antitumor Activity
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Burda, C.; Chen, X.B.; Narayanan, R.; El-Sayed, M.A. Chemistry and properties of nanocrystals of different shapes. Chem. Rev. 2005, 105, 1025–1102. [Google Scholar] [CrossRef] [PubMed]
- Rosi, N.L.; Mirkin, C.A. Nanostructures in biodiagnostics. Chem. Rev. 2005, 105, 1547–1562. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.Z.; Langer, R.; Farokhzad, O.C. Nanoparticle delivery of cancer drugs. Annu. Rev. Med. 2012, 6363, 185–198. [Google Scholar] [CrossRef] [PubMed]
- Lok, C.N.; Zou, T.; Zhang, J.J.; Lin, I.W.S.; Che, C.M. Controlled-release systems for metal-based nanomedicine: Encapsulated/self-assembled nanoparticles of anticancer gold(iii)/platinum(ii) complexes and antimicrobial silver nanoparticles. Adv. Mater. 2014, 26, 5550–5557. [Google Scholar] [CrossRef] [PubMed]
- Locatelli, E.; Naddaka, M.; Uboldi, C.; Loudos, G.; Fragogeorgi, E.; Molinari, V.; Pucci, A.; Tsotakos, T.; Psimadas, D.; Ponti, J.; et al. Targeted delivery of silver nanoparticles and alisertib: In vitro and in vivo synergistic effect against glioblastoma. Nanomedicine 2014, 9, 839–849. [Google Scholar] [CrossRef]
- Prabhakar, U.; Maeda, H.; Jain, R.K.; Sevick-Muraca, E.M.; Zamboni, W.; Farokhzad, O.C.; Barry, S.T.; Gabizon, A.; Grodzinski, P.; Blakey, D.C. Challenges and key considerations of the enhanced permeability and retention effect for nanomedicine drug delivery in oncology. Cancer Res. 2013, 73, 2412–2417. [Google Scholar] [CrossRef] [PubMed]
- Duncan, R.; Sat-Klopsch, Y.N.; Burger, A.M.; Bibby, M.C.; Fiebig, H.H.; Sausville, E.A. Validation of tumour models for use in anticancer nanomedicine evaluation: The epr effect and cathepsin b-mediated drug release rate. Cancer Chemother. Pharmacol. 2013, 72, 417–427. [Google Scholar] [CrossRef] [PubMed]
- Boca, S.C.; Potara, M.; Gabudean, A.M.; Juhem, A.; Baldeck, P.L.; Astilean, S. Chitosan-coated triangular silver nanoparticles as a novel class of biocompatible, highly effective photothermal transducers for in vitro cancer cell therapy. Cancer Lett. 2011, 311, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Di Corato, R.; Palumberi, D.; Marotta, R.; Scotto, M.; Carregal-Romero, S.; Rivera, G.P.; Parak, W.J.; Pellegrino, T. Magnetic nanobeads decorated with silver nanoparticles as cytotoxic agents and photothermal probes. Small 2012, 8, 2731–2742. [Google Scholar] [CrossRef]
- Jain, P.K.; Huang, X.H.; El-Sayed, I.H.; El-Sayed, M.A. Noble metals on the nanoscale: Optical and photothermal properties and some applications in imaging, sensing, biology, and medicine. Acc. Chem. Res. 2008, 41, 1578–1586. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Zhou, T.; Berliner, A.; Banerjee, P.; Zhou, S. Smart core−shell hybrid nanogels with ag nanoparticle core for cancer cell imaging and gel shell for ph-regulated drug delivery. Chem. Mater. 2010, 22, 1966–1976. [Google Scholar] [CrossRef]
- Zong, S.; Wang, Z.; Yang, J.; Wang, C.; Xu, S.; Cui, Y. A sers and fluorescence dual mode cancer cell targeting probe based on silica coated au@ag core–shell nanorods. Talanta 2012, 97, 368–375. [Google Scholar] [CrossRef]
- Shenashen, M.A.; El-Safty, S.A.; Elshehy, E.A. Synthesis, morphological control, and properties of silver nanoparticles in potential applications. Part. Part. Syst. Charact. 2014, 31, 293–316. [Google Scholar]
- Begum, N.A.; Mondal, S.; Basu, S.; Laskar, R.A.; Mandal, D. Biogenic synthesis of au and ag nanoparticles using aqueous solutions of black tea leaf extracts. Colloid. Surf. B 2009, 71, 113–118. [Google Scholar]
- Krishnaraj, C.; Jagan, E.G.; Rajasekar, S.; Selvakumar, P.; Kalaichelvan, P.T.; Mohan, N. Synthesis of silver nanoparticles using acalypha indica leaf extracts and its antibacterial activity against water borne pathogens. Colloid. Surf. B 2010, 76, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Mittal, A.K.; Bhaumik, J.; Kumar, S.; Banerjee, U.C. Biosynthesis of silver nanoparticles: Elucidation of prospective mechanism and therapeutic potential. J. Colloid Interface Sci. 2014, 415, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Nagata, M.; Matsuo, Y.; Hidaka, M.; Kawano, Y.; Okumura, M.; Tokunaga, J.; Takamura, N.; Arimori, K. Effect of acute hepatic failure on epirubicin pharmacokinetics after intrahepatic arterial injection in rats. Biol. Pharm. Bull. 2008, 31, 493–496. [Google Scholar] [CrossRef]
- Li, S.Y.; Wang, M. Novel core–shell structured paclitaxel-loaded plga@ag–au nanoparticles. Mater. Lett. 2013, 92, 350–353. [Google Scholar] [CrossRef]
- Bettini, S.; Pagano, R.; Valli, L.; Giancane, G. Drastic nickel ion removal from aqueous solution by curcumin-capped ag nanoparticles. Nanoscale 2014, 6, 10113–10117. [Google Scholar] [PubMed]
- Sweeney, S.F.; Woehrle, G.H.; Hutchison, J.E. Rapid purification and size separation of gold nanoparticles via diafiltration. J. Am. Chem. Soc. 2006, 128, 3190–3197. [Google Scholar] [CrossRef] [PubMed]
- Min, K.H.; Park, K.; Kim, Y.S.; Bae, S.M.; Lee, S.; Jo, H.G.; Park, R.W.; Kim, I.S.; Jeong, S.Y.; Kim, K.; et al. Hydrophobically modified glycol chitosan nanoparticles-encapsulated camptothecin enhance the drug stability and tumor targeting in cancer therapy. J. Control. Release 2008, 127, 208–218. [Google Scholar] [CrossRef]
- Skehan, P.; Storeng, R.; Scudiero, D.; Monks, A.; McMahon, J.; Vistica, D.; Warren, J.T.; Bokesch, H.; Kenney, S.; Boyd, M.R. New colorimetric cytotoxicity assay for anticancer-drug screening. J. Natl. Cancer Inst. 1990, 82, 1107–1112. [Google Scholar] [CrossRef]
- DeLean, A.; Munson, P.J.; Rodbard, D. Simultaneous analysis of families of sigmoidal curves: Application to bioassay, radioligand assay, and physiological dose-response curves. Am. J. Physiol. 1978, 235, 97–102. [Google Scholar] [CrossRef]
- Fomenko, I.; Durst, M.; Balaban, D. Robust regression for high throughput drug screening. Comput. Methods Programs Biomed. 2006, 82, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Gubler, H.; Schopfer, U.; Jacoby, E. Theoretical and experimental relationships between percent inhibition and IC50 data observed in high-throughput screening. J. Biomol. Screen. 2018, 18, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Evangelatov, A.; Skrobanska, R.; Mladenov, N.; Petkova, M.; Yordanov, G.; Pankov, R. Epirubicin loading in poly(butyl cyanoacrylate) nanoparticles manifests via altered intracellular localization and cellular response in cervical carcinoma (hela) cells. Drug Deliv. 2016, 23, 2235–2244. [Google Scholar]
- Akter, M.; Sikder, M.T.; Rahman, M.M.; Ullah, A.K.M.A.; Hossain, K.F.B.; Banik, S.; Hosokawa, T.; Saito, T.; Kurasaki, M. A systematic review on silver nanoparticles-induced cytotoxicity: Physicochemical properties and perspectives. J. Adv. Res. 2018, 9, 1–16. [Google Scholar] [PubMed]
- Zhang, H.Z.; Li, X.M.; Gao, F.P.; Liu, L.R.; Zhou, Z.M.; Zhang, Q.Q. Preparation of folate-modified pullulan acetate nanoparticles for tumor-targeted drug delivery. Drug Deliv. 2010, 17, 48–57. [Google Scholar] [PubMed]
- Di-Wen, S.; Pan, G.Z.; Hao, L.; Zhang, J.; Xue, Q.Z.; Wang, P.; Yuan, Q.Z. Improved antitumor activity of epirubicin-loaded cxcr4-targeted polymeric nanoparticles in liver cancers. Int. J. Pharm. 2016, 500, 54–61. [Google Scholar] [PubMed]
- Tariq, M.; Alam, M.A.; Singh, A.T.; Iqbal, Z.; Panda, A.K.; Talegaonkar, S. Biodegradable polymeric nanoparticles for oral delivery of epirubicin: In vitro, ex vivo, and in vivo investigations. Colloid. Surf. B 2015, 128, 448–456. [Google Scholar] [CrossRef] [PubMed]





| Drug | IC50 (μg/mL) | Hill Slope |
|---|---|---|
| Epirubicin-capped silver NPs | 1.92 | 2.43 |
| Epirubicin | 0.11 | 0.57 |
| Nanoparticle | Cell | IC50 | Reference |
|---|---|---|---|
| Epirubicin-loaded folate-modified PA nanoparticles | Human nasopharyngeal epidermal carcinoma cell | 2.75 μg/mL | [28] |
| Epirubicin-loaded PLGA/TPGS nanoparticles | Hep G2 cells | 0.78 μg/mL | [29] |
| Epirubicin-loaded poly(lactic-co-glycolic acid) nanoparticles | MCF-7 cells | 824 nM | [30] |
| Epirubicin-capped silver NPs | Hep G2 cells | 0.11 μg/mL | This work |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ding, J.; Chen, G.; Chen, G.; Guo, M. One-Pot Synthesis of Epirubicin-Capped Silver Nanoparticles and Their Anticancer Activity against Hep G2 Cells. Pharmaceutics 2019, 11, 123. https://doi.org/10.3390/pharmaceutics11030123
Ding J, Chen G, Chen G, Guo M. One-Pot Synthesis of Epirubicin-Capped Silver Nanoparticles and Their Anticancer Activity against Hep G2 Cells. Pharmaceutics. 2019; 11(3):123. https://doi.org/10.3390/pharmaceutics11030123
Chicago/Turabian StyleDing, Jun, Guilin Chen, Guofang Chen, and Mingquan Guo. 2019. "One-Pot Synthesis of Epirubicin-Capped Silver Nanoparticles and Their Anticancer Activity against Hep G2 Cells" Pharmaceutics 11, no. 3: 123. https://doi.org/10.3390/pharmaceutics11030123
APA StyleDing, J., Chen, G., Chen, G., & Guo, M. (2019). One-Pot Synthesis of Epirubicin-Capped Silver Nanoparticles and Their Anticancer Activity against Hep G2 Cells. Pharmaceutics, 11(3), 123. https://doi.org/10.3390/pharmaceutics11030123