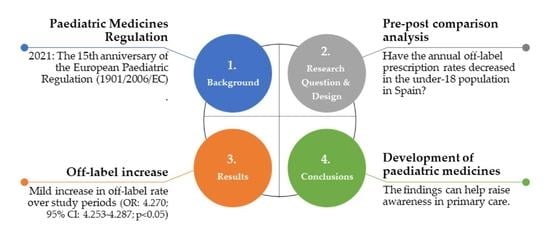
Effects of the Off-Label Drug Prescription in the Paediatric Population in Spain from the Adoption of the Latest European Regulation: A Pre-Post Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Population and Eligibility Criteria
2.3. Data Sources
2.4. Variables
2.5. Data Analysis
3. Results
3.1. Total Prescriptions and Off-Label Rates in the Under-18 Population: Global Results
3.2. Total Prescriptions and Off-Label Rates in the Under-18 Population: Results by Age Group
4. Discussion
4.1. Total Prescriptions and Off-Label Rates in the Under-18 Population: Global Results
4.2. Total Prescriptions and Off-Label Rates in the Under-18 Population: Results by Age Group
4.3. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Official Journal of the European Union. Regulation (EC) No 1901/2006 of the European Parliament and of the Council of 12 December 2006 on Medicinal Products for Paediatric Use and Amending Regulation (EEC) No 1768/92, Directive 2001/20/EC, Directive 2001/83/EC and Regulation (EC) No 726/2004 (Text with EEA Relevance). OJ L 378, of 27 Dec 2006. pp. 1–19, [Updated 28 January 2019]. Available online: http://data.europa.eu/eli/reg/2006/1901/oj (accessed on 25 January 2021).
- European Medicines Agency (EMA). Paediatric Investigation Plans. Available online: https://www.ema.europa.eu/en/human-regulatory/research-development/paediatric-medicines/paediatric-investigation-plans (accessed on 25 January 2021).
- European Federation of Pharmaceutical Industries and Associations (EFPIA). Clinical Trials. Available online: https://www.efpia.eu/about-medicines/development-of-medicines/regulations-safety-supply/clinical-trials/ (accessed on 25 January 2021).
- European Commission. Joint Evaluation of Regulation (EC) No 1901/2006 of the European Parliament and of the Council of 12 December 2006 on Medicinal Products for Paediatric Use and Regulation (EC) No 141/2000 of the European Parliament and of the Council of 16 December 1999 on Orphan Medicinal Products. Part 1/6. SWD (2020) 163 Final. Commission Staff Working Document. Brussels: European Union. 11 August 2020. Available online: https://ec.europa.eu/health/sites/health/files/files/paediatrics/docs/orphan-regulation_eval_swd_2020-163_part-1.pdf (accessed on 25 January 2021).
- Weda, M.; Hoebert, J.; Vervloet, M.; Moltó, C.; Damen, N.; Marchange, S.; Langedijk, J.; Lisman, J.; van Dijk, L. Study on Off-Label Use of Medicinal Products in the European Union. Brussels: European Union. 2017, pp. 1–193. Available online: https://ec.europa.eu/health/sites/health/files/files/documents/2017_02_28_final_study_report_on_off-label_use_.pdf (accessed on 25 January 2021).
- European Medicines Agency (EMA). How to Better Apply the Paediatric Regulation to Boost Development of Medicines for Children. Report on a Multi-Stakeholder Workshop Held at EMA on 20 March 2018. EMA/224241/2018. Available online: https://www.ema.europa.eu/en/documents/report/how-better-apply-paediatric-legislation-boost-development-medicines-children-report-multi_en.pdf (accessed on 25 January 2021).
- Schrier, L.; Hadjipanayis, A.; Stiris, T.; Ross-Russell, R.I.; Valiulis, A.; Turner, M.A.; Zhao, W.; De Cock, P.; De Wildt, S.N.; Allegaert, K.; et al. Off-label use of Medicines in neonates, infants, children, and adolescents: A joint policy statement by the european academy of paediatrics and the european society for developmental perinatal and pediatric pharmacology. Eur. J. Pediatr. 2020, 179, 839–847. [Google Scholar] [CrossRef] [PubMed]
- Kargodorian, J.; Rocher-Redondo, A.; Modamio, P.; Lizano, I.; Lastra, C.F.; Mariño, E.L. Off-label use of medicines in paediatrics during the years 2015 and 2016 in Spain. Int. J. Clin. Pharm. 2018, 40, 216–217. [Google Scholar]
- Dedeu, T.; Bolibar, B.; Gené, J.; Pareja, C.; Violan, C. Copenhagen (Denmark): European observatory on health systems and policies. In Building Primary Care in a Changing Europe: Case Studies; Observatory Studies Series, No. 40; Kringos, D.S., Boerma, W.G.W., Hutchinson, A., Saltman, R.B., Eds.; World Health Organization (WHO): Copenhagen, Denmark, 2015; pp. 253–264. Available online: https://www.ncbi.nlm.nih.gov/books/NBK459029/ (accessed on 25 January 2021).
- Ministry of Health, Social Services and Equality. 2018 Annual Report on the National Health System. Available online: http://www.mscbs.es/estadEstudios/estadisticas/sisInfSanSNS/tablasEstadisticas/InfAnualSNS2018/Cap.4_R.Humanos.pdf (accessed on 25 January 2021).
- National Statistics Institute (INE). Demography and Population. Available online: https://www.ine.es/en/index.htm (accessed on 25 January 2021).
- IQVIA. The Pharmaceutical Market (Spain). 2020. Available online: https://www.iqvia.com/ (accessed on 1 December 2020).
- Spanish General Council of Official Colleges of Pharmacists (CGCOF). BotPlus 2.0. Available online: https://botplusweb.portalfarma.com/ (accessed on 25 January 2021).
- World Health Organization (WHO) Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index [Updated 16 December 2019]. Available online: https://www.whocc.no/atc_ddd_index/ (accessed on 25 January 2021).
- European Medicines Agency (EMA). Clinical Investigation of Medicinal Products in the Paediatric Population (CPMP/ICH/2711/99). ICH Topic E11. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/international-conference-harmonisation-technical-requirements-registration-pharmaceuticals-human-use_en-1.pdf (accessed on 25 January 2021).
- Official State Gazette (BOE). Royal Decree-Law 16/2012, of April, 20, 2012, on Urgent Measures to Guarantee the Sustainability of the National Health System and Improve the Quality and Safety of its Services, 24 April 2012; pp. 31278–31312, BOE 98, BOE-A-2012-5403. [Updated 1 July 2017].
- Official State Gazette (BOE). Law 25/1990, of December 20, on Medicines, 22 December 1990; pp. 382228–382246, BOE 306, BOE-A-1990-30938. [Revoked 28 July 2006].
- Official State Gazette (BOE). Royal Legislative Decree 1/2015, of July 24, Approving the Revised Text of the La Won Guarantees and Rational Use of Medicines and Medical Devices Are Approved, 25 July 2015; pp. 62935–63030, BOE 177, BOE-A-2015-8343. [Updated 31 December 2020].
- Ruiz-Antoran, B.; Agusti, A.; Vallano, A.; Danés, I.; Riba, N.; Mateu, S.; Costa, J.; Santiago, M.B.S.; Laredo, L.; Quintana, J.A.D.; et al. Use of non-specific intravenous human immunoglobulins in Spanish hospitals; need for a hospital protocol. Eur. J. Clin. Pharmacol. 2010, 66, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Allen, H.C.; Garbe, M.C.; Lees, J.; Aziz, N.; Chaaban, H.; Miller, J.L.; Johnson, P.; DeLeon, S. Off-label medication use in children, more common than we think: A systematic review of the literature. J. Okla State Med. Assoc. 2018, 111, 776–783. [Google Scholar] [PubMed]
- Blanco-Reina, E.; Medina-Claros, A.F.; Vega-Jiménez, M.A.; Ocaña-Riola, R.; Márquez-Romero, E.I.; Ruiz-Extremera, A. Drug utilization pattern in children and off-label use of medicines in a pediatric intensive care unit. Med. Intensiva 2016, 40, 1–8. [Google Scholar] [CrossRef] [PubMed]
- García-López, I.; Fuentes-Ríos, J.E.; Manrique-Rodríguez, S.; Fernández-Llamazares, C. Off-label and unlicensed drug use: Results from a pilot study in a pediatric intensive care unit. An. Pediatr. 2017, 86, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Piñeiro, R.; Ruiz, M.B.; Avendaño, C.; Román, E.; Cabrera, L.; Cilleruelo, M.J.; Mellado Peña, M.J. Results from the 2012–2013 paediatric national survey on off-label drug use in children in Spain (OL-PED study). An. Pediatr. 2014, 81, 16–21. [Google Scholar]
- Official State Gazette (BOE). Royal Decree 1015/2009, of June 19, which Regulates Access to Medicinal Products in Special Situations, 20 July 2009; pp. 60904–60913, BOE 174, BOE-A-2009-12002. [Updated 27 July 2013].
- Almeida Andrade, S.R.; Nascimento de Moraes Santos, P.A.; Santos Andrade, P.H.; Barros da Silva, W. Unlicensed and off-label prescription of drugs to children in primary health care: A systematic review. J. Evid.-Based Med. 2020, 13, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Van den Anker, J.N.; McCune, S.; Annaert, P.; Baer, G.R.; Mulugeta, Y.; Abdelrahman, R.; Wu, K.; Krudys, K.M.; Fisher, J.; Slikker, W.; et al. Approaches to dose finding in neonates, illustrating the variability between neonatal drug development programs. Pharmaceutics 2020, 12, 685. [Google Scholar] [CrossRef] [PubMed]
| Inconsistency Description | Examples | Assumption/Decision |
|---|---|---|
| Medicines with the same active ingredient, similar formulation and administration route, where low doses were classified as off-label but not high doses. | Pantoprazole and Omeprazole 20 mg (tablets or capsules) were defined as off-label in the under-18 population but not 40 mg. | Pantoprazole and Omeprazole 20 mg (tablets or capsules) were considered off-label in the under-18 population. |
| Paracetamol 500 mg effervescent tablets and 1 g tablets (effervescent or not) were defined as off-label in the under-18 population, but not 500 mg tablets or capsules. | Paracetamol 500 mg tablets and capsules were considered off-label in the under-18 population. | |
| Topical medicines with the same active ingredient, same dose or concentration and administration route, where some formulations were classified as off-label, but others were not depending on the formulation. | Similar formulations: Ketoconazole cream was defined as off-label in the under-18 population but not the gel, which is also a semi-solid. Both were formulated with the same concentration (2%; 20 mg/g). | Both Ketoconazole cream and Ketoconazole gel were considered off-label in the under-18 population. |
| Topical medicines with the same active ingredient, different dose or concentration and same administration route, where some formulations were classified as off-label, but others were not depending on the formulation. | Different formulations: Centella asiatica herba in combination with antibiotics formulated as powder (solid) was defined as off-label in the under-18 population but not the ointment (semi-solid). Both were formulated with a different concentration (powder, 1%; ointment, 2%). | Only Centella asiatica herba powder was considered off-label in the under-18 population. |
| Topical medicines with the same active ingredient, same dose or concentration and administration route, where some formulations were classified as off-label, but others were not depending on whether they were brands or generics. | In the case of Ciclopirox, the variability in off-label designation depended on the brand name, ranging from nail lacquer to shampoo, topical solution and cream. | For Ciclopirox brand names, the off-label designation was assessed following BotPlus 2.0 criteria brand by brand in the under-18 population. |
| In the case of Ciclopirox generics, all formulations have been assessed as potentially off-label in the under-18 population. | ||
| Medicines with many generics in the market, where some were classified as off-label, but others were not. | Many generics of Paracetamol 1 g and 500 mg tablets. | Due to the high number of cases identified under this condition, all Paracetamol 1 g and 500 mg prescriptions by active ingredient were assessed as potentially off-label in the under-18 population. |
| Period (MAT) | Prescriptions (Total), n | Prescriptions by Brand Name, n (%) * | Prescriptions by Active Ingredient, n (%) * | Off-Label Prescriptions (Total), n (%) * | Off-Label Prescriptions by Brand Name, n (%) *,† | Off-Label Prescriptions by Active Ingredient, n (%) *,† |
|---|---|---|---|---|---|---|
| October 2004–September 2005 | 44,348,661 | 37,916,646 (85%) | 6,432,015 (15%) | 2,924,240 (7%) | 1,171,325 (3%; 3%) | 1,752,915 (4%; 27%) |
| October 2017–September 2018 | 37,698,501 | 26,838,326 (71%) | 10,860,175 (29%) | 2,098,955 (6%) | 1,372,365 (4%; 5%) | 726,590 (2%; 7%) |
| October 2018–September 2019 | 37,135,180 | 26,974,055 (73%) | 10,161,125 (27%) | 2,686,781 (7%) | 2,154,107 (6%; 8%) | 532,674 (1%; 5%) |
| October 2019–September 2020 | 32,385,213 | 23,546,363 (73%) | 8,838,850 (27%) | 2,577,342 (8%) | 2,037,325 (6%; 9%) | 540,017 (2%; 6%) |
| Period (MAT) | Regulation in Force | Comments |
|---|---|---|
| October 2004–September 2005 | Law 25/1990 [17] | Aim: The primary objective is to contribute to the provision of safe, effective and quality medicines, properly identified and with appropriate information. Prescription of medicines: No specific references to the prioritization of generics over branded medicines are included. |
| October 2017–September 2018 | Royal Legislative Decree 1/2015 [18] | Aim: To guarantee the quality of all benefits being provided by the Spanish National Health System, ensuring better protections for the rational use of medicines and that access to medicines is done through a more effective system with tighter safety controls. Prescription of medicines: The general rule is to prescribe by active ingredient whereby the least expensive medicinal product within its homogeneous group * will be supplied and, if the prices are the same, the appropriate generic or biosimilar medicinal product will be supplied.
|
| October 2018–September 2019 | ||
| October 2019–September 2020 |
| Period | Active Ingredient | Off-Label Prescriptions (Total), n (%) * | |
|---|---|---|---|
| October 2004–September 2005 | Ibuprofen | 1,092,261 | (37%) |
| Paracetamol | 759,027 | (26%) | |
| Silicones | 130,981 | (4%) | |
| Dexamethasone and anti-infectives | 129,455 | (4%) | |
| Budesonide | 125,352 | (4%) | |
| Methylprednisolone aceponate | 119,932 | (4%) | |
| Acetylcysteine | 78,621 | (3%) | |
| Benzydamine | 49,359 | (2%) | |
| Ketoconazole | 38,289 | (1%) | |
| Domperidone | 29,477 | (1%) | |
| October 2017– September 2018 | Colecalciferol | 503,925 | (24%) |
| Paracetamol | 241,082 | (11%) | |
| Budesonide | 142,668 | (7%) | |
| Omeprazole | 118,773 | (6%) | |
| Ibuprofen | 113,440 | (5%) | |
| Ketoconazole | 93,149 | (4%) | |
| Acetylcysteine | 90,283 | (4%) | |
| Methylprednisolone aceponate | 84,551 | (4%) | |
| Dexamethasone and anti-infectives | 52,953 | (3%) | |
| Terbinafine | 45,736 | (2%) | |
| October 2018–September 2019 | Colecalciferol | 623,089 | (23%) |
| Mepyramine theophyllinacetate | 579,251 | (22%) | |
| Paracetamol | 224,193 | (8%) | |
| Budesonide | 116,142 | (4%) | |
| Omeprazole | 95,049 | (4%) | |
| Dexamethasone and anti-infectives | 72,970 | (3%) | |
| Acetylcysteine | 63,630 | (2%) | |
| Methylprednisolone aceponate | 61,324 | (2%) | |
| Ketoconazole | 60,069 | (2%) | |
| Silicones | 59,920 | (2%) | |
| October 2019–September 2020 | Colecalciferol | 658,774 | (26%) |
| Mepyramine theophyllinacetate | 360,325 | (14%) | |
| Dexchlorpheniramine | 199,125 | (8%) | |
| Paracetamol | 197,504 | (8%) | |
| Budesonide | 105,940 | (4%) | |
| Omeprazole | 104,163 | (4%) | |
| Methylprednisolone aceponate | 78,827 | (3%) | |
| Ciclopirox | 62,718 | (2%) | |
| Dexamethasone and anti-infectives | 60,289 | (2%) | |
| Silicones | 59,611 | (2%) | |
| Period | Pharmacological Subgroups (ATC Code and Description) | Off-Label Prescriptions (Total), n (%) * | ||
|---|---|---|---|---|
| October 2004–September 2005 | M01A | Anti-inflammatory and antirheumatic products, non-steroids | 1,121,520 | (38%) |
| N02B | Other analgesics and antipyretics | 760,808 | (26%) | |
| A03A | Drugs for functional gastrointestinal disorders | 130,981 | (4%) | |
| S03C | Corticosteroids and anti-infectives in combination | 129,455 | (4%) | |
| R01A | Decongestants and other nasal preparations for topical use | 123,399 | (4%) | |
| October 2017–September 2018 | A11C | Vitamin A and D, incl, combinations of the two | 505,517 | (24%) |
| N02B | Other analgesics and antipyretics | 242,700 | (12%) | |
| A02B | Drugs for peptic ulcer and gastro-esophageal reflux disease | 159,644 | (8%) | |
| M01A | Anti-inflammatory and antirheumatic products, non-steroids | 151,669 | (7%) | |
| A07E | Intestinal anti-inflammatory agents | 148,852 | (7%) | |
| October 2018–September 2019 | A11C | Vitamin A and D, incl. combinations of the two | 646,194 | (24%) |
| R03D | Other systemic drugs for obstructive airway diseases | 579,251 | (22%) | |
| N02B | Other analgesics and antipyretics | 224,193 | (8%) | |
| A02B | Drugs for peptic ulcer and gastro-esophageal reflux disease | 127,022 | (5%) | |
| R01A | Decongestants and other nasal preparations for topical use | 119,031 | (4%) | |
| October 2019–September 2020 | A11C | Vitamin A and D, incl. combinations of the two | 674,105 | (26%) |
| R03D | Other systemic drugs for obstructive airway diseases | 360,325 | (14%) | |
| R06A | Antihistamines for systemic use | 199,125 | (8%) | |
| N02B | Other analgesics and antipyretics | 197,504 | (8%) | |
| A02B | Drugs for peptic ulcer and gastro-esophageal reflux disease | 137,866 | (5%) | |
| Period (MAT) | <1 Year Old | 1–<2 Years Old | 2–11 Years Old | 12–<18 Years Old | ||||
|---|---|---|---|---|---|---|---|---|
| Prescriptions (Total), n (%) * | Off-Label Prescriptions, n (%) **,§ | Prescriptions (Total), n (%) * | Off-Label Prescriptions, n (%) **,§ | Prescriptions (Total), n (%) * | Off-Label Prescriptions, n (%) **,§ | Prescriptions (Total), n (%) * | Off-Label Prescriptions, n (%) **,§ | |
| October 2004 –September 2005 | 7,315,428 (16%) | 287,438 (4%; 10%) | 4,476,495 (10%) | 173,453 (4%; 6%) | 29,011,169 (65%) | 1,882,158 (6%; 64%) | 3,545,569 (8%) | 581,191 (16%; 20%) |
| October 2017–September 2018 | 5,126,880 (14%) | 545,457 (11%; 26%) | 3,086,318 (8%) | 75,746 (2%; 4%) | 24,640,700 (65%) | 857,149 (3%; 41%) | 4,844,603 (13%) | 620,603 (13%; 30%) |
| October 2018–September 2019 | 5,148,416 (14%) | 871,102 (17%; 32%) | 2,982,650 (8%) | 141,300 (5%; 5%) | 24,126,595 (65%) | 1,025,690 (4%; 38%) | 4,877,519 (13%) | 648,689 (13%; 24%) |
| October 2019–September 2020 | 5,193,250 (16%) | 883,044 (17%; 34%) | 2,552,232 (8%) | 131,328 (5%; 5%) | 20,128,907 (62%) | 1,002,657 (5%; 39%) | 4,510,824 (14%) | 560,313 (12%; 22%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lizano-Díez, I.; Aldalur-Uranga, I.; Figueiredo-Escribá, C.; Lastra, C.F.; Mariño, E.L.; Modamio, P. Effects of the Off-Label Drug Prescription in the Paediatric Population in Spain from the Adoption of the Latest European Regulation: A Pre-Post Study. Pharmaceutics 2021, 13, 588. https://doi.org/10.3390/pharmaceutics13040588
Lizano-Díez I, Aldalur-Uranga I, Figueiredo-Escribá C, Lastra CF, Mariño EL, Modamio P. Effects of the Off-Label Drug Prescription in the Paediatric Population in Spain from the Adoption of the Latest European Regulation: A Pre-Post Study. Pharmaceutics. 2021; 13(4):588. https://doi.org/10.3390/pharmaceutics13040588
Chicago/Turabian StyleLizano-Díez, Irene, Itziar Aldalur-Uranga, Carlos Figueiredo-Escribá, Cecilia F. Lastra, Eduardo L. Mariño, and Pilar Modamio. 2021. "Effects of the Off-Label Drug Prescription in the Paediatric Population in Spain from the Adoption of the Latest European Regulation: A Pre-Post Study" Pharmaceutics 13, no. 4: 588. https://doi.org/10.3390/pharmaceutics13040588
APA StyleLizano-Díez, I., Aldalur-Uranga, I., Figueiredo-Escribá, C., Lastra, C. F., Mariño, E. L., & Modamio, P. (2021). Effects of the Off-Label Drug Prescription in the Paediatric Population in Spain from the Adoption of the Latest European Regulation: A Pre-Post Study. Pharmaceutics, 13(4), 588. https://doi.org/10.3390/pharmaceutics13040588