An Insight into Biomolecules for the Treatment of Skin Infectious Diseases
Abstract
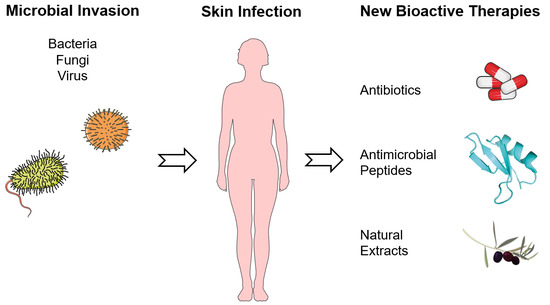
:1. Introduction
2. Skin: The First Line of Defense
3. Biomolecules: Types, Properties, and Mechanisms of Action against Pathogens
3.1. Antibiotics
3.2. Antimicrobial Peptides
3.3. Natural Extracts
4. Prevalent Skin Infections and the Biomolecules Employed in Their Treatment
4.1. Atopic Dermatitis
4.2. Psoriasis
4.3. Herpes Simplex and Zoster
4.4. Acne
4.5. Tinea
4.6. Wound- and Burn-Derived Infections
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rohr, J.R.; Barrett, C.B.; Civitello, D.J.; Craft, M.E.; Delius, B.; DeLeo, G.A.; Hudson, P.J.; Jouanard, N.; Nguyen, K.H.; Ostfeld, R.S. Emerging human infectious diseases and the links to global food production. Nat. Sustain. 2019, 2, 445–456. [Google Scholar] [CrossRef]
- Jones, K.E.; Patel, N.G.; Levy, M.A.; Storeygard, A.; Balk, D.; Gittleman, J.L.; Daszak, P. Global trends in emerging infectious diseases. Nature 2008, 451, 990–993. [Google Scholar] [CrossRef]
- Kumar, S.; Bhatt, M.L.; Saxena, S.K. Global trends in emerging viral infectious diseases: Challenges to the mankind. RASSA J. Sci. Soc. 2019, 1, 7–12. [Google Scholar]
- Bloom, D.E.; Black, S.; Rappuoli, R. Emerging infectious diseases: A proactive approach. Proc. Natl. Acad. Sci. USA 2017, 114, 4055–4059. [Google Scholar] [CrossRef] [Green Version]
- Tizek, L.; Schielein, M.; Seifert, F.; Biedermann, T.; Böhner, A.; Zink, A. Skin diseases are more common than we think: Screening results of an unreferred population at the Munich Oktoberfest. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 1421–1428. [Google Scholar] [CrossRef]
- Seth, D.; Cheldize, K.; Brown, D.; Freeman, E.E. Global burden of skin disease: Inequities and innovations. Curr. Dermatol. Rep. 2017, 6, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Kwiecien, K.; Zegar, A.; Jung, J.; Brzoza, P.; Kwitniewski, M.; Godlewska, U.; Grygier, B.; Kwiecinska, P.; Morytko, A.; Cichy, J. Architecture of antimicrobial skin defense. Cytokine Growth Factor Rev. 2019, 49, 70–84. [Google Scholar] [CrossRef] [PubMed]
- Tavares, T.D.; Antunes, J.C.; Ferreira, F.; Felgueiras, H.P. Biofunctionalization of natural fiber-reinforced biocomposites for biomedical applications. Biomolecules 2020, 10, 148. [Google Scholar] [CrossRef] [Green Version]
- Kaye, K.S.; Petty, L.A.; Shorr, A.F.; Zilberberg, M.D. Current epidemiology, etiology, and burden of acute skin infections in the United States. Clin. Infect. Dis. 2019, 68, S193–S199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miranda, C.S.; Ribeiro, A.R.; Homem, N.C.; Felgueiras, H.P. Spun Biotextiles in Tissue Engineering and Biomolecules Delivery Systems. Antibiotics 2020, 9, 174. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, M.A.; Amorim, M.T.P.; Felgueiras, H.P. Poly (vinyl alcohol)-based nanofibrous electrospun scaffolds for tissue engineering applications. Polymers 2020, 12, 7. [Google Scholar] [CrossRef] [Green Version]
- Teixeira, M.A.; Paiva, M.C.; Amorim, M.T.P. Electrospun nanocomposites containing cellulose and its derivatives modified with specialized biomolecules for an enhanced wound healing. Nanomater 2020, 10, 557. [Google Scholar] [CrossRef] [Green Version]
- Godlewska, U.; Brzoza, P.; Kwiecień, K.; Kwitniewski, M.; Cichy, J. Metagenomic Studies in Inflammatory Skin Diseases. Curr. Microbiol. 2020, 77, 3201–3212. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.E.; Fischbach, M.A.; Belkaid, Y. Skin microbiota–host interactions. Nature 2018, 553, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.H. Aging of the skin barrier. Clin. Dermatol. 2019, 37, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Lebre, M.C.; van der Aar, A.M.; van Baarsen, L.; van Capel, T.M.; Schuitemaker, J.H.; Kapsenberg, M.L.; de Jong, E.C. Human keratinocytes express functional Toll-like receptor 3, 4, 5, and 9. J. Investig. Dermatol. 2007, 127, 331–341. [Google Scholar] [CrossRef] [Green Version]
- Felgueiras, H.P.; Amorim, M.T.P. Functionalization of electrospun polymeric wound dressings with antimicrobial peptides. Colloids Surf. B 2017, 156, 133–148. [Google Scholar] [CrossRef]
- Fischer, C.L. Antimicrobial activity of host-derived lipids. Antibiotics 2020, 9, 75. [Google Scholar] [CrossRef] [PubMed]
- Strnadova, K.; Sandera, V.; Dvorankova, B.; Kodet, O.; Duskova, M.; Smetana, K.; Lacina, L. Skin aging: The dermal perspective. Clin. Dermatol 2019, 37, 326–335. [Google Scholar] [CrossRef]
- Felgueiras, H.P.; Teixeira, M.A.; Tavares, T.D.; Homem, N.C.; Zille, A.; Amorim, M.T.P. Antimicrobial action and clotting time of thin, hydrated poly (vinyl alcohol)/cellulose acetate films functionalized with LL37 for prospective wound-healing applications. J. Appl. Polym. Sci. 2020, 137, 48626. [Google Scholar] [CrossRef]
- Graham, H.K.; Eckersley, A.; Ozols, M.; Mellody, K.T.; Sherratt, M.J. Human Skin: Composition, Structure and Visualisation Methods. In Skin Biophysics; Springer: Berlin/Heidelberg, Germany, 2019; pp. 1–18. [Google Scholar]
- Zhang, L.-j.; Guerrero-Juarez, C.F.; Hata, T.; Bapat, S.P.; Ramos, R.; Plikus, M.V.; Gallo, R.L. Dermal adipocytes protect against invasive Staphylococcus aureus skin infection. Science 2015, 347, 67–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tavares, T.D.; Antunes, J.C.; Padrão, J.; Ribeiro, A.I.; Zille, A.; Amorim, M.T.P.; Ferreira, F.; Felgueiras, H.P. Activity of specialized biomolecules against Gram-positive and Gram-negative bacteria. Antibiotics 2020, 9, 314. [Google Scholar] [CrossRef] [PubMed]
- Hutchings, M.I.; Truman, A.W.; Wilkinson, B. Antibiotics: Past, present and future. Curr. Opin. Microbiol. 2019, 51, 72–80. [Google Scholar] [CrossRef]
- Baquero, F.; Levin, B.R. Proximate and ultimate causes of the bactericidal action of antibiotics. Nat. Rev. Microbiol. 2020, 19, 123–132. [Google Scholar] [CrossRef]
- Douafer, H.; Andrieu, V.; Phanstiel IV, O.; Brunel, J.M. Antibiotic adjuvants: Make antibiotics great again! J. Med. Chem. 2019, 62, 8665–8681. [Google Scholar] [CrossRef]
- Bahar, A.A.; Ren, D. Antimicrobial peptides. Pharmaceuticals 2013, 6, 1543–1575. [Google Scholar] [CrossRef] [Green Version]
- Lei, J.; Sun, L.; Huang, S.; Zhu, C.; Li, P.; He, J.; Mackey, V.; Coy, D.H.; He, Q. The antimicrobial peptides and their potential clinical applications. Am. J. Transl. Res. 2019, 11, 3919. [Google Scholar] [PubMed]
- Homem, N.C.; Tavares, T.D.; Miranda, C.S.; Antunes, J.C.; Amorim, M.T.P.; Felgueiras, H.P. Functionalization of Crosslinked Sodium Alginate/Gelatin Wet-Spun Porous Fibers with Nisin Z for the Inhibition of Staphylococcus aureus-Induced Infections. Int. J. Mol. Sci. 2021, 22, 1930. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Kizhakkedathu, J.N.; Straus, S.K. Antimicrobial peptides: Diversity, mechanism of action and strategies to improve the activity and biocompatibility in vivo. Biomolecules 2018, 8, 4. [Google Scholar] [CrossRef] [Green Version]
- Magana, M.; Pushpanathan, M.; Santos, A.L.; Leanse, L.; Fernandez, M.; Ioannidis, A.; Giulianotti, M.A.; Apidianakis, Y.; Bradfute, S.; Ferguson, A.L. The value of antimicrobial peptides in the age of resistance. Lancet Infect. Dis 2020. [Google Scholar] [CrossRef]
- Caesar, L.K.; Cech, N.B. Synergy and antagonism in natural product extracts: When 1+ 1 does not equal 2. Nat. Prod. Rep. 2019, 36, 869–888. [Google Scholar] [CrossRef] [Green Version]
- Pavithra, P.; Mehta, A.; Verma, R.S. Essential oils: From prevention to treatment of skin cancer. Drug Discov. Today 2019, 24, 644–655. [Google Scholar] [CrossRef]
- Eljounaidi, K.; Lichman, B.R. Nature’s chemists: The discovery and engineering of phytochemical biosynthesis. Front. Chem. 2020, 8, 1041. [Google Scholar] [CrossRef]
- Laube, S. Skin infections and ageing. Ageing Res. Rev. 2004, 3, 69–89. [Google Scholar] [CrossRef] [PubMed]
- Leung, D.Y.; Boguniewicz, M.; Howell, M.D.; Nomura, I.; Hamid, Q.A. New insights into atopic dermatitis. J. Clin. Investig. 2004, 113, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Renert-Yuval, Y.; Guttman-Yassky, E. What’s new in atopic dermatitis. Dermatol. Clin. 2019, 37, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Lepoittevin, J.-P.; Lafforgue, C. Molecular aspects in allergic and irritant contact dermatitis. Contact. Derm. 2020, 1–18. [Google Scholar] [CrossRef]
- Boguniewicz, M. Biologics for atopic dermatitis. Immunol. Allergy Clin. 2020, 40, 593–607. [Google Scholar] [CrossRef] [PubMed]
- Seiti Yamada Yoshikawa, F.; Feitosa de Lima, J.; Notomi Sato, M.; Álefe Leuzzi Ramos, Y.; Aoki, V.; Leao Orfali, R. Exploring the role of Staphylococcus aureus toxins in atopic dermatitis. Toxins 2019, 11, 321. [Google Scholar] [CrossRef] [Green Version]
- Petry, V.; Bessa, G.R.; Poziomczyck, C.S.; Oliveira, C.F.D.; Weber, M.B.; Bonamigo, R.R.; d’Azevedo, P.A. Bacterial skin colonization and infections in patients with atopic dermatitis. An. Bras. Dermatol. 2012, 87, 729–734. [Google Scholar] [CrossRef] [Green Version]
- Montes-Torres, A.; Llamas-Velasco, M.; Pérez-Plaza, A.; Solano-López, G.; Sánchez-Pérez, J. Biological treatments in atopic dermatitis. J. Clin. Med. 2015, 4, 593–613. [Google Scholar] [CrossRef]
- Kim, J.; seok Lee, I.; Park, S.; Choue, R. Effects of Scutellariae radix and Aloe vera gel extracts on immunoglobulin E and cytokine levels in atopic dermatitis NC/Nga mice. J. Ethnopharmacol. 2010, 132, 529–532. [Google Scholar] [CrossRef]
- Antley, C.M.; Anderson, R.; Margulies, J. Cannabis in Dermatology. In Cannabis Medicine; Springer: Berlin/Heidelberg, Germany, 2020; pp. 383–400. [Google Scholar]
- Ferreira, E.B.; Ciol, M.A.; de Meneses, A.G.; Bontempo, P.d.S.; Hoffman, J.M.; Reis, P.E.D. Chamomile Gel versus Urea Cream to Prevent Acute Radiation Dermatitis in Head and Neck Cancer Patients: Results from a Preliminary Clinical Trial. Integr. Cancer Ther. 2020, 19, 1534735420962174. [Google Scholar] [CrossRef] [PubMed]
- Takahagi, S.; Harada, N.; Kamegashira, A.; Suzuki, S.; Shindo, H.; Kanatani, H.; Tanaka, A.; Mizuno, H.; Hide, M. Randomized double-blind cross-over trial of bath additive containing tannic acid in patients with atopic dermatitis. J. Cutan. Immunol. Allergy 2020, 3, 56–61. [Google Scholar] [CrossRef]
- Nguyen, H.L.T.; Trujillo-Paez, J.V.; Umehara, Y.; Yue, H.; Peng, G.; Kiatsurayanon, C.; Chieosilapatham, P.; Song, P.; Okumura, K.; Ogawa, H. Role of antimicrobial peptides in skin barrier repair in individuals with atopic dermatitis. Int. J. Mol. Sci. 2020, 21, 7607. [Google Scholar] [CrossRef]
- Smits, J.P.H.; Ederveen, T.H.A.; Rikken, G.; van den Brink, N.J.M.; van Vlijmen-Willems, I.M.J.J.; Boekhorst, J.; Kamsteeg, M.; Schalkwijk, J.; van Hijum, S.A.F.T.; Zeeuwen, P.L.J.M.; et al. Targeting the Cutaneous Microbiota in Atopic Dermatitis by Coal Tar via AHR-Dependent Induction of Antimicrobial Peptides. J. Investig. Dermatol. 2020, 140, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Benhadou, F.; Mintoff, D.; del Marmol, V. Psoriasis: Keratinocytes or immune cells—Which is the trigger? Dermatolog 2019, 235, 91–100. [Google Scholar] [CrossRef]
- Griffiths, C.E.M.; van der Walt, J.M.; Ashcroft, D.M.; Flohr, C.; Naldi, L.; Nijsten, T.; Augustin, M. The global state of psoriasis disease epidemiology: A workshop report. Br. J. Dermatol. 2017, 177, e4–e7. [Google Scholar] [CrossRef]
- Rapalli, V.K.; Waghule, T.; Gorantla, S.; Dubey, S.K.; Saha, R.N.; Singhvi, G. Psoriasis: Pathological mechanisms, current pharmacological therapies, and emerging drug delivery systems. Drug Discov. Today 2020. [Google Scholar] [CrossRef]
- Rendon, A.; Schäkel, K. Psoriasis pathogenesis and treatment. Int. J. Mol. Sci. 2019, 20, 1475. [Google Scholar] [CrossRef] [Green Version]
- Fry, L.; Baker, B.S. Triggering psoriasis: The role of infections and medications. Clin. Dermatol. 2007, 25, 606–615. [Google Scholar] [CrossRef] [PubMed]
- Groot, J.; Blegvad, C.; Nybo Andersen, A.M.; Zachariae, C.; Jarløv, J.; Skov, L. Presence of streptococci and frequent tonsillitis among adolescents with psoriasis. Br. J. Dermatol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Oenarta, D.G.; Budayanti, N.S.; Fatmawati, N.D.; Tarini, N.A. Staphylococcus aureus colonization on an erythrodermic psoriasis patient. J. Widya Med. 2019, 5, 132–140. [Google Scholar] [CrossRef]
- Lewis, D.J.; Chan, W.H.; Hinojosa, T.; Hsu, S.; Feldman, S.R. Mechanisms of microbial pathogenesis and the role of the skin microbiome in psoriasis: A review. Clin. Dermatol. 2019, 37, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Kleyn, E.C.; Morsman, E.; Griffin, L.; Wu, J.J.; Cm van de Kerkhof, P.; Gulliver, W.; van der Walt, J.M.; Iversen, L. Review of international psoriasis guidelines for the treatment of psoriasis: Recommendations for topical corticosteroid treatments. J. Dermatol. Treat. 2019, 30, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.-C.; Tsai, T.-F. A review of antibiotics and psoriasis: Induction, exacerbation, and amelioration. Expert Rev. Clin. Pharmacol. 2019, 12, 981–989. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.B.; Amin, M.; Bhutani, T.; Wu, J.J. Emerging therapies in psoriasis: A systematic review. Cutis 2018, 101, 5–9. [Google Scholar]
- Campione, E.; Cosio, T.; Lanna, C.; Mazzilli, S.; Ventura, A.; Dika, E.; Gaziano, R.; Dattola, A.; Candi, E.; Bianchi, L. Predictive role of vitamin A serum concentration in psoriatic patients treated with IL-17 inhibitors to prevent skin and systemic fungal infections. J. Pharmacol. Sci. 2020, 144, 52–56. [Google Scholar] [CrossRef]
- Sukare, P.; Bhattacharya, R. Herbal plant used in treatment of psoriasis—A systematic review. Res. J. Pharmacogn. Phytochem. 2020, 12, 57–62. [Google Scholar] [CrossRef]
- Algahtani, M.S.; Ahmad, M.Z.; Ahmad, J. Nanoemulsion loaded polymeric hydrogel for topical delivery of curcumin in psoriasis. J. Drug Deliv. Sci. Technol. 2020, 59, 101847. [Google Scholar] [CrossRef]
- Ramanunny, A.K.; Wadhwa, S.; Singh, S.K.; Sharma, D.S.; Khursheed, R.; Awasthi, A. Treatment strategies against psoriasis: Principle, perspectives and practices. Curr. Drug Deliv. 2020, 17, 52–73. [Google Scholar] [CrossRef] [PubMed]
- Steiner, I.; Kennedy, P.G.E.; Pachner, A.R. The neurotropic herpes viruses: Herpes simplex and varicella-zoster. Lancet Neurol. 2007, 6, 1015–1028. [Google Scholar] [CrossRef]
- Jevšnik, M.; Lusa, L.; Uršič, T.; Biškup, U.G.; Petrovec, M. Detection of herpes simplex and varicella-zoster virus from skin lesions: Comparison of RT-PCR and isothermal amplification for rapid identification. Diagn. Microbiol. Infect. Dis. 2020, 115015. [Google Scholar] [CrossRef]
- Vanti, G.; Dourdouni, V.; Lazari, D.; Panagiotidis, C.; Ntallis, S.; Litsiou, S.; Patsoura, C.; Piazzini, V.; Risaliti, L.; Bergonzi, M. Melissa officinalis essential oil loaded glycerosomes: Preparation and in vitro activity evaluation against herpes labialis (HSV-1). Planta Med. 2019, 85, SL-YRW. [Google Scholar]
- Yang, Q.; George, M.G.; Chang, A.; Tong, X.; Merritt, R.; Hong, Y. Effect of herpes zoster vaccine and antiviral treatment on risk of ischemic stroke. Neurology 2020, 95, e708–e717. [Google Scholar] [CrossRef] [PubMed]
- Fatima, G.; Jabeen, A.; Siddiqui, S.A.; Khalid, M. A review on Glycyrrhiza glabra L.(Aṣl al-Sūs) with unani perspective and modern pharmacology. J. Drug Deliv. Ther. 2019, 9, 736–741. [Google Scholar] [CrossRef]
- Shenefelt, P.D. Herbal Treatment for Dermatologic Disorders. In Herbal Medicine: Biomolecular and Clinical Aspects, 2nd ed.; Benzie, I., Wachtel-Galor, S., Eds.; Taylor and Francis Group, LLC.: Boca Raton, FL, USA, 2011; p. 383. [Google Scholar]
- Ogé, L.K.; Broussard, A.; Marshall, M.D. Acne vulgaris: Diagnosis and treatment. Am. Fam. Physician 2019, 100, 475–484. [Google Scholar] [PubMed]
- Ak, M. A comprehensive review of acne vulgaris. J. Clin. Pharm. 2019, 1, 17–45. [Google Scholar]
- Chomnawang, M.T.; Surassmo, S.; Nukoolkarn, V.S.; Gritsanapan, W. Antimicrobial effects of Thai medicinal plants against acne-inducing bacteria. J. Ethnopharmacol. 2005, 101, 330–333. [Google Scholar] [CrossRef]
- Whitehouse, H.; Solman, L.; Eady, E.; Layton, A. Oral antibiotics in acne: A retrospective single-centre analysis of current prescribing in primary care and its alignment with the national antibiotic quality premium. Br. J. Dermatol. 2019, 181, 1341–1342. [Google Scholar] [CrossRef]
- Bek-Thomsen, M.; Lomholt, H.B.; Kilian, M. Acne is not associated with yet-uncultured bacteria. J. Clin. Microbiol. 2008, 46, 3355–3360. [Google Scholar] [CrossRef] [Green Version]
- McInturff, J.E.; Wang, S.-J.; Machleidt, T.; Richard Lin, T.; Oren, A.; Hertz, C.J.; Krutzik, S.R.; Hart, S.; Zeh, K.; Anderson, D.H.; et al. Granulysin-derived peptides demonstrate antimicrobial and anti-inflammatory effects against Propionibacterium acnes. J. Investig. Dermatol. 2005, 125, 256–263. [Google Scholar] [CrossRef] [Green Version]
- Ryu, S.; Han, H.M.; Song, P.I.; Armstrong, C.A.; Park, Y. Suppression of Propionibacterium acnes infection and the associated inflammatory response by the antimicrobial peptide P5 in mice. PLoS ONE 2015, 10, e0132619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, W.-R.; Kim, K.-H.; An, H.-J.; Kim, J.-y.; Chang, Y.-C.; Chung, H.; Park, Y.-Y.; Lee, M.-L.; Park, K.-k. The protective effects of Melittin on Propionibacterium acnes–induced inflammatory responses in vitro and in vivo. J. Investig. Dermatol. 2014, 134, 1922–1930. [Google Scholar] [CrossRef] [Green Version]
- Woodburn, K.W.; Jaynes, J.; Clemens, L.E. Designed antimicrobial peptides for topical treatment of antibiotic resistant Acne vulgaris. Antibiotics 2020, 9, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vora, J.; Srivastava, A.; Modi, H. Antibacterial and antioxidant strategies for acne treatment through plant extracts. Inform. Med. Unlocked 2019, 16, 100229. [Google Scholar] [CrossRef]
- Fabbrocini, G.; Staibano, S.; De Rosa, G.; Battimiello, V.; Fardella, N.; Ilardi, G.; La Rotonda, M.I.; Longobardi, A.; Mazzella, M.; Siano, M.; et al. Resveratrol-Containing Gel for the Treatment of Acne Vulgaris. Am. J. Clin. Dermatol. 2011, 12, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Gervason, S.; Metton, I.; Gemrot, E.; Ranouille, E.; Skorski, G.; Cabannes, M.; Berthon, J.-Y.; Filaire, E. Rhodomyrtus tomentosa fruit extract and skin microbiota: A focus on C. acnes phylotypes in acne subjects. Cosmetics 2020, 7, 53. [Google Scholar] [CrossRef]
- Esmael, A.; Hassan, M.G.; Amer, M.M.; Abdelrahman, S.; Hamed, A.M.; Abd-raboh, H.A.; Foda, M.F. Antimicrobial activity of certain natural-based plant oils against the antibiotic-resistant acne bacteria. Saudi J. Biol. Sci. 2020, 27, 448–455. [Google Scholar] [CrossRef] [PubMed]
- Bunrathep, S.; Thongphasuk, P.; Settharaksa, S.; Kamkaen, N. Effect of an essential oil blend of citronella, lemongrass, and patchouli on acne-causing bacteria. Songklanakarin J. Sci. Technol. 2020, 42, 1106–1112. [Google Scholar]
- Woo, T.E.; Somayaji, R.; Haber, R.; Parsons, L. Diagnosis and management of cutaneous tinea infections. Adv. Skin Wound Care 2019, 32, 350–357. [Google Scholar] [CrossRef]
- Leung, A.K.; Lam, J.M.; Leong, K.F.; Hon, K.L. Tinea corporis: An updated review. Drugs Context 2020, 9. [Google Scholar] [CrossRef] [PubMed]
- Mercer, D.K.; Stewart, C.S. Keratin hydrolysis by dermatophytes. Med. Mycol. 2019, 57, 13–22. [Google Scholar] [CrossRef]
- Shah, B.; Shah, S.; Jangid, N.; Dhoot, D.; Deshmukh, G.; Barkate, H. Comparative evaluation of efficacy and safety of terbinafine and itraconazole in the management of tinea corporis et cruris. IP Indian J. Clin. Exp. Dermatol. 2020, 6, 231–236. [Google Scholar]
- Fritz, P.; Beck-Jendroschek, V.; Brasch, J. Inhibition of dermatophytes by the antimicrobial peptides human β-defensin-2, ribonuclease 7 and psoriasin. Med. Mycol. 2012, 50, 579–584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lima, P.G.; Souza, P.F.N.; Freitas, C.D.T.; Bezerra, L.P.; Neto, N.A.S.; Silva, A.F.B.; Oliveira, J.T.A.; Sousa, D.O.B. Synthetic peptides against Trichophyton mentagrophytes and T. rubrum: Mechanisms of action and efficiency compared to griseofulvin and itraconazole. Life Sci. 2020, 118803. [Google Scholar] [CrossRef]
- Parrish, N.; Fisher, S.L.; Gartling, A.; Craig, D.; Boire, N.; Khuvis, J.; Riedel, S.; Zhang, S. Activity of various essential oils against clinical dermatophytes of Microsporum and Trichophyton. Front. Cell Infect. Microbiol. 2020, 10. [Google Scholar] [CrossRef]
- Wong, J.H.; Lau, K.-M.; Wu, Y.-O.; Cheng, L.; Wong, C.-W.; Yew, D.T.-W.; Leung, P.-C.; Fung, K.-P.; Hui, M.; Ng, T.-B. Antifungal mode of action of macrocarpal C extracted from Eucalyptus globulus Labill (Lan An) towards the dermatophyte Trichophyton mentagrophytes. Chin. Med. 2015, 10, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Kakande, T.; Batunge, Y.; Eilu, E.; Shabohurira, A.; Abimana, J.; Akinola, S.A.; Muhwezi, R.; Sunusi Adam, A.; Kemuma Onkoba, S.; Almustapha Aliero, A.; et al. Prevalence of dermatophytosis and antifungal activity of ethanolic crude leaf extract of Tetradenia riparia against dermatophytes isolated from patients attending Kampala International University Teaching Hospital, Uganda. Dermatol. Res. Pract. 2019, 2019, 9328621. [Google Scholar] [CrossRef] [Green Version]
- Mohammad Al-Edani, A.J.; Hussein, S.F.; Al-khafaji, B.A.H. Evaluation of the activity of alcoholic extract of Gujarat plant(Hibiscussabdariffa L.) against some dermatophytes. IOP Conf. Ser. Mater. Sci. Eng. 2020, 928, 062009. [Google Scholar] [CrossRef]
- Abazari, M.; Ghaffari, A.; Rashidzadeh, H.; Momeni badeleh, S.; Maleki, Y. Current status and future outlook of nano-based systems for burn wound management. J. Biomed. Mater. Res. B Appl. Biomater. 2020, 108, 1934–1952. [Google Scholar] [CrossRef]
- Havlikova, J.; May, R.C.; Styles, I.B.; Cooper, H.J. Direct identification of bacterial and human proteins from infected wounds in living 3D skin models. Sci. Rep. 2020, 10, 1–9. [Google Scholar] [CrossRef]
- Pfalzgraff, A.; Brandenburg, K.; Weindl, G. Antimicrobial peptides and their therapeutic potential for bacterial skin infections and wounds. Front. Pharmacol. 2018, 9. [Google Scholar] [CrossRef]
- Gestano, R.; Parlianta, I. Effectiveness of Nano Silver Sulfadiazine and Silver Sulfadiazine on the Growth of Germ Colonies in Deep Dermal Burns. Sriwijaya J. Surg. 2019, 2, 30–40. [Google Scholar] [CrossRef]
- Rutthapol, S.; Charisopon, C.; Sukanjana, K.; Wilaiporn, B.; Janwit, D.; Tan, S.; Somchai, S.; Jongdee, N.; Teerapol, S. The safety and efficacy of Mupirocin topical spray for burn wound healing in a rat model. Int. J. Pharm. Qual. Assur. 2019, 10, 51–59. [Google Scholar] [CrossRef]
- Nethery, W.A.; Warner, P.; Durkee, P.J.; Zembrodt, J.; Dwyer, A.; Fowler, L. Efficacy of topical antimicrobial agents against bacterial isolates from burn wounds. J. Burn Care Res. 2020, 41, S60. [Google Scholar] [CrossRef]
- Jacobsen, F.; Mohammadi-Tabrisi, A.; Hirsch, T.; Mittler, D.; Mygind, P.; Sonksen, C.; Raventos, D.; Kristensen, H.; Gatermann, S.; Lehnhardt, M. Antimicrobial activity of the recombinant designer host defence peptide P-novispirin G10 in infected full-thickness wounds of porcine skin. J. Antimicrob. Chemother. 2007, 59, 493–498. [Google Scholar] [CrossRef] [Green Version]
- Björn, C.; Noppa, L.; Salomonsson, E.N.; Johansson, A.-L.; Nilsson, E.; Mahlapuu, M.; Håkansson, J. Efficacy and safety profile of the novel antimicrobial peptide PXL150 in a mouse model of infected burn wounds. Int. J. Antimicrob. Agents 2015, 45, 519–524. [Google Scholar] [CrossRef]
- Gomes, D.; Santos, R.; Soares, R.; Reis, S.; Carvalho, S.; Rego, P.; Peleteiro, M.; Tavares, L.; Oliveira, M. Pexiganan in combination with nisin to control polymicrobial diabetic foot infections. Antibiotics 2020, 9, 128. [Google Scholar] [CrossRef] [Green Version]
- Teixeira, M.O.; Antunes, J.C.; Felgueiras, H.P. Recent Advances in Fiber–Hydrogel Composites for Wound Healing and Drug Delivery Systems. Antibiotics 2021, 10, 248. [Google Scholar] [CrossRef]
- Liang, J.; Cui, L.; Li, J.; Guan, S.; Zhang, K.; Li, J. Aloe vera: A medicinal plant used in skin wound healing. Tissue Eng. Part B Rev. 2020. [Google Scholar] [CrossRef]
- Huang, X.; Sun, J.; Chen, G.; Niu, C.; Wang, Y.; Zhao, C.; Sun, J.; Huang, H.; Huang, S.; Liang, Y. Resveratrol promotes diabetic wound healing via SIRT1-FOXO1-c-Myc signaling pathway-mediated angiogenesis. Front. Pharmacol. 2019, 10, 421. [Google Scholar] [CrossRef] [Green Version]
- García-Salinas, S.; Evangelopoulos, M.; Gámez-Herrera, E.; Arruebo, M.; Irusta, S.; Taraballi, F.; Mendoza, G.; Tasciotti, E. Electrospun anti-inflammatory patch loaded with essential oils for wound healing. Int. J. Pharm. 2020, 577, 119067. [Google Scholar] [CrossRef] [PubMed]
- Antunes, J.C.; Tavares, T.D.; Teixeira, M.A.; Teixeira, M.O.; Homem, N.C.; Amorim, M.T.P.; Felgueiras, H.P. Eugenol-containing essential oils loaded onto Chitosan/Polyvinyl alcohol blended films and their ability to eradicate Staphylococcus aureus or Pseudomonas aeruginosa from infected microenvironments. Pharmaceutics 2021, 13, 195. [Google Scholar] [CrossRef] [PubMed]
- Ghodrati, M.; Farahpour, M.R.; Hamishehkar, H. Encapsulation of Peppermint essential oil in nanostructured lipid carriers: In-vitro antibacterial activity and accelerative effect on infected wound healing. Colloids Surf. A 2019, 564, 161–169. [Google Scholar] [CrossRef]
- Felgueiras, H.P.; Homem, N.C.; Teixeira, M.A.; Ribeiro, A.R.; Antunes, J.C.; Amorim, M.T.P. Physical, thermal, and antibacterial effects of active essential oils with potential for biomedical applications loaded onto cellulose acetate/polycaprolactone wet-spun microfibers. Biomolecules 2020, 10, 1129. [Google Scholar] [CrossRef]



| Antibiotic | Bacterial Target | Mechanism | Effect on Psoriasis |
|---|---|---|---|
| Amoxicillin | G(+): streptococci, staphylococci, Enterococcus faecalis. G(−): Escherichia coli, Helicobacter pylori, etc. | Release of pro-inflammatory cytokines by macrophages. | Induces generalized pustular psoriasis. |
| Vancomycin | G(+): enterococci, streptococci, S. aureus (MRSA), S. epidermidis. | Dysregulates gut and skin microbiota; activation of T cells. | Increases the susceptibility of plaque psoriasis. |
| Erythromycin | G(+): streptococci, Corynebacterium spp., S. aureus, etc. G(−): Legionella pneumophila, Neisseria gonorrhoeae, Chlamydia trachomatis, etc. | Reduces neutrophil activity; inhibits the action of the cytokines TNFα, IL-6, and IL-8. | Improves plaque psoriasis. |
| Azithromycin | G(+): streptococci, S. aureus. G(−): N. gonorrhoeae, Haemophilus spp., Moraxella catarrhalis, etc. | Restores keratinocyte differentiation and decreases hyper-proliferation; reduces cytokines’ action. | Improves plaque psoriasis. |
| Tetracyclines | G(+): streptococci, S. aureus, Listeria monocytogenes, Bacillus anthracis, etc. G(−): bacilli spp. | Increases the photosensitivity of the skin; influences the arachidonic acid system. | Exacerbates or induces plaque psoriasis. |
| Rifampin | G(+): S. aureus (MRSA), S. epidermidis. G(−): Haemophilus influenza, Neisseria meningitidis. | Supresses T-lymphocytes; inhibits TNFα; increases secretion of IL-6 and IL-10. | Improves plaque psoriasis. |
| Abbreviations: G(+)—Gram-positive; G(−)—Gram-negative; MRSA—methicillin-resistant S. aureus. | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Felgueiras, H.P. An Insight into Biomolecules for the Treatment of Skin Infectious Diseases. Pharmaceutics 2021, 13, 1012. https://doi.org/10.3390/pharmaceutics13071012
Felgueiras HP. An Insight into Biomolecules for the Treatment of Skin Infectious Diseases. Pharmaceutics. 2021; 13(7):1012. https://doi.org/10.3390/pharmaceutics13071012
Chicago/Turabian StyleFelgueiras, Helena P. 2021. "An Insight into Biomolecules for the Treatment of Skin Infectious Diseases" Pharmaceutics 13, no. 7: 1012. https://doi.org/10.3390/pharmaceutics13071012
APA StyleFelgueiras, H. P. (2021). An Insight into Biomolecules for the Treatment of Skin Infectious Diseases. Pharmaceutics, 13(7), 1012. https://doi.org/10.3390/pharmaceutics13071012