In Vitro Effect of Photodynamic Therapy with Different Lights and Combined or Uncombined with Chlorhexidine on Candida spp.
Abstract
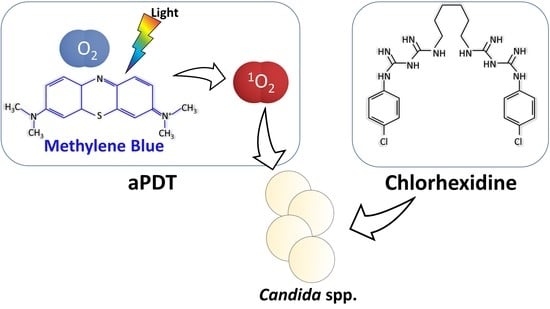
:1. Introduction
2. Materials and Methods
2.1. Chemicals, Media, Strains and Light Sources
- -
- Solvent: Distilled water.
- -
- Culture Media: Sabouraud dextrose agar (CM0041 Oxoid®, Thermo Scientific, Waltham, MA, USA) and Columbia blood agar BA (Oxoid®; Madrid, Spain).
- -
- Antiseptic: Chlorhexidine (CHX) (CN162301.0, Miclorbic®, Madrid, Spain). Stock CHX solution was diluted in distilled water. CHX was applied at a concentration of 10 μg/mL.
- -
- Photosensitizer: Methylene blue (MB), (Sigma-Aldrich®; Madrid, Spain). Stock MB solution was diluted in distilled water. All solutions were prepared no more than a week prior to use and handled under light-restricted conditions. The concentration ranges from 640 to 0.03 μg/mL were used.
- -
- Strains: C. albicans, C. parapsilosis and C. krusei were acquired from the American Type Culture Collection (ATCC, Rockville, MD, USA). C. albicans ATCC 10231, C. parapsilosis ATCC 22019 and C. krusei ATCC 6258 were used.
- -
- Light sources: Light-emitting diode (LED) lamp, Showtec LED Par 64 Short 18 × RGB 3-in-1 LED, Highlite International, emitting at 625 ± 10 nm (power density 7 mW/cm2 at a distance between the LEDs and the microtiter plate with the microbial suspension of 17 cm where the diameter of the light beam is approximately 25 cm) and white metal halide lamp (WMH), made by the Department of Applied Physics of the University of Zaragoza, Spain, emitting at 420–700 nm (power density 90 mW/cm2 at a distance between the lamp and the 96-well microtiter plate of 10 cm where the diameter of the light beam is approximately 21 cm). Supplementary Figure S1 shows the lamps and their emission spectrums. Both were used at a fluence of 18 J/cm2. This fluence corresponds to a 42.86 min (≈43 min) irradiation time for the samples using the red-LED lamp and 3 min and 25 sec for the samples irradiated with WMH lamp.
2.2. In Vitro Photodynamic Treatment of Yeast Suspension
2.3. Efficacy
3. Results
3.1. Photoinactivation of Yeasts by MB-aPDT (MB+/CHX−/Light+)
3.2. Fungicidal Effect of MB-aPDT Combined with CHX (MB+/CHX+/Light+)
3.3. Control of Inoculum and Toxic Effects of MB (MB+/CHX−/Light−), CHX (MB−/CHX+/Light−) and Irradiation (MB−/CHX−/Light+)
4. Discussion
5. Conclusions
- -
- MB-aPDT is active against Candida spp. in water suspension.
- -
- CHX enhances the photoinactivation of Candida spp. (aPDT plus CHX increases the photoactivity of MB).
- -
- White light is a suitable light source for aPDT.
- -
- MB-aPDT using a broad-spectrum white light is more efficient than a specific red-LED lamp.
- -
- Transfer of this therapy to the clinic could be very convenient.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rex, J.H.; Walsh, T.J.; Sobel, J.D.; Filler, S.G.; Pappas, P.G.; Dismukes, W.E.; Edwards, J.E. Practice Guidelines for the Treatment of Candidiasis. Clin. Infect. Dis. 2000, 30, 662–678. [Google Scholar] [CrossRef] [PubMed]
- Lalla, R.; Patton, L.; Dongari-Bagtzoglou, A. Oral Candidiasis: Pathogenesis, Clinical Presentation, Diagnosis and Treatment Strategies. J. Calif. Dent. Assoc. 2013, 41, 263–268. [Google Scholar]
- Moran, G.; Coleman, D.; Sullivan, D. An Introduction to the Medically Important Candida Species. In Candida and Candidiasis, 2nd ed.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2011; pp. 9–25. [Google Scholar] [CrossRef]
- Kashem, S.W.; Kaplan, D.H. Skin Immunity to Candida Albicans. Trends Immunol. 2016, 37, 440–450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gavara, R.; de Llanos, R.; Pérez-Laguna, V.; Arnau del Valle, C.; Miravet, J.F.; Rezusta, A.; Galindo, F. Broad-Spectrum Photo-Antimicrobial Polymers Based on Cationic Polystyrene and Rose Bengal. Front. Med. 2021, 8. [Google Scholar] [CrossRef]
- Perez-Laguna, V.; Garcia-Malinis, A.J.; Aspiroz, C.; Rezusta, A.; Gilaberte, Y. Antimicrobial Effects of Photodynamic Therapy: An Overview. G. Ital. Dermatol. Venereol. Organo Uff. Soc. Ital. Dermatol. Sifilogr. 2018, 153, 833–846. [Google Scholar] [CrossRef]
- Rezusta, A.; López-Chicón, P.; Paz-Cristobal, M.P.; Alemany-Ribes, M.; Royo-Díez, D.; Agut, M.; Semino, C.; Nonell, S.; Revillo, M.J.; Aspiroz, C.; et al. In Vitro Fungicidal Photodynamic Effect of Hypericin on Candida Species. Photochem. Photobiol. 2012, 88, 613–619. [Google Scholar] [CrossRef]
- Kashef, N.; Esmaeeli Djavid, G.; Siroosy, M.; Taghi Khani, A.; Hesami Zokai, F.; Fateh, M. Photodynamic Inactivation of Drug-Resistant Bacteria Isolated from Diabetic Foot Ulcers. Iran. J. Microbiol. 2011, 3, 36–41. [Google Scholar] [PubMed]
- Pérez-Laguna, V.; Rezusta, A.; Ramos, J.J.; Ferrer, L.M.; Gené, J.; Revillo, M.J.; Gilaberte, Y. Daylight Photodynamic Therapy Using Methylene Blue to Treat Sheep with Dermatophytosis Caused by Arthroderma vanbreuseghemii. Small Rumin. Res. 2017, 150, 97–101. [Google Scholar] [CrossRef] [Green Version]
- Paz-Cristobal, M.P.; Royo, D.; Rezusta, A.; Andrés-Ciriano, E.; Alejandre, M.C.; Meis, J.F.; Revillo, M.J.; Aspiroz, C.; Nonell, S.; Gilaberte, Y. Photodynamic Fungicidal Efficacy of Hypericin and Dimethyl Methylene Blue against Azole-Resistant Candida albicans Strains. Mycoses 2014, 57, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, C.F.; Rodrigues, M.E.; Henriques, M.C.R. Promising Alternative Therapeutics for Oral Candidiasis. Curr. Med. Chem. 2019, 26, 2515–2528. [Google Scholar] [CrossRef] [PubMed]
- Soria-Lozano, P.; Gilaberte, Y.; Paz-Cristobal, M.; Pérez-Artiaga, L.; Lampaya-Pérez, V.; Aporta, J.; Pérez-Laguna, V.; García-Luque, I.; Revillo, M.; Rezusta, A. In Vitro Effect Photodynamic Therapy with Differents Photosensitizers on Cariogenic Microorganisms. BMC Microbiol. 2015, 15, 187. [Google Scholar] [CrossRef] [Green Version]
- Valkov, A.; Zinigrad, M.; Nisnevitch, M. Photodynamic Eradication of Trichophyton Rubrum and Candida albicans. Pathogens 2021, 10, 263. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Laguna, V.; García-Luque, I.; Ballesta, S.; Rezusta, A.; Gilaberte, Y. Photodynamic Therapy Combined with Antibiotics or Antifungals against Microorganisms That Cause Skin and Soft Tissue Infections: A Planktonic and Biofilm Approach to Overcome Resistances. Pharmaceuticals 2021, 14, 603. [Google Scholar] [CrossRef]
- Pérez-Laguna, V.; Gilaberte, Y.; Millán-Lou, M.I.; Agut, M.; Nonell, S.; Rezusta, A.; Hamblin, M.R. A Combination of Photodynamic Therapy and Antimicrobial Compounds to Treat Skin and Mucosal Infections: A Systematic Review. Photochem. Photobiol. Sci. 2019, 18, 1020–1029. [Google Scholar] [CrossRef]
- Wozniak, A.; Grinholc, M. Combined Antimicrobial Activity of Photodynamic Inactivation and Antimicrobials-State of the Art. Front. Microbiol. 2018, 9, 930. [Google Scholar] [CrossRef] [PubMed]
- Martin, V.T.; Abdullahi Abdi, M.; Li, J.; Li, D.; Wang, Z.; Zhang, X.; Elodie, W.H.; Yu, B. Preoperative Intranasal Decolonization with Topical Povidone-Iodine Antiseptic and the Incidence of Surgical Site Infection: A Review. Med. Sci. Monit. 2020, 26, e927052. [Google Scholar] [CrossRef]
- Millán-Lou, M.I.; López, C.; Bueno, J.; Pérez-Laguna, V.; Lapresta, C.; Fuertes, M.E.; Rite, S.; Santiago, M.; Romo, M.; Samper, S.; et al. Successful Control of Serratia Marcescens Outbreak in a Neonatal Unit of a Tertiary-Care Hospital in Spain. Enferm. Infecc. Microbiol. Clínica 2021. [Google Scholar] [CrossRef] [PubMed]
- Napolitani, M.; Bezzini, D.; Moirano, F.; Bedogni, C.; Messina, G. Methods of Disinfecting Stethoscopes: Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 1856. [Google Scholar] [CrossRef] [Green Version]
- Yamashita, T.; Takamori, A.; Nakagawachi, A.; Tanigawa, Y.; Hamada, Y.; Aoki, Y.; Sakaguchi, Y. Early Prophylaxis of Central Venous Catheter-Related Thrombosis Using 1% Chlorhexidine Gluconate and Chlorhexidine-Gel-Impregnated Dressings: A Retrospective Cohort Study. Sci. Rep. 2020, 10, 15952. [Google Scholar] [CrossRef] [PubMed]
- Ellepola, A.N.; Samaranayake, L.P. Adjunctive Use of Chlorhexidine in Oral Candidoses: A Review. Oral Dis. 2001, 7, 11–17. [Google Scholar] [CrossRef]
- Fathilah, A.R.; Himratul-Aznita, W.H.; Fatheen, A.R.N.; Suriani, K.R. The Antifungal Properties of Chlorhexidine Digluconate and Cetylpyrinidinium Chloride on Oral Candida. J. Dent. 2012, 40, 609–615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suci, P.A.; Tyler, B.J. Action of Chlorhexidine Digluconate against Yeast and Filamentous Forms in an Early-Stage Candida albicans Biofilm. Antimicrob. Agents Chemother. 2002, 46, 3522–3531. [Google Scholar] [CrossRef] [Green Version]
- Vergara-Buenaventura, A.; Castro-Ruiz, C. Use of Mouthwashes against COVID-19 in Dentistry. Br. J. Oral Maxillofac. Surg. 2020, 58, 924–927. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Laguna, V.; García-Luque, I.; Ballesta, S.; Pérez-Artiaga, L.; Lampaya-Pérez, V.; Rezusta, A.; Gilaberte, Y. Photodynamic Therapy Using Methylene Blue, Combined or Not with Gentamicin, against Staphylococcus aureus and Pseudomonas aeruginosa. Photodiagnosis Photodyn. Ther. 2020, 31, 101810. [Google Scholar] [CrossRef]
- Pérez-Laguna, V.; García-Luque, I.; Ballesta, S.; Pérez-Artiaga, L.; Lampaya-Pérez, V.; Samper, S.; Soria-Lozano, P.; Rezusta, A.; Gilaberte, Y. Antimicrobial Photodynamic Activity of Rose Bengal, Alone or in Combination with Gentamicin, against Planktonic and Biofilm Staphylococcus Aureus. Photodiagnosis Photodyn. Ther. 2018, 21, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Laguna, V.; Pérez-Artiaga, L.; Lampaya-Pérez, V.; García-Luque, I.; Ballesta, S.; Nonell, S.; Paz-Cristobal, M.P.; Gilaberte, Y.; Rezusta, A. Bactericidal Effect of Photodynamic Therapy, Alone or in Combination with Mupirocin or Linezolid, on Staphylococcus Aureus. Front. Microbiol. 2017. [Google Scholar] [CrossRef] [Green Version]
- Daliri, F.; Azizi, A.; Goudarzi, M.; Lawaf, S.; Rahimi, A. In Vitro Comparison of the Effect of Photodynamic Therapy with Curcumin and Methylene Blue on Candida albicans Colonies. Photodiagnosis Photodyn. Ther. 2019, 26, 193–198. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira-Silva, T.; Alvarenga, L.H.; Lima-Leal, C.; Godoy-Miranda, B.; Carribeiro, P.; Suzuki, L.C.; Simões Ribeiro, M.; Tiemy Kato, I.; Pavani, C.; Prates, R.A. Effect of Photodynamic Antimicrobial Chemotherapy on Candida albicans in the Presence of Glucose. Photodiagnosis Photodyn. Ther. 2019, 27, 54–58. [Google Scholar] [CrossRef]
- Ferreira, L.R.; Sousa, A.S.; Alvarenga, L.H.; Deana, A.M.; de Santi, M.E.O.S.; Kato, I.T.; Leal, C.R.L.; Ribeiro, M.S.; Prates, R.A. Antimicrobial Photodynamic Therapy on Candida albicans Pre-Treated by Fluconazole Delayed Yeast Inactivation. Photodiagnosis Photodyn. Ther. 2016, 15, 25–27. [Google Scholar] [CrossRef]
- Güzel Tunçcan, Ö.; Kalkancı, A.; Unal, E.A.; Abdulmajed, O.; Erdoğan, M.; Dizbay, M.; Çağlar, K. The In Vitro Effect of Antimicrobial Photodynamic Therapy on Candida and Staphylococcus Biofilms. Turk. J. Med. Sci. 2018, 48, 873–879. [Google Scholar] [CrossRef]
- Černáková, L.; Chupáčová, J.; Židlíková, K.; Bujdáková, H. Effectiveness of the Photoactive Dye Methylene Blue versus Caspofungin on the Candida Parapsilosis Biofilm In Vitro and Ex Vivo. Photochem. Photobiol. 2015, 91, 1181–1190. [Google Scholar] [CrossRef]
- Ahmed, H.Y.A.; Mekawey, A.A.I.; Morsy, M.E. Cellular Structural Changes in Two Candida Species Caused by Photodynamic Therapy. Merit Res. J. Microbiol. Biol. Sci. 2016, 4, 39–54. [Google Scholar]
- Lyon, J.P.; Carvalho, C.R.; Rezende, R.R.; Lima, C.J.; Santos, F.V.; Moreira, L.M. Synergism between Fluconazole and Methylene Blue-Photodynamic Therapy against Fluconazole-Resistant Candida Strains. Indian J. Med. Microbiol. 2016, 34, 506–508. [Google Scholar] [CrossRef]
- Queiroga, A.S.; Trajano, V.N.; Lima, E.O.; Ferreira, A.F.M.; Queiroga, A.S.; Limeira, F.A. In Vitro Photodynamic Inactivation of Candida spp. by Different Doses of Low Power Laser Light. Photodiagnosis Photodyn. Ther. 2011, 8, 332–336. [Google Scholar] [CrossRef] [PubMed]
- de Souza, S.C.; Junqueira, J.C.; Balducci, I.; Koga-Ito, C.Y.; Munin, E.; Jorge, A.O.C. Photosensitization of Different Candida Species by Low Power Laser Light. J. Photochem. Photobiol. B Biol. 2006, 83, 34–38. [Google Scholar] [CrossRef]
- Jamiu, A.T.; Albertyn, J.; Sebolai, O.M.; Pohl, C.H. Update on Candida Krusei, a Potential Multidrug-Resistant Pathogen. Med. Mycol. 2021, 59, 14–30. [Google Scholar] [CrossRef]
- Valandro, P.; Massuda, M.B.; Rusch, E.; Birgel, D.B.; Pereira, P.P.L.; Sellera, F.P.; Ribeiro, M.S.; Pogliani, F.C.; Birgel Junior, E.H. Antimicrobial Photodynamic Therapy Can Be an Effective Adjuvant for Surgical Wound Healing in Cattle. Photodiagnosis Photodyn. Ther. 2021, 33, 102168. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; Li, Y.; Wang, Y.; Chen, S.; Jiang, S.; Ge, H.; Lei, L.; Huang, X. Disinfect Porphyromonas gingivalis Biofilm on Titanium Surface with Combined Application of Chlorhexidine and Antimicrobial Photodynamic Therapy. Photochem. Photobiol. 2019, 95, 839–845. [Google Scholar] [CrossRef]
- Giroldo, L.M.; Felipe, M.P.; de Oliveira, M.A.; Munin, E.; Alves, L.P.; Costa, M.S. Photodynamic Antimicrobial Chemotherapy (PACT) with Methylene Blue Increases Membrane Permeability in Candida albicans. Lasers Med. Sci. 2009, 24, 109–112. [Google Scholar] [CrossRef]
- Snell, S.B.; Foster, T.H.; Haidaris, C.G. Miconazole Induces Fungistasis and Increases Killing of Candida albicans Subjected to Photodynamic Therapy. Photochem. Photobiol. 2012, 88, 596–603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scwingel, A.R.; Barcessat, A.R.P.; Núñez, S.C.; Ribeiro, M.S. Antimicrobial Photodynamic Therapy in the Treatment of Oral Candidiasis in HIV-Infected Patients. Photomed. Laser Surg. 2012, 30, 429–432. [Google Scholar] [CrossRef]
- Azizi, A.; Amirzadeh, Z.; Rezai, M.; Lawaf, S.; Rahimi, A. Effect of Photodynamic Therapy with Two Photosensitizers on Candida albicans. J. Photochem. Photobiol. B 2016, 158, 267–273. [Google Scholar] [CrossRef] [PubMed]
- do Vale, L.R.; Delbem, A.; Arias, L.S.; Fernandes, R.A.; Vieira, A.; Barbosa, D.B.; Monteiro, D.R. Differential Effects of the Combination of Tyrosol with Chlorhexidine Gluconate on Oral Biofilms. Oral Dis. 2017, 23, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Ellepola, A.N.B.; Chandy, R.; Khan, Z.U. In Vitro Impact of Limited Exposure to Subtherapeutic Concentrations of Chlorhexidine Gluconate on the Adhesion-Associated Attributes of Oral Candida Species. Med. Princ. Pract. 2016, 25, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Niu, T.; Tian, Y.; Ren, Q.; Wei, L.; Li, X.; Cai, Q. Red Light Interferes in UVA-Induced Photoaging of Human Skin Fibroblast Cells. Photochem. Photobiol. 2014, 90, 1349–1358. [Google Scholar] [CrossRef]
- Jagdeo, J.; Austin, E.; Mamalis, A.; Wong, C.; Ho, D.; Siegel, D.M. Light-Emitting Diodes in Dermatology: A Systematic Review of Randomized Controlled Trials. Lasers Surg. Med. 2018, 50, 613–628. [Google Scholar] [CrossRef] [PubMed]
- Andrade, M.C.; Ribeiro, A.P.D.; Dovigo, L.N.; Brunetti, I.L.; Giampaolo, E.T.; Bagnato, V.S.; Pavarina, A.C. Effect of Different Pre-Irradiation Times on Curcumin-Mediated Photodynamic Therapy against Planktonic Cultures and Biofilms of Candida spp. Arch. Oral Biol. 2013, 58, 200–210. [Google Scholar] [CrossRef] [Green Version]
- Fitzmaurice, S.; Eisen, D.B. Daylight Photodynamic Therapy: What Is Known and What Is Yet to be Determined. Dermatol. Surg. 2016, 42, 286–295. [Google Scholar] [CrossRef]
- Lee, C.-N.; Hsu, R.; Chen, H.; Wong, T.-W. Daylight Photodynamic Therapy: An Update. Molecules 2020, 25, 5195. [Google Scholar] [CrossRef]
- Nguyen, M.; Sandhu, S.S.; Sivamani, R.K. Clinical Utility of Daylight Photodynamic Therapy in the Treatment of Actinic Keratosis–a Review of the Literature. Clin. Cosmet. Investig. Dermatol. 2019, 12, 427–435. [Google Scholar] [CrossRef] [Green Version]
- Torres-Hurtado, S.A.; Ramírez-Ramírez, J.; Larios-Morales, A.C.; Ramírez-San-Juan, J.C.; Ramos-García, R.; Espinosa-Texis, A.P.; Spezzia-Mazzocco, T. Efficient in Vitro Photodynamic Inactivation Using Repetitive Light Energy Density on Candida albicans and Trichophyton mentagrophytes. Photodiagnosis Photodyn. Ther. 2019, 26, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Souza, R.C.; Junqueira, J.C.; Rossoni, R.D.; Pereira, C.A.; Munin, E.; Jorge, A.O.C. Comparison of the Photodynamic Fungicidal Efficacy of Methylene Blue, Toluidine Blue, Malachite Green and Low-Power Laser Irradiation Alone against Candida albicans. Lasers Med. Sci. 2010, 25, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Peloi, L.S.; Soares, R.R.S.; Biondo, C.E.G.; Souza, V.R.; Hioka, N.; Kimura, E. Photodynamic Effect of Light-Emitting Diode Light on Cell Growth Inhibition Induced by Methylene Blue. J. Biosci. 2008, 33, 231–237. [Google Scholar] [CrossRef] [PubMed]

| Reduction in the Number of CFU/100 μL | Lamp Used | Treatment | MB Concentration Required for Each Yeast | ||
|---|---|---|---|---|---|
| C. albicans | C. parapsilosis | C. krusei | |||
| 3 log10 | 625 nm LED-lamp | MB-aPDT | 40 | 40–80 | 160 |
| MB-aPDT + CHX | 5 | 20 | 80–160 | ||
| WMH lamp | MB-aPDT | 40 | 20–40 | 80–160 | |
| MB-aPDT + CHX | 20 | 5–10 | 40–80 | ||
| 6 log10 | 625 nm LED-lamp | MB-aPDT | 320 | 320 | 320 |
| MB-aPDT + CHX | 320 | 320 | 320 | ||
| WMH lamp | MB-aPDT | 320 | 80 | 320–640 | |
| MB-aPDT + CHX | 80 | 80 | 320–640 | ||
| Study | Strain | Concentration (μg/mL) | Media | Source and Wavelength (nm) | Fluence (J/cm2) | Irradiance (mW/cm2) | Initial Load (CFU/mL) | Load Reduction (log10) |
|---|---|---|---|---|---|---|---|---|
| Güzel Tunçcan et al. (2018) [31] | C. albicans ATCC 90028 | 25 | saline | LED-660 | 0.233 | ND | 106 | 3 log10 |
| de Oliveira-Silva et al. (2019) [29] | C. albicans ATCC 10231 | 32 | PBS | LED-660 | 10 | 165 | 2.5 × 106 | 0.5 log10 |
| 30 | 6 log10 | |||||||
| 60 | 6 log10 | |||||||
| Ferreira et al. (2016) [30] | C. albicans ATCC 90028 | 32 | ND | LED-660 | 30 | 250 | 6.31 × 105 | 0.5 log10 |
| 60 | 6 log10 | |||||||
| 120 | 6 log10 | |||||||
| Daliri et al. (2019) [28] | C. albicans ATCC 10231 | 100 | ND | Laser-660 | ND | ND | 1.5 × 108 | 3.3 log10 |
| 200 | 3.43 log10 | |||||||
| Torres-Hurtado et al. (2019) [52] | C. albicans | 6.4 | PBS | LED-600-650 | 60 | 85 | 2–4 × 105 | >5 log10 |
| Souza et al. (2010) [53] | C. albicans ATCC 18804 | 100 | saline 0.85% | Laser-660 | 39.5 | 92 | 106 | 3 log10 |
| Peloi et al. (2008) [54] | C. albicans ATCC 90028 | 22.5 | saline 0.85% | LED-663 | 6 | ND | 1–2 × 108 | 1.31 log10 |
| Souza et al. (2006) [36] | C. albicans ATCC 18804 | 100 | saline 0.85% | Laser-685 | 28 | 92 | 106 | 1.25 log10 |
| Valkov et al. (2021) [13] | C. albicans ATCC 90028 | 1.6 | saline 0.90% | 18 W white luminescent lamp-400–700 | 27 | 1.9 ± 0.1 | 1–3 × 106 | 0 |
| Soria-Lozano et al. (2015) [12] | C. albicans ATCC 10231 | 160 | sterile distilled water | WMH-420-700 | 37 | 90 | 1 × 106−7 | 5 log10 |
| This work | C. albicans ATCC 10231 | 320 | sterile distilled water | LED-625 | 18 | 7 | >106 | 6 log10 |
| 320 | WMH-420-700 | 90 | 6 log10 | |||||
| Güzel Tunçcan et al. (2018) [31] | C. parapsilosis ATCC 96142 | 25 | saline | LED-660 | 0.233 | ND | 3 × 106 | 4 log10 |
| Černáková et al. (2015) [32] | C. parapsilosis ATCC 22019 | 9,6 | ND | LED-576-672 | 15 | 1.67 | ND | 1.16 log10 |
| C. parapsilosis 16755/2 | 1.27 log10 | |||||||
| C. parapsilosis 21922/1 | 1.13 log10 | |||||||
| Ahmed et al. (2016) [33] | C. parapsilosis | 100 | ND | Laser-660 | 90 | 300 | 350 | 0.59 log10 |
| 180 | 0.85 log10 | |||||||
| This work | C. parapsilosis ATCC 22019 | 320 | sterile distilled water | LED-625 | 18 | 7 | >106 | 6 log10 |
| 80 | WMH-420-700 | 90 | 6 log10 | |||||
| Lyon et al. (2016) [34] | C. krusei | 16 | ND | ND | ND | 200 | ≈5 × 105 | 0.25 log10 |
| Queiroga et al. (2011) [35] | C. krusei (ATCC 6258, ATCC 6358, LM08, LM12, LM120) | 150 | saline 0.85% | Laser-660 | 60 | 1000 | 6 × 105 | 0.18 log10 |
| 120 | 0.40 log10 | |||||||
| 180 | 0.65 log10 | |||||||
| Souza et al. (2006) [36] | C. krusei ATCC 6258 | 100 | saline 0.85% | Laser-685 | 28 | 92 | 106 | 1.54 log10 |
| This work | C. krusei ATCC 6258 | 320 | sterile distilled water | LED-625 | 18 | 7 | >106 | 6 log10 |
| 320–640 | WMH-420-700 | 90 | 6 log10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Laguna, V.; Barrena-López, Y.; Gilaberte, Y.; Rezusta, A. In Vitro Effect of Photodynamic Therapy with Different Lights and Combined or Uncombined with Chlorhexidine on Candida spp. Pharmaceutics 2021, 13, 1176. https://doi.org/10.3390/pharmaceutics13081176
Pérez-Laguna V, Barrena-López Y, Gilaberte Y, Rezusta A. In Vitro Effect of Photodynamic Therapy with Different Lights and Combined or Uncombined with Chlorhexidine on Candida spp. Pharmaceutics. 2021; 13(8):1176. https://doi.org/10.3390/pharmaceutics13081176
Chicago/Turabian StylePérez-Laguna, Vanesa, Yolanda Barrena-López, Yolanda Gilaberte, and Antonio Rezusta. 2021. "In Vitro Effect of Photodynamic Therapy with Different Lights and Combined or Uncombined with Chlorhexidine on Candida spp." Pharmaceutics 13, no. 8: 1176. https://doi.org/10.3390/pharmaceutics13081176
APA StylePérez-Laguna, V., Barrena-López, Y., Gilaberte, Y., & Rezusta, A. (2021). In Vitro Effect of Photodynamic Therapy with Different Lights and Combined or Uncombined with Chlorhexidine on Candida spp. Pharmaceutics, 13(8), 1176. https://doi.org/10.3390/pharmaceutics13081176