Physicochemical Stability and Compatibility Testing of Voriconazole in All-in-One Parenteral Nutrition Admixtures
Abstract
:1. Introduction
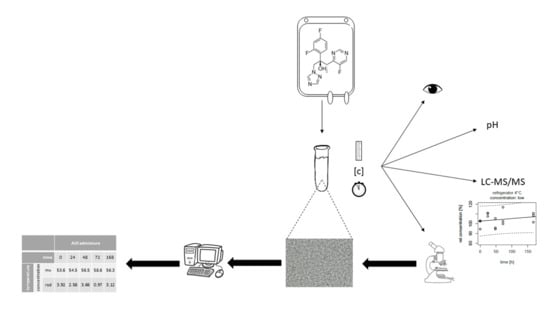
2. Materials and Methods
2.1. Sample Preparation
2.2. Visual Inspection
2.3. LC–MS/MS Analysis
2.3.1. Pretesting
2.3.2. Testing
2.3.3. pH Measurement
2.3.4. Microscopic Evaluation
2.4. Statistical Analysis
3. Results
3.1. Visual Inspection
3.2. pH Measurement
3.3. LC–MS/MS Analysis
3.4. Microscopic Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dudrick, S.J. History of parenteral nutrition. J. Am. Coll. Nutr. 2009, 28, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Reber, E.; Messerli, M.; Stanga, Z.; Mühlebach, S. Pharmaceutical Aspects of Artificial Nutrition. J. Clin. Med. 2019, 8, 2017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mühlebach, S. Practical aspects of multichamber bags for total parenteral nutrition. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Mühlebach, S. Basics in clinical nutrition: Drugs and nutritional admixtures. e-SPEN Eur. E-J. Clin. Nutr. Metab. 2009, 4, e134–e136. [Google Scholar] [CrossRef] [Green Version]
- Mühlebach, S. Diets and Diet Therapy: Parenteral Nutrition. In Encyclopedia of Food Security and Sustainability, 2nd ed.; Ferranti, P., Berry, E.M., Anderson, J.R., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 131–142. [Google Scholar]
- Steger, P.J.; Mühlebach, S.F. Lipid peroxidation of intravenous lipid emulsions and all-in-one admixtures in total parenteral nutrition bags: The influence of trace elements. JPEN J. Parenter. Enter. Nutr. 2000, 24, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, D.F. Lipid injectable emulsions: Pharmacopeial and safety issues. Pharm. Res. 2006, 23, 1959–1969. [Google Scholar] [CrossRef] [PubMed]
- Hill, S.E.; Heldman, L.S.; Goo, E.D.; Whippo, P.E.; Perkinson, J.C. Fatal microvascular pulmonary emboli from precipitation of a total nutrient admixture solution. JPEN J. Parenter. Enter. Nutr. 1996, 20, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Mühlebach, S.; Discroll, D.F.; Aeberhard, C.; Stanga, Z. Stability and compatibility of parenteral nutrition (PN) admixtures. In Basics in Clinical Nutrition, 5th ed.; Sobotka, L., Allison, S.P., Forbes, A., Meier, R.F., Schneider, S.M., Soeters, P.B., Stanga, Z., van Gossum, A., Eds.; Galén: Prague, Czech Republic, 2019; pp. 354–362. [Google Scholar]
- Mühlebach, S.; Aeberhard, C.; Stanga, Z. Drugs and nutritional admixtures. In Basics in Clinical Nutrition, 5th ed.; Sobotka, L., Allison, S.P., Forbes, A., Meier, R.F., Schneider, S.M., Soeters, P.B., Stanga, Z., van Gossum, A., Eds.; Galén: Prague, Czech Republic, 2019; pp. 362–370. [Google Scholar]
- Globule Size Distribution in Lipid Injectable Emulsions; United States Pharmacopeia and National Formulary (USP 43–NF 38); 4: United States Pharmacopeial Convention: Rockville, MD, USA; pp. 6963–6966.
- Schmutz, C.W. Zubereitung Parenteraler Ernährungsmischungen in der Spitalapotheke; Untersuchungen zur pharmazeutischen Qualität und Stabilität: Bern, Switzerland, 1993. [Google Scholar]
- Cano, S.M.; Montoro, J.B.; Pastor, C.; Pou, L.; Sabin, P. Stability of ranitidine hydrochloride in total nutrient admixtures. Am. J. Hosp. Pharm. 1988, 45, 1100–1102. [Google Scholar] [CrossRef] [PubMed]
- Trissel, L.A.; Gilbert, D.L.; Martinez, J.F.; Baker, M.B.; Walter, W.V.; Mirtallo, J.M. Compatibility of medications with 3-in-1 parenteral nutrition admixtures. JPEN J. Parenter. Enter. Nutr. 1999, 23, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Husson, E.; Crauste-Manciet, S.; Hadj-Salah, E.; Séguier, J.-C.; Brossard, D. Compatibility of parenteral drugs with commercialized total parenteraladmixtures during simulated Y-site infusion. Nutr. Clin. Métabolisme 2003, 17, 72–79. [Google Scholar] [CrossRef]
- Husson, E.; Crauste-Manciet, S.; Hadj-Salah, È.; Séguier, J.-C.; Brossard, D. Compatibility of parenteral drugs with commercialized total parenteral admixtures: Injection of drug inside the admixtures. Nutr. Clin. Métabolisme 2003, 17, 8–14. [Google Scholar] [CrossRef]
- Bullock, L.; Clark, J.H.; Fitzgerald, J.F.; Glick, M.R.; Hancock, B.G.; Baenziger, J.C.; Black, C.D. The stability of amikacin, gentamicin, and tobramycin in total nutrient admixtures. JPEN J. Parenter. Enter. Nutr. 1989, 13, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Hussaarts, L.; Mühlebach, S.; Shah, V.P.; McNeil, S.; Borchard, G.; Fluhmann, B.; Weinstein, V.; Neervannan, S.; Griffiths, E.; Jiang, W.; et al. Equivalence of complex drug products: Advances in and challenges for current regulatory frameworks. Ann. N. Y. Acad. Sci. 2017, 1407, 39–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Ministry of Health Labour and Welfare. The Japanese Pharmacopoeia, 17th ed.; The Ministry of Health Labour and Welfare: Tokyo, Japan, 2016. [Google Scholar]
- MacKay, M.; Rusho, W.; Jackson, D.; McMillin, G.; Winther, B. Physical and chemical stability of iron sucrose in parenteral nutrition. Nutr. Clin. Pract. Off. Publ. Am. Soc. Parenter. Enter. Nutr. 2009, 24, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Aeberhard, C.; Steuer, C.; Saxer, C.; Huber, A.; Stanga, Z.; Mühlebach, S. Physicochemical stability and compatibility testing of levetiracetam in all-in-one parenteral nutrition admixtures in daily practice. Eur. J. Pharm. Sci. Off. J. Eur. Fed. Pharm. Sci. 2017, 96, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Matuszewski, B.K.; Constanzer, M.L.; Chavez-Eng, C.M. Strategies for the assessment of matrix effect in quantitative bioanalytical methods based on HPLC-MS/MS. Anal. Chem. 2003, 75, 3019–3030. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, D.F.; Thoma, A.; Franke, R.; Klutsch, K.; Nehne, J.; Bistrian, B.R. Lipid globule size in total nutrient admixtures prepared in three-chamber plastic bags. Am. J. Health-Syst. Pharm. AJHP Off. J. Am. Soc. Health-Syst. Pharm. 2009, 66, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Pertkiewicz, M.; Cosslett, A.; Mühlebach, S.; Dudrick, S.J. Basics in clinical nutrition: Stability of parenteral nutrition admixtures. e-SPEN Eur. E-J. Clin. Nutr. Metab. 2009, 4, e117–e119. [Google Scholar] [CrossRef] [Green Version]
- Bischoff, S.C.; Arends, J.; Dörje, F.; Engeser, P.; Hanke, G.; Köchling, K.; Leischker, A.H.; Mühlebach, S.; Schneider, A.; Seipt, C.; et al. S3-Guideline of the German Society for Nutritional Medicine (DGEM) in Cooperation with the GESKES and the AKE Nutritional Support in the Homecare and Outpatient Sector. Aktuel. Ernahr. 2013, 38, e101–e154. [Google Scholar]


| AiO admixture | SmofKabiven (SMK) | Nutriflex Lipid Special (NLS) | Nutriflex Omega Special (OLS) |
|---|---|---|---|
| Manufacturer | Fresenius Kabi AG | B. Braun Medical AG | B. Braun Medical AG |
| Volume (14) | 986 | 625 | 625 |
| Glucose [g] | 125 | 90 | 90 |
| Amino acid [g] | 50 | 35 | 35.9 |
| Fat [g] | 38 | 25 | 25 |
| Total energy [kcal] | 1100 | 738 | 740 |
| Nonprotein Energy [kcal] | 900 | 600 | 600 |
| Nitrogen [g] | 8 | 5 | 5 |
| Osmolarity [mOsmol/L] | 1500 | 1545 | 1545 |
| pH | 5.6 | 5–6 | 5–6 |
| Ratio kcal/g N | 113 | 120 | 120 |
| Fat [g] | |||
| Soybean oil (LCT) | 11.5 | 12.5 | 10 |
| Olive oil (LCT) | 9.5 | N/A | N/A |
| Fish oil (LCT) | 5.7 | N/A | N/A |
| Medium-Chain Triglycerides | 11.5 | 12.5 | 12.5 |
| Egg lecithin | N/A | 1.5 | N/A |
| Ω-3 fatty acids | 2.5 | N/A | 2.5 g |
| Monounsaturated fatty acids | N/A | 13 | 11.4 |
| Polyunsaturated fatty acids | N/A | 30.7 | 34.0 |
| Ratio Ω-3:Ω-6 | 1:2.5 | 1:7 | 1:2.7 |
| Essential fatty acids | N/A | 30.7 | 31.7 |
| Electrolyte [mmol] | |||
| Sodium | 41 | 33.5 | 33.5 |
| Potassium | 30 | 23.5 | 23.5 |
| Magnesium | 5.1 | 2.65 | 2.65 |
| Calcium | 2.5 | 2.65 | 2.65 |
| Phosphate | 12.2 | 10 | 10 |
| Chloride | 35.5 | 30 | 30 |
| Acetate | 105.5 | 30 | 30 |
| Zinc | 0.04 | 0.02 | 0.02 |
| Sulphate | 5.1 | N/A | N/A |
| Microscopic Parameter | Abbreviation | Unit | Specification |
|---|---|---|---|
| Largest lipid droplet in 15 fields | LLD1-15 | [µm] | ≤8 |
| Mean largest lipid droplet | MLLDmax | [µm] | <4.5 |
| Standard deviation of the largest lipid droplets | SDLLD | [µm] | ≤2 |
| Number of lipid droplets >5 um | LD > 5 µm | [n] | ≤9 |
| AiO Admix | SMK | NLS | OLS | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hours | 0 | 24 | 48 | 72 | 168 | 0 | 24 | 48 | 72 | 168 | 0 | 24 | 48 | 72 | 168 | ||
| KS | L | mv | 53.6 | 58.7 | 52.8 | 57.0 | 57.3 | 52.8 | 56.1 | 51.0 | 54.5 | 51.4 | 53.4 | 56.7 | 55.6 | 55.2 | 53.4 |
| rsd | 3.92 | 1.37 | 4.98 | 7.02 | 3.64 | 2.28 | 3.50 | 2.03 | 3.22 | 2.53 | 5.18 | 3.46 | 3.32 | 2.07 | 6.81 | ||
| M | mv | 256 | 264 | 256 | 238 | 262 | 247 | 246 | 244 | 246 | 231 | 238 | 253 | 257 | 239 | 221 | |
| rsd | 4.97 | 2.85 | 5.03 | 2.06 | 3.52 | 1.12 | 0.52 | 4.58 | 2.74 | 1.65 | 3.97 | 2.29 | 4.24 | 2.12 | 6.14 | ||
| H | mv | 480 | 514 | 500 | 475 | 514 | 480 | 469 | 473 | 474 | 430 | 447 | 433 | 438 | 472 | 465 | |
| rsd | 2.30 | 2.14 | 1.15 | 4.53 | 2.79 | 2.71 | 3.97 | 3.29 | 2.04 | 3.00 | 7.59 | 11.2 | 10.5 | 4.59 | 4.72 | ||
| RT | L | mv | 53.6 | 56.3 | 56.5 | 56.3 | 56.2 | 52.8 | 56.0 | 54.8 | 53.5 | 50.2 | 53.4 | 54.8 | 56.9 | 53.4 | 55.4 |
| rsd | 3.92 | 0.85 | 2.61 | 3.31 | 3.93 | 2.28 | 4.60 | 3.16 | 3.67 | 3.34 | 5.18 | 0.39 | 2.12 | 3.99 | 4.50 | ||
| M | mv | 256 | 264 | 257 | 241 | 266 | 247 | 251 | 255 | 254 | 231 | 238 | 248 | 232 | 241 | 254 | |
| rsd | 4.97 | 3.32 | 0.92 | 0.51 | 0.73 | 1.12 | 0.85 | 3.87 | 1.32 | 3.74 | 3.97 | 3.55 | 3.53 | 1.53 | 2.38 | ||
| H | mv | 480 | 526 | 489 | 471 | 504 | 480 | 496 | 496 | 487 | 468 | 447 | 484 | 465 | 484 | 469 | |
| rsd | 2.30 | 3.92 | 3.54 | 4.85 | 1.56 | 2.71 | 0.62 | 3.46 | 3.91 | 1.42 | 7.59 | 0.77 | 4.14 | 5.77 | 12.2 | ||
| WB | L | mv | 53.6 | 54.5 | 56.5 | 58.6 | 56.3 | 52.8 | 54.4 | 54.9 | 56.6 | 49.1 | 53.4 | 55.3 | 53.9 | 55.3 | 52.3 |
| rsd | 3.92 | 2.58 | 3.66 | 0.97 | 3.12 | 2.28 | 1.33 | 1.36 | 4.49 | 3.12 | 5.18 | 4.61 | 0.56 | 2.54 | 3.31 | ||
| M | mv | 256 | 246 | 254 | 243 | 251 | 247 | 252 | 257 | 257 | 219 | 238 | 236 | 255 | 264 | 237 | |
| rsd | 4.97 | 3.17 | 3.78 | 1.16 | 0.96 | 1.12 | 2.16 | 0.14 | 0.63 | 4.87 | 3.97 | 2.28 | 2.78 | 10.2 | 3.57 | ||
| H | mv | 480 | 482 | 523 | 492 | 511 | 480 | 497 | 501 | 513 | 416 | 447 | 481 | 486 | 484 | 467 | |
| rsd | 2.30 | 4.70 | 3.41 | 2.59 | 1.25 | 2.71 | 2.77 | 1.69 | 3.01 | 3.40 | 7.59 | 6.52 | 0.68 | 0.16 | 2.11 | ||
| SMK | NLS | OLS | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hours | 0 | 24 | 48 | 72 | 168 | 0 | 24 | 48 | 72 | 168 | 0 | 24 | 48 | 72 | 168 | ||
| MLLD | |||||||||||||||||
| KS | L | mv | - | 0.0 | 3.1 | 2.9 | 0.0 | - | 1.4 | 1.3 | 1.4 | 1.4 | - | 1.3 | 1.9 | 1.6 | 1.4 |
| M | mv | - | 0.0 | 2.9 | 2.6 | 2.7 | - | 1.6 | 1.5 | 1.3 | 1.3 | - | 1.5 | 2.1 | 1.4 | 1.3 | |
| H | mv | - | 0.0 | 2.7 | 2.6 | 2.7 | - | 1.8 | 1.6 | 1.6 | 1.7 | - | 1.3 | 1.3 | 1.3 | 1.7 | |
| RT | L | mv | 2.7 | 0.0 | 2.6 | 2.6 | 2.6 | 1.7 | 1.7 | 1.3 | 1.5 | 1.6 | 1.5 | 1.3 | 1.4 | 1.3 | 1.6 |
| M | mv | 2.6 | 0.0 | 2.6 | 0.0 | 2.6 | 2.0 | 1.5 | 1.6 | 1.6 | 1.6 | 1.5 | 1.6 | 1.8 | 1.3 | 1.5 | |
| H | mv | 2.6 | 0.0 | 2.6 | 2.6 | 0.0 | 1.9 | 1.3 | 1.6 | 1.3 | 1.7 | 1.3 | 1.5 | 1.8 | 1.3 | 1.7 | |
| WB | L | mv | - | 2.6 | 2.6 | 3.0 | 2.6 | - | 1.9 | 1.6 | 1.7 | 1.7 | - | 1.3 | 1.4 | 1.8 | 2.6 |
| M | mv | - | 2.6 | 2.6 | 2.8 | 2.6 | - | 1.8 | 1.6 | 2.1 | 1.7 | - | 1.3 | 2.3 | 1.4 | 2.6 | |
| H | mv | - | 3.0 | 2.6 | 2.9 | 0.0 | - | 1.4 | 1.3 | 1.8 | 3.0 | - | 1.8 | 1.4 | 1.3 | 2.4 | |
| LLD | |||||||||||||||||
| KS | L | mv | - | 0.0 | 5.2 | 3.9 | 0.0 | - | 2.6 | 1.3 | 2.6 | 2.6 | - | 1.3 | 2.6 | 2.6 | 2.6 |
| M | mv | - | 0.0 | 3.9 | 2.6 | 3.9 | - | 2.6 | 2.6 | 1.3 | 1.3 | - | 2.6 | 2.6 | 2.6 | 1.3 | |
| H | mv | - | 0.0 | 3.9 | 2.6 | 3.9 | - | 5.2 | 5.2 | 5.2 | 7.8 | - | 1.3 | 1.3 | 1.3 | 3.9 | |
| RT | L | mv | 3.9 | 0.0 | 2.6 | 2.6 | 2.6 | 2.6 | 5.2 | 1.3 | 2.6 | 3.9 | 2.6 | 1.3 | 2.6 | 1.3 | 5.2 |
| M | mv | 2.6 | 0.0 | 2.6 | 0.0 | 2.6 | 2.6 | 2.6 | 2.6 | 5.2 | 5.2 | 2.6 | 2.6 | 3.9 | 1.3 | 2.6 | |
| H | mv | 2.6 | 0.0 | 2.6 | 2.6 | 0.0 | 5.2 | 1.3 | 2.6 | 1.3 | 5.2 | 1.3 | 2.6 | 3.9 | 1.3 | 5.2 | |
| WB | L | mv | - | 2.6 | 2.6 | 3.9 | 2.6 | - | 5.2 | 2.6 | 6.5 | 3.9 | - | 1.3 | 2.6 | 3.9 | 3.9 |
| M | mv | - | 2.6 | 2.6 | 3.9 | 2.6 | - | 7.8 | 2.6 | 7.8 | 5.2 | - | 1.3 | 2.6 | 2.6 | 5.2 | |
| H | mv | - | 3.9 | 2.6 | 3.9 | 0.0 | - | 2.6 | 1.3 | 5.2 | 6.5 | - | 2.6 | 2.6 | 1.3 | 5.2 | |
| SDLLD | |||||||||||||||||
| KS | L | std | - | 0.0 | 0.8 | 0.0 | 0.0 | - | 0.3 | 0.0 | 0.3 | 0.3 | - | 0.0 | 0.6 | 0.6 | 0.3 |
| M | std | - | 0.0 | 0.6 | 0.0 | 0.4 | - | 0.6 | 0.4 | 0.0 | 0.0 | - | 0.5 | 0.6 | 0.4 | 0.0 | |
| H | std | - | 0.0 | 0.4 | 0.5 | 0.3 | - | 1.0 | 1.0 | 1.0 | 1.6 | - | 0.0 | 0.0 | 0.0 | 0.7 | |
| RT | L | std | 0.4 | 0.0 | 0.0 | 0.0 | 0.0 | 0.6 | 1.1 | 0.0 | 0.4 | 0.7 | 0.4 | 0.0 | 0.3 | 0.0 | 1.0 |
| M | std | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.6 | 0.5 | 0.5 | 1.0 | 1.0 | 0.4 | 0.6 | 0.8 | 0.0 | 0.4 | |
| H | std | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 1.0 | 0.0 | 0.5 | 0.0 | 1.0 | 0.0 | 0.5 | 0.8 | 0.0 | 1.0 | |
| WB | L | std | - | 0.0 | 0.0 | 0.6 | 0.0 | - | 1.1 | 0.6 | 1.3 | 0.7 | - | 0.0 | 0.3 | 0.9 | 0.8 |
| M | std | - | 0.0 | 0.0 | 0.5 | 0.0 | - | 1.6 | 0.6 | 1.6 | 1.1 | - | 0.0 | 0.5 | 0.4 | 0.8 | |
| H | std | - | 0.6 | 0.0 | 0.5 | 0.0 | - | 0.3 | 0.0 | 1.1 | 2.0 | - | 0.6 | 0.3 | 0.0 | 1.3 | |
| LD > 5 µm | |||||||||||||||||
| KS | L | n | - | 0 | 2 | 0 | 0 | - | 0 | 2 | 0 | 0 | - | 0 | 0 | 0 | 0 |
| M | n | - | 0 | 0 | 0 | 0 | - | 0 | 0 | 0 | 0 | - | 0 | 0 | 0 | 0 | |
| H | n | - | 0 | 0 | 0 | 0 | - | 1 | 1 | 1 | 1 | - | 0 | 0 | 0 | 0 | |
| RT | L | n | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| M | n | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | |
| H | n | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | |
| WB | L | n | - | 0 | 0 | 0 | 0 | - | 1 | 0 | 1 | 0 | - | 0 | 0 | 0 | 0 |
| M | n | - | 0 | 0 | 0 | 0 | - | 1 | 0 | 1 | 1 | - | 0 | 0 | 0 | 1 | |
| H | n | - | 0 | 0 | 0 | 0 | - | 0 | 0 | 1 | 2 | - | 0 | 0 | 0 | 2 | |
| SMK | NLS | OLS | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hours | 0 | 24 | 48 | 72 | 168 | 0 | 24 | 48 | 72 | 168 | 0 | 24 | 48 | 72 | 168 | ||
| MLLD | |||||||||||||||||
| KS | L | mv | - | 2.7 | 2.9 | 2.9 | 4.1 | - | 3.2 | 2.7 | 2.7 | 2.9 | - | 2.3 | 4.9 | 0.0 | 2.2 |
| M | mv | - | 2.1 | 3.0 | 3.0 | 2.9 | - | 2.1 | 2.4 | 2.4 | 3.2 | - | 3.2 | 3.3 | 3.3 | 3.9 | |
| H | mv | - | 2.4 | 3.0 | 3.0 | 2.6 | - | 3.9 | 2.6 | 2.6 | 0.0 | - | 2.3 | 3.6 | 3.6 | 3.6 | |
| RT | L | mv | 2.6 | 2.1 | 3.3 | 3.3 | 3.4 | 2.7 | 2.4 | 3.2 | 3.2 | 3.3 | 3.0 | 2.7 | 2.1 | 2.1 | 3.1 |
| M | mv | 2.4 | 2.1 | 2.2 | 2.2 | 2.7 | 2.4 | 2.5 | 3.2 | 3.2 | 4.5 | 3.4 | 3.4 | 2.1 | 2.1 | 2.6 | |
| H | mv | 2.6 | 4.2 | 4.9 | 0.0 | 2.2 | 2.6 | 2.4 | 5.3 | 0.0 | 2.5 | 3.5 | 2.6 | 2.5 | 2.5 | 2.4 | |
| WB | L | mv | - | 2.1 | 2.5 | 2.5 | 14 | - | 2.7 | 2.4 | 2.4 | 3.2 | - | 3.7 | 3.4 | 3.4 | 2.8 |
| M | mv | - | 2.8 | 2.7 | 2.7 | 3.5 | - | 3.9 | 3.4 | 3.4 | 2.7 | - | 2.5 | 3.5 | 3.5 | 3.1 | |
| H | mv | - | 2.0 | 4.1 | 4.1 | 3.2 | - | 2.8 | 2.9 | 3.0 | 4.5 | - | 2.7 | 3.6 | 3.6 | 6.3 | |
| LLD | |||||||||||||||||
| KS | L | mv | - | 2.7 | 4.6 | 4.6 | 0.0 | - | 4.8 | 3.0 | 3.0 | 3.9 | - | 2.6 | 15 | 0.0 | 2.4 |
| M | mv | - | 2.2 | 3.7 | 3.7 | 6.9 | - | 2.1 | 2.6 | 2.6 | 7.5 | - | 5.6 | 5.8 | 5.8 | 9.7 | |
| H | mv | - | 3.2 | 4.1 | 4.1 | 4.0 | - | 14 | 3.7 | 3.7 | 0.0 | - | 2.7 | 4.8 | 4.8 | 12 | |
| RT | L | mv | 3.3 | 2.3 | 3.9 | 3.9 | 7.7 | 3.0 | 3.0 | 5.5 | 5.5 | 3.8 | 4.1 | 4.5 | 2.1 | 2.1 | 5.4 |
| M | mv | 2.7 | 2.2 | 2.2 | 2.2 | 3.3 | 2.6 | 2.7 | 3.8 | 3.8 | 4.5 | 3.5 | 7.7 | 2.3 | 2.3 | 3.7 | |
| H | mv | 3.7 | 6.0 | 9.0 | 0.0 | 2.6 | 3.7 | 3.0 | 10 | 0.0 | 2.8 | 0.0 | 3.2 | 3.0 | 3.0 | 2.8 | |
| WB | L | mv | - | 2.2 | 3.4 | 3.4 | 26 | - | 5.7 | 3.0 | 3.0 | 7.8 | - | 4.7 | 6.1 | 6.1 | 5.8 |
| M | mv | - | 3.2 | 3.5 | 3.5 | 9.3 | - | 7.4 | 5.1 | 5.1 | 6.5 | - | 2.8 | 5.3 | 5.3 | 5.8 | |
| H | mv | - | 2.1 | 14 | 0.0 | 9.7 | - | 3.5 | 3.9 | 3.9 | 9.3 | - | 3.5 | 4.0 | 4.0 | 16 | |
| SDLLD | |||||||||||||||||
| KS | L | std | - | 0.0 | 0.9 | 0.9 | 0.0 | - | 1.3 | 0.3 | 0.3 | 0.7 | - | 0.4 | 4.6 | 0.0 | 0.2 |
| M | std | - | 0.1 | 0.9 | 0.9 | 1.7 | - | 0.0 | 0.3 | 0.3 | 1.7 | - | 0.9 | 1.2 | 1.2 | 2.6 | |
| H | std | - | 0.4 | 0.6 | 0.6 | 0.6 | - | 3.4 | 1.0 | 1.0 | 0.0 | - | 0.3 | 0.8 | 0.8 | 2.9 | |
| RT | L | std | 0.4 | 0.2 | 0.6 | 0.6 | 2.4 | 0.3 | 0.3 | 1.2 | 1.2 | 0.4 | 0.8 | 1.0 | 0.0 | 0.0 | 1.6 |
| M | std | 0.2 | 0.1 | 0.0 | 0.0 | 0.6 | 0.3 | 0.2 | 0.8 | 0.8 | 0.0 | 0.1 | 2.2 | 0.1 | 0.1 | 0.5 | |
| H | std | 0.9 | 2.6 | 3.4 | 0.0 | 0.4 | 1.0 | 0.4 | 4.1 | 0.0 | 0.4 | 0.0 | 0.5 | 0.4 | 0.4 | 0.4 | |
| WB | L | std | - | 0.1 | 0.6 | 0.6 | 16 | - | 1.0 | 0.3 | 0.3 | 1.5 | - | 1.0 | 1.5 | 1.5 | 1.1 |
| M | std | - | 0.6 | 0.7 | 0.7 | 1.8 | - | 3.1 | 1.6 | 1.6 | 1.0 | - | 0.4 | 1.2 | 1.2 | 1.0 | |
| H | std | - | 0.1 | 3.9 | 0.0 | 1.6 | - | 0.4 | 0.7 | 0.7 | 2.6 | - | 0.4 | 0.3 | 0.3 | 4.9 | |
| LD > 5 µm | |||||||||||||||||
| KS | L | n | - | 2 | 2 | 2 | 2 | - | 3 | 3 | 3 | 3 | - | 5 | 1 | 1 | 5 |
| M | n | - | 1 | 1 | 1 | 1 | - | 1 | 1 | 1 | 1 | - | 1 | 2 | 2 | 6 | |
| H | n | - | 1 | 1 | 1 | 1 | - | 3 | 3 | 3 | 0 | - | 1 | 1 | 1 | 1 | |
| RT | L | n | 2 | 1 | 1 | 1 | 1 | 3 | 3 | 1 | 1 | 3 | 1 | 1 | 1 | 1 | 1 |
| M | n | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 2 | |
| H | n | 1 | 1 | 2 | 2 | 1 | 3 | 3 | 2 | 2 | 3 | 1 | 1 | 1 | 1 | 1 | |
| WB | L | n | - | 1 | 1 | 1 | 1 | - | 1 | 1 | 1 | 1 | - | 2 | 1 | 1 | 2 |
| M | n | - | 3 | 3 | 3 | 3 | - | 1 | 1 | 1 | 1 | - | 2 | 1 | 1 | 2 | |
| H | n | - | 8 | 2 | 2 | 8 | - | 3 | 3 | 3 | 3 | - | 5 | 5 | 5 | 5 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reber, E.; Neyer, P.; Schönenberger, K.A.; Saxer, C.; Bernasconi, L.; Stanga, Z.; Huber, A.; Hammerer-Lercher, A.; Mühlebach, S. Physicochemical Stability and Compatibility Testing of Voriconazole in All-in-One Parenteral Nutrition Admixtures. Pharmaceutics 2021, 13, 1447. https://doi.org/10.3390/pharmaceutics13091447
Reber E, Neyer P, Schönenberger KA, Saxer C, Bernasconi L, Stanga Z, Huber A, Hammerer-Lercher A, Mühlebach S. Physicochemical Stability and Compatibility Testing of Voriconazole in All-in-One Parenteral Nutrition Admixtures. Pharmaceutics. 2021; 13(9):1447. https://doi.org/10.3390/pharmaceutics13091447
Chicago/Turabian StyleReber, Emilie, Peter Neyer, Katja A. Schönenberger, Christoph Saxer, Luca Bernasconi, Zeno Stanga, Andreas Huber, Angelika Hammerer-Lercher, and Stefan Mühlebach. 2021. "Physicochemical Stability and Compatibility Testing of Voriconazole in All-in-One Parenteral Nutrition Admixtures" Pharmaceutics 13, no. 9: 1447. https://doi.org/10.3390/pharmaceutics13091447
APA StyleReber, E., Neyer, P., Schönenberger, K. A., Saxer, C., Bernasconi, L., Stanga, Z., Huber, A., Hammerer-Lercher, A., & Mühlebach, S. (2021). Physicochemical Stability and Compatibility Testing of Voriconazole in All-in-One Parenteral Nutrition Admixtures. Pharmaceutics, 13(9), 1447. https://doi.org/10.3390/pharmaceutics13091447