Development and Evaluation of a Thermosensitive In Situ Gel Formulation for Intravaginal Delivery of Lactobacillus gasseri
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Microorganism and Cultivation
2.3. Freeze-Drying Procedure
2.4. Preparation of the Thermosensitive Gel Formulations Containing L. gasseri
2.5. Preparation of Hydrogels Diluted by Simulated Vaginal Fluid
2.6. Characterization of Gels
2.7. Response Surface Methodology (RSM)
2.8. Rheological Characterization of the Hydrogels
2.9. Assessment of the Distribution of L. gasseri within the Gel
2.10. In Vitro Release of L. gasseri
2.11. Evaluation of Different Prebiotics Added into the Gel
2.12. Microencapsulation of L. gasseri
2.13. Morphology and Particle Size Measurements
2.14. Stability Studies of the Gel
2.15. Statistical Analysis
3. Results
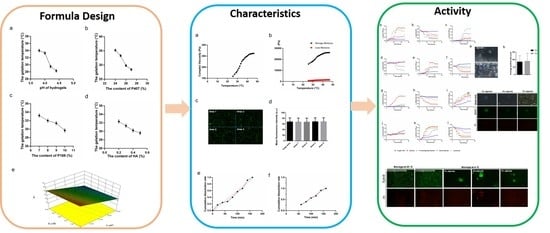
3.1. Effect of Hydrogels Composition on Gelation Temperature
3.2. RSM Model and Target Formulation
3.3. Rheological Characterization
3.4. Distribution of L. gasseri within the Gel
3.5. In Vitro Release of L. gasseri
3.6. Fermentation Profiles of Prebiotics by Vaginal Microbes
3.7. Morphology and Particle Size of Microspheres
3.8. Influence of the Storage Conditions
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kalia, N.; Singh, J.; Kaur, M. Microbiota in vaginal health and pathogenesis of recurrent vulvovaginal infections: A critical review. Ann. Clin. Microbiol. Antimicrob. 2020, 19, 5. [Google Scholar] [CrossRef] [PubMed]
- Bagnall, P.; Rizzolo, D. Bacterial vaginosis: A practical review. JAAPA 2017, 30, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Brotman, R.M.; Klebanoff, M.A.; Nansel, T.R.; Yu, K.F.; Andrews, W.W.; Zhang, J.; Schwebke, J.R. Bacterial vaginosis assessed by gram stain and diminished colonization resistance to incident gonococcal, chlamydial, and trichomonal genital infection. J. Infect. Dis. 2010, 202, 1907–1915. [Google Scholar] [CrossRef] [PubMed]
- Cohen, C.R.; Lingappa, J.R.; Baeten, J.M.; Ngayo, M.O.; Spiegel, C.A.; Hong, T.; Donnell, D.; Celum, C.; Kapiga, S.; Delany, S.; et al. Bacterial vaginosis associated with increased risk of female-to-male HIV-1 transmission: A prospective cohort analysis among African couples. PLoS Med. 2012, 9, e1001251. [Google Scholar] [CrossRef] [PubMed]
- Sobel, R.; Sobel, J.D. Metronidazole for the treatment of vaginal infections. Expert Opin. Pharmacother. 2015, 16, 1109–1115. [Google Scholar] [CrossRef]
- Taylor, B.D.; Darville, T.; Haggerty, C.L. Does bacterial vaginosis cause pelvic inflammatory disease? Sex Transm Dis. 2013, 40, 117–122. [Google Scholar] [CrossRef]
- Zhang, Q.-Q.; Liu, Z.-H.; Liu, L.-L.; Hu, G.; Lei, G.-L.; Wang, Y.; Cao, Y.; Wu, W.; Zhang, L.; Liao, Q.-P. Prebiotic Maltose Gel Can Promote the Vaginal Microbiota From BV-Related Bacteria Dominant to Lactobacillus in Rhesus Macaque. Front. Microbiol. 2020, 11, 594065. [Google Scholar] [CrossRef]
- Ravel, J.; Gajer, P.; Abdo, Z.; Schneider, G.M.; Koenig, S.S.; McCulle, S.L.; Karlebach, S.; Gorle, R.; Russell, J.; Tacket, C.O.; et al. Vaginal microbiome of reproductive-age women. Proc. Natl. Acad. Sci. USA 2011, 108 (Suppl. 1), 4680–4687. [Google Scholar] [CrossRef]
- Ricci, A.; Allende, A.; Bolton, D.; Chemaly, M.; Davies, R.; Girones, R.; Koutsoumanis, K.; Lindqvist, R.; Nørrung, B.; Robertson, L.; et al. Update of the list of QPS-recommended biological agents intentionally added to food or feed as notified to EFSA 6: Suitability of taxonomic units notified to EFSA until March 2017. Efsa J. 2017, 15, e04884. [Google Scholar] [CrossRef]
- Selle, K.; Klaenhammer, T.R. Genomic and phenotypic evidence for probiotic influences of Lactobacillus gasseri on human health. FEMS Microbiol. Rev. 2013, 37, 915–935. [Google Scholar] [CrossRef] [Green Version]
- Parolin, C.; Marangoni, A.; Laghi, L.; Foschi, C.; Ñahui Palomino, R.A.; Calonghi, N.; Cevenini, R.; Vitali, B. Isolation of Vaginal Lactobacilli and Characterization of Anti-Candida Activity. PLoS ONE 2015, 10, e0131220. [Google Scholar] [CrossRef]
- Maldonado-Barragán, A.; Caballero-Guerrero, B.; Martín, V.; Ruiz-Barba, J.L.; Rodríguez, J.M. Purification and genetic characterization of gassericin E, a novel co-culture inducible bacteriocin from Lactobacillus gasseri EV1461 isolated from the vagina of a healthy woman. BMC Microbiol. 2016, 16, 37. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Tian, W.; Guo, X.; Zhang, Y.; Liu, X.; Li, X.; Tian, Y.; Man, C.; Jiang, Y. Lactobacillus gasseri JM1 with potential probiotic characteristics alleviates inflammatory response by activating the PI3K/Akt signaling pathway in vitro. J. Dairy Sci. 2020, 103, 7851–7864. [Google Scholar] [CrossRef] [PubMed]
- Itapary Dos Santos, C.; Ramos França, Y.; Duarte Lima Campos, C.; Quaresma Bomfim, M.R.; Oliveira Melo, B.; Assunção Holanda, R.; Santos, V.L.; Gomes Monteiro, S.; Buozzi Moffa, E.; Souza Monteiro, A.; et al. Antifungal and Antivirulence Activity of Vaginal Lactobacillus Spp. Products against Candida Vaginal Isolates. Pathogens 2019, 8, 150. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Wang, Z.; Li, X.; Zhang, X.; Du, S.; Jia, M.; Hu, D.; Jia, X.; Cong, B.; Zhang, Y. A new Lactobacillus gasseri strain HMV18 inhibits the growth of pathogenic bacteria. Food Sci. Hum. Wellness 2022, 11, 247–254. [Google Scholar] [CrossRef]
- Ehrström, S.; Daroczy, K.; Rylander, E.; Samuelsson, C.; Johannesson, U.; Anzén, B.; Påhlson, C. Lactic acid bacteria colonization and clinical outcome after probiotic supplementation in conventionally treated bacterial vaginosis and vulvovaginal candidiasis. Microbes Infect. 2010, 12, 691–699. [Google Scholar] [CrossRef]
- Thapa, R.; Gurung, S.; Parat, M.-O.; Parekh, H.S.; Pandey, P. Application of Sol-Gels for Treatment of Gynaecological Conditions-Physiological Perspectives and Emerging Concepts in Intravaginal Drug Delivery. Gels 2022, 8, 99. [Google Scholar] [CrossRef]
- Dos Santos, A.M.; Carvalho, S.G.; Araujo, V.H.S.; Carvalho, G.C.; Gremião, M.P.D.; Chorilli, M. Recent advances in hydrogels as strategy for drug delivery intended to vaginal infections. Int. J. Pharm. 2020, 590, 119867. [Google Scholar] [CrossRef]
- Karavana, S.Y. A new in-situ gel formulation of itraconazole for vaginal administration. Pharmacol. Pharm. 2012, 3, 417. [Google Scholar] [CrossRef]
- N’Guessan Gnaman, K.C.; Bouttier, S.; Yeo, A.; Aka Any-Grah, A.A.S.; Geiger, S.; Huang, N.; Nicolas, V.; Villebrun, S.; Faye-Kette, H.; Ponchel, G.; et al. Characterization and in vitro evaluation of a vaginal gel containing Lactobacillus crispatus for the prevention of gonorrhea. Int. J. Pharm. 2020, 588, 119733. [Google Scholar] [CrossRef]
- Wang, X.; Liu, G.; Ma, J.; Guo, S.; Gao, L.; Jia, Y.; Li, X.; Zhang, Q. In situ gel-forming system: An attractive alternative for nasal drug delivery. Crit. Rev. Ther. Drug Carrier Syst. 2013, 30, 411–434. [Google Scholar] [CrossRef] [PubMed]
- Vigani, B.; Faccendini, A.; Rossi, S.; Sandri, G.; Bonferoni, M.C.; Grisoli, P.; Ferrari, F. Development of a Mucoadhesive in Situ Gelling Formulation for the Delivery of Lactobacillus gasseri into Vaginal Cavity. Pharmaceutics 2019, 11, 511. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.Y.; Oh, Y.K.; Kong, H.S.; Kim, E.J.; Jang, D.D.; Nam, K.T.; Kim, C.K. Prolonged antifungal effects of clotrimazole-containing mucoadhesive thermosensitive gels on vaginitis. J. Control Release 2002, 82, 39–50. [Google Scholar] [CrossRef]
- Giuliano, E.; Paolino, D.; Fresta, M.; Cosco, D. Drug-Loaded Biocompatible Nanocarriers Embedded in Poloxamer 407 Hydrogels as Therapeutic Formulations. Medicines 2018, 6, 7. [Google Scholar] [CrossRef]
- Chen, Y.; Lee, J.-H.; Meng, M.; Cui, N.; Dai, C.; Jia, Q.; Lee, E.-S.; Jiang, H. An Overview on Thermosensitive Oral Gel Based on Poloxamer 407. Materials 2021, 14, 4522. [Google Scholar] [CrossRef]
- Owen, D.H.; Katz, D.F. A vaginal fluid simulant. Contraception 1999, 59, 91–95. [Google Scholar] [CrossRef]
- Mayol, L.; Quaglia, F.; Borzacchiello, A.; Ambrosio, L.; La Rotonda, M.I. A novel poloxamers/hyaluronic acid in situ forming hydrogel for drug delivery: Rheological, mucoadhesive and in vitro release properties. Eur. J. Pharm. Biopharm. 2008, 70, 199–206. [Google Scholar] [CrossRef]
- Moore, S.; Kailasapathy, K.; Phillips, M.; Jones, M.R. Development of a viability standard curve for microencapsulated probiotic bacteria using confocal microscopy and image analysis software. J. Microbiol. Methods 2015, 114, 16–22. [Google Scholar] [CrossRef]
- Zhang, M.; Zhuang, B.; Du, G.; Han, G.; Jin, Y. Curcumin solid dispersion-loaded in situ hydrogels for local treatment of injured vaginal bacterial infection and improvement of vaginal wound healing. J. Pharm. Pharmacol. 2019, 71, 1044–1054. [Google Scholar] [CrossRef]
- Ur-Rehman, T.; Tavelin, S.; Grobner, G. Chitosan in situ gelation for improved drug loading and retention in poloxamer 407 gels. Int. J. Pharm. 2011, 409, 19–29. [Google Scholar] [CrossRef]
- Nappi, R.E.; Kotek, M.; Brest’ansky, A.; Giordan, N.; Beriotto, I.; Tramentozzi, E. Treatment of vulvo-vaginal atrophy with hyaluronate-based gel: A randomized controlled study. Minerva Obstet. Gynecol. 2021, 11. [Google Scholar] [CrossRef] [PubMed]
- Coudray, M.S.; Madhivanan, P. Bacterial vaginosis-A brief synopsis of the literature. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 245, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Zotta, T.; Guidone, A.; Tremonte, P.; Parente, E.; Ricciardi, A. A comparison of fluorescent stains for the assessment of viability and metabolic activity of lactic acid bacteria. World J. Microbiol. Biotechnol. 2012, 28, 919–927. [Google Scholar] [CrossRef] [PubMed]
- Di Costanzo, M.; Berni Canani, R. Lactose Intolerance: Common Misunderstandings. Ann. Nutr. Metab. 2018, 73 (Suppl. 4), 30–37. [Google Scholar] [CrossRef]
- Kaur, N.; Singh, B.; Sharma, S. Hydrogels for potential food application: Effect of sodium alginate and calcium chloride on physical and morphological properties. Pharma Innov. J. 2018, 7, 142–148. [Google Scholar]
- Oerlemans, M.; Bellen, G.; Claes, I.; Henkens, T.; Allonsius, N.; Wittouck, S.; Lebeer, S. Impact of a lactobacilli-containing gel on vulvovaginal candidosis and the vaginal microbiome. Sci. Rep. 2020, 10, 7976. [Google Scholar] [CrossRef]
- Unagolla, M.; Jayasuriya, C. Drug transport mechanisms and in vitro release kinetics of vancomycin encapsulated chitosan-alginate polyelectrolyte microparticles as a controlled drug delivery system. Eur. J. Pharm. Sci. 2018, 114, 199–209. [Google Scholar] [CrossRef]
- Nayak, K.; Pal, D.; Pradhan, J.; Hasnain, S. Fenugreek seed mucilage-alginate mucoadhesive beads of metformin HCl: Design, optimization and evaluation. Int. J. Biol. Macromol. 2013, 4, 144–154. [Google Scholar] [CrossRef]
- Hajar-Azhari, S.; Hafiz Abd Rahim, M.; Razid Sarbini, S.; Muhialdin, B.J.; Olusegun, L.; Saari, N. Enzymatically synthesised fructooligosaccharides from sugarcane syrup modulate the composition and short-chain fatty acid production of the human intestinal microbiota. Food Res. Int. 2021, 149, 110677. [Google Scholar] [CrossRef]
- Silva, K.C.G.; Sato, A.C.K. Biopolymer gels containing fructooligosaccharides. Food Res. Int. 2017, 101, 88–95. [Google Scholar] [CrossRef]
- Shimokawa, K.; Saegusa, K.; Ishii, F. Rheological properties of reversible thermo-setting in situ gelling solutions with the methylcellulose-polyethylene glycol-citric acid ternary system (2): Effects of various water-soluble polymers and salts on the gelling temperature. Colloids Surf. B Biointerfaces 2009, 74, 56–58. [Google Scholar] [CrossRef] [PubMed]





| Formulation | Low Actual | High Actual |
|---|---|---|
| P407 (%) | 24 | 27 |
| P188 (%) | 7 | 10 |
| HA (%) | 0.2 | 0.5 |
| pH | 3.8 | 4.4 |
| Formulation | P407 (%) | P188 (%) | Mean (±SD) Gelation Temperature (°C) |
|---|---|---|---|
| F1 | 25.00 | 7.00 | 35.3 ± 0.5 |
| F2 | 27.00 | 8.50 | 28.4 ± 0.5 |
| F3 | 27.00 | 6.38 | 29.5 ± 0.5 |
| F4 | 24.17 | 8.50 | 34.2 ± 0.5 |
| F5 | 27.00 | 10.62 | 27.5 ± 0.5 |
| F6 | 27.00 | 8.50 | 28.1 ± 0.5 |
| F7 | 27.00 | 8.50 | 28.2 ± 0.5 |
| F8 | 29.00 | 10.00 | 19 ± 0.5 |
| F9 | 29.83 | 8.50 | 20 ± 0.5 |
| F10 | 27.00 | 8.50 | 28.3 ± 0.5 |
| F11 | 25.00 | 10.00 | 29.8 ± 0.5 |
| F12 | 27.00 | 8.50 | 28.2 ± 0.5 |
| F13 | 29.00 | 7.00 | 22 ± 0.5 |
| Source | Sum of Squares | F Value | p-Value Prob > F |
|---|---|---|---|
| Model | 260.05 | 79.10 | *** |
| P407 | 244.00 | 148.45 | *** |
| P188 | 16.04 | 9.76 | * |
| Residual | 16.44 | ||
| Lack of Fit | 16.39 | 210.07 | *** |
| Pure Error | 0.052 | ||
| Cor Total | 276.48 |
| P407 (%) | P188 (%) | Desirability Gelation Temperature (°C) | Mean (±SD) Actuality Gelation Temperature (°C) |
|---|---|---|---|
| 26 | 8.86 | 30 | 29.6 ± 0.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Y.; Wang, T.; Chen, Z.; Ren, H.; Song, P.; Zhu, Y.; Liang, S.; Tzeng, C. Development and Evaluation of a Thermosensitive In Situ Gel Formulation for Intravaginal Delivery of Lactobacillus gasseri. Pharmaceutics 2022, 14, 1934. https://doi.org/10.3390/pharmaceutics14091934
Zhao Y, Wang T, Chen Z, Ren H, Song P, Zhu Y, Liang S, Tzeng C. Development and Evaluation of a Thermosensitive In Situ Gel Formulation for Intravaginal Delivery of Lactobacillus gasseri. Pharmaceutics. 2022; 14(9):1934. https://doi.org/10.3390/pharmaceutics14091934
Chicago/Turabian StyleZhao, Ye, Tianyuan Wang, Ziyi Chen, Hao Ren, Ping Song, Yingying Zhu, Shan Liang, and Chimeng Tzeng. 2022. "Development and Evaluation of a Thermosensitive In Situ Gel Formulation for Intravaginal Delivery of Lactobacillus gasseri" Pharmaceutics 14, no. 9: 1934. https://doi.org/10.3390/pharmaceutics14091934
APA StyleZhao, Y., Wang, T., Chen, Z., Ren, H., Song, P., Zhu, Y., Liang, S., & Tzeng, C. (2022). Development and Evaluation of a Thermosensitive In Situ Gel Formulation for Intravaginal Delivery of Lactobacillus gasseri. Pharmaceutics, 14(9), 1934. https://doi.org/10.3390/pharmaceutics14091934