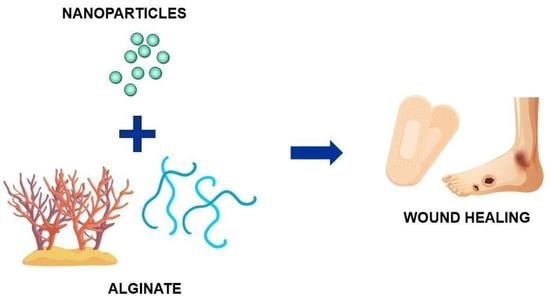
Alginate-Based Materials Loaded with Nanoparticles in Wound Healing
Abstract
:1. Introduction
2. Wounds: Pathophysiology, Classification, Therapeutic Approaches
3. Alginate: Structure, Properties, and Biomedical Applications
4. Alginate in Wound Dressings
5. Alginate Wound Dressings Loaded with Inorganic Particles
5.1. Nanocrystalline Silver (AgNP)
5.1.1. AgNP in Alginate-Only Matrices
5.1.2. AgNP in Hydrogels Composed of Alginate and Other Polymers
5.2. Zinc Oxide Nanoparticles (ZnO NP)
5.3. Other Inorganic Nanoparticles
6. Alginate Wound Dressings with Antibiotic and Antiseptic-Loaded Nanoparticles
7. Alginate Wound Dressings with Other Nanoparticles
8. Wound Healing Materials with Alginate Nanoparticles
9. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mervis, J.S.; Phillips, T.J. Pressure Ulcers: Pathophysiology, Epidemiology, Risk Factors, and Presentation. J. Am. Acad. Dermatol. 2019, 81, 881–890. [Google Scholar] [CrossRef]
- Grey, J.E.; Harding, K.G.; Enoch, S. Pressure Ulcers. BMJ 2006, 332, 472–475. [Google Scholar] [CrossRef] [PubMed]
- Kapp, S.; Miller, C.; Santamaria, N. The Quality of Life of People Who Have Chronic Wounds and Who Self-Treat. J. Clin. Nurs. 2018, 27, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Kapp, S.; Santamaria, N. The Financial and Quality-of-Life Cost to Patients Living with a Chronic Wound in the Community. Int. Wound J. 2017, 14, 1108–1119. [Google Scholar] [CrossRef]
- Renner, R.; Erfurt-Berge, C. Depression and Quality of Life in Patients with Chronic Wounds: Ways to Measure Their Influence and Their Effect on Daily Life. CWCMR 2017, 4, 143–151. [Google Scholar] [CrossRef] [Green Version]
- Järbrink, K.; Ni, G.; Sönnergren, H.; Schmidtchen, A.; Pang, C.; Bajpai, R.; Car, J. Prevalence and Incidence of Chronic Wounds and Related Complications: A Protocol for a Systematic Review. Syst. Rev. 2016, 5, 152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, R.; Liang, H.; Clarke, E.; Jackson, C.; Xue, M. Inflammation in Chronic Wounds. Int. J. Mol. Sci. 2016, 17, 2085. [Google Scholar] [CrossRef]
- Sen, C.K. Human Wound and Its Burden: Updated 2020 Compendium of Estimates. Adv. Wound Care 2021, 10, 281–292. [Google Scholar] [CrossRef]
- Nussbaum, S.R.; Carter, M.J.; Fife, C.E.; DaVanzo, J.; Haught, R.; Nusgart, M.; Cartwright, D. An Economic Evaluation of the Impact, Cost, and Medicare Policy Implications of Chronic Nonhealing Wounds. Value Health 2018, 21, 27–32. [Google Scholar] [CrossRef] [Green Version]
- Lindholm, C.; Searle, R. Wound Management for the 21st Century: Combining Effectiveness and Efficiency. Int. Wound J. 2016, 13, 5–15. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.S.; Sun, X.; Lee, J.-H.; Kim, H.-W.; Fu, X.; Leong, K.W. Advanced Drug Delivery Systems and Artificial Skin Grafts for Skin Wound Healing. Adv. Drug. Deliv. Rev. 2019, 146, 209–239. [Google Scholar] [CrossRef] [PubMed]
- Rezvani Ghomi, E.; Khalili, S.; Nouri Khorasani, S.; Esmaeely Neisiany, R.; Ramakrishna, S. Wound Dressings: Current Advances and Future Directions. J. Appl. Polym. Sci. 2019, 136, 47738. [Google Scholar] [CrossRef] [Green Version]
- Vowden, K.; Vowden, P. Wound Dressings: Principles and Practice. Surgery 2017, 35, 489–494. [Google Scholar] [CrossRef]
- Bi, D.; Yang, X.; Yao, L.; Hu, Z.; Li, H.; Xu, X.; Lu, J. Potential Food and Nutraceutical Applications of Alginate: A Review. Mar. Drugs 2022, 20, 564. [Google Scholar] [CrossRef] [PubMed]
- Jadach, B.; Świetlik, W.; Froelich, A. Sodium Alginate as a Pharmaceutical Excipient: Novel Applications of a Well-Known Polymer. J. Pharm. Sci. 2022, 111, 1250–1261. [Google Scholar] [CrossRef]
- Kozlowska, J.; Prus, W.; Stachowiak, N. Microparticles Based on Natural and Synthetic Polymers for Cosmetic Applications. Int. J. Biol. Macromol. 2019, 129, 952–956. [Google Scholar] [CrossRef]
- Sahoo, D.R.; Biswal, T. Alginate and Its Application to Tissue Engineering. SN Appl. Sci. 2021, 3, 30. [Google Scholar] [CrossRef]
- Morgan, D. Alginate Dressings: Part 1: Historical Aspects. J. Tissue Viability 1997, 7, 4–9. [Google Scholar] [CrossRef]
- Sorbsan—Sterile Calcium Aginate Wound Dressing Range. Available online: https://sorbsan.co.uk/ (accessed on 16 February 2023).
- Biatain® Alginate. Available online: https://products.coloplast.co.uk/coloplast/wound-care/biatain-alginate/ (accessed on 16 February 2023).
- Biatain® Alginate Ag. Available online: https://products.coloplast.co.uk/coloplast/wound-care/biatain-alginate-ag/ (accessed on 16 February 2023).
- Comfeel® Plus Dressing. Available online: https://products.coloplast.co.uk/coloplast/wound-care/comfeel-plus/comfeel-plus-dressing/ (accessed on 16 February 2023).
- KALTOSTAT® Calcium Sodium Alginate Dressing. Available online: https://www.convatec.com/products/advanced-wound-care/wound-type/wound-burns/kaltostat-calcium-sodium-alginate-dressing/ (accessed on 16 February 2023).
- CarboFlex® Dressing. Available online: https://www.convatec.com/en-gb/products/advanced-wound-care/wound-type/pc-wound-pressure-ulcers-stage-3-4/carboflex-dressing/ (accessed on 16 February 2023).
- 3MTM TegadermTM High Integrity Alginate Dressing. Available online: https://www.3m.com/3M/en_US/p/d/b5005108002/ (accessed on 16 February 2023).
- Sorbalgon®. Available online: https://www.hartmann.info/en-us/our-products/wound-management/advanced-wound-care-dressings/alginates/sorbalgon® (accessed on 16 February 2023).
- Sorbalgon® Ag. Available online: https://www.hartmann.info/en-us/our-products/wound-management/advanced-wound-care-dressings/alginates/sorbalgon®-ag (accessed on 16 February 2023).
- ACTICOAT Global. Available online: https://www.smith-nephew.com/en/health-care-professionals/products/advanced-wound-management/acticoat-global (accessed on 19 February 2023).
- Najahi-Missaoui, W.; Arnold, R.D.; Cummings, B.S. Safe Nanoparticles: Are We There Yet? Int. J. Mol. Sci. 2021, 22, 385. [Google Scholar] [CrossRef] [PubMed]
- Berthet, M.; Gauthier, Y.; Lacroix, C.; Verrier, B.; Monge, C. Nanoparticle-Based Dressing: The Future of Wound Treatment? Trends Biotechnol. 2017, 35, 770–784. [Google Scholar] [CrossRef]
- Tirumala, M.G.; Anchi, P.; Raja, S.; Rachamalla, M.; Godugu, C. Novel Methods and Approaches for Safety Evaluation of Nanoparticle Formulations: A Focus Towards In Vitro Models and Adverse Outcome Pathways. Front. Pharmacol. 2021, 12, 612659. [Google Scholar] [CrossRef] [PubMed]
- Vachhrajani, V.; Khakhkhar, P. Different Types of Wounds. In Science of Wound Healing and Dressing Materials; Vachhrajani, V., Khakhkhar, P., Eds.; Springer: Singapore, 2020; pp. 163–176. ISBN 978-981-329-236-9. [Google Scholar]
- McGuire, L.; Heffner, K.; Glaser, R.; Needleman, B.; Malarkey, W.; Dickinson, S.; Lemeshow, S.; Cook, C.; Muscarella, P.; Scott Melvin, W.; et al. Pain and Wound Healing in Surgical Patients. Ann. Behav. Med. 2006, 31, 165–172. [Google Scholar] [CrossRef]
- Gorin, D.R.; Cordts, P.R.; LaMorte, W.W.; Menzoian, J.O. The Influence of Wound Geometry on the Measurement of Wound Healing Rates in Clinical Trials. J. Vasc. Surg. 1996, 23, 524–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Percival, N.J. Classification of Wounds and Their Management. Surgery 2002, 20, 114–117. [Google Scholar] [CrossRef]
- Labbé, J.; Caouette, G. Recent Skin Injuries in Normal Children. Pediatrics 2001, 108, 271–276. [Google Scholar] [CrossRef] [Green Version]
- Bailey, B.R.; Eckerman, K.F.; Townsend, L.W. An Analysis of a Puncture Wound Case with Medical Intervention. Radiat. Prot. Dosim. 2003, 105, 509–512. [Google Scholar] [CrossRef]
- Thirupathi Kumara Raja, S.; Thiruselvi, T.; Sailakshmi, G.; Ganesh, S.; Gnanamani, A. Rejoining of Cut Wounds by Engineered Gelatin–Keratin Glue. Biochim. Biophys. Acta (BBA)—Gen. Subj. 2013, 1830, 4030–4039. [Google Scholar] [CrossRef] [PubMed]
- Barington, K.; Jensen, H.E. The Impact of Force on the Timing of Bruises Evaluated in a Porcine Model. J. Forensic Leg. Med. 2016, 40, 61–66. [Google Scholar] [CrossRef]
- Mlambo, S.S.; Parkar, H.; Naude, L.; Cromarty, A.D. Treatment of Acute Wounds and Injuries: Cuts, Bites, Bruises and Sprains. SA Pharm. J. 2022, 89, 12–18. [Google Scholar]
- Mankowitz, S.L. Laceration Management. J. Emerg. Med. 2017, 53, 369–382. [Google Scholar] [CrossRef]
- Lee, C.J.; Santos, P.J.F.; Vyas, R.M. Epidemiology, Socioeconomic Analysis, and Specialist Involvement in Dog Bite Wounds in Adults. J. Craniofacial Surg. 2019, 30, 753. [Google Scholar] [CrossRef] [PubMed]
- Rothe, K.; Tsokos, M.; Handrick, W. Animal and Human Bite Wounds. Dtsch. Arztebl. Int. 2015, 112, 433–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dreifke, M.B.; Jayasuriya, A.A.; Jayasuriya, A.C. Current Wound Healing Procedures and Potential Care. Mater. Sci. Eng. C 2015, 48, 651–662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, G.; Ceilley, R. Chronic Wound Healing: A Review of Current Management and Treatments. Adv. Ther. 2017, 34, 599–610. [Google Scholar] [CrossRef] [Green Version]
- Kirsner, R.S.; Eaglstein, W.H. The Wound Healing Process. Dermatol. Clin. 1993, 11, 629–640. [Google Scholar] [CrossRef]
- Alhajj, M.; Goyal, A. Physiology, Granulation Tissue. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Sorg, H.; Tilkorn, D.J.; Hager, S.; Hauser, J.; Mirastschijski, U. Skin Wound Healing: An Update on the Current Knowledge and Concepts. ESR 2017, 58, 81–94. [Google Scholar] [CrossRef]
- Weledji, E. Perspectives on Wound Healing. Austin J. Surg. 2017, 4, 1104. [Google Scholar] [CrossRef]
- Guo, S.; DiPietro, L.A. Factors Affecting Wound Healing. J. Dent. Res. 2010, 89, 219–229. [Google Scholar] [CrossRef]
- Abazari, M.; Ghaffari, A.; Rashidzadeh, H.; Badeleh, S.M.; Maleki, Y. A Systematic Review on Classification, Identification, and Healing Process of Burn Wound Healing. Int. J. Low. Extrem. Wounds 2022, 21, 18–30. [Google Scholar] [CrossRef]
- Gosain, A.; DiPietro, L.A. Aging and Wound Healing. World J. Surg. 2004, 28, 321–326. [Google Scholar] [CrossRef]
- Rezaie, F.; Momeni-Moghaddam, M.; Naderi-Meshkin, H. Regeneration and Repair of Skin Wounds: Various Strategies for Treatment. Int. J. Low. Extrem. Wounds 2019, 18, 247–261. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, R.G.; Unverdorben, M. Wound Cleaning and Wound Healing: A Concise Review. Adv. Ski. Wound Care 2013, 26, 160. [Google Scholar] [CrossRef]
- Das, A.; Datta, S.; Roche, E.; Chaffee, S.; Jose, E.; Shi, L.; Grover, K.; Khanna, S.; Sen, C.K.; Roy, S. Novel Mechanisms of Collagenase Santyl Ointment (CSO) in Wound Macrophage Polarization and Resolution of Wound Inflammation. Sci. Rep. 2018, 8, 1696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Percival, S.L.; Mayer, D.; Malone, M.; Swanson, T.; Gibson, D.; Schultz, G. Surfactants and Their Role in Wound Cleansing and Biofilm Management. J. Wound Care 2017, 26, 680–690. [Google Scholar] [CrossRef] [PubMed]
- Urban, M.V.; Rath, T.; Radtke, C. Hydrogen Peroxide (H2O2): A Review of Its Use in Surgery. Wien. Med. Wochenschr. 2019, 169, 222–225. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.-X.; Wu, Y.; Liang, P.-F.; Wu, R.-C.; Tian, L.-Y.; Mo, H.-Y. Efficacy of Combination of Localized Closure, Ethacridine Lactate Dressing, and Phototherapy in Treatment of Severe Extravasation Injuries: A Case Series. World J. Clin. Cases 2021, 9, 4599–4606. [Google Scholar] [CrossRef] [PubMed]
- Bai, M.-Y.; Chen, M.-C.; Yu, W.-C.; Lin, J.-Y. Foam Dressing Incorporating Herbal Extract: An All-Natural Dressing for Potential Use in Wound Healing. J. Bioact. Compat. Polym. 2017, 32, 293–308. [Google Scholar] [CrossRef]
- Guiomar, A.J.; Urbano, A.M. Polyhexanide-Releasing Membranes for Antimicrobial Wound Dressings: A Critical Review. Membranes 2022, 12, 1281. [Google Scholar] [CrossRef]
- Nuutila, K.; Eriksson, E. Moist Wound Healing with Commonly Available Dressings. Adv. Wound Care 2021, 10, 685–698. [Google Scholar] [CrossRef]
- Weller, C.; Weller, C.; Team, V. 4—Interactive Dressings and Their Role in Moist Wound Management. In Advanced Textiles for Wound Care, 2nd ed.; Rajendran, S., Ed.; The Textile Institute Book Series; Woodhead Publishing: Sawston, UK, 2019; pp. 105–134. ISBN 978-0-08-102192-7. [Google Scholar]
- Tellechea, A.; Leal, E.C.; Kafanas, A.; Auster, M.E.; Kuchibhotla, S.; Ostrovsky, Y.; Tecilazich, F.; Baltzis, D.; Zheng, Y.; Carvalho, E.; et al. Mast Cells Regulate Wound Healing in Diabetes. Diabetes 2016, 65, 2006–2019. [Google Scholar] [CrossRef] [Green Version]
- Thelwall, S.; Harrington, P.; Sheridan, E.; Lamagni, T. Impact of Obesity on the Risk of Wound Infection Following Surgery: Results from a Nationwide Prospective Multicentre Cohort Study in England. Clin. Microbiol. Infect. 2015, 21, 1008.e1–1008.e8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, E.; Zhang, H.; Jackson, J.K.; Lim, C.J.; Chiao, M. Janus Films with Stretchable and Waterproof Properties for Wound Care and Drug Delivery Applications. RSC Adv. 2016, 6, 79900–79909. [Google Scholar] [CrossRef]
- Olsson, M.; Järbrink, K.; Divakar, U.; Bajpai, R.; Upton, Z.; Schmidtchen, A.; Car, J. The Humanistic and Economic Burden of Chronic Wounds: A Systematic Review. Wound Repair. Regen. 2019, 27, 114–125. [Google Scholar] [CrossRef] [Green Version]
- Morton, L.M.; Phillips, T.J. Wound Healing and Treating Wounds: Differential Diagnosis and Evaluation of Chronic Wounds. J. Am. Acad. Dermatol. 2016, 74, 589–605. [Google Scholar] [CrossRef] [PubMed]
- Rowan, M.P.; Cancio, L.C.; Elster, E.A.; Burmeister, D.M.; Rose, L.F.; Natesan, S.; Chan, R.K.; Christy, R.J.; Chung, K.K. Burn Wound Healing and Treatment: Review and Advancements. Crit. Care 2015, 19, 243. [Google Scholar] [CrossRef] [Green Version]
- Kimmel, H.M.; Grant, A.; Ditata, J. The Presence of Oxygen in Wound Healing. Wounds 2016, 28, 264–270. [Google Scholar]
- Gompelman, M.; van Asten, S.A.V.; Peters, E.J.G. Update on the Role of Infection and Biofilms in Wound Healing: Pathophysiology and Treatment. Plast. Reconstr. Surg. 2016, 138, 61S–70S. [Google Scholar] [CrossRef]
- Mangoni, M.L.; McDermott, A.M.; Zasloff, M. Antimicrobial Peptides and Wound Healing: Biological and Therapeutic Considerations. Exp. Dermatol. 2016, 25, 167–173. [Google Scholar] [CrossRef] [Green Version]
- Sgonc, R.; Gruber, J. Age-Related Aspects of Cutaneous Wound Healing: A Mini-Review. GER 2013, 59, 159–164. [Google Scholar] [CrossRef]
- Rønø, B.; Engelholm, L.H.; Lund, L.R.; Hald, A. Gender Affects Skin Wound Healing in Plasminogen Deficient Mice. PLoS ONE 2013, 8, e59942. [Google Scholar] [CrossRef]
- Pastar, I.; Stojadinovic, O.; Yin, N.C.; Ramirez, H.; Nusbaum, A.G.; Sawaya, A.; Patel, S.B.; Khalid, L.; Isseroff, R.R.; Tomic-Canic, M. Epithelialization in Wound Healing: A Comprehensive Review. Adv. Wound Care 2014, 3, 445–464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hughes, O.; MacQuhae, F.; Rakosi, A.; Herskovitz, I.; Kirsner, R.S. Stress and Wound Healing. In Stress and Skin Disorders: Basic and Clinical Aspects; França, K., Jafferany, M., Eds.; Springer International Publishing: Cham, Switerland, 2017; pp. 185–207. ISBN 978-3-319-46352-0. [Google Scholar]
- Wynn, M.; Holloway, S. The Impact of Psychological Stress on Wound Healing: A Theoretical and Clinical Perspective. Wounds UK 2019, 15, 20–27. [Google Scholar]
- Makrantonaki, E.; Wlaschek, M.; Scharffetter-Kochanek, K. Pathogenesis of Wound Healing Disorders in the Elderly. JDDG J. Der Dtsch. Dermatol. Ges. 2017, 15, 255–275. [Google Scholar] [CrossRef] [PubMed]
- Pierpont, Y.N.; Dinh, T.P.; Salas, R.E.; Johnson, E.L.; Wright, T.G.; Robson, M.C.; Payne, W.G. Obesity and Surgical Wound Healing: A Current Review. ISRN Obes. 2014, 2014, 638936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fairweather, M.; Heit, Y.I.; Buie, J.; Rosenberg, L.M.; Briggs, A.; Orgill, D.P.; Bertagnolli, M.M. Celecoxib Inhibits Early Cutaneous Wound Healing. J. Surg. Res. 2015, 194, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.S.; Armstrong, E.J.; Armstrong, A.W. Corticosteroids and Wound Healing: Clinical Considerations in the Perioperative Period. Am. J. Surg. 2013, 206, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, D.; Jung, M.K.; Wang, H.J. Alcohol and the Immune System. Alcohol. Res. 2015, 37, 153–155. [Google Scholar]
- Lassig, A.A.D.; Bechtold, J.E.; Lindgren, B.R.; Pisansky, A.; Itabiyi, A.; Yueh, B.; Joseph, A.M. Tobacco Exposure and Wound Healing in Head and Neck Surgical Wounds. Laryngoscope 2018, 128, 618–625. [Google Scholar] [CrossRef]
- Larouche, J.; Sheoran, S.; Maruyama, K.; Martino, M.M. Immune Regulation of Skin Wound Healing: Mechanisms and Novel Therapeutic Targets. Adv. Wound Care 2018, 7, 209–231. [Google Scholar] [CrossRef]
- Toczek, J.; Sadłocha, M.; Major, K.; Stojko, R. Benefit of Silver and Gold Nanoparticles in Wound Healing Process after Endometrial Cancer Protocol. Biomedicines 2022, 10, 679. [Google Scholar] [CrossRef]
- Leaper, D.; Assadian, O.; Edmiston, C.E. Approach to Chronic Wound Infections. Br. J. Dermatol. 2015, 173, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Ousey, K.; Rogers, A.A.; Rippon, M.G. Hydro-Responsive Wound Dressings Simplify T.I.M.E. Wound Management Framework. Br. J. Community Nurs. 2016, 21, S39–S49. [Google Scholar] [CrossRef] [PubMed]
- Piemonte, G.; Benelli, L.; Braschi, F.; Rasero, L. The Local Treatment: Methodology, Debridement and Wound Bed Preparation. In Atlas of Ulcers in Systemic Sclerosis: Diagnosis and Management; Matucci-Cerinic, M., Denton, C.P., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 145–159. ISBN 978-3-319-98477-3. [Google Scholar]
- Zhang, H.; Cheng, J.; Ao, Q. Preparation of Alginate-Based Biomaterials and Their Applications in Biomedicine. Mar. Drugs 2021, 19, 264. [Google Scholar] [CrossRef] [PubMed]
- Urtuvia, V.; Maturana, N.; Acevedo, F.; Peña, C.; Díaz-Barrera, A. Bacterial Alginate Production: An Overview of Its Biosynthesis and Potential Industrial Production. World J. Microbiol. Biotechnol. 2017, 33, 198. [Google Scholar] [CrossRef]
- Fu, S.; Thacker, A.; Sperger, D.M.; Boni, R.L.; Buckner, I.S.; Velankar, S.; Munson, E.J.; Block, L.H. Relevance of Rheological Properties of Sodium Alginate in Solution to Calcium Alginate Gel Properties. AAPS PharmSciTech 2011, 12, 453–460. [Google Scholar] [CrossRef] [Green Version]
- Aguero, L.; Alpdagtas, S.; Ilhan, E.; Zaldivar-Silva, D.; Gunduz, O. Functional Role of Crosslinking in Alginate Scaffold for Drug Delivery and Tissue Engineering: A Review. Eur. Polym. J. 2021, 160, 110807. [Google Scholar] [CrossRef]
- Sanchez-Ballester, N.M.; Bataille, B.; Soulairol, I. Sodium Alginate and Alginic Acid as Pharmaceutical Excipients for Tablet Formulation: Structure-Function Relationship. Carbohydr. Polym. 2021, 270, 118399. [Google Scholar] [CrossRef]
- Lim, J.; Choi, G.; Joo, K.I.; Cha, H.J.; Kim, J. Embolization of Vascular Malformations via In Situ Photocrosslinking of Mechanically Reinforced Alginate Microfibers Using an Optical-Fiber-Integrated Microfluidic Device. Adv. Mater. 2021, 33, 2006759. [Google Scholar] [CrossRef]
- Agüero, L.; Zaldivar-Silva, D.; Peña, L.; Dias, M.L. Alginate Microparticles as Oral Colon Drug Delivery Device: A Review. Carbohydr. Polym. 2017, 168, 32–43. [Google Scholar] [CrossRef]
- Xu, M.; Qin, M.; Cheng, Y.; Niu, X.; Kong, J.; Zhang, X.; Huang, D.; Wang, H. Alginate Microgels as Delivery Vehicles for Cell-Based Therapies in Tissue Engineering and Regenerative Medicine. Carbohydr. Polym. 2021, 266, 118128. [Google Scholar] [CrossRef]
- Azarpira, N.; Kaviani, M.; Sarvestani, F.S. Incorporation of VEGF-and BFGF-Loaded Alginate Oxide Particles in Acellular Collagen-Alginate Composite Hydrogel to Promote Angiogenesis. Tissue Cell 2021, 72, 101539. [Google Scholar] [CrossRef]
- Kong, X.; Chen, L.; Li, B.; Quan, C.; Wu, J. Applications of Oxidized Alginate in Regenerative Medicine. J. Mater. Chem. B 2021, 9, 2785–2801. [Google Scholar] [CrossRef]
- Cheng, L.; Yao, B.; Hu, T.; Cui, X.; Shu, X.; Tang, S.; Wang, R.; Wang, Y.; Liu, Y.; Song, W.; et al. Properties of an Alginate-Gelatin-Based Bioink and Its Potential Impact on Cell Migration, Proliferation, and Differentiation. Int. J. Biol. Macromol. 2019, 135, 1107–1113. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, E.M.; Sayed, M.; El-Kady, A.M.; Elsayed, H.; Naga, S.M. In Vitro and in Vivo Study of Naturally Derived Alginate/Hydroxyapatite Bio Composite Scaffolds. Int. J. Biol. Macromol. 2020, 165, 1346–1360. [Google Scholar] [CrossRef]
- Liu, W.; Madry, H.; Cucchiarini, M. Application of Alginate Hydrogels for Next-Generation Articular Cartilage Regeneration. Int. J. Mol. Sci. 2022, 23, 1147. [Google Scholar] [CrossRef]
- Grijalvo, S.; Nieto-Díaz, M.; Maza, R.M.; Eritja, R.; Díaz, D.D. Alginate Hydrogels as Scaffolds and Delivery Systems to Repair the Damaged Spinal Cord. Biotechnol. J. 2019, 14, 1900275. [Google Scholar] [CrossRef] [Green Version]
- Wei, Q.; Zhou, J.; An, Y.; Li, M.; Zhang, J.; Yang, S. Modification, 3D Printing Process and Application of Sodium Alginate Based Hydrogels in Soft Tissue Engineering: A Review. Int. J. Biol. Macromol. 2023, 232, 123450. [Google Scholar] [CrossRef] [PubMed]
- Xie, F.; Zou, L.; Xu, Z.; Ou, X.; Guo, W.; Gao, Y.; Gao, G. Alginate Foam Gel Modified by Graphene Oxide for Wound Dressing. Int. J. Biol. Macromol. 2022, 223, 391–403. [Google Scholar] [CrossRef]
- Vijayan, A.; Vipin, C.L.; Kumar, G.S.V. Dual Growth Factor Entrapped Nanoparticle Enriched Alginate Wafer-Based Delivery System for Suppurating Wounds. Int. J. Biol. Macromol. 2022, 208, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Najafiasl, M.; Osfouri, S.; Azin, R.; Zaeri, S. Alginate-Based Electrospun Core/Shell Nanofibers Containing Dexpanthenol: A Good Candidate for Wound Dressing. J. Drug. Deliv. Sci. Technol. 2020, 57, 101708. [Google Scholar] [CrossRef]
- Shi, M.; Zhang, H.; Song, T.; Liu, X.; Gao, Y.; Zhou, J.; Li, Y. Sustainable Dual Release of Antibiotic and Growth Factor from PH-Responsive Uniform Alginate Composite Microparticles to Enhance Wound Healing. ACS Appl. Mater. Interfaces 2019, 11, 22730–22744. [Google Scholar] [CrossRef]
- Choudhary, M.; Chhabra, P.; Tyagi, A.; Singh, H. Scar Free Healing of Full Thickness Diabetic Wounds: A Unique Combination of Silver Nanoparticles as Antimicrobial Agent, Calcium Alginate Nanoparticles as Hemostatic Agent, Fresh Blood as Nutrient/Growth Factor Supplier and Chitosan as Base Matrix. Int. J. Biol. Macromol. 2021, 178, 41–52. [Google Scholar] [CrossRef]
- Salehi, M.; Ehterami, A.; Farzamfar, S.; Vaez, A.; Ebrahimi-Barough, S. Accelerating Healing of Excisional Wound with Alginate Hydrogel Containing Naringenin in Rat Model. Drug. Deliv. Transl. Res. 2021, 11, 142–153. [Google Scholar] [CrossRef] [PubMed]
- Aderibigbe, B.A.; Buyana, B. Alginate in Wound Dressings. Pharmaceutics 2018, 10, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ehterami, A.; Salehi, M.; Farzamfar, S.; Samadian, H.; Vaez, A.; Ghorbani, S.; Ai, J.; Sahrapeyma, H. Chitosan/Alginate Hydrogels Containing Alpha-Tocopherol for Wound Healing in Rat Model. J. Drug. Deliv. Sci. Technol. 2019, 51, 204–213. [Google Scholar] [CrossRef]
- Dhivya, S.; Padma, V.V.; Santhini, E. Wound Dressings—A Review. BioMed 2015, 5, 22. [Google Scholar] [CrossRef]
- Varaprasad, K.; Jayaramudu, T.; Kanikireddy, V.; Toro, C.; Sadiku, E.R. Alginate-Based Composite Materials for Wound Dressing Application:A Mini Review. Carbohydr. Polym. 2020, 236, 116025. [Google Scholar] [CrossRef] [PubMed]
- Sutar, T.; Bangde, P.; Dandekar, P.; Adivarekar, R. Herbal Hemostatic Biopolymeric Dressings of Alginate/Pectin Coated with Croton Oblongifolius Extract. Carbohydr. Polym. Technol. Appl. 2021, 2, 100025. [Google Scholar] [CrossRef]
- Sun, X.; Ma, C.; Gong, W.; Ma, Y.; Ding, Y.; Liu, L. Biological Properties of Sulfanilamide-Loaded Alginate Hydrogel Fibers Based on Ionic and Chemical Crosslinking for Wound Dressings. Int. J. Biol. Macromol. 2020, 157, 522–529. [Google Scholar] [CrossRef]
- Pelgrift, R.Y.; Friedman, A.J. Nanotechnology as a Therapeutic Tool to Combat Microbial Resistance. Adv. Drug. Deliv. Rev. 2013, 65, 1803–1815. [Google Scholar] [CrossRef] [PubMed]
- Wahid, F.; Zhong, C.; Wang, H.-S.; Hu, X.-H.; Chu, L.-Q. Recent Advances in Antimicrobial Hydrogels Containing Metal Ions and Metals/Metal Oxide Nanoparticles. Polymers 2017, 9, 636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alavi, M.; Nokhodchi, A. An Overview on Antimicrobial and Wound Healing Properties of ZnO Nanobiofilms, Hydrogels, and Bionanocomposites Based on Cellulose, Chitosan, and Alginate Polymers. Carbohydr. Polym. 2020, 227, 115349. [Google Scholar] [CrossRef] [PubMed]
- Carpa, R.; Remizovschi, A.; Culda, C.A.; Butiuc-Keul, A.L. Inherent and Composite Hydrogels as Promising Materials to Limit Antimicrobial Resistance. Gels 2022, 8, 70. [Google Scholar] [CrossRef] [PubMed]
- Meaume, S.; Vallet, D.; Morere, M.N.; Téot, L. Evaluation of a Silver-Releasing Hydroalginate Dressing in Chronic Wounds with Signs of Local Infection. J. Wound Care 2005, 14, 411–419. [Google Scholar] [CrossRef] [Green Version]
- Woo, K.Y.; Coutts, P.M.; Sibbald, R.G. A Randomized Controlled Trial to Evaluate an Antimicrobial Dressing with Silver Alginate Powder for the Management of Chronic Wounds Exhibiting Signs of Critical Colonization. Adv. Ski. Wound Care 2012, 25, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Fong, J.; Wood, F. Nanocrystalline Silver Dressings in Wound Management: A Review. Int. J. Nanomed. 2006, 1, 441–449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seo, S.Y.; Lee, G.H.; Lee, S.G.; Jung, S.Y.; Lim, J.O.; Choi, J.H. Alginate-Based Composite Sponge Containing Silver Nanoparticles Synthesized in Situ. Carbohydr. Polym. 2012, 90, 109–115. [Google Scholar] [CrossRef]
- Neibert, K.; Gopishetty, V.; Grigoryev, A.; Tokarev, I.; Al-Hajaj, N.; Vorstenbosch, J.; Philip, A.; Minko, S.; Maysinger, D. Wound-Healing with Mechanically Robust and Biodegradable Hydrogel Fibers Loaded with Silver Nanoparticles. Adv. Healthc. Mater. 2012, 1, 621–630. [Google Scholar] [CrossRef] [Green Version]
- Stojkovska, J.; Djurdjevic, Z.; Jancic, I.; Bufan, B.; Milenkovic, M.; Jankovic, R.; Miskovic-Stankovic, V.; Obradovic, B. Comparative in Vivo Evaluation of Novel Formulations Based on Alginate and Silver Nanoparticles for Wound Treatments. J. Biomater. Appl. 2018, 32, 1197–1211. [Google Scholar] [CrossRef]
- Cai, J.; Chen, X.; Wang, X.; Tan, Y.; Ye, D.; Jia, Y.; Liu, P.; Yu, H. High-Water-Absorbing Calcium Alginate Fibrous Scaffold Fabricated by Microfluidic Spinning for Use in Chronic Wound Dressings. RSC Adv. 2018, 8, 39463–39469. [Google Scholar] [CrossRef] [Green Version]
- Hu, W.-W.; Lin, Y.-T. Alginate/Polycaprolactone Composite Fibers as Multifunctional Wound Dressings. Carbohydr. Polym. 2022, 289, 119440. [Google Scholar] [CrossRef] [PubMed]
- Mokhena, T.C.; Luyt, A.S. Electrospun Alginate Nanofibres Impregnated with Silver Nanoparticles: Preparation, Morphology and Antibacterial Properties. Carbohydr. Polym. 2017, 165, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Yu, L.; Yin, X.; Lin, Y.; Xu, Y.; Niu, Y. Silver Nanoparticles with Vanadium Oxide Nanowires Loaded into Electrospun Dressings for Efficient Healing of Bacterium-Infected Wounds. J. Colloid Interface Sci. 2022, 622, 117–125. [Google Scholar] [CrossRef]
- Linhart, A.N.; Wortman-Otto, K.M.; Deninger, I.; Dudek, A.L.; Lange, H.R.; Danhausen, D.M.; Graverson, C.F.; Beckmann, T.J.; Havens, M.A.; Keleher, J.J. Strategic Design of Antimicrobial Hydrogels Containing Biomimetic Additives for Enhanced Matrix Responsiveness and HDFa Wound Healing Rates. ACS Appl. Bio Mater. 2020, 3, 5750–5758. [Google Scholar] [CrossRef] [PubMed]
- Ambrogi, V.; Pietrella, D.; Donnadio, A.; Latterini, L.; Di Michele, A.; Luffarelli, I.; Ricci, M. Biocompatible Alginate Silica Supported Silver Nanoparticles Composite Films for Wound Dressing with Antibiofilm Activity. Mater. Sci. Eng. C 2020, 112, 110863. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.U.; Gwon, J.; Lee, S.-Y.; Yoo, H.S. Silver-Incorporated Nanocellulose Fibers for Antibacterial Hydrogels. ACS Omega 2018, 3, 16150–16157. [Google Scholar] [CrossRef]
- Liang, L.; Hou, T.; Ouyang, Q.; Xie, L.; Zhong, S.; Li, P.; Li, S.; Li, C. Antimicrobial Sodium Alginate Dressing Immobilized with Polydopamine-Silver Composite Nanospheres. Compos. Part B Eng. 2020, 188, 107877. [Google Scholar] [CrossRef]
- Zhou, M.; Lin, F.; Li, W.; Shi, L.; Li, Y.; Shan, G. Development of Nanosilver Doped Carboxymethyl Chitosan-Polyamideamine Alginate Composite Dressing for Wound Treatment. Int. J. Biol. Macromol. 2021, 166, 1335–1351. [Google Scholar] [CrossRef]
- Gómez Chabala, L.F.; Cuartas, C.E.E.; López, M.E.L. Release Behavior and Antibacterial Activity of Chitosan/Alginate Blends with Aloe Vera and Silver Nanoparticles. Mar. Drugs 2017, 15, 328. [Google Scholar] [CrossRef] [Green Version]
- Gordienko, M.G.; Palchikova, V.V.; Kalenov, S.V.; Lebedev, E.A.; Belov, A.A.; Menshutina, N.V. The Alginate–Chitosan Composite Sponges with Biogenic Ag Nanoparticles Produced by Combining of Cryostructuration, Ionotropic Gelation and Ion Replacement Methods. Int. J. Polym. Mater. Polym. Biomater. 2022, 71, 34–44. [Google Scholar] [CrossRef]
- Chalitangkoon, J.; Wongkittisin, M.; Monvisade, P. Silver Loaded Hydroxyethylacryl Chitosan/Sodium Alginate Hydrogel Films for Controlled Drug Release Wound Dressings. Int. J. Biol. Macromol. 2020, 159, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Tan, Y.; Chen, X.; Ran, Y.; Tong, Q.; Tang, L.; Su, W.; Wang, X.; Li, X. Injectable Oxidized Alginate/Carboxylmethyl Chitosan Hydrogels Functionalized with Nanoparticles for Wound Repair. Carbohydr. Polym. 2022, 293, 119733. [Google Scholar] [CrossRef] [PubMed]
- Abou-Okeil, A.; Fahmy, H.M.; El-Bisi, M.K.; Ahmed-Farid, O.A. Hyaluronic Acid/Na-Alginate Films as Topical Bioactive Wound Dressings. Eur. Polym. J. 2018, 109, 101–109. [Google Scholar] [CrossRef]
- Tarusha, L.; Paoletti, S.; Travan, A.; Marsich, E. Alginate Membranes Loaded with Hyaluronic Acid and Silver Nanoparticles to Foster Tissue Healing and to Control Bacterial Contamination of Non-Healing Wounds. J. Mater. Sci. Mater. Med. 2018, 29, 22. [Google Scholar] [CrossRef] [Green Version]
- Catanzano, O.; D’Esposito, V.; Pulcrano, G.; Maiolino, S.; Ambrosio, M.R.; Esposito, M.; Miro, A.; Ungaro, F.; Formisano, P.; Catania, M.R.; et al. Ultrasmall Silver Nanoparticles Loaded in Alginate–Hyaluronic Acid Hybrid Hydrogels for Treating Infected Wounds. Int. J. Polym. Mater. Polym. Biomater. 2017, 66, 626–634. [Google Scholar] [CrossRef]
- Pankongadisak, P.; Ruktanonchai, U.R.; Supaphol, P.; Suwantong, O. Preparation and Characterization of Silver Nanoparticles-Loaded Calcium Alginate Beads Embedded in Gelatin Scaffolds. AAPS PharmSciTech 2014, 15, 1105–1115. [Google Scholar] [CrossRef] [Green Version]
- Baukum, J.; Pranjan, J.; Kaolaor, A.; Chuysinuan, P.; Suwantong, O.; Supaphol, P. The Potential Use of Cross-Linked Alginate/Gelatin Hydrogels Containing Silver Nanoparticles for Wound Dressing Applications. Polym. Bull. 2020, 77, 2679–2695. [Google Scholar] [CrossRef]
- Diniz, F.R.; Maia, R.C.A.P.; de Andrade, L.R.M.; Andrade, L.N.; Vinicius Chaud, M.; da Silva, C.F.; Corrêa, C.B.; de Albuquerque Junior, R.L.C.; Pereira da Costa, L.; Shin, S.R.; et al. Silver Nanoparticles-Composing Alginate/Gelatine Hydrogel Improves Wound Healing In Vivo. Nanomaterials 2020, 10, 390. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.; Peng, M.; Cheng, T.; Zhao, P.; Qiu, L.; Zhou, J.; Lu, G.; Chen, J. Silver Nanoparticles-Doped Collagen–Alginate Antimicrobial Biocomposite as Potential Wound Dressing. J. Mater. Sci. 2018, 53, 14944–14952. [Google Scholar] [CrossRef]
- Tao, G.; Cai, R.; Wang, Y.; Zuo, H.; He, H. Fabrication of Antibacterial Sericin Based Hydrogel as an Injectable and Mouldable Wound Dressing. Mater. Sci. Eng. C 2021, 119, 111597. [Google Scholar] [CrossRef]
- Vidovic, S.; Stojkovska, J.; Stevanovic, M.; Balanc, B.; Vukasinovic-Sekulic, M.; Marinkovic, A.; Obradovic, B. Effects of Poly(Vinyl Alcohol) Blending with Ag/Alginate Solutions to Form Nanocomposite Fibres for Potential Use as Antibacterial Wound Dressings. R. Soc. Open Sci. 2022, 9, 211517. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Wang, F.; Liu, S.; Wu, X.; Xu, L.; Zhang, D. In Situ Reduction of Silver Nanoparticles by Sodium Alginate to Obtain Silver-Loaded Composite Wound Dressing with Enhanced Mechanical and Antimicrobial Property. Int. J. Biol. Macromol. 2020, 148, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.; Fan, C.; Yang, Y.; Lee, B.H.; Wei, K. 5-Hydroxymethylfurfural-Embedded Poly (Vinyl Alcohol)/Sodium Alginate Hybrid Hydrogels Accelerate Wound Healing. Int. J. Biol. Macromol. 2019, 138, 933–949. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Singh, D. Radiation Synthesis of PVP/Alginate Hydrogel Containing Nanosilver as Wound Dressing. J. Mater. Sci. Mater. Med. 2012, 23, 2649–2658. [Google Scholar] [CrossRef] [PubMed]
- Król, A.; Pomastowski, P.; Rafińska, K.; Railean-Plugaru, V.; Buszewski, B. Zinc Oxide Nanoparticles: Synthesis, Antiseptic Activity and Toxicity Mechanism. Adv. Colloid. Interface Sci. 2017, 249, 37–52. [Google Scholar] [CrossRef]
- Loera-Valencia, R.; Neira, R.E.; Urbina, B.P.; Camacho, A.; Galindo, R.B. Evaluation of the Therapeutic Efficacy of Dressings with ZnO Nanoparticles in the Treatment of Diabetic Foot Ulcers. Biomed. Pharm. 2022, 155, 113708. [Google Scholar] [CrossRef]
- Cleetus, C.M.; Alvarez Primo, F.; Fregoso, G.; Lalitha Raveendran, N.; Noveron, J.C.; Spencer, C.T.; Ramana, C.V.; Joddar, B. Alginate Hydrogels with Embedded ZnO Nanoparticles for Wound Healing Therapy. Int. J. Nanomed. 2020, 15, 5097–5111. [Google Scholar] [CrossRef]
- Rahman, M.A.; Islam, M.S.; Haque, P.; Khan, M.N.; Takafuji, M.; Begum, M.; Chowdhury, G.W.; Khan, M.; Rahman, M.M. Calcium Ion Mediated Rapid Wound Healing by Nano-ZnO Doped Calcium Phosphate-Chitosan-Alginate Biocomposites. Materialia 2020, 13, 100839. [Google Scholar] [CrossRef]
- Nozari, M.; Gholizadeh, M.; Zahiri Oghani, F.; Tahvildari, K. Studies on Novel Chitosan/Alginate and Chitosan/Bentonite Flexible Films Incorporated with ZnO Nano Particles for Accelerating Dermal Burn Healing: In Vivo and in Vitro Evaluation. Int. J. Biol. Macromol. 2021, 184, 235–249. [Google Scholar] [CrossRef]
- Mohandas, A.; Pt, S.K.; Raja, B.; Lakshmanan, V.-K.; Jayakumar, R. Exploration of Alginate Hydrogel/Nano Zinc Oxide Composite Bandages for Infected Wounds. Int. J. Nanomed. 2015, 10, 53–66. [Google Scholar] [CrossRef] [Green Version]
- Zhang, M.; Qiao, X.; Han, W.; Jiang, T.; Liu, F.; Zhao, X. Alginate-Chitosan Oligosaccharide-ZnO Composite Hydrogel for Accelerating Wound Healing. Carbohydr. Polym. 2021, 266, 118100. [Google Scholar] [CrossRef]
- Arshad, R.; Sohail, M.F.; Sarwar, H.S.; Saeed, H.; Ali, I.; Akhtar, S.; Hussain, S.Z.; Afzal, I.; Jahan, S.; Anees-ur-Rehman; et al. ZnO-NPs Embedded Biodegradable Thiolated Bandage for Postoperative Surgical Site Infection: In Vitro and in Vivo Evaluation. PLoS ONE 2019, 14, e0217079. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, J.; Jiang, G.; Song, G.; Liu, T.; Cao, C.; Yang, Y.; Zhang, Y.; Hong, W. Incorporation of ZnO/Bioactive Glass Nanoparticles into Alginate/Chitosan Composite Hydrogels for Wound Closure. ACS Appl. Bio Mater. 2019, 2, 5042–5052. [Google Scholar] [CrossRef] [PubMed]
- Raguvaran, R.; Manuja, B.K.; Chopra, M.; Thakur, R.; Anand, T.; Kalia, A.; Manuja, A. Sodium Alginate and Gum Acacia Hydrogels of ZnO Nanoparticles Show Wound Healing Effect on Fibroblast Cells. Int. J. Biol. Macromol. 2017, 96, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Manuja, A.; Raguvaran, R.; Kumar, B.; Kalia, A.; Tripathi, B.N. Accelerated Healing of Full Thickness Excised Skin Wound in Rabbits Using Single Application of Alginate/Acacia Based Nanocomposites of ZnO Nanoparticles. Int. J. Biol. Macromol. 2020, 155, 823–833. [Google Scholar] [CrossRef] [PubMed]
- Buyana, B.; Aderibigbe, B.A.; Ndinteh, D.T.; Fonkui, Y.T.; Kumar, P. Alginate-Pluronic Topical Gels Loaded with Thymol, Norfloxacin and ZnO Nanoparticles as Potential Wound Dressings. J. Drug Deliv. Sci. Technol. 2020, 60, 101960. [Google Scholar] [CrossRef]
- Ndlovu, S.P.; Fonkui, T.Y.; Ndinteh, D.T.; Aderibigbe, B.A. Dissolvable Wound Dressing Loaded with Silver Nanoparticles Together with Ampicillin and Ciprofloxacin. Ther. Deliv. 2022, 13, 295–311. [Google Scholar] [CrossRef]
- Shalumon, K.T.; Anulekha, K.H.; Nair, S.V.; Nair, S.V.; Chennazhi, K.P.; Jayakumar, R. Sodium Alginate/Poly(Vinyl Alcohol)/Nano ZnO Composite Nanofibers for Antibacterial Wound Dressings. Int. J. Biol. Macromol. 2011, 49, 247–254. [Google Scholar] [CrossRef]
- Dodero, A.; Scarfi, S.; Pozzolini, M.; Vicini, S.; Alloisio, M.; Castellano, M. Alginate-Based Electrospun Membranes Containing ZnO Nanoparticles as Potential Wound Healing Patches: Biological, Mechanical, and Physicochemical Characterization. ACS Appl. Mater. Interfaces 2020, 12, 3371–3381. [Google Scholar] [CrossRef]
- Dodero, A.; Alloisio, M.; Castellano, M.; Vicini, S. Multilayer Alginate–Polycaprolactone Electrospun Membranes as Skin Wound Patches with Drug Delivery Abilities. ACS Appl. Mater. Interfaces 2020, 12, 31162–31171. [Google Scholar] [CrossRef]
- Gutierrez, E.; Burdiles, P.A.; Quero, F.; Palma, P.; Olate-Moya, F.; Palza, H. 3D Printing of Antimicrobial Alginate/Bacterial-Cellulose Composite Hydrogels by Incorporating Copper Nanostructures. ACS Biomater. Sci. Eng. 2019, 5, 6290–6299. [Google Scholar] [CrossRef] [PubMed]
- Maheswary, T.; Nurul, A.A.; Fauzi, M.B. The Insights of Microbes’ Roles in Wound Healing: A Comprehensive Review. Pharmaceutics 2021, 13, 981. [Google Scholar] [CrossRef] [PubMed]
- Punjataewakupt, A.; Napavichayanun, S.; Aramwit, P. The Downside of Antimicrobial Agents for Wound Healing. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 39–54. [Google Scholar] [CrossRef] [PubMed]
- Alzarea, A.I.; Alruwaili, N.K.; Ahmad, M.M.; Munir, M.U.; Butt, A.M.; Alrowaili, Z.A.; Shahari, M.S.B.; Almalki, Z.S.; Alqahtani, S.S.; Dolzhenko, A.V.; et al. Development and Characterization of Gentamicin-Loaded Arabinoxylan-Sodium Alginate Films as Antibacterial Wound Dressing. Int. J. Mol. Sci. 2022, 23, 2899. [Google Scholar] [CrossRef] [PubMed]
- Shahzad, A.; Khan, A.; Afzal, Z.; Umer, M.F.; Khan, J.; Khan, G.M. Formulation Development and Characterization of Cefazolin Nanoparticles-Loaded Cross-Linked Films of Sodium Alginate and Pectin as Wound Dressings. Int. J. Biol. Macromol. 2019, 124, 255–269. [Google Scholar] [CrossRef]
- Reczyńska-Kolman, K.; Hartman, K.; Kwiecień, K.; Brzychczy-Włoch, M.; Pamuła, E. Composites Based on Gellan Gum, Alginate and Nisin-Enriched Lipid Nanoparticles for the Treatment of Infected Wounds. Int. J. Mol. Sci. 2022, 23, 321. [Google Scholar] [CrossRef]
- Fan, Y.; Wu, W.; Lei, Y.; Gaucher, C.; Pei, S.; Zhang, J.; Xia, X. Edaravone-Loaded Alginate-Based Nanocomposite Hydrogel Accelerated Chronic Wound Healing in Diabetic Mice. Mar. Drugs 2019, 17, 285. [Google Scholar] [CrossRef] [Green Version]
- Atia, N.M.; Hazzah, H.A.; Gaafar, P.M.E.; Abdallah, O.Y. Diosmin Nanocrystal–Loaded Wafers for Treatment of Diabetic Ulcer: In Vitro and In Vivo Evaluation. J. Pharm. Sci. 2019, 108, 1857–1871. [Google Scholar] [CrossRef]
- Monou, P.K.; Mamaligka, A.M.; Tzimtzimis, E.K.; Tzetzis, D.; Vergkizi-Nikolakaki, S.; Vizirianakis, I.S.; Andriotis, E.G.; Eleftheriadis, G.K.; Fatouros, D.G. Fabrication and Preliminary In Vitro Evaluation of 3D-Printed Alginate Films with Cannabidiol (CBD) and Cannabigerol (CBG) Nanoparticles for Potential Wound-Healing Applications. Pharmaceutics 2022, 14, 1637. [Google Scholar] [CrossRef]
- Guadarrama-Acevedo, M.C.; Mendoza-Flores, R.A.; Del Prado-Audelo, M.L.; Urbán-Morlán, Z.; Giraldo-Gomez, D.M.; Magaña, J.J.; González-Torres, M.; Reyes-Hernández, O.D.; Figueroa-González, G.; Caballero-Florán, I.H.; et al. Development and Evaluation of Alginate Membranes with Curcumin-Loaded Nanoparticles for Potential Wound-Healing Applications. Pharmaceutics 2019, 11, 389. [Google Scholar] [CrossRef] [Green Version]
- Saygili, E.; Kaya, E.; Ilhan-Ayisigi, E.; Saglam-Metiner, P.; Alarcin, E.; Kazan, A.; Girgic, E.; Kim, Y.-W.; Gunes, K.; Eren-Ozcan, G.G.; et al. An Alginate-Poly(Acrylamide) Hydrogel with TGF-Β3 Loaded Nanoparticles for Cartilage Repair: Biodegradability, Biocompatibility and Protein Adsorption. Int. J. Biol. Macromol. 2021, 172, 381–393. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Guan, X.; Wu, Y.; Zhuang, S.; Wu, Y.; Du, L.; Zhao, J.; Rong, J.; Zhao, J.; Tu, M. An Alginate/Poly(N-Isopropylacrylamide)-Based Composite Hydrogel Dressing with Stepwise Delivery of Drug and Growth Factor for Wound Repair. Mater. Sci. Eng. C 2020, 115, 111123. [Google Scholar] [CrossRef]
- Mihai, M.M.; Dima, M.B.; Dima, B.; Holban, A.M. Nanomaterials for Wound Healing and Infection Control. Materials 2019, 12, 2176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pacho, M.N.; Manzano, V.E.; D’Accorso, N.B. Chapter 16—Synthesis of Micro- and Nanoparticles of Alginate and Chitosan for Controlled Release of Drugs. In Natural Polysaccharides in Drug Delivery and Biomedical Applications; Hasnain, M.S., Nayak, A.K., Eds.; Academic Press: Cambridge, MA, USA, 2019; pp. 363–398. ISBN 978-0-12-817055-7. [Google Scholar]
- Del Gaudio, P.; Amante, C.; Civale, R.; Bizzarro, V.; Petrella, A.; Pepe, G.; Campiglia, P.; Russo, P.; Aquino, R.P. In Situ Gelling Alginate-Pectin Blend Particles Loaded with Ac2-26: A New Weapon to Improve Wound Care Armamentarium. Carbohydr. Polym. 2020, 227, 115305. [Google Scholar] [CrossRef]
- Oliveira, D.M.L.; Rezende, P.S.; Barbosa, T.C.; Andrade, L.N.; Bani, C.; Tavares, D.S.; da Silva, C.F.; Chaud, M.V.; Padilha, F.; Cano, A.; et al. Double Membrane Based on Lidocaine-Coated Polymyxin-Alginate Nanoparticles for Wound Healing: In Vitro Characterization and in Vivo Tissue Repair. Int. J. Pharm. 2020, 591, 120001. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Zhang, Q.; Wang, Z.; Xu, Y.; Tao, Q.; Wang, J.; Kong, X.; Sheng, K.; Wang, Y. Investigation of Construction and Characterization of Carboxymethyl Chitosan—Sodium Alginate Nanoparticles to Stabilize Pickering Emulsion Hydrogels for Curcumin Encapsulation and Accelerating Wound Healing. Int. J. Biol. Macromol. 2022, 209, 1837–1847. [Google Scholar] [CrossRef]
- Sheir, M.M.; Nasra, M.M.A.; Abdallah, O.Y. Chitosan Alginate Nanoparticles as a Platform for the Treatment of Diabetic and Non-Diabetic Pressure Ulcers: Formulation and in Vitro/in Vivo Evaluation. Int. J. Pharm. 2021, 607, 120963. [Google Scholar] [CrossRef] [PubMed]
- Montaser, A.S.; Abdel-Mohsen, A.M.; Ramadan, M.A.; Sleem, A.A.; Sahffie, N.M.; Jancar, J.; Hebeish, A. Preparation and Characterization of Alginate/Silver/Nicotinamide Nanocomposites for Treating Diabetic Wounds. Int. J. Biol. Macromol. 2016, 92, 739–747. [Google Scholar] [CrossRef]
- Maatouk, B.; Jaffa, M.A.; Karam, M.; Fahs, D.; Nour-Eldine, W.; Hasan, A.; Jaffa, A.A.; Mhanna, R. Sulfated Alginate/Polycaprolactone Double-Emulsion Nanoparticles for Enhanced Delivery of Heparin-Binding Growth Factors in Wound Healing Applications. Colloids Surf. B Biointerfaces 2021, 208, 112105. [Google Scholar] [CrossRef] [PubMed]
- Hosny, A.E.-D.M.; Rasmy, S.A.; Aboul-Magd, D.S.; Kashef, M.T.; El-Bazza, Z.E. The Increasing Threat of Silver-Resistance in Clinical Isolates from Wounds and Burns. Infect. Drug. Resist. 2019, 12, 1985–2001. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Percival, S.L.; Salisbury, A.-M.; Chen, R. Silver, Biofilms and Wounds: Resistance Revisited. Crit. Rev. Microbiol. 2019, 45, 223–237. [Google Scholar] [CrossRef] [PubMed]
- Catanzano, O.; Quaglia, F.; Boateng, J.S. Wound Dressings as Growth Factor Delivery Platforms for Chronic Wound Healing. Expert. Opin. Drug. Deliv. 2021, 18, 737–759. [Google Scholar] [CrossRef] [PubMed]
- Bierhalz, A.C.K.; Moraes, Â.M. Composite Membranes of Alginate and Chitosan Reinforced with Cotton or Linen Fibers Incorporating Epidermal Growth Factor. Mater. Sci. Eng. C 2017, 76, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.-Y.; Huang, Y.-C. Basic Fibroblast Growth Factor Released from Fucoidan-Modified Chitosan/Alginate Scaffolds for Promoting Fibroblasts Migration. J. Polym. Res. 2018, 25, 83. [Google Scholar] [CrossRef]
- Mohammadi, S.; Ramakrishna, S.; Laurent, S.; Shokrgozar, M.A.; Semnani, D.; Sadeghi, D.; Bonakdar, S.; Akbari, M. Fabrication of Nanofibrous PVA/Alginate-Sulfate Substrates for Growth Factor Delivery. J. Biomed. Mater. Res. Part A 2019, 107, 403–413. [Google Scholar] [CrossRef]
- McCarthy, S.; Dvorakova, V.; O’Sullivan, P.; Bourke, J.F. Anaphylaxis Caused by Alginate Dressing. Contact Dermat. 2018, 79, 396–397. [Google Scholar] [CrossRef]
- Ionita, M.; Pandele, M.A.; Iovu, H. Sodium Alginate/Graphene Oxide Composite Films with Enhanced Thermal and Mechanical Properties. Carbohydr. Polym. 2013, 94, 339–344. [Google Scholar] [CrossRef]
- Song, J.-L.; Fu, X.-Y.; Raza, A.; Shen, N.-A.; Xue, Y.-Q.; Wang, H.-J.; Wang, J.-Y. Enhancement of Mechanical Strength of TCP-Alginate Based Bioprinted Constructs. J. Mech. Behav. Biomed. Mater. 2020, 103, 103533. [Google Scholar] [CrossRef]
- Stoppel, W.L.; White, J.C.; Horava, S.D.; Henry, A.C.; Roberts, S.C.; Bhatia, S.R. Terminal Sterilization of Alginate Hydrogels: Efficacy and Impact on Mechanical Properties. J. Biomed. Mater. Res. Part B Appl. Biomater. 2014, 102, 877–884. [Google Scholar] [CrossRef]
- Fu, P.-S.; Wang, J.-C.; Lai, P.-L.; Liu, S.-M.; Chen, Y.-S.; Chen, W.-C.; Hung, C.-C. Effects of Gamma Radiation on the Sterility Assurance, Antibacterial Ability, and Biocompatibility of Impregnated Hydrogel Macrosphere Protein and Drug Release. Polymers 2021, 13, 938. [Google Scholar] [CrossRef]
- Mollah, M.Z.I.; Rahaman, M.S.; Faruque, M.R.I.; Khandaker, M.U.; Osman, H.; Alamri, S.; Al-Assaf, S. Effects of Radiation Sterilization Dose on the Molecular Weight and Gelling Properties of Commercial Alginate Samples. Front. Mater. 2021, 8, 761995. [Google Scholar] [CrossRef]
- Bernhardt, A.; Wehrl, M.; Paul, B.; Hochmuth, T.; Schumacher, M.; Schütz, K.; Gelinsky, M. Improved Sterilization of Sensitive Biomaterials with Supercritical Carbon Dioxide at Low Temperature. PLoS ONE 2015, 10, e0129205. [Google Scholar] [CrossRef] [PubMed] [Green Version]













| Brand Name | Manufacturer | Composition | Applications | Reference |
|---|---|---|---|---|
| Biatain® Alginate | Coloplast (Humlebaek, Denmark) | Alginate (85%), CMC 1 | Moderate to heavily exuding wounds | [20] |
| Biatain® Alginate Ag | Alginate, CMC, ionic silver complex | Moderate to heavily exuding wounds, infected wounds | [21] | |
| Comfeel® Plus Ulcer | CMC particles, alginate (as an additive), polyurethane semipermeable film | Low to moderately exuding wounds | [22] | |
| Kaltostat® | ConvaTec (Reading, UK) | Calcium sodium alginate | Moderate to heavily exuding wounds | [23] |
| CarboFlex® | Five-layer dressing with alginate absorbent layer, internal charcoal layer, and water-resistant top | Malodorous wounds | [24] | |
| Tegaderm™ Alginate | 3M™ (Saint Paul, MN, USA) | Calcium alginate | Moderate to heavily exuding wounds | [25] |
| Sorbalgon® | Hartmann (Heidenheim, Germany) | Calcium alginate | Moderate to heavily exuding wounds | [26] |
| Sorbalgon® Ag | Calcium alginate, silver | Moderate to heavily exuding wounds, infected wounds | [27] |
| Dressing Type | Properties | Examples |
|---|---|---|
| Semipermeable films |
|
|
| Semipermeable foams |
|
|
| Hydrogel dressings |
|
|
| Hydrocolloid dressings |
|
|
| Alginate dressings |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Froelich, A.; Jakubowska, E.; Wojtyłko, M.; Jadach, B.; Gackowski, M.; Gadziński, P.; Napierała, O.; Ravliv, Y.; Osmałek, T. Alginate-Based Materials Loaded with Nanoparticles in Wound Healing. Pharmaceutics 2023, 15, 1142. https://doi.org/10.3390/pharmaceutics15041142
Froelich A, Jakubowska E, Wojtyłko M, Jadach B, Gackowski M, Gadziński P, Napierała O, Ravliv Y, Osmałek T. Alginate-Based Materials Loaded with Nanoparticles in Wound Healing. Pharmaceutics. 2023; 15(4):1142. https://doi.org/10.3390/pharmaceutics15041142
Chicago/Turabian StyleFroelich, Anna, Emilia Jakubowska, Monika Wojtyłko, Barbara Jadach, Michał Gackowski, Piotr Gadziński, Olga Napierała, Yulia Ravliv, and Tomasz Osmałek. 2023. "Alginate-Based Materials Loaded with Nanoparticles in Wound Healing" Pharmaceutics 15, no. 4: 1142. https://doi.org/10.3390/pharmaceutics15041142
APA StyleFroelich, A., Jakubowska, E., Wojtyłko, M., Jadach, B., Gackowski, M., Gadziński, P., Napierała, O., Ravliv, Y., & Osmałek, T. (2023). Alginate-Based Materials Loaded with Nanoparticles in Wound Healing. Pharmaceutics, 15(4), 1142. https://doi.org/10.3390/pharmaceutics15041142