Toward a New Generation of Bio-Scaffolds for Neural Tissue Engineering: Challenges and Perspectives
Abstract
:1. Introduction
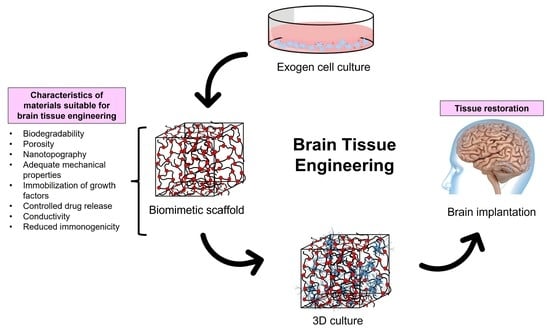
2. The Challenge of Designing Materials for Neuron Tissue Engineering
3. Main Requirements for Scaffolds for Brain Tissue Engineering
3.1. Biocompatibility and Biodegradability
3.2. Mechanical Properties
3.3. Topography
3.4. Porosity
3.5. Immobilization of Active Substances
3.6. Conductivity
4. Materials and Techniques Commonly Used for the Fabrication of Bioscaffolds for Neural Tissue Engineering
5. Future Perspectives
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Material | Origin | Characteristics | Applications | References |
|---|---|---|---|---|
| Alginate | Natural | Hydrogel-based biodegradable scaffold. | Axonal regeneration. | [138] |
| Cellulose | Natural | Hydrogel | Tissue repair, stem cell therapy, anti-inflammatory drug delivery. | [139] |
| Chitosan | Natural | Hydrogel-based biodegradable scaffold. | Restoration of cell function, axonal regeneration, drugs, and neurotrophic factor release. | [140,141,142] |
| Collagen | Natural | Hydrogel-based biodegradable scaffold. | Cell survival and proliferation, tissue repair, restoration of cell function, growth factors release, axonal regeneration, and stem cell therapy. To date, this is the only material in clinical trials used for neural tissue engineering. | [143,144] |
| Nanopeptide hydrogel | Natural | Hydrogel-based biodegradable scaffold. | Cell survival and proliferation, tissue repair, restoration of cell function, angiogenesis. | [145] |
| Gelatin | Natural | Hydrogel-based biodegradable scaffold. | Cell survival, proliferation, blood–brain barrier restoration, tissue repair, anti-inflammatory properties, and stem cell therapy. | [146,147,148] |
| HA | Natural | Hydrogel | Cell survival; axonal regeneration, growth factor release; stem cell therapy; promotion of glial, neuronal, or immature/progenitor states; vascularization. | [88,149,150] |
| Xyloglucan | Natural | Hydrogel | Axonal regeneration, tissue repair, stem cell survival. | [151] |
| PVA | Synthetic | Hydrogel-based scaffold. | Cell survival and proliferation, controlled drug release. | [152] |
| PCL | Synthetic | Hydrogel-based biodegradable scaffold. | Axonal regeneration, cell survival, restoration of cell function, neurotrophic factors release, stem cell therapy. | [132,153] |
| PEG | Synthetic | Hydrogel-based biodegradable scaffold. | Axonal regeneration, reduced microglia and astrocyte response; and neurotrophic factor release. | [154,155] |
| PHEMA | Synthetic | Hydrogel-based scaffold. | Axonal regeneration, cell survival, growth factor release. | [156] |
| PHMA | Synthetic | Hydrogel | Axonal regeneration, anti-inflammatory properties. | [157] |
| PLGA | Synthetic | Hydrogel-based biodegradable scaffold. | Axonal regeneration, vascularization, tissue repair. | [158] |
| Polyurethan | Synthetic | Hydrogel-based biodegradable scaffold. | Axonal regeneration, cell survival, cell function restoration, and stem cell therapy. | [107,159,160] |
| PuraMatrix® | Synthetic | Hydrogel-based biodegradable scaffold. | Stem cell therapy. | [161] |
| Ppy | Synthetic | Conductive scaffold | Axonal regeneration, cell proliferation, drug release, electrical stimulation. | [162,163] |
| PANi | Synthetic | Conductive scaffold | Axonal regeneration, cell proliferation, drug release, electrical stimulation. | [164] |
| PEDOT | Synthetic | Conductive scaffold | Axonal regeneration, cell proliferation, drug release, electrical stimulation, and recording. | [129,165] |
Appendix B
| Fabrication Method | Principle | Pros | Cons | Examples of Materials | References |
|---|---|---|---|---|---|
| Electrospinning | Electrospinning uses electricity and fluid dynamics to create fibers. It starts by electrifying a liquid droplet, which then forms a jet. This jet is then stretched and elongated to produce one or more fibers. | *Wide material choice. *Nanofibrous architecture that offers benefits for cells. *Simplicity. | *Poor scalability. *Low reproducibility. *Difficulties in creating 3D scaffolds with well-defined pore architecture. *No shapes other than cylinders and sheets are possible. | PLGA, PCL, PEO, PVA, collagen, gelatin, chitosan, silk protein, fibrinogen. | [166,167] |
| Solvent casting | Solvent casting utilizes the evaporation of certain solvents to create scaffolds in a mold. | *Simple procedure. *Pore size can be controlled using appropriate molds. *Easy incorporation of drugs into the scaffold. | *Use of highly toxic solvents. *Poor pore interconnectivity. | PCL, PLA. | [168] |
| Soft lithography | Soft lithography is a collection of techniques that involve fabricating or replicating structures using elastomeric stamps, molds, and conformable photomasks. | *Low cost. *High biocompatibility. *High resolution (5 to 100 nm). | *The resolution can be reduced by the diffusion of ink. | GPS, PMMA, soft-gel materials. | [169,170] |
| Electrospray | Electrospray uses a conductive solvent to create micro and nanoparticles from a polymer solution. Unlike electrospinning, the size and shape of the particles produced can be controlled by adjusting factors such as concentration, solvent choice, and viscosity. | *Wide material choice. *Formation of homogeneous nanoparticles. *Simplicity. *Nanoparticles with high loading capacity. | *Poor scalability. *No shapes other than nano and microspheres. | Chitosan. | [171] |
| Porogen leaching | Porogen leaching entails casting a solution of polymer and porogen into a mold, drying the mixture, evaporating the solvent, and then leaching the embedded porogen with water to create pores. | *Control over porosity and pore geometry. *Low-cost. | *Inadequate pore size and interconnectivity. | PLA, alginate, gelatin. | [172] |
| Self-assembly | A natural arrangement of molecules, where disordered entities organize into ordered structures due to specific interactions (van der Waals forces, hydrophobic, electrostatic, hydrogen bonding, π–π aromatic stacking, metal coordination, etc.) among the components. | *Control over porosity and fiber diameter. *Regular structures are obtained. *Simple and versatile strategy. *Mimics natural structures. | *Minimal control over the shape. *Limited use of materials. | Silk, liposomes, VLP, DNA. | [173,174] |
| Bioprinting | Bioprinting is an additive manufacturing technique involving layer-by-layer printing of living cells using bioinks. This process aims to create structures that mimic the behavior and structures found in natural tissues. | *Offers flexibility, customization, scalability, reliability, durability, and relatively high speed. *Enables the design of both 2D and 3D structures. | *Expensive *Limited cell viability.*Poor reproducibility and scalability. *It is challenging to recreate the intricate microarchitecture and vascular networks. | PCL, PLA, PLGA, PEO/PBT, pluronic, GelMA, HA, PVA. | [175] |
| Microcontact printing | Microcontact printing involves creating a stamp or mold with the desired pattern or features on its surface. The stamp is then inked or coated with a material, such as an ink or self-assembled monolayer, which can adhere to the substrate. | *Enables the patterning of proteins of interest on substrates. *Low-cost. | *Poor reproducibility and scalability. *It is not possible to print different molecules with one stamp. *It is difficult to control the amount of protein transferred. | PVA, polyacrylamide, GelMA, graphene. | [176] |
| Gas foaming | Gas foaming utilizes gas, such as carbon dioxide, as a porogen instead of a solvent. | *Generates highly porous scaffolds. *Low-cost. *Eliminaes the need for harsh chemical solvents. | *Limited mechanical properties. *Inadequate pore interconnectivity. *Poor control of pore size. | PLGA, PEG. | [177,178] |
References
- Pina, S.; Ribeiro, V.P.; Marques, C.F.; Maia, F.R.; Silva, T.H.; Reis, R.L.; Oliveira, J.M. Scaffolding Strategies for Tissue Engineering and Regenerative Medicine Applications. Materials 2019, 12, 1824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilmour, G.S.; Nielsen, G.; Teodoro, T.; Yogarajah, M.; Coebergh, J.A.; Dilley, M.D.; Martino, D.; Edwards, M.J. Management of functional neurological disorder. J. Neurol. 2020, 267, 2164–2172. [Google Scholar] [CrossRef] [Green Version]
- Dehqan Niri, A.; Karimi Zarchi, A.A.; Ghadiri Harati, P.; Salimi, A.; Mujokoro, B. Tissue engineering scaffolds in the treatment of brain disorders in geriatric patients. Artif. Organs. 2019, 43, 947–960. [Google Scholar] [CrossRef] [PubMed]
- Martinez, B.; Peplow, P.V. Biomaterial and tissue-engineering strategies for the treatment of brain neurodegeneration. Neural Regen. Res. 2022, 17, 2108–2116. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhou, L.; Zhang, W. Control of scaffold degradation in tissue engineering: A review. Tissue Eng. Part B Rev. 2014, 20, 492–502. [Google Scholar] [CrossRef]
- Shafiee, A.; Atala, A. Tissue Engineering: Toward a New Era of Medicine. Annu. Rev. Med. 2017, 68, 29–40. [Google Scholar] [CrossRef]
- Echeverria Molina, M.I.; Malollari, K.G.; Komvopoulos, K. Design Challenges in Polymeric Scaffolds for Tissue Engineering. Front. Bioeng. Biotechnol. 2021, 9, 617141. [Google Scholar] [CrossRef]
- Peressotti, S.; Koehl, G.E.; Goding, J.A.; Green, R.A. Self-Assembling Hydrogel Structures for Neural Tissue Repair. ACS Biomater. Sci. Eng. 2021, 7, 4136–4163. [Google Scholar] [CrossRef]
- Ballios, B.G.; Cooke, M.J.; Donaldson, L.; Coles, B.L.; Morshead, C.M.; van der Kooy, D.; Shoichet, M.S. A Hyaluronan-Based Injectable Hydrogel Improves the Survival and Integration of Stem Cell Progeny following Transplantation. Stem Cell Rep. 2015, 4, 1031–1045. [Google Scholar] [CrossRef] [Green Version]
- Adil, M.M.; Vazin, T.; Ananthanarayanan, B.; Rodrigues, G.M.C.; Rao, A.T.; Kulkarni, R.U.; Miller, E.W.; Kumar, S.; Schaffer, D.V. Engineered hydrogels increase the post-transplantation survival of encapsulated hESC-derived midbrain dopaminergic neurons. Biomaterials 2017, 136, 1–11. [Google Scholar] [CrossRef]
- Marcus, M.; Baranes, K.; Park, M.; Choi, I.S.; Kang, K.; Shefi, O. Interactions of Neurons with Physical Environments. Adv. Healthc. Mater. 2017, 6, 1700267. [Google Scholar] [CrossRef] [Green Version]
- Burdick, J.A.; Mauck, R.L.; Gerecht, S. To Serve and Protect: Hydrogels to Improve Stem Cell-Based Therapies. Cell Stem Cell. 2016, 18, 13–15. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.M.; Olanrele, O.S.; Zhang, X.; Hsu, C.C. Fabrication of Hydrogel Materials for Biomedical Applications. Adv. Exp. Med. Biol. 2018, 1077, 197–224. [Google Scholar] [CrossRef]
- Mirzaei, S.; Kulkarni, K.; Zhou, K.; Crack, P.J.; Aguilar, M.I.; Finkelstein, D.I.; Forsythe, J.S. Biomaterial Strategies for Restorative Therapies in Parkinson’s Disease. ACS Chem. Neurosci. 2021, 12, 4224–4235. [Google Scholar] [CrossRef]
- Guo, W.; Qiu, J.; Liu, J.; Liu, H. Graphene microfiber as a scaffold for regulation of neural stem cells differentiation. Sci. Rep. 2017, 7, 5678. [Google Scholar] [CrossRef]
- Vashist, A.; Kaushik, A.; Vashist, A.; Sagar, V.; Ghosal, A.; Gupta, Y.K.; Ahmad, S.; Nair, M. Advances in Carbon Nanotubes-Hydrogel Hybrids in Nanomedicine for Therapeutics. Adv. Healthc. Mater. 2018, 7, e1701213. [Google Scholar] [CrossRef]
- Sang, S.; Cheng, R.; Cao, Y.; Yan, Y.; Shen, Z.; Zhao, Y.; Han, Y. Biocompatible chitosan/polyethylene glycol/multi-walled carbon nanotube composite scaffolds for neural tissue engineering. J. Zhejiang Univ. Sci. B 2022, 23, 58–73. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, J.; Shi, X.; Zhu, Z.; Chen, P.; Peng, H. Electronic Neurons for a New Learning Paradigm. Adv. Healthc. Mater. 2023, 28, e2203247. [Google Scholar] [CrossRef]
- Al-Hadeethi, Y.; Nagarajan, A.; Hanuman, S.; Mohammed, H.; Vetekar, A.M.; Thakur, G.; Dinh, L.N.M.; Yao, Y.; Mkawi, E.M.; Hussein, M.A.; et al. Schwann cell-matrix coated PCL-MWCNT multifunctional nanofibrous scaffolds for neural regeneration. RSC Adv. 2023, 13, 1392–1401. [Google Scholar] [CrossRef]
- Cheng, Y.; Chen, Z.; Yang, S.; Liu, T.; Yin, L.; Pu, Y.; Liang, G. Nanomaterials-induced toxicity on cardiac myocytes and tissues, and emerging toxicity assessment techniques. Sci. Total Environ. 2021, 800, 149584. [Google Scholar] [CrossRef]
- Witkowska, M.; Florek, E.; Mrówczyński, R. Assessment of Pristine Carbon Nanotubes Toxicity in Rodent Models. Int. J. Mol. Sci. 2022, 23, 15343. [Google Scholar] [CrossRef] [PubMed]
- Lazăr, A.I.; Aghasoleimani, K.; Semertsidou, A.; Vyas, J.; Roșca, A.L.; Ficai, D.; Ficai, A. Graphene-Related Nanomaterials for Biomedical Applications. Nanomaterials 2023, 13, 1092. [Google Scholar] [CrossRef] [PubMed]
- Halim, A.; Qu, K.Y.; Zhang, X.F.; Huang, N.P. Recent Advances in the Application of Two-Dimensional Nanomaterials for Neural Tissue Engineering and Regeneration. ACS Biomater. Sci. Eng. 2021, 7, 3503–3529. [Google Scholar] [CrossRef] [PubMed]
- Zamproni, L.N.; Mundim, M.T.V.V.; Porcionatto, M.A. Neurorepair and Regeneration of the Brain: A Decade of Bioscaffolds and Engineered Microtissue. Front. Cell Dev. Biol. 2021, 9, 649891. [Google Scholar] [CrossRef]
- Rantataro, S.; Parkkinen, I.; Pande, I.; Domanskyi, A.; Airavaara, M.; Peltola, E.; Laurila, T. Nanoscale geometry determines mechanical biocompatibility of vertically aligned nanofibers. Acta Biomater. 2022, 146, 235–247. [Google Scholar] [CrossRef]
- Khan, F.; Tanaka, M. Designing Smart Biomaterials for Tissue Engineering. Int. J. Mol. Sci. 2017, 19, 17. [Google Scholar] [CrossRef] [Green Version]
- Salatino, J.W.; Ludwig, K.A.; Kozai, T.D.Y.; Purcell, E.K. Glial responses to implanted electrodes in the brain. Nat. Biomed. Eng. 2017, 1, 862–877. [Google Scholar] [CrossRef]
- Biran, R.; Martin, D.C.; Tresco, P.A. Neuronal cell loss accompanies the brain tissue response to chronically implanted silicon microelectrode arrays. Exp. Neurol. 2005, 195, 115–126. [Google Scholar] [CrossRef]
- McConnell, G.C.; Rees, H.D.; Levey, A.I.; Gutekunst, C.A.; Gross, R.E.; Bellamkonda, R.V. Implanted neural electrodes cause chronic, local inflammation that is correlated with local neurodegeneration. J. Neural. Eng. 2009, 6, 056003. [Google Scholar] [CrossRef]
- Kozai, T.D.; Gugel, Z.; Li, X.; Gilgunn, P.J.; Khilwani, R.; Ozdoganlar, O.B.; Fedder, G.K.; Weber, D.J.; Cui, X.T. Chronic tissue response to carboxymethyl cellulose based dissolvable insertion needle for ultra-small neural probes. Biomaterials 2014, 35, 9255–9268. [Google Scholar] [CrossRef]
- Lee, W.H.; Cha, G.D.; Kim, D.H. Flexible and biodegradable electronic implants for diagnosis and treatment of brain diseases. Curr. Opin. Biotechnol. 2021, 72, 13–21. [Google Scholar] [CrossRef]
- Kaurav, H.; Kapoor, D.N. Implantable systems for drug delivery to the brain. Ther. Deliv. 2017, 8, 1097–1107. [Google Scholar] [CrossRef]
- Caliari, S.R.; Burdick, J.A. A practical guide to hydrogels for cell culture. Nat. Methods 2016, 13, 405–414. [Google Scholar] [CrossRef] [Green Version]
- Xia, T.; Liu, W.; Yang, L. A review of gradient stiffness hydrogels used in tissue engineering and regenerative medicine. J. Biomed. Mater. Res. A 2017, 105, 1799–1812. [Google Scholar] [CrossRef]
- Tusan, C.G.; Man, Y.H.; Zarkoob, H.; Johnston, D.A.; Andriotis, O.G.; Thurner, P.J.; Yang, S.; Sander, E.A.; Gentleman, E.; Sengers, B.G.; et al. Collective Cell Behavior in Mechanosensing of Substrate Thickness. Biophys. J. 2018, 114, 2743–2755. [Google Scholar] [CrossRef] [Green Version]
- Robinson, M.; Valente, K.P.; Willerth, S.M. A Novel Toolkit for Characterizing the Mechanical and Electrical Properties of Engineered Neural Tissues. Biosensors 2019, 9, 51. [Google Scholar] [CrossRef] [Green Version]
- Aregueta-Robles, U.A.; Martens, P.J.; Poole-Warren, L.A.; Green, R.A. Tissue engineered hydrogels supporting 3D neural networks. Acta Biomater. 2019, 95, 269–284. [Google Scholar] [CrossRef]
- Rosso, G.; Wehner, D.; Schweitzer, C.; Möllmert, S.; Sock, E.; Guck, J.; Shahin, V. Matrix stiffness mechanosensing modulates the expression and distribution of transcription factors in Schwann cells. Bioeng. Transl. Med. 2021, 7, e10257. [Google Scholar] [CrossRef]
- Zhu, J.; Marchant, R.E. Design properties of hydrogel tissue-engineering scaffolds. Expert Rev. Med. Devices 2011, 8, 607–626. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, K.; Gu, X.; Leong, K.W. Biophysical Regulation of Cell Behavior-Cross Talk between Substrate Stiffness and Nanotopography. Engineering 2017, 3, 36–54. [Google Scholar] [CrossRef]
- Marinval, N.; Chew, S.Y. Mechanotransduction assays for neural regeneration strategies: A focus on glial cells. APL Bioeng. 2021, 5, 021505. [Google Scholar] [CrossRef] [PubMed]
- Georges, P.C.; Miller, W.J.; Meaney, D.F.; Sawyer, E.S.; Janmey, P.A. Matrices with compliance comparable to that of brain tissue select neuronal over glial growth in mixed cortical cultures. Biophys. J. 2006, 90, 3012–3018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, L.; Wang, K.; Li, Y.; Yang, Y. Nanotopography promoted neuronal differentiation of human induced pluripotent stem cells. Colloids Surf. B Biointerfaces 2016, 48, 49–58. [Google Scholar] [CrossRef]
- Seo, J.; Kim, J.; Joo, S.; Choi, J.Y.; Kang, K.; Cho, W.K.; Choi, I.S. Nanotopography-Promoted Formation of Axon Collateral Branches of Hippocampal Neurons. Small 2018, 20, e1801763. [Google Scholar] [CrossRef] [PubMed]
- Fischer, R.S.; Lam, P.Y.; Huttenlocher, A.; Waterman, C.M. Filopodia and focal adhesions: An integrated system driving branching morphogenesis in neuronal pathfinding and angiogenesis. Dev. Biol. 2019, 451, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Leclech, C.; Barakat, A.I. Is there a universal mechanism of cell alignment in response to substrate topography? Cytoskeleton 2021, 78, 284–292. [Google Scholar] [CrossRef]
- Park, S.; Kim, D.; Park, S.; Kim, S.; Lee, D.; Kim, W.; Kim, J. Nanopatterned Scaffolds for Neural Tissue Engineering and Regenerative Medicine. Adv. Exp. Med. Biol. 2018, 1078, 421–443. [Google Scholar] [CrossRef]
- Schnell, E.; Klinkhammer, K.; Balzer, S.; Brook, G.; Klee, D.; Dalton, P.; Mey, J. Guidance of glial cell migration and axonal growth on electrospun nanofibers of poly-epsilon-caprolactone and a collagen/poly-epsilon-caprolactone blend. Biomaterials 2007, 28, 3012–3025. [Google Scholar] [CrossRef]
- Jang, M.J.; Namgung, S.; Hong, S.; Nam, Y. Directional neurite growth using carbon nanotube patterned substrates as a biomimetic cue. Nanotechnology 2010, 21, 235102. [Google Scholar] [CrossRef]
- Ferrari, A.; Cecchini, M.; Dhawan, A.; Micera, S.; Tonazzini, I.; Stabile, R.; Pisignano, D.; Beltram, F. Nanotopographic control of neuronal polarity. Nano Lett. 2011, 11, 505–511. [Google Scholar] [CrossRef]
- Fan, L.; Feng, C.; Zhao, W.; Qian, L.; Wang, Y.; Li, Y. Directional neurite outgrowth on superaligned carbon nanotube yarn patterned substrate. Nano Lett. 2012, 12, 3668–3673. [Google Scholar] [CrossRef]
- Krishna, L.; Dhamodaran, K.; Jayadev, C.; Chatterjee, K.; Shetty, R.; Khora, S.S.; Das, D. Nanostructured scaffold as a determinant of stem cell fate. Stem Cell Res. Ther. 2016, 7, 188. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.J.; Zhu, W.; Nowicki, M.; Lee, G.; Heo, D.N.; Kim, J.; Zuo, Y.Y.; Zhang, L.G. 3D printing nano conductive multi-walled carbon nanotube scaffolds for nerve regeneration. J. Neural. Eng. 2018, 15, 016018. [Google Scholar] [CrossRef]
- Wang, L.; Wu, Y.; Hu, T.; Ma, P.X.; Guo, B. Aligned conductive core-shell biomimetic scaffolds based on nanofiber yarns/hydrogel for enhanced 3D neurite outgrowth alignment and elongation. Acta Biomater. 2019, 96, 175–187. [Google Scholar] [CrossRef]
- Moslehi, S.; Rowland, C.; Smith, J.H.; Griffiths, W.; Watterson, W.J.; Niell, C.M.; Alemán, B.J.; Perez, M.T.; Taylor, R.P. Comparison of fractal and grid electrodes for studying the effects of spatial confinement on dissociated retinal neuronal and glial behavior. Sci. Rep. 2022, 12, 17513. [Google Scholar] [CrossRef]
- Haq, F.; Anandan, V.; Keith, C.; Zhang, G. Neurite development in PC12 cells cultured on nanopillars and nanopores with sizes comparable with filopodia. Int. J. Nanomed. 2007, 2, 107–115. [Google Scholar] [CrossRef]
- Hoffman-Kim, D.; Mitchel, J.A.; Bellamkonda, R.V. Topography, cell response, and nerve regeneration. Annu. Rev. Biomed. Eng. 2010, 12, 203–231. [Google Scholar] [CrossRef] [Green Version]
- Leclech, C.; Villard, C. Cellular and Subcellular Contact Guidance on Microfabricated Substrates. Front. Bioeng. Biotechnol. 2020, 8, 551505. [Google Scholar] [CrossRef]
- Villard, C. Spatial confinement: A spur for axonal growth. Semin. Cell Dev. Biol. 2023, 140, 54–62. [Google Scholar] [CrossRef]
- Onesto, V.; Cancedda, L.; Coluccio, M.L.; Nanni, M.; Pesce, M.; Malara, N.; Cesarelli, M.; Di Fabrizio, E.; Amato, F.; Gentile, F. Nano-topography Enhances Communication in Neural Cells Networks. Sci. Rep. 2017, 7, 9841. [Google Scholar] [CrossRef] [Green Version]
- Amores de Sousa, M.C.; Rodrigues, C.A.V.; Ferreira, I.A.F.; Diogo, M.M.; Linhardt, R.J.; Cabral, J.M.S.; Ferreira, F.C. Functionalization of Electrospun Nanofibers and Fiber Alignment Enhance Neural Stem Cell Proliferation and Neuronal Differentiation. Front. Bioeng. Biotechnol. 2020, 8, 580135. [Google Scholar] [CrossRef] [PubMed]
- Shan, D.; Ma, C.; Yang, J. Enabling biodegradable functional biomaterials for the management of neurological disorders. Adv. Drug Deliv. Rev. 2019, 148, 219–238. [Google Scholar] [CrossRef] [PubMed]
- Jorfi, M.; Skousen, J.L.; Weder, C.; Capadona, J.R. Progress towards biocompatible intracortical microelectrodes for neural interfacing applications. J. Neural. Eng. 2015, 12, 011001. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Amato, A.R.; Puhl, D.L.; Ziemba, A.M.; Johnson, C.D.L.; Doedee, J.; Bao, J.; Gilbert, R.J. Exploring the effects of electrospun fiber surface nanotopography on neurite outgrowth and branching in neuron cultures. PLoS ONE 2019, 14, e0211731. [Google Scholar] [CrossRef] [Green Version]
- Miller, R.J.; Chan, C.Y.; Rastogi, A.; Grant, A.M.; White, C.M.; Bette, N.; Schaub, N.J.; Corey, J.M. Combining electrospun nanofibers with cell-encapsulating hydrogel fibers for neural tissue engineering. J. Biomater. Sci. Polym. Ed. 2018, 29, 1625–1642. [Google Scholar] [CrossRef]
- Mai, P.; Hampl, J.; Baca, M.; Brauer, D.; Singh, S.; Weise, F.; Borowiec, J.; Schmidt, A.; Küstner, J.M.; Klett, M.; et al. MatriGrid® Based Biological Morphologies: Tools for 3D Cell Culturing. Bioengineering 2022, 9, 220. [Google Scholar] [CrossRef]
- Shi, M.; Xu, Q.; Ding, L.; Xia, Y.; Zhang, C.; Lai, H.; Liu, C.; Deng, D.Y.B. Cell Infiltrative Inner Connected Porous Hydrogel Improves Neural Stem Cell Migration and Differentiation for Functional Repair of Spinal Cord Injury. ACS Biomater. Sci. Eng. 2022, 8, 5307–5318. [Google Scholar] [CrossRef]
- Li, H.; Wijekoon, A.; Leipzig, N.D. 3D differentiation of neural stem cells in macroporous photopolymerizable hydrogel scaffolds. PLoS ONE 2012, 7, e48824. [Google Scholar] [CrossRef] [Green Version]
- Potjewyd, G.; Moxon, S.; Wang, T.; Domingos, M.; Hooper, N.M. Tissue Engineering 3D Neurovascular Units: A Biomaterials and Bioprinting Perspective. Trends Biotechnol. 2018, 36, 457–472. [Google Scholar] [CrossRef]
- Moztarzadeh, F.; Sadeghi, A. Design and manufacture of neural tissue engineering scaffolds using hyaluronic acid and polycaprolactone nanofibers with controlled porosity. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 69, 380–387. [Google Scholar] [CrossRef]
- O’Brien, F.J.; Harley, B.A.; Yannas, I.V.; Gibson, L.J. The effect of pore size on cell adhesion in collagen-GAG scaffolds. Biomaterials 2005, 26, 433–441. [Google Scholar] [CrossRef]
- Nam, J.; Huang, Y.; Agarwal, S.; Lannutti, J. Improved cellular infiltration in electrospun fiber via engineered porosity. Tissue Eng. 2007, 13, 2249–2257. [Google Scholar] [CrossRef] [Green Version]
- Bružauskaitė, I.; Bironaitė, D.; Bagdonas, E.; Bernotienė, E. Scaffolds and cells for tissue regeneration: Different scaffold pore sizes-different cell effects. Cytotechnology 2016, 68, 355–369. [Google Scholar] [CrossRef] [Green Version]
- Yan, M.; Wang, L.; Wu, Y.; Wang, L.; Lu, Y. Three-dimensional highly porous hydrogel scaffold for neural circuit dissection and modulation. Acta Biomater. 2023, 157, 252–262. [Google Scholar] [CrossRef]
- Joshi, J.; Homburg, S.V.; Ehrmann, A. Atomic Force Microscopy (AFM) on Biopolymers and Hydrogels for Biotechnological Applications-Possibilities and Limits. Polymers 2022, 14, 1267. [Google Scholar] [CrossRef]
- Willerth, S.M.; Sakiyama-Elbert, S.E. Approaches to neural tissue engineering using scaffolds for drug delivery. Adv. Drug Deliv. Rev. 2007, 59, 325–338. [Google Scholar] [CrossRef] [Green Version]
- de Sousa Victor, R.; Marcelo da Cunha Santos, A.; Viana de Sousa, B.; de Araújo Neves, G.; Navarro de Lima Santana, L.; Rodrigues Menezes, R. A Review on Chitosan’s Uses as Biomaterial: Tissue Engineering, Drug Delivery Systems and Cancer Treatment. Materials 2020, 13, 4995. [Google Scholar] [CrossRef]
- El-Husseiny, H.M.; Mady, E.A.; Hamabe, L.; Abugomaa, A.; Shimada, K.; Yoshida, T.; Tanaka, T.; Yokoi, A.; Elbadawy, M.; Tanaka, R. Smart/stimuli-responsive hydrogels: Cutting-edge platforms for tissue engineering and other biomedical applications. Mater. Today Bio 2021, 13, 100186. [Google Scholar] [CrossRef]
- Tarus, D.; Hamard, L.; Caraguel, F.; Wion, D.; Szarpak-Jankowska, A.; van der Sanden, B.; Auzély-Velty, R. Design of Hyaluronic Acid Hydrogels to Promote Neurite Outgrowth in Three Dimensions. ACS Appl. Mater. Interfaces 2016, 8, 25051–25059. [Google Scholar] [CrossRef]
- Luo, Y.; Shoichet, M.S. A photolabile hydrogel for guided three-dimensional cell growth and migration. Nat. Mater. 2004, 3, 249–253. [Google Scholar] [CrossRef]
- Li, W.; Guo, Y.; Wang, H.; Shi, D.; Liang, C.; Ye, Z.; Qing, F.; Gong, J. Electrospun nanofibers immobilized with collagen for neural stem cells culture. J. Mater. Sci. Mater. Med. 2008, 19, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.Y.; Chen, M.H.; Chang, W.H.; Huang, M.Y.; Wang, T.W. Neural stem cells encapsulated in a functionalized self-assembling peptide hydrogel for brain tissue engineering. Biomaterials 2013, 34, 2005–2016. [Google Scholar] [CrossRef] [PubMed]
- Balion, Z.; Cėpla, V.; Svirskiene, N.; Svirskis, G.; Druceikaitė, K.; Inokaitis, H.; Rusteikaitė, J.; Masilionis, I.; Stankevičienė, G.; Jelinskas, T.; et al. Cerebellar Cells Self-Assemble into Functional Organoids on Synthetic, Chemically Crosslinked ECM-Mimicking Peptide Hydrogels. Biomolecules 2020, 10, 754. [Google Scholar] [CrossRef]
- Long, Y.; Yan, L.; Dai, H.; Yang, D.; Wu, X.; Dong, X.; Liu, K.; Wei, W.; Chen, Y. Enhanced proliferation and differentiation of neural stem cells by peptide-containing temperature-sensitive hydrogel scaffold. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 116, 111258. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Kumar, R.; Jha, N.N.; Maji, S.K. Controlled Exposure of Bioactive Growth Factor in 3D Amyloid Hydrogel for Stem Cells Differentiation. Adv. Healthc. Mater. 2017, 6, 1700368. [Google Scholar] [CrossRef]
- Hatakeyama, M.; Ninomiya, I.; Kanazawa, M. Angiogenesis and neuronal remodeling after ischemic stroke. Neural Regen. Res. 2020, 15, 16–19. [Google Scholar] [CrossRef]
- Kfoury, G.; El Habbaki, V.; Malaeb, W.; Weaver, S.; Momotenko, D.; Mhanna, R. Alginate Sulfate Substrates Control Growth Factor Binding and Growth of Primary Neurons: Toward Engineered 3D Neural Networks. Adv. Biosyst. 2020, 4, e2000047. [Google Scholar] [CrossRef]
- Lu, J.; Guan, F.; Cui, F.; Sun, X.; Zhao, L.; Wang, Y.; Wang, X. Enhanced angiogenesis by the hyaluronic acid hydrogels immobilized with a VEGF mimetic peptide in a traumatic brain injury model in rats. Regen. Biomater. 2019, 6, 325–334. [Google Scholar] [CrossRef] [Green Version]
- McCormick, A.M.; Jarmusik, N.A.; Leipzig, N.D. Co-immobilization of semaphorin3A and nerve growth factor to guide and pattern axons. Acta Biomater. 2015, 28, 33–44. [Google Scholar] [CrossRef] [Green Version]
- Delgado-Rivera, R.; Harris, S.L.; Ahmed, I.; Babu, A.N.; Patel, R.P.; Ayres, V.; Flowers, D.; Meiners, S. Increased FGF-2 secretion and ability to support neurite outgrowth by astrocytes cultured on polyamide nanofibrillar matrices. Matrix Biol. 2009, 28, 137–147. [Google Scholar] [CrossRef]
- Alberti, K.; Davey, R.E.; Onishi, K.; George, S.; Salchert, K.; Seib, F.P.; Bornhäuser, M.; Pompe, T.; Nagy, A.; Werner, C.; et al. Functional immobilization of signaling proteins enables control of stem cell fate. Nat. Methods 2008, 5, 645–650. [Google Scholar] [CrossRef]
- Horne, M.K.; Nisbet, D.R.; Forsythe, J.S.; Parish, C.L. Three-dimensional nanofibrous scaffolds incorporating immobilized BDNF promote proliferation and differentiation of cortical neural stem cells. Stem Cells Dev. 2010, 19, 843–852. [Google Scholar] [CrossRef]
- Xia, M.; Zhao, T.; Wang, X.; Li, Y.; Li, Y.; Zheng, T.; Li, J.; Feng, Y.; Wei, Y.; Sun, P. Brain-derived Neurotrophic Factor and Its Applications through Nanosystem Delivery. Iran. J. Pharm. Res. 2021, 20, 137–151. [Google Scholar] [CrossRef]
- Klaver, C.L.; Caplan, M.R. Bioactive surface for neural electrodes: Decreasing astrocyte proliferation via transforming growth factor-beta1. J. Biomed. Mater. Res. A 2007, 81, 1011–1016. [Google Scholar] [CrossRef]
- Chen, B.K.; Madigan, N.N.; Hakim, J.S.; Dadsetan, M.; McMahon, S.S.; Yaszemski, M.J.; Windebank, A.J. GDNF Schwann cells in hydrogel scaffolds promote regional axon regeneration, remyelination and functional improvement after spinal cord transection in rats. J. Tissue Eng. Regen. Med. 2018, 12, e398–e407. [Google Scholar] [CrossRef] [Green Version]
- Alegret, N.; Dominguez-Alfaro, A.; Mecerreyes, D. 3D Scaffolds Based on Conductive Polymers for Biomedical Applications. Biomacromolecules 2019, 20, 73–89. [Google Scholar] [CrossRef]
- Bierman-Duquette, R.D.; Safarians, G.; Huang, J.; Rajput, B.; Chen, J.Y.; Wang, Z.Z.; Seidlits, S.K. Engineering Tissues of the Central Nervous System: Interfacing Conductive Biomaterials with Neural Stem/Progenitor Cells. Adv. Healthc. Mater. 2022, 11, e2101577. [Google Scholar] [CrossRef]
- Gebeyehu, E.K.; Sui, X.; Adamu, B.F.; Beyene, K.A.; Tadesse, M.G. Cellulosic-Based Conductive Hydrogels for Electro-Active Tissues: A Review Summary. Gels 2022, 8, 140. [Google Scholar] [CrossRef]
- Suarez-Cedeno, G.; Suescun, J.; Schiess, M.C. Earlier Intervention with Deep Brain Stimulation for Parkinson’s Disease. Park. Dis. 2017, 2017, 9358153. [Google Scholar] [CrossRef] [Green Version]
- Elias, G.J.B.; Namasivayam, A.A.; Lozano, A.M. Deep brain stimulation for stroke: Current uses and future directions. Brain Stimul. 2018, 11, 3–28. [Google Scholar] [CrossRef]
- Arya, S.; Filkowski, M.M.; Nanda, P.; Sheth, S.A. Deep brain stimulation for obsessive-compulsive disorder. Bull. Menn. Clin. 2019, 83, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Figee, M.; Riva-Posse, P.; Choi, K.S.; Bederson, L.; Mayberg, H.S.; Kopell, B.H. Deep Brain Stimulation for Depression. Neurotherapeutics 2022, 19, 1229–1245. [Google Scholar] [CrossRef] [PubMed]
- Gordon, T. Electrical Stimulation to Enhance Axon Regeneration After Peripheral Nerve Injuries in Animal Models and Humans. Neurotherapeutics 2016, 13, 295–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertucci, C.; Koppes, R.; Dumont, C.; Koppes, A. Neural responses to electrical stimulation in 2D and 3D in vitro environments. Brain Res. Bull. 2019, 152, 265–284. [Google Scholar] [CrossRef] [PubMed]
- Doron, G.; Brecht, M. What single-cell stimulation has told us about neural coding. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2015, 370, 20140204. [Google Scholar] [CrossRef] [Green Version]
- Edwards, C.A.; Kouzani, A.; Lee, K.H.; Ross, E.K. Neurostimulation Devices for the Treatment of Neurologic Disorders. Mayo Clin. Proc. 2017, 92, 1427–1444. [Google Scholar] [CrossRef] [Green Version]
- Huang, A.P.; Lai, D.M.; Hsu, Y.H.; Tsai, H.H.; Su, C.Y.; Hsu, S.H. An anti-inflammatory gelatin hemostatic agent with biodegradable polyurethane nanoparticles for vulnerable brain tissue. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 121, 111799. [Google Scholar] [CrossRef]
- Fabbro, A.; Cellot, G.; Prato, M.; Ballerini, L. Interfacing neurons with carbon nanotubes: (Re)engineering neuronal signaling. Prog. Brain Res. 2011, 194, 241–252. [Google Scholar] [CrossRef]
- John, A.A.; Subramanian, A.P.; Vellayappan, M.V.; Balaji, A.; Mohandas, H.; Jaganathan, S.K. Carbon nanotubes and graphene as emerging candidates in neuroregeneration and neurodrug delivery. Int. J. Nanomed. 2015, 10, 4267–4277. [Google Scholar] [CrossRef] [Green Version]
- Gibney, S.; Hicks, J.M.; Robinson, A.; Jain, A.; Sanjuan-Alberte, P.; Rawson, F.J. Toward nanobioelectronic medicine: Unlocking new applications using nanotechnology. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2021, 13, e1693. [Google Scholar] [CrossRef]
- Cellot, G.; Cilia, E.; Cipollone, S.; Rancic, V.; Sucapane, A.; Giordani, S.; Gambazzi, L.; Markram, H.; Grandolfo, M.; Scaini, D.; et al. Carbon nanotubes might improve neuronal performance by favouring electrical shortcuts. Nat. Nanotechnol. 2009, 4, 126–133. [Google Scholar] [CrossRef]
- Bareket-Keren, L.; Hanein, Y. Carbon nanotube-based multi electrode arrays for neuronal interfacing: Progress and prospects. Front. Neural. Circuits 2013, 6, 122. [Google Scholar] [CrossRef] [Green Version]
- Cellot, G.; Franceschi Biagioni, A.; Ballerini, L. Nanomedicine and graphene-based materials: Advanced technologies for potential treatments of diseases in the developing nervous system. Pediatr. Res. 2022, 92, 71–79. [Google Scholar] [CrossRef]
- Lanone, S.; Andujar, P.; Kermanizadeh, A.; Boczkowski, J. Determinants of carbon nanotube toxicity. Adv. Drug Deliv. Rev. 2013, 65, 2063–2069. [Google Scholar] [CrossRef]
- Chetyrkina, M.R.; Fedorov, F.S.; Nasibulin, A.G. In vitro toxicity of carbon nanotubes: A systematic review. RSC Adv. 2022, 12, 16235–16256. [Google Scholar] [CrossRef]
- Salih, S.J.; Ghobadi, M.Z. Evaluating the cytotoxicity and pathogenicity of multi-walled carbon nanotube through weighted gene co-expression network analysis: A nanotoxicogenomics study. BMC Genom. Data 2022, 23, 12. [Google Scholar] [CrossRef]
- Duke, K.S.; Bonner, J.C. Mechanisms of carbon nanotube-induced pulmonary fibrosis: A physicochemical characteristic perspective. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2018, 10, e1498. [Google Scholar] [CrossRef]
- Ema, M.; Gamo, M.; Honda, K. A review of toxicity studies of single-walled carbon nanotubes in laboratory animals. Regul. Toxicol. Pharmacol. 2016, 74, 42–63. [Google Scholar] [CrossRef]
- Liang, Y.; Goh, J.C. Polypyrrole-Incorporated Conducting Constructs for Tissue Engineering Applications: A Review. Bioelectricity 2020, 2, 101–119. [Google Scholar] [CrossRef]
- Farokhi, M.; Mottaghitalab, F.; Saeb, M.R.; Shojaei, S.; Zarrin, N.K.; Thomas, S.; Ramakrishna, S. Conductive Biomaterials as Substrates for Neural Stem Cells Differentiation towards Neuronal Lineage Cells. Macromol. Biosci. 2021, 21, e2000123. [Google Scholar] [CrossRef]
- Humpolíček, P.; Kašpárková, V.; Pacherník, J.; Stejskal, J.; Bober, P.; Capáková, Z.; Radaszkiewicz, K.A.; Junkar, I.; Lehocký, M. The biocompatibility of polyaniline and polypyrrole: A comparative study of their cytotoxicity, embryotoxicity and impurity profile. Mater. Sci. Eng. C Mater. Biol. Appl. 2018, 91, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Garrudo, F.F.F.; Mikael, P.E.; Rodrigues, C.A.V.; Udangawa, R.W.; Paradiso, P.; Chapman, C.A.; Hoffman, P.; Colaço, R.; Cabral, J.M.S.; Morgado, J.; et al. Polyaniline-polycaprolactone fibers for neural applications: Electroconductivity enhanced by pseudo-doping. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 120, 111680. [Google Scholar] [CrossRef] [PubMed]
- Pires, F.; Ferreira, Q.; Rodrigues, C.A.; Morgado, J.; Ferreira, F.C. Neural stem cell differentiation by electrical stimulation using a cross-linked PEDOT substrate: Expanding the use of biocompatible conjugated conductive polymers for neural tissue engineering. Biochim. Biophys. Acta 2015, 1850, 1158–1168. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Tian, G.; Duan, X.; Chen, H.L.; Kim Richie, D.H. Nanostructured PEDOT Coatings for Electrode-Neuron Integration. ACS Appl. Bio Mater. 2021, 4, 5556–5565. [Google Scholar] [CrossRef]
- Widge, A.S.; Jeffries-El, M.; Cui, X.; Lagenaur, C.F.; Matsuoka, Y. Self-assembled monolayers of polythiophene conductive polymers improve biocompatibility and electrical impedance of neural electrodes. Biosens. Bioelectron. 2007, 2022, 1723–1732. [Google Scholar] [CrossRef]
- Yu, Z.H.; Chen, W.J.; Liu, X.; Xia, Q.Y.; Yang, Y.N.; Dong, M.; Liu, J.H.; Guan, H.J.; Sun, C.; Feng, F.D.; et al. Folate-Modified Photoelectric Responsive Polymer Microarray as Bionic Artificial Retina to Restore Visual Function. ACS Appl. Mater. Interfaces 2020, 12, 28759–28767. [Google Scholar] [CrossRef]
- Granato, A.E.C.; Ribeiro, A.C.; Marciano, F.R.; Rodrigues, B.V.M.; Lobo, A.O.; Porcionatto, M. Polypyrrole increases branching and neurite extension by Neuro2A cells on PBAT ultrathin fibers. Nanomedicine 2018, 14, 1753–1763. [Google Scholar] [CrossRef]
- Cui, C.; Faraji, N.; Lauto, A.; Travaglini, L.; Tonkin, J.; Mahns, D.; Humphrey, E.; Terracciano, C.; Gooding, J.J.; Seidel, J.; et al. A flexible polyaniline-based bioelectronic patch. Biomater. Sci. 2018, 6, 493–500. [Google Scholar] [CrossRef]
- Richardson-Burns, S.M.; Hendricks, J.L.; Foster, B.; Povlich, L.K.; Kim, D.H.; Martin, D.C. Polymerization of the conducting polymer poly(3,4-ethylenedioxythiophene) (PEDOT) around living neural cells. Biomaterials 2007, 28, 1539–1552. [Google Scholar] [CrossRef] [Green Version]
- Asplund, M.; Thaning, E.; Lundberg, J.; Sandberg-Nordqvist, A.C.; Kostyszyn, B.; Inganäs, O.; von Holst, H. Toxicity evaluation of PEDOT/biomolecular composites intended for neural communication electrodes. Biomed. Mater. 2009, 4, 045009. [Google Scholar] [CrossRef]
- Kolaya, E.; Firestein, B.L. Deep brain stimulation: Challenges at the tissue-electrode interface and current solutions. Biotechnol. Prog. 2021, 37, e3179. [Google Scholar] [CrossRef]
- Limongi, T.; Rocchi, A.; Cesca, F.; Tan, H.; Miele, E.; Giugni, A.; Orlando, M.; Perrone Donnorso, M.; Perozziello, G.; Benfenati, F.; et al. Delivery of Brain-Derived Neurotrophic Factor by 3D Biocompatible Polymeric Scaffolds for Neural Tissue Engineering and Neuronal Regeneration. Mol. Neurobiol. 2018, 55, 8788–8798. [Google Scholar] [CrossRef]
- Villanueva-Flores, F.; Castro-Lugo, A.; Ramírez, O.T.; Palomares, L.A. Understanding cellular interactions with nanomaterials: Towards a rational design of medical nanodevices. Nanotechnology 2020, 31, 132002. [Google Scholar] [CrossRef]
- Shabani, L.; Abbasi, M.; Azarnew, Z.; Amani, A.M.; Vaez, A. Neuro-nanotechnology: Diagnostic and therapeutic nano-based strategies in applied neuroscience. Biomed. Eng. Online 2023, 22, 1. [Google Scholar] [CrossRef]
- Knowlton, S.; Anand, S.; Shah, T.; Tasoglu, S. Bioprinting for Neural Tissue Engineering. Trends Neurosci. 2018, 41, 31–46. [Google Scholar] [CrossRef]
- Matai, I.; Kaur, G.; Seyedsalehi, A.; McClinton, A.; Laurencin, C.T. Progress in 3D bioprinting technology for tissue/organ regenerative engineering. Biomaterials 2020, 226, 119536. [Google Scholar] [CrossRef]
- Cadena, M.; Ning, L.; King, A.; Hwang, B.; Jin, L.; Serpooshan, V.; Sloan, S.A. 3D Bioprinting of Neural Tissues. Adv. Healthc. Mater. 2021, 10, e2001600. [Google Scholar] [CrossRef]
- Pawar, K.; Prang, P.; Müller, R.; Caioni, M.; Bogdahn, U.; Kunz, W.; Weidner, N. Intrinsic and extrinsic determinants of central nervous system axon outgrowth into alginate-based anisotropic hydrogels. Acta Biomater. 2015, 27, 131–139. [Google Scholar] [CrossRef]
- Wang, Y.; Cooke, M.J.; Morshead, C.M.; Shoichet, M.S. Hydrogel delivery of erythropoietin to the brain for endogenous stem cell stimulation after stroke injury. Biomaterials 2012, 33, 2681–2692. [Google Scholar] [CrossRef]
- Mo, L.; Yang, Z.; Zhang, A.; Li, X. The repair of the injured adult rat hippocampus with NT-3-chitosan carriers. Biomaterials 2010, 31, 2184–2192. [Google Scholar] [CrossRef]
- Azadi, A.; Hamidi, M.; Rouini, M.R. Methotrexate-loaded chitosan nanogels as ‘Trojan Horses’ for drug delivery to brain: Preparation and in vitro/in vivo characterization. Int. J. Biol. Macromol. 2013, 62, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Zhao, L.; Gu, J.; Nie, D.; Chen, Y.; Zuo, H.; Huan, W.; Shi, J.; Chen, J.; Shi, W. The migration and differentiation of hUC-MSCs(CXCR4/GFP) encapsulated in BDNF/chitosan scaffolds for brain tissue engineering. Biomed. Mater. 2016, 11, 035004. [Google Scholar] [CrossRef] [PubMed]
- Gil, V.; del Río, J.A. Analysis of axonal growth and cell migration in 3D hydrogel cultures of embryonic mouse CNS tissue. Nat. Protoc. 2012, 7, 268–280. [Google Scholar] [CrossRef] [PubMed]
- Duan, H.; Li, X.; Wang, C.; Hao, P.; Song, W.; Li, M.; Zhao, W.; Gao, Y.; Yang, Z. Functional hyaluronate collagen scaffolds induce NSCs differentiation into functional neurons in repairing the traumatic brain injury. Acta Biomater. 2016, 45, 182–195. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.W.; Chang, K.C.; Chen, L.H.; Liao, S.Y.; Yeh, C.W.; Chuang, Y.J. Effects of an injectable functionalized self-assembling nanopeptide hydrogel on angiogenesis and neurogenesis for regeneration of the central nervous system. Nanoscale 2017, 9, 16281–16292. [Google Scholar] [CrossRef]
- Lim, T.C.; Toh, W.S.; Wang, L.S.; Kurisawa, M.; Spector, M. The effect of injectable gelatin-hydroxyphenylpropionic acid hydrogel matrices on the proliferation, migration, differentiation and oxidative stress resistance of adult neural stem cells. Biomaterials 2012, 33, 3446–3455. [Google Scholar] [CrossRef]
- Sarnowska, A.; Jablonska, A.; Jurga, M.; Dainiak, M.; Strojek, L.; Drela, K.; Wright, K.; Tripathi, A.; Kumar, A.; Jungvid, H.; et al. Encapsulation of mesenchymal stem cells by bioscaffolds protects cell survival and attenuates neuroinflammatory reaction in injured brain tissue after transplantation. Cell Transpl. 2013, 22 (Suppl. 1), S67–S82. [Google Scholar] [CrossRef]
- Kumosa, L.S.; Zetterberg, V.; Schouenborg, J. Gelatin promotes rapid restoration of the blood brain barrier after acute brain injury. Acta Biomater. 2018, 65, 137–149. [Google Scholar] [CrossRef]
- Moshayedi, P.; Nih, L.R.; Llorente, I.L.; Berg, A.R.; Cinkornpumin, J.; Lowry, W.E.; Segura, T.; Carmichael, S.T. Systematic optimization of an engineered hydrogel allows for selective control of human neural stem cell survival and differentiation after transplantation in the stroke brain. Biomaterials 2016, 105, 145–155. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Zhang, D.; Ren, Y.; Guo, S.; Li, J.; Ma, S.; Yao, M.; Guan, F. Injectable hyaluronic acid hydrogel loaded with BMSC and NGF for traumatic brain injury treatment. Mater. Today Bio 2021, 13, 100201. [Google Scholar] [CrossRef]
- Nisbet, D.R.; Rodda, A.E.; Horne, M.K.; Forsythe, J.S.; Finkelstein, D.I. Implantation of functionalized thermally gelling xyloglucan hydrogel within the brain: Associated neurite infiltration and inflammatory response. Tissue Eng. Part A 2010, 16, 2833–2842. [Google Scholar] [CrossRef]
- Villanueva-Flores, F.; Miranda-Hernández, M.; Flores-Flores, J.O.; Porras-Sanjuanico, A.; Hu, H.; Pérez-Martínez, L.; Ramírez, O.T.; Palomares, L.A. Poly(vinyl alcohol co-vinyl acetate) as a novel scaffold for mammalian cell culture and controlled drug release. J. Mater. Sci. 2019, 54, 7867–7882. [Google Scholar] [CrossRef]
- Fon, D.; Zhou, K.; Ercole, F.; Fehr, F.; Marchesan, S.; Minter, M.R.; Crack, P.J.; Finkelstein, D.I.; Forsythe, J.S. Nanofibrous scaffolds releasing a small molecule BDNF-mimetic for the re-direction of endogenous neuroblast migration in the brain. Biomaterials 2014, 35, 2692–2712. [Google Scholar] [CrossRef]
- Bjugstad, K.B.; Lampe, K.; Kern, D.S.; Mahoney, M. Biocompatibility of poly(ethylene glycol)-based hydrogels in the brain: An analysis of the glial response across space and time. J. Biomed. Mater. Res. A 2010, 95, 79–91. [Google Scholar] [CrossRef]
- Lampe, K.J.; Kern, D.S.; Mahoney, M.J.; Bjugstad, K.B. The administration of BDNF and GDNF to the brain via PLGA microparticles patterned within a degradable PEG-based hydrogel: Protein distribution and the glial response. J. Biomed. Mater. Res A 2011, 96, 595–607. [Google Scholar] [CrossRef]
- Jhaveri, S.J.; Hynd, M.R.; Dowell-Mesfin, N.; Turner, J.N.; Shain, W.; Ober, C.K. Release of nerve growth factor from HEMA hydrogel-coated substrates and its effect on the differentiation of neural cells. Biomacromolecules 2009, 10, 174–183. [Google Scholar] [CrossRef]
- Plant, G.W.; Woerly, S.; Harvey, A.R. Hydrogels containing peptide or aminosugar sequences implanted into the rat brain: Influence on cellular migration and axonal growth. Exp. Neurol. 1997, 143, 287–299. [Google Scholar] [CrossRef]
- Álvarez, Z.; Castaño, O.; Castells, A.A.; Mateos-Timoneda, M.A.; Planell, J.A.; Engel, E.; Alcántara, S. Neurogenesis and vascularization of the damaged brain using a lactate-releasing biomimetic scaffold. Biomaterials 2014, 35, 4769–4781. [Google Scholar] [CrossRef]
- Carlberg, B.; Axell, M.Z.; Nannmark, U.; Liu, J.; Kuhn, H.G. Electrospun polyurethane scaffolds for proliferation and neuronal differentiation of human embryonic stem cells. Biomed. Mater. 2009, 4, 045004. [Google Scholar] [CrossRef]
- Hsieh, F.Y.; Lin, H.H.; Hsu, S.H. 3D bioprinting of neural stem cell-laden thermoresponsive biodegradable polyurethane hydrogel and potential in central nervous system repair. Biomaterials 2015, 71, 48–57. [Google Scholar] [CrossRef]
- Aligholi, H.; Rezayat, S.M.; Azari, H.; Ejtemaei Mehr, S.; Akbari, M.; Modarres Mousavi, S.M.; Attari, F.; Alipour, F.; Hassanzadeh, G.; Gorji, A. Preparing neural stem/progenitor cells in PuraMatrix hydrogel for transplantation after brain injury in rats: A comparative methodological study. Brain Res. 2016, 1642, 197–208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wadhwa, R.; Lagenaur, C.F.; Cui, X.T. Electrochemically controlled release of dexamethasone from conducting polymer polypyrrole coated electrode. J. Control. Release 2006, 110, 531–541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Q.; Esrafilzadeh, D.; Crook, J.M.; Kapsa, R.; Stewart, E.M.; Tomaskovic-Crook, E.; Wallace, G.G.; Huang, X.F. Electrical Stimulation Using Conductive Polymer Polypyrrole Counters Reduced Neurite Outgrowth of Primary Prefrontal Cortical Neurons from NRG1-KO and DISC1-LI Mice. Sci. Rep. 2017, 7, 42525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zarrintaj, P.; Ahmadi, Z.; Vahabi, H.; Ducos, F.; Reza Saeb, M.; Mozafari, M. Polyaniline in retrospect and prospect. Mater. Today Proc. 2018, 5, 15852–15860. [Google Scholar] [CrossRef]
- Mandal, H.S.; Knaack, G.L.; Charkhkar, H.; McHail, D.G.; Kastee, J.S.; Dumas, T.C.; Peixoto, N.; Rubinson, J.F.; Pancrazio, J.J. Improving the performance of poly(3,4-ethylenedioxythiophene) for brain-machine interface applications. Acta Biomater. 2014, 10, 2446–2454. [Google Scholar] [CrossRef]
- Tang, W.; Fang, F.; Liu, K.; Huang, Z.; Li, H.; Yin, Y.; Wang, J.; Wang, G.; Wei, L.; Ou, Y.; et al. Aligned Biofunctional Electrospun PLGA-LysoGM1 Scaffold for Traumatic Brain Injury Repair. ACS Biomater. Sci. Eng. 2020, 6, 2209–2218. [Google Scholar] [CrossRef]
- Smith, L.A.; Liu, X.; Ma, P.X. Tissue Engineering with Nano-Fibrous Scaffolds. Soft Matter. 2008, 4, 2144–2149. [Google Scholar] [CrossRef] [Green Version]
- Diban, N.; Ramos-Vivas, J.; Remuzgo-Martinez, S.; Ortiz, I.; Urtiaga, A. Poly(ε-caprolactone) films with favourable properties for neural cell growth. Curr. Top. Med. Chem. 2014, 14, 2743–2749. [Google Scholar] [CrossRef]
- Yang, K.; Lee, J.; Lee, J.S.; Kim, D.; Chang, G.E.; Seo, J.; Cheong, E.; Lee, T.; Cho, S.W. Graphene Oxide Hierarchical Patterns for the Derivation of Electrophysiologically Functional Neuron-like Cells from Human Neural Stem Cells. ACS Appl. Mater. Interfaces 2016, 8, 17763–17774. [Google Scholar] [CrossRef]
- Tong, A.; Voronov, R. A Minireview of Microfluidic Scaffold Materials in Tissue Engineering. Front. Mol. Biosci. 2022, 8, 783268. [Google Scholar] [CrossRef]
- Skop, N.B.; Calderon, F.; Cho, C.H.; Gandhi, C.D.; Levison, S.W. Optimizing a multifunctional microsphere scaffold to improve neural precursor cell transplantation for traumatic brain injury repair. J. Tissue Eng. Regen. Med. 2016, 10, E419–E432. [Google Scholar] [CrossRef]
- Büyüköz, M.; Erdal, E.; Alsoy Altinkaya, S. Nanofibrous gelatine scaffolds integrated with nerve growth factor-loaded alginate microspheres for brain tissue engineering. J. Tissue Eng. Regen. Med. 2018, 12, e707–e719. [Google Scholar] [CrossRef]
- Sozzi, E.; Kajtez, J.; Bruzelius, A.; Wesseler, M.F.; Nilsson, F.; Birtele, M.; Larsen, N.B.; Ottosson, D.R.; Storm, P.; Parmar, M.; et al. Silk scaffolding drives self-assembly of functional and mature human brain organoids. Front. Cell Dev. Biol. 2022, 10, 1023279. [Google Scholar] [CrossRef]
- Yadav, S.; Sharma, A.K.; Kumar, P. Nanoscale Self-Assembly for Therapeutic Delivery. Front. Bioeng. Biotechnol. 2020, 8, 127. [Google Scholar] [CrossRef] [Green Version]
- Layrolle, P.; Payoux, P.; Chavanas, S. Message in a Scaffold: Natural Biomaterials for Three-Dimensional (3D) Bioprinting of Human Brain Organoids. Biomolecules 2022, 13, 25. [Google Scholar] [CrossRef]
- Hong, D.; Bae, K.; Yoo, S.; Kang, K.; Jang, B.; Kim, J.; Kim, S.; Jeon, S.; Nam, Y.; Kim, Y.G.; et al. Generation of cellular micropatterns on a single-layered graphene film. Macromol. Biosci. 2014, 14, 314–319. [Google Scholar] [CrossRef]
- Namba, R.M.; Cole, A.A.; Bjugstad, K.B.; Mahoney, M.J. Development of porous PEG hydrogels that enable efficient, uniform cell-seeding and permit early neural process extension. Acta Biomater. 2009, 5, 1884–1897. [Google Scholar] [CrossRef]
- Mooney, D.J.; Baldwin, D.F.; Suh, N.P.; Vacanti, J.P.; Langer, R. Novel approach to fabricate porous sponges of poly(D,L-lactic-co-glycolic acid) without the use of organic solvents. Biomaterials 1996, 17, 1417–1422. [Google Scholar] [CrossRef]



| Immobilized Growth Factor | Effect | Substrate | Reference |
|---|---|---|---|
| VEGF | Enhanced angiogenesis and inhibited formation of glial scars at the injured sites | HA | [88] |
| NGF and FGF-2 | Improves extension and infiltration of neurites and provides neurite guidance. | Chitosan films, Polyamide nanofibers. | [89,90] |
| LIF and SCF | Maintenance of pluripotent state up to two weeks. | Maleic anhydride copolymer thin films. | [91] |
| BNDF | Triggers pluripotent cell differentiation into specific lineages such as neurons or oligodendrocytes, and improvement in synaptic communication. Enhances neural stem cell proliferation. | 3-D electrospun poly-epsilon-caprolactone nanofibers. | [92,93] |
| TGF-β1 | Reduced astrocyte proliferation and glial scar. | Oxidized dextran with sodium metaperiodate. | [94] |
| GDNF | Increased myelination of regenerating axons. | Positively-charged oligo[poly(ethylene glycol)fumarate]. | [95] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Villanueva-Flores, F.; Garcia-Atutxa, I.; Santos, A.; Armendariz-Borunda, J. Toward a New Generation of Bio-Scaffolds for Neural Tissue Engineering: Challenges and Perspectives. Pharmaceutics 2023, 15, 1750. https://doi.org/10.3390/pharmaceutics15061750
Villanueva-Flores F, Garcia-Atutxa I, Santos A, Armendariz-Borunda J. Toward a New Generation of Bio-Scaffolds for Neural Tissue Engineering: Challenges and Perspectives. Pharmaceutics. 2023; 15(6):1750. https://doi.org/10.3390/pharmaceutics15061750
Chicago/Turabian StyleVillanueva-Flores, Francisca, Igor Garcia-Atutxa, Arturo Santos, and Juan Armendariz-Borunda. 2023. "Toward a New Generation of Bio-Scaffolds for Neural Tissue Engineering: Challenges and Perspectives" Pharmaceutics 15, no. 6: 1750. https://doi.org/10.3390/pharmaceutics15061750
APA StyleVillanueva-Flores, F., Garcia-Atutxa, I., Santos, A., & Armendariz-Borunda, J. (2023). Toward a New Generation of Bio-Scaffolds for Neural Tissue Engineering: Challenges and Perspectives. Pharmaceutics, 15(6), 1750. https://doi.org/10.3390/pharmaceutics15061750