Particulate Matter (PM10 and PM2.5) in Subway Systems: Health-Based Economic Assessment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Estimation Framework
2.1.1. Selection of Health Endpoints
- health endpoints reported with a robust characterization of exposure-response relationships;
- health endpoints provided by reliable statistics, such as those based on the International Classification of Diseases (ICD).
2.1.2. Cost-of-Illness (COI) Model
A. Direct Costs
- a = 1, 2, …, n diseases;
- i = 1, 2 genders;
- j = 0, 1, …, n age;
- is the total treatment amount of inpatients for a, i and j in the health insurance data;
- is the total treatment amount of outpatients for a, i and j in the health insurance data;
- α is the percentage of hospitalization expenses borne by the patient;
- β is the percentage of outpatient expenses borne by the patient;
- is the number of outpatient-visit days for a, i and j;
- OM is the average round-trip transportation costs per outpatient visit;
- is the number of hospitalization days for a, i and j;
- M is the average round-trip transportation costs of admission, and
- I is the daily average costs of caregivers for inpatients.
B. Indirect Costs
- a = 1, 2, …, n diseases;
- i = 1, 2 genders;
- j = 0, 1, …, n age;
- t is the age at time of death;
- τ is the number of years;
- is the number of deaths;
- is the annual expected income at t + τ;
- pij is the labor force participation rate;
- eij is the employment rate, and
- r is the discount rate.
- a = 1, 2, …, n diseases;
- i = 1, 2 genders;
- j = 0, 1, …, n age;
- is the number of hospitalization days for a, i and j;
- δ is the non-production rate for an outpatient vs. a hospitalized patient;
- is the number of outpatient-visit days for a, i and j;
- pij is the labor force participation rate;
- eij is the employment rate, and
- yij is patients’ daily average income.
2.1.3. Exposed Population
2.2. Economic Benefit Estimation Methods
- there is no exposure threshold below which PM10 and PM2.5 are not a cause of morbidity or mortality;
- there are no differences in exposure or susceptibility among different populations;
- differences in methodology or sample size among epidemiological studies are ignored;
- the data for all age groups will be applied to the estimations in cases where the data for a particular age is unavailable [23].
2.2.1. Mortality and Morbidity Characterization
- Table 3 summarizes the data used in the calculations of the per-year reductions in morbidity and mortality cases due to 10 μg/m3 decrement of PM10 and PM2.5 levels. Generally, country-specific or local epidemiological studies are the most proper indicators for the assessment of associations between environmental pollution and health outcome in a given region. Nevertheless, given that such studies require time and cost investments as well as there are inadequate domestic data, epidemiological studies established in other countries can be adopted assuming that human reaction is similar in different regions [21,23]. In this study, analytical epidemiological studies used as data sources of the prevention rates in correspondence with 10 μg/m3 PM10 and PM2.5 decrements were considered based on some essential criteria, including: studies assess the association between the change in concentration of PM10 or PM2.5 and one of health endpoints;
- the range of change in concentration of PM10 or PM2.5 in health assessment is 10 μg/m3;
- some approaches are applied to handle potential confoundings or uncertainties.
2.2.2. Economic Benefit Estimation
A. Economic Benefit from Direct Cost Curtailment
B. Economic Benefit from Indirect Cost Curtailment
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Authors | Year Published | Description | Types of Data |
|---|---|---|---|
| Hamra et al. [39] | 2014 | Meta-analyses of studies examining the relationship of exposure to PM2.5 and PM10 with lung cancer incidence and mortality were conducted. In total, 18 studies met authors’ inclusion criteria and provided the information necessary to estimate the change in lung cancer risk per 10 µg/m3 increase in exposure to PM. Random-effects analyses were used to allow between-study variability to contribute to meta-estimates. Estimates were robust to restriction to studies that considered potential confounders, as well as subanalyses by exposure assessment method. | Prevention rate for all lung cancer morbidity associated with each 10 μg/m3 decrement in PM10 concentration; Prevention rate for all lung cancer morbidity associated with each 10 μg/m3 decrement in PM2.5 concentration |
| Zanobetti et al. [40] | 2000 | The association between PM10 and hospital admission for heart and lung disease in ten United States cities was examined. A Poisson regression model in each city was fit to allow for city-specific differences and then the city-specific results were combined. Potential confounding was examined by a meta-regression of the city-specific results. The results were stable when controlling for confounding by sulfur dioxide, ozone, and carbon monoxide. | Prevention rate for cardiovascular morbidity associated with each 10 μg/m3 decrement in PM10 concentration |
| Stafoggia et al. [41] | 2013 | City-specific Poisson models were fitted to estimate associations of daily concentrations of PM2.5, PM10 and PM2.5–10 with daily counts of emergency hospitalizations for cardiovascular and respiratory diseases in eight Southern European cities, within the MED-PARTICLES project. Pooled estimates were derived from random-effects meta-analysis and the robustness of results to co-pollutant exposure adjustment and model specification was evaluated. Pooled concentration—response curves were estimated using a meta-smoothing approach. | Prevention rate for cardiovascular morbidity associated with each 10 μg/m3 decrement in PM2.5 concentration |
| Cui et al. [42] | 2015 | PUBMED and EMBASE databases were utilized to search for prospective cohort studies that evaluated the association between PM2.5, PM10 and lung cancer incidence and mortality. Relative risks and 95% confidence interval were calculated using fixed-effect or random-effects models when appropriate. | Prevention rate for all lung cancer mortality associated with each 10 μg/m3 decrement in PM10 concentration; Prevention rate for all lung cancer mortality associated with each 10 μg/m3 decrement in PM2.5 concentration |
| Analitis et al. [43] | 2006 | The estimated effects of ambient particle concentrations (black smoke and PM10) on cardiovascular and respiratory mortality, from 29 European cities, within the Air Pollution and Health: a European Approach (APHEA2) project, were reported. A 2-stage hierarchical modeling approach assessing city-specific effects first and then overall effects was applied. City characteristics were considered as potential effect modifiers. | Prevention rate for cardiovascular mortality associated with each 10 μg/m3 decrement in PM10 concentration |
| Pope et al. [44] | 2002 | Vital status and cause of death data were collected by the American Cancer Society as part of the Cancer Prevention II study, an on-going prospective mortality study, which enrolled approximately 1.2 million adults in 1982. Participants completed a questionnaire detailing individual risk factor data. The risk factor data for approximately 500,000 adults were linked with air pollution data for metropolitan areas throughout the United States and combined with vital status and cause of death data through 31 December 1998. | Prevention rate for cardiovascular mortality associated with each 10 μg/m3 decrement in PM2.5 concentration |
| ICD-10 Codes | Numbers of Patients | Costs of Treatment | ||
|---|---|---|---|---|
| Inpatient | Outpatient | Inpatient | Outpatient | |
| C33–C34 | 38,581 | 67,715 | 334,299,667 | 208,118,814 |
| I00–I02 | 47 | 2608 | 116,783 | 1,669,552 |
| I05–I09 | 2065 | 22,467 | 24,953,117 | 8,812,322 |
| I10 | 43,036 | 5,441,082 | 143,089,704 | 2,519,175,578 |
| I11–I15 | 7317 | 365,159 | 19,725,153 | 167,941,670 |
| I21–I22 | 25,733 | 80,968 | 211,588,391 | 70,228,942 |
| I20, I23–I25 | 105,212 | 719,564 | 388,519,479 | 435,165,181 |
| I26 | 4335 | 10,913 | 19,794,763 | 5,766,361 |
| I44–I49 | 35,458 | 321,855 | 183,208,643 | 120,725,083 |
| I50 | 21,383 | 110,872 | 81,249,269 | 46,900,788 |
| I27–I43, I51–I52 | 16,112 | 110,810 | 146,047,446 | 53,766,890 |
| I60–I62 | 35,061 | 69,961 | 492,407,437 | 48,315,017 |
| I63 | 95,876 | 402,872 | 794,037,741 | 324,810,885 |
| I64 | 3222 | 18,943 | 17,277,939 | 8,606,552 |
| I65–I69 | 69,486 | 374,877 | 537,458,460 | 180,360,429 |
| I70 | 5736 | 83,279 | 37,061,120 | 31,090,296 |
| I73 | 2092 | 182,660 | 8,762,639 | 26,780,384 |
| I74 | 1580 | 8463 | 9,811,723 | 2,968,997 |
| I71–I72, I77–I79 | 7119 | 46,068 | 90,497,721 | 18,350,586 |
| I80–I82 | 3317 | 26,474 | 11,850,703 | 7,213,287 |
| I83 | 39,273 | 145,276 | 24,240,327 | 13,473,489 |
| I84 | 183,732 | 633,098 | 171,306,439 | 64,124,463 |
| I85–I99 | 16,263 | 174,771 | 26,318,701 | 19,886,521 |
| ICD-10 Codes | Visit Days | |
|---|---|---|
| Inpatient | Outpatient | |
| C33–C34 | 1,274,169 | 743,627 |
| I00–I02 | 1270 | 12,365 |
| I05–I09 | 35,777 | 95,769 |
| I10 | 2,024,940 | 41,110,659 |
| I11–I15 | 196,580 | 1,837,922 |
| I21–I22 | 266,695 | 299,949 |
| I20, I23–I25 | 715,308 | 2,807,472 |
| I26 | 87,656 | 45,975 |
| I44–I49 | 357,476 | 1,146,368 |
| I50 | 486,385 | 428,545 |
| I27–I43, I51–I52 | 303,881 | 389,758 |
| I60–I62 | 2,902,925 | 376,549 |
| I63 | 6,652,417 | 2,058,337 |
| I64 | 192,008 | 58,811 |
| I65–I69 | 4,859,746 | 1,563,194 |
| I70 | 102,666 | 261,618 |
| I73 | 46,398 | 445,746 |
| I74 | 32,867 | 26,545 |
| I71–I72, I77–I79 | 130,265 | 139,906 |
| I80–I82 | 48,735 | 77,906 |
| I83 | 78,269 | 350,942 |
| I84 | 541,883 | 1,536,758 |
| I85–I99 | 111,001 | 359,372 |
| ICD-10 Code(s) | Ratio of Non-Benefit Cost to Treatment Cost | |
|---|---|---|
| Inpatient | Outpatient | |
| C33–C34 | 7.63 | 5.98 |
| I00–I02 | 23.33 | 24.70 |
| I05–I09 | 9.35 | 38.55 |
| I10 | 27.24 | 29.00 |
| I11–I15 | 24.14 | 31.48 |
| I21–I22 | 6.97 | 33.31 |
| I20, I23–I25 | 10.15 | 34.31 |
| I26 | 19.94 | 38.18 |
| I44–I49 | 10.73 | 37.72 |
| I50 | 20.38 | 33.79 |
| I27–I43, I51–I52 | 11.23 | 23.91 |
| I60–I62 | 15.92 | 36.11 |
| I63 | 23.32 | 33.61 |
| I64 | 25.44 | 37.29 |
| I65–I69 | 20.96 | 34.92 |
| I70 | 20.25 | 35.04 |
| I73 | 18.31 | 30.44 |
| I74 | 21.07 | 35.44 |
| I71–I72, I77–I79 | 10.49 | 39.89 |
| I80–I82 | 21.84 | 38.19 |
| I83 | 20.52 | 36.66 |
| I84 | 18.77 | 33.44 |
| I85–I99 | 20.82 | 38.20 |
| Gender | Age | Participation Rate (%) | Employment Rate (%) |
|---|---|---|---|
| Male | 15–19 | 9.6 | 8.5 |
| 20–29 | 64.7 | 57.6 | |
| 30–39 | 93.3 | 90.6 | |
| 40–49 | 94.8 | 93.0 | |
| 50–59 | 90.0 | 88.1 | |
| 60+ | 54.4 | 52.9 | |
| Female | 15–19 | 12.0 | 10.9 |
| 20–29 | 65.6 | 60.7 | |
| 30–39 | 61.4 | 59.5 | |
| 40–49 | 67.7 | 66.4 | |
| 50–59 | 64.6 | 63.2 | |
| 60+ | 32.7 | 32.2 | |
| Total | 63.7 | 61.5 |
| Age | ICD-10 Code(s) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C33–C34 | I00–I09 | I10–I13 | I20–I25 | I26–I51 | I60–I69 | I70 | I71–I99 | |||||||||
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | |
| 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 12 | 7 | 1 | 1 | 0 | 0 | 0 | 0 |
| 1–4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 4 | 2 | 0 | 0 | 0 | 0 | 1 |
| 5–9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 5 | 3 | 2 | 0 | 0 | 0 | 0 |
| 10–14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 4 | 5 | 0 | 0 | 1 | 0 |
| 15–19 | 0 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 16 | 7 | 7 | 4 | 0 | 0 | 0 | 0 |
| 20–24 | 0 | 1 | 1 | 0 | 1 | 0 | 7 | 2 | 27 | 5 | 7 | 11 | 0 | 0 | 1 | 2 |
| 25–29 | 4 | 6 | 0 | 0 | 1 | 0 | 11 | 2 | 30 | 10 | 20 | 12 | 0 | 0 | 3 | 1 |
| 30–34 | 12 | 11 | 0 | 1 | 3 | 1 | 30 | 6 | 56 | 18 | 38 | 23 | 0 | 0 | 8 | 2 |
| 35–39 | 32 | 26 | 1 | 0 | 6 | 1 | 90 | 10 | 89 | 31 | 89 | 47 | 0 | 0 | 3 | 5 |
| 40–44 | 83 | 64 | 0 | 2 | 10 | 0 | 188 | 30 | 141 | 57 | 212 | 93 | 2 | 0 | 17 | 4 |
| 45–49 | 170 | 107 | 2 | 3 | 17 | 3 | 337 | 44 | 230 | 71 | 385 | 177 | 0 | 0 | 25 | 6 |
| 50–54 | 427 | 208 | 1 | 2 | 33 | 9 | 475 | 66 | 341 | 86 | 579 | 215 | 2 | 0 | 34 | 6 |
| 55–59 | 815 | 289 | 3 | 3 | 45 | 12 | 606 | 100 | 430 | 134 | 716 | 284 | 4 | 1 | 45 | 17 |
| 60–64 | 1,239 | 358 | 5 | 7 | 55 | 21 | 675 | 174 | 499 | 143 | 761 | 371 | 2 | 0 | 48 | 21 |
| 65–69 | 1,825 | 426 | 4 | 9 | 99 | 49 | 762 | 227 | 551 | 256 | 933 | 507 | 4 | 3 | 59 | 34 |
| 70–74 | 2,618 | 678 | 9 | 15 | 162 | 155 | 1056 | 533 | 730 | 568 | 1705 | 1110 | 15 | 4 | 111 | 75 |
| 75–79 | 2,737 | 856 | 9 | 17 | 288 | 411 | 1331 | 1139 | 995 | 1055 | 2335 | 2191 | 35 | 6 | 146 | 103 |
| 80–84 | 1,779 | 894 | 9 | 26 | 321 | 739 | 1078 | 1580 | 958 | 1618 | 2085 | 2987 | 23 | 27 | 120 | 117 |
| 85–89 | 714 | 536 | 5 | 20 | 273 | 1054 | 797 | 1649 | 655 | 1767 | 1234 | 2796 | 19 | 22 | 78 | 126 |
| 90+ | 222 | 260 | 4 | 8 | 191 | 1090 | 382 | 1334 | 395 | 1586 | 676 | 1825 | 12 | 30 | 31 | 86 |
References
- Pan, S.; Fan, L.; Liu, J.; Xie, J.; Sun, Y.; Cui, N.; Zhang, L.; Zheng, B. A review of the piston effect in subway stations. Adv. Mech. Eng. 2013, 5, 950205. [Google Scholar] [CrossRef]
- Li, T.-T.; Bai, Y.-H.; Liu, Z.-R.; Li, J.-L. In-train air quality assessment of the railway transit system in Beijing: A note. Transp. Res. Part D 2007, 12, 64–67. [Google Scholar] [CrossRef]
- Midander, K.; Elihn, K.; Wallen, A.; Belova, L.; Karlsson, A.B.; Wallinder, I.O. Characterisation of nano- and micron-sized airborne and collected subway particles, a multi-analytical approach. Sci. Total Environ. 2012, 427–428, 390–400. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuijsen, M.J.; Gómez-Perales, J.E.; Colvile, R.N. Levels of particulate air pollution, its elemental composition, determinants and health effects in metro system. Atmos. Environ. 2007, 41, 7995–8006. [Google Scholar] [CrossRef]
- Park, D.-U.; Ha, K.-C. Characteristics of PM10, PM2.5, CO2 and CO monitored in interiors and platforms of subway train in Seoul, Korea. Environ. Int. 2008, 34, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Ripanucci, G.; Grana, M.; Vicentini, L.; Magrini, A.; Bergamaschi, A. Dust in the underground railway tunnels of an Italian town. J. Occup. Environ. Hyg. 2006, 3, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Sohn, J.R.; Kim, J.-C.; Kim, M.Y.; Son, Y.-S.; Sunwoo, Y. Particulate behavior in subway airspace. Asian J. Atmos. Environ. 2008, 2, 54–59. [Google Scholar] [CrossRef]
- Son, Y.-S.; Salama, A.; Jeong, H.-S.; Kim, S.; Jeong, J.-H.; Lee, J.; Sunwoo, Y.; Kim, J.-C. The effect of platform screen doors on PM10 levels in a subway station and a trial to reduce PM10 in tunnels. Asian J. Atmos. Environ. 2013, 7, 38–47. [Google Scholar] [CrossRef]
- Schwarze, P.E.; Øvrevik, J.; Låg, M.; Refsnes, M.; Nafstad, P.; Hetland, R.B.; Dybing, E. Particulate matter properties and health effects: Consistency of epidemiological and toxicological studies. Hum. Exp. Toxicol. 2006, 25, 559–579. [Google Scholar] [CrossRef] [PubMed]
- Querol, X.; Moreno, T.; Karanasiou, A.; Reche, C.; Alastuey, A.; Viana, M.; Querol, X.; Font, O.; Gil, J.; de Miguel, E.; et al. Variability of levels and composition of PM10 and PM2.5 in the Barcelona metro system. Atmos. Chem. Phys. 2012, 12, 5055–5076. [Google Scholar] [CrossRef]
- The World Bank Group. Project guidelines: Pollutants. In Pollution Prevention and Abatement Handbook 1998; The World Bank Group: Washington, DC, USA, 1999; pp. 179–440. [Google Scholar]
- Bae, H.-J. Effects of short-term exposure to PM10 and PM2.5 on mortality in Seoul. Korean J. Environ. Health Sci. 2014, 40, 346–354. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Europe. Health Effects of Particulate Matter: Policy Implications for Countries in Eastern Europe, Caucasus and Central Asia; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2013. [Google Scholar]
- Karlsson, H.L.; Nilsson, L.M.; Moller, L. Subway particles are more genotoxic than street particles and induce oxidative stress in cultured human lung cells. Chem. Res. Toxicol. 2005, 18, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.Y.; Park, J.B.; Kim, C.N.; Lee, K.J. Assessment of airborne bacteria and particulate matters distributed in Seoul metropolitan subway stations. Korean J. Environ. Health Sci. 2006, 32, 254–261. [Google Scholar]
- World Health Organization Regional Office for Europe. Air Quality Guidelines. Global Update 2005. Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2005. [Google Scholar]
- World Health Organization Regional Office for Europe. Health Relevance of Particulate Matter from Various Sources: Report on a WHO Workshop, Bonn, Germany 26–27 March 2007; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2007. [Google Scholar]
- Kim, J.-B.; Kim, S.; Lee, G.-J.; Bae, G.-N.; Cho, Y.; Park, D.; Lee, D.-H.; Kwon, S.-B. Status of PM in Seoul metropolitan subway cabins and effectiveness of subway cabin air purifier (SCAP). Clean Technol. Environ. Policy 2014, 16, 1193–1200. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, D.K.; Jo, Y.M. Evaluation of cost and environmental benefits by enhancement of dust filtration in a subway MVAC. J. Korean Soc. Indoor Environ. 2011, 8, 223–232. [Google Scholar]
- World Health Organization. Seoul’s Challenges and Achievements: For an Environmentally Sustainable Healthy Urban Transport System; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Park, D.; Lee, Y.; Jung, W.; Jeong, W.; Kwon, S.B.; Cho, Y.; Ko, S. Economic analysis of particulate matter control technologies used in a subway. J. Odor Indoor Environ. 2016, 15, 46–52. [Google Scholar] [CrossRef]
- Ettaro, L.; Songer, T.J.; Zhang, P.; Engelgau, M.M. Cost-of-illness studies in diabetes mellitus. Pharmacoeconomics 2004, 22, 149–164. [Google Scholar] [CrossRef] [PubMed]
- El-Fadel, M.; Massoud, M. Particulate matter in urban areas: Health-based economic assessment. Sci. Total Environ. 2000, 257, 133–146. [Google Scholar] [CrossRef]
- Yin, H.; Xu, L.; Cai, Y. Monetary valuation of PM10-related health risks in Beijing China: The necessity for PM10 pollution indemnity. Int. J. Environ. Res. Public Health 2015, 12, 9967–9987. [Google Scholar] [CrossRef] [PubMed]
- Alberini, A.; Krupnick, A. Cost-of-illness and willingness-to-pay estimates of the benefits of improved air quality: Evidence from Taiwan. Land Econ. 2000, 76, 37–53. [Google Scholar] [CrossRef]
- Byford, S.; Torgerson, D.J.; Raftery, J. Economic note: Cost of illness studies. BMJ 2000, 320, 1335. [Google Scholar] [CrossRef] [PubMed]
- Rice, D.P. Estimating the cost of illness. Am. J. Public Health Nations Health 1967, 57, 424–440. [Google Scholar] [CrossRef] [PubMed]
- Rice, D.P. Cost of illness studies: What is good about them? Inj. Prev. 2000, 6, 177–179. [Google Scholar] [CrossRef] [PubMed]
- Pervin, T.; Gerdtham, U.-G.; Lyttkens, C.H. Societal costs of air pollution-related health hazards: A review of methods and results. Cost Eff. Resour. Alloc. 2008, 6, 19. [Google Scholar] [CrossRef] [PubMed]
- Jo, C. Cost-of-illness studies: Concepts, scopes, and methods. Clin. Mol. Hepatol. 2014, 20, 327–337. [Google Scholar] [CrossRef] [PubMed]
- National Health Insurance Corporation (NHIC); Health Insurance Review & Assessment Service. National Health Insurance Statistical Yearbook of 2015. NHIC Web Site. 2016. Available online: http://www.nhis.or.kr/bbs7/boards/B0075/21824?boardKey=28&sort=sequence&order=desc&rows=10&messageCategoryKey=&pageNumber=1&viewType=generic&targetType=12&targetKey=28&status=&period=&startdt=&enddt=&queryField=&query= (accessed on 21 August 2017).
- Ministry for Health, Welfare and Family Affairs, Korea Institute for Health and Social Affairs. The Third Korea National Health and Nutrition Estimation Survey (KNHANES III) 2005; Ministry for Health, Welfare and Family Affairs, Korea Institute for Health and Social Affairs: Gwacheon, Korea, 2006. Available online: http://repository.kihasa.re.kr:8080/handle/201002/1514 (accessed on 21 August 2017).
- The Korea Patient Helper Society. Available online: http://www.help114.or.kr/ (accessed on 21 August 2017).
- Statistics Korea, Korean Statistical Information Service. Cause of Death Statistics in 2015 (Nationwide). 2016. Available online: http://kosis.kr/ups/ups_01List.jsp (accessed on 21 August 2017).
- Statistics Korea, Korean Statistical Information Service. Economically Active Population Survey. 2017. Available online: http://kosis.kr/eng/statisticsList/statisticsList_01List.jsp?vwcd=MT_ETITLE&parmTabId=M_01_01 (accessed on 21 August 2017).
- Ministry of Employment and Labor. Survey Report on Labor Conditions by Employment Type. 2016. Available online: http://laborstat.molab.go.kr/newOut/renewal/menu05/menu05_search_popup.jsp (accessed on 21 August 2017).
- Koopmanschap, M.A.; Rutten, F.F.H. Indirect costs in economic studies. Confronting the confusion. PharmacoEconomics 1993, 4, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Ko, S.; Jung, Y.-H. Analysis of Drinking-Related Socioeconomic Costs and Cost Effectiveness of Drinking Prevention Policy; Korea Institute for Health and Social Affairs: Seoul, Korea, 2013. [Google Scholar]
- Hamra, G.B.; Guha, N.; Cohen, A.; Laden, F.; Raaschou-Nielsen, O.; Samet, J.M.; Vineis, P.; Forastiere, F.; Saldiva, P.; Yorifuji, T.; et al. Outdoor particulate matter exposure and lung cancer: A systematic review and meta-analysis. Environ. Health Perspect. 2014, 122, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Zanobetti, A.; Schwartz, J.; Dockery, D.W. Airborne particles are a risk factor for hospital admissions for heart and lung disease. Environ. Health Perspect. 2000, 108, 1071–1077. [Google Scholar] [CrossRef] [PubMed]
- Stafoggia, M.; Samoli, E.; Alessandrini, E.; Cadum, E.; Ostro, B.; Berti, G.; Faustini, A.; Jacquemin, B.; Linares, C.; Pascal, M.; et al. Short-term associations between fine and coarse particulate matter and hospitalizations in Southern Europe: Results from the MED-PARTICLES project. Environ. Health Perspect. 2013, 121, 1026–1033. [Google Scholar] [CrossRef] [PubMed]
- Cui, P.; Huang, Y.; Han, J.; Song, F.; Chen, K. Ambient particulate matter and lung cancer incidence and mortality: A meta-analysis of prospective studies. Eur. J. Public Health 2015, 25, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Analitis, A.; Katsouyanni, K.; Dimakopoulou, K.; Samoli, E.; Nikoloulopoulos, A.K.; Petasakis, Y.; Touloumi, G.; Schwartz, J.; Anderson, H.R.; Cambra, K.; et al. Short-term effects of ambient particles on cardiovascular and respiratory mortality. Epidemiology 2006, 17, 230–233. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.A.; Burnett, R.T.; Thun, M.J.; Calle, E.E.; Krewski, D.; Ito, K.; Thurston, G.D. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. J. Am. Med. Assoc. 2002, 287, 1132–1141. [Google Scholar]
- Statistics Korea. Population, Households and Housing Units. 2017. Available online: http://kosis.kr/eng/statisticsList/statisticsList_01List.jsp?vwcd=MT_ETITLE&parentId=A#SubCont (accessed on 21 August 2017).
- Statistics Korea. Consumer Price Index in May 2017. 2017. Available online: http://kostat.go.kr/portal/eng/pressReleases/9/1/index.board?bmode=read&bSeq=&aSeq=360960&pageNo=1&rowNum=10&navCount=10&currPg=&sTarget=title&sTxt= (accessed on 21 August 2017).
- Sung, W.; You, H.; Yoon, T.Y.; Lee, S.-J. Socioeconomic costs of overactive bladder and stress urinary incontinence in Korea. Int. Neurourol. J. 2012, 16, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Chung, W.; Hyun, K.-R. Socioeconomic costs of liver disease in Korea. Korean J. Hepatol. 2011, 17, 274–291. [Google Scholar] [CrossRef] [PubMed]
| Types of Disease | Sub-Types of Disease | ICD-10 Codes |
|---|---|---|
| All lung cancer | Malignant neoplasm of trachea | C33 |
| Malignant neoplasm of bronchus and lung | C34 | |
| Cardiovascular diseases | Acute rheumatic fever | I00–I02 |
| Chronic rheumatic heart diseases | I05–I09 | |
| Essential (primary) hyper tension | I10 | |
| Other hypertensive diseases | I11–I15 | |
| Acute myocardial infarction | I21–I22 | |
| Other ischemic heart diseases | I20, I23–I25 | |
| Pulmonary embolism | I26 | |
| Conduction disorders and cardiac arrhythmias | I44–I49 | |
| Heart failure | I50 | |
| Other heart diseases | I27–I43, I51–I52 | |
| Intracranial hemorrhage | I60–I62 | |
| Cerebral infarction | I63 | |
| Stroke (not specified as hemorrhage or infarction) | I64 | |
| Other cerebrovascular diseases | I65–I69 | |
| Atherosclerosis | I70 | |
| Other peripheral vascular diseases | I73 | |
| Arterial embolism and thrombosis | I74 | |
| Other diseases of arteries, arterioles and capillaries | I71–I72, I77–I79 | |
| Phlebitis, thrombophlebitis, venous embolism and thrombosis | I80–I82 | |
| Varicose veins of lower extremities | I83 | |
| Hemorrhoids | I84 | |
| Other diseases of circulatory system | I85–I99 |
| Types of Cost | Categories | Estimation Variables | Data Sources | |
|---|---|---|---|---|
| Direct costs | Direct medical costs | Benefit sector | Treatment amount of hospitalization and outpatient | National Health Insurance Statistical Yearbook [31] |
| Non-benefit sector | Treatment amount and non-benefit rate of hospitalization and outpatient | |||
| Direct non-medical costs | Transportation | Outpatient-visit days, Round-trip transportation cost | National Health Insurance Statistical Yearbook [31], The Third Korea National Health and Nutrition Estimation Survey [32] | |
| Caregiver | Hospitalization days, Average daily care-giver cost | National Health Insurance Statistical Yearbook [31], The Korea Patient Helper Society [33] | ||
| Indirect costs | Future income loss due to premature death | Number of deaths, Number of years , Employment rate, Average annual real wage, Discount rate | Cause of Death Statistics [34], Economically Active Population Survey [35], Survey Report on Labor Conditions by Employment Type [36] | |
| Productivity loss resulting from absence from work | Hospitalization days, Outpatient visit days, Employment rate, Average daily wage | National Health Insurance Statistical Yearbook [31], Economically Active Population Survey [35], Survey Report on Labor Conditions by Employment Type [36] | ||
| Types of Data | PM Decreased by 10 μg/m3 | Data Values |
|---|---|---|
| Prevention rate for all lung cancer morbidity (%) | PM10 | 8 [39] |
| PM2.5 | 9 [39] | |
| Prevention rate for cardiovascular morbidity (%) | PM10 | 1.27 [40] |
| PM2.5 | 0.51 [41] | |
| Prevention rate for all lung cancer mortality (%) | PM10 | 5 [42] |
| PM2.5 | 9 [42] | |
| Prevention rate for cardiovascular mortality (%) | PM10 | 0.76 [43] |
| PM2.5 | 6 [44] | |
| Total number of all-lung-cancer patients (persons) | - | 106,296 [31] |
| Total number of cardiovascular patients (persons) | - | 10,076,495 [31] |
| Total number of deaths related to all lung cancer (deaths) | - | 3719 a [34] |
| Total number of deaths related to cardiovascular diseases (deaths) | - | 15,709 a [34] |
| Number of passengers exposed to PM10 and PM2.5 (persons) | - | 13,000 [21] |
| Number of workers exposed to PM10 and PM2.5 (persons) | - | 5060 [21] |
| Nationwide population (persons) | 51,069,375 [45] |
| Exposed Target | Exposed PM | Types of Disease | Morbidity Cases Avoided/Year | Mortality Cases Avoided/Year |
|---|---|---|---|---|
| Passenger | PM10 | All lung cancer | 2.16 | 0.05 |
| Cardiovascular diseases | 32.58 | 0.03 | ||
| PM2.5 | All lung cancer | 2.44 | 0.09 | |
| Cardiovascular diseases | 13.08 | 0.24 | ||
| Worker | PM10 | All lung cancer | 0.84 | 0.02 |
| Cardiovascular diseases | 12.68 | 0.01 | ||
| PM2.5 | All lung cancer | 0.95 | 0.03 | |
| Cardiovascular diseases | 5.09 | 0.09 |
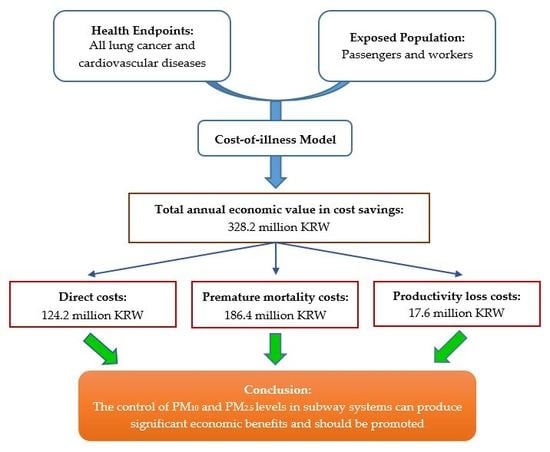
| Exposed Target | Exposed PM | Types of Disease | Economic Value | Total Economic Value |
|---|---|---|---|---|
| Passenger | PM10 | All lung cancer | 14.6 | 89.4 |
| Cardiovascular diseases | 41.6 | |||
| PM2.5 | All lung cancer | 16.5 | ||
| Cardiovascular diseases | 16.7 | |||
| Worker | PM10 | All lung cancer | 5.7 | 34.8 |
| Cardiovascular diseases | 16.2 | |||
| PM2.5 | All lung cancer | 6.4 | ||
| Cardiovascular diseases | 6.5 | |||
| Total | 124.2 |
| Exposed Target | Exposed PM | Types of Disease | Economic Value | Total Economic Value |
|---|---|---|---|---|
| Passenger | PM10 | All lung cancer | 19.9 | 136.6 |
| Cardiovascular diseases | 9.0 | |||
| PM2.5 | All lung cancer | 35.7 | ||
| Cardiovascular diseases | 72.0 | |||
| Worker | PM10 | All lung cancer | 7.9 | 49.8 |
| Cardiovascular diseases | 3.0 | |||
| PM2.5 | All lung cancer | 11.9 | ||
| Cardiovascular diseases | 27.0 | |||
| Total | 186.4 |
| Exposed Target | Exposed PM | Types of Disease | Economic Value | Total Economic Value |
|---|---|---|---|---|
| Passenger | PM10 | All lung cancer | 1.6 | 12.7 |
| Cardiovascular diseases | 6.6 | |||
| PM2.5 | All lung cancer | 1.8 | ||
| Cardiovascular diseases | 2.7 | |||
| Worker | PM10 | All lung cancer | 0.6 | 4.9 |
| Cardiovascular diseases | 2.6 | |||
| PM2.5 | All lung cancer | 0.7 | ||
| Cardiovascular diseases | 1.0 | |||
| Total | 17.6 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, T.N.; Park, D.; Lee, Y.; Lee, Y.-C. Particulate Matter (PM10 and PM2.5) in Subway Systems: Health-Based Economic Assessment. Sustainability 2017, 9, 2135. https://doi.org/10.3390/su9112135
Nguyen TN, Park D, Lee Y, Lee Y-C. Particulate Matter (PM10 and PM2.5) in Subway Systems: Health-Based Economic Assessment. Sustainability. 2017; 9(11):2135. https://doi.org/10.3390/su9112135
Chicago/Turabian StyleNguyen, Thanh Ngoc, Duckshin Park, Yongil Lee, and Young-Chul Lee. 2017. "Particulate Matter (PM10 and PM2.5) in Subway Systems: Health-Based Economic Assessment" Sustainability 9, no. 11: 2135. https://doi.org/10.3390/su9112135
APA StyleNguyen, T. N., Park, D., Lee, Y., & Lee, Y. -C. (2017). Particulate Matter (PM10 and PM2.5) in Subway Systems: Health-Based Economic Assessment. Sustainability, 9(11), 2135. https://doi.org/10.3390/su9112135