Soluble HLA in the Aqueous Humour of Uveal Melanoma Is Associated with Unfavourable Tumour Characteristics
Abstract
:1. Introduction
2. Results
2.1. Patient Demographics
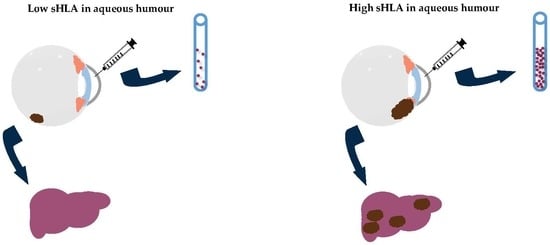
2.2. sHLA in Aqueous Humour Is Related to Survival
2.3. Tumour HLA Expression and Infiltrate in the Tumour, Determined by a Fluidigm qPCR Assay
2.4. Tumour Location in Relation to sHLA in Aqueous Humour
3. Discussion
4. Materials and Methods
4.1. Patient Population
4.2. Collection of Aqueous Humour
4.3. Luminex Assay
4.4. Chromosome Status and BAP1 Immunohistochemistry
4.5. qPCR Analysis Using Fluidigm Array
4.6. Statistical Analyses
4.7. Study Approval
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Singh, A.D.; Turell, M.E.; Topham, A.K. Uveal melanoma: Trends in incidence, treatment, and survival. Ophthalmology 2011, 118, 1881–1885. [Google Scholar] [CrossRef] [PubMed]
- Baily, C.; O’Neill, V.; Dunne, M.; Cunningham, M.; Gullo, G.; Kennedy, S.; Walsh, P.M.; Deady, S.; Horgan, N. Uveal Melanoma in Ireland. Ocul. Oncol Pathol 2019, 5, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Onken, M.D.; Li, J.; Cooper, J.A. Uveal melanoma cells utilize a novel route for transendothelial migration. PLoS ONE 2014, 9, e115472. [Google Scholar] [CrossRef] [PubMed]
- Kalirai, H.; Dodson, A.; Faqir, S.; Damato, B.E.; Coupland, S.E. Lack of BAP1 protein expression in uveal melanoma is associated with increased metastatic risk and has utility in routine prognostic testing. Br. J. Cancer 2014, 111, 1373–1380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cassoux, N.; Rodrigues, M.J.; Plancher, C.; Asselain, B.; Levy-Gabriel, C.; Lumbroso-Le Rouic, L.; Piperno-Neumann, S.; Dendale, R.; Sastre, X.; Desjardins, L.; et al. Genome-wide profiling is a clinically relevant and affordable prognostic test in posterior uveal melanoma. Br. J. Ophthalmol. 2014, 98, 769–774. [Google Scholar] [CrossRef]
- Dogrusoz, M.; Jager, M.J. Genetic prognostication in uveal melanoma. Acta Ophthalmol. 2018, 96, 331–347. [Google Scholar] [CrossRef] [PubMed]
- Versluis, M.; de Lange, M.J.; van Pelt, S.I.; Ruivenkamp, C.A.; Kroes, W.G.; Cao, J.; Jager, M.J.; Luyten, G.P.; van der Velden, P.A. Digital PCR validates 8q dosage as prognostic tool in uveal melanoma. PLoS ONE 2015, 10, e0116371. [Google Scholar] [CrossRef]
- Harbour, J.W.; Onken, M.D.; Roberson, E.D.; Duan, S.; Cao, L.; Worley, L.A.; Council, M.L.; Matatall, K.A.; Helms, C.; Bowcock, A.M. Frequent mutation of BAP1 in metastasizing uveal melanomas. Science 2010, 330, 1410–1413. [Google Scholar] [CrossRef]
- Damato, B.; Coupland, S.E. Translating uveal melanoma cytogenetics into clinical care. Arch. Ophthalmol. 2009, 127, 423–429. [Google Scholar] [CrossRef]
- Prescher, G.; Bornfeld, N.; Hirche, H.; Horsthemke, B.; Jockel, K.H.; Becher, R. Prognostic implications of monosomy 3 in uveal melanoma. Lancet 1996, 347, 1222–1225. [Google Scholar] [CrossRef]
- Maat, W.; Ly, L.V.; Jordanova, E.S.; de Wolff-Rouendaal, D.; Schalij-Delfos, N.E.; Jager, M.J. Monosomy of chromosome 3 and an inflammatory phenotype occur together in uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2008, 49, 505–510. [Google Scholar] [CrossRef] [PubMed]
- van Essen, T.H.; van Pelt, S.I.; Bronkhorst, I.H.; Versluis, M.; Nemati, F.; Laurent, C.; Luyten, G.P.; van Hall, T.; van den Elsen, P.J.; van der Velden, P.A.; et al. Upregulation of HLA Expression in Primary Uveal Melanoma by Infiltrating Leukocytes. PLoS ONE 2016, 11, e0164292. [Google Scholar] [CrossRef] [PubMed]
- Gezgin, G.; Dogrusoz, M.; van Essen, T.H.; Kroes, W.G.M.; Luyten, G.P.M.; van der Velden, P.A.; Walter, V.; Verdijk, R.M.; van Hall, T.; van der Burg, S.H.; et al. Genetic evolution of uveal melanoma guides the development of an inflammatory microenvironment. Cancer Immunol. Immunother. 2017, 66, 903–912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jager, M.J.; Hurks, H.M.; Levitskaya, J.; Kiessling, R. HLA expression in uveal melanoma: There is no rule without some exception. Hum. Immunol. 2002, 63, 444–451. [Google Scholar] [CrossRef]
- Blom, D.J.; Schurmans, L.R.; De Waard-Siebinga, I.; De Wolff-Rouendaal, D.; Keunen, J.E.; Jager, M.J. HLA expression in a primary uveal melanoma, its cell line, and four of its metastases. Br. J. Ophthalmol. 1997, 81, 989–993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ericsson, C.; Seregard, S.; Bartolazzi, A.; Levitskaya, E.; Ferrone, S.; Kiessling, R.; Larsson, O. Association of HLA class I and class II antigen expression and mortality in uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2001, 42, 2153–2156. [Google Scholar]
- Dithmar, S.; Crowder, J.; Jager, M.J.; Vigniswaran, N.; Grossniklaus, H.E. HLA class I antigen expression correlates with histological cell type in uveal melanoma. Der Ophthalmol. 2002, 99, 625–628. [Google Scholar] [CrossRef]
- Hurks, H.M.; Metzelaar-Blok, J.A.; Mulder, A.; Claas, F.H.; Jager, M.J. High frequency of allele-specific down-regulation of HLA class I expression in uveal melanoma cell lines. Int. J. Cancer 2000, 85, 697–702. [Google Scholar] [CrossRef]
- Sato, T.; Carvajal, R.; Nathan, P.; Orloff, M.; Little, N.; McAlpine, C.; Krige, D.; Hassan, N.J.; Hulstine, A.M.; Coughlin, C.M.; et al. Safety, efficacy and biology of the gp100 TCR-based bispecific T cell redirector IMCgp100 in advanced uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2018, 59, 3622. [Google Scholar]
- van Rood, J.J.; van Leeuwen, A.; van Santen, M.C. Anti HL-A2 inhibitor in normal human serum. Nature 1970, 226, 366–367. [Google Scholar] [CrossRef]
- Dobbe, L.M.; Stam, N.J.; Neefjes, J.J.; Giphart, M.J. Biochemical complexity of serum HLA class I molecules. Immunogenetics 1988, 27, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Liem, L.M.; Koelman, C.A.; Doxiadis, I.I.N.; van Houwelingen, J.C.; Goulmy, E.; Claas, F.H.J. Elevated serum HLA class I levels coincide with acute and chronic graft-versus-host disease. Bone Marrow Transplant. 1997, 20, 227–234. [Google Scholar] [CrossRef] [Green Version]
- Koelman, C.A.; Vaessen, L.M.; Balk, A.H.; Weimar, W.; Doxiadis, I.I.N.; Claas, F.H. Donor-derived soluble HLA plasma levels can not be used to monitor graft rejection in heart transplant recipients. Transpl. Immunol. 2000, 8, 57–64. [Google Scholar] [CrossRef]
- Shraibman, B.; Barnea, E.; Kadosh, D.M.; Haimovich, Y.; Slobodin, G.; Rosner, I.; Lopez-Larrea, C.; Hilf, N.; Kuttruff, S.; Song, C.; et al. Identification of Tumor Antigens Among the HLA Peptidomes of Glioblastoma Tumors and Plasma. Mol. Cell. Proteom. 2018, 17, 2132–2145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koelman, C.A.; Coumans, A.B.; Nijman, H.W.; Doxiadis, I.I.N.; Dekker, G.A.; Claas, F.H. Correlation between oral sex and a low incidence of preeclampsia: A role for soluble HLA in seminal fluid? J. Reprod. Immunol. 2000, 46, 155–166. [Google Scholar] [CrossRef]
- Stevenson, F.K.; George, A.J.; Walters, M.T.; Hamblin, T.J. Analysis of soluble HLA class II antigenic material in patients with immunological diseases using monoclonal antibodies. J. Immunol. Methods 1986, 86, 187–190. [Google Scholar] [CrossRef]
- Alvarez-Cermeno, J.C.; Casado, C.; Villar, L.M.; Ferreira, A.; Varela, J.M.; Dominguez, M.; Bootello, A.; Najera, R.; Gonzalez-Porque, P. Soluble class 1 antigens (sHLA) in CSF and serum of patients with HIV infection. Acta Neurol. Scand. 1990, 82, 14–16. [Google Scholar] [CrossRef] [PubMed]
- Zavazava, N.; Bottcher, H.; Ruchholtz, W.M. Soluble MHC class I antigens (sHLA) and anti-HLA antibodies in heart and kidney allograft recipients. Tissue Antigens 1993, 42, 20–26. [Google Scholar] [CrossRef]
- Schutt, P.; Schutt, B.; Switala, M.; Bauer, S.; Stamatis, G.; Opalka, B.; Eberhardt, W.; Schuler, M.; Horn, P.A.; Rebmann, V. Prognostic relevance of soluble human leukocyte antigen-G and total human leukocyte antigen class I molecules in lung cancer patients. Hum. Immunol. 2010, 71, 489–495. [Google Scholar] [CrossRef]
- Campoli, M.; Ferrone, S. Tumor escape mechanisms: Potential role of soluble HLA antigens and NK cells activating ligands. Tissue Antigens 2008, 72, 321–334. [Google Scholar] [CrossRef]
- Nagarkatti-Gude, N.; Bronkhorst, I.H.; van Duinen, S.G.; Luyten, G.P.; Jager, M.J. Cytokines and chemokines in the vitreous fluid of eyes with uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2012, 53, 6748–6755. [Google Scholar] [CrossRef] [PubMed]
- Loumagne, L.; Baudhuin, J.; Favier, B.; Montespan, F.; Carosella, E.D.; Rouas-Freiss, N. In vivo evidence that secretion of HLA-G by immunogenic tumor cells allows their evasion from immunosurveillance. Int. J. Cancer 2014, 135, 2107–2117. [Google Scholar] [CrossRef] [PubMed]
- Bassani-Sternberg, M.; Barnea, E.; Beer, I.; Avivi, I.; Katz, T.; Admon, A. Soluble plasma HLA peptidome as a potential source for cancer biomarkers. Proc. Natl. Acad. Sci. USA 2010, 107, 18769–18776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albitar, M.; Vose, J.M.; Johnson, M.M.; Do, K.A.; Day, A.; Jilani, I.; Kantarjian, H.; Keating, M.; O’Brien, S.M.; Verstovsek, S.; et al. Clinical relevance of soluble HLA-I and beta2-microglobulin levels in non-Hodgkin’s lymphoma and Hodgkin’s disease. Leuk. Res. 2007, 31, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, N.; Shiota, M.; Yamaguchi, A.; Ito, K. Elevated serum level of soluble HLA class I antigens in patients with systemic lupus erythematosus. Arthritis Rheumatol. 1996, 39, 792–796. [Google Scholar] [CrossRef] [PubMed]
- Kubysheva, N.; Soodaeva, S.; Novikov, V.; Eliseeva, T.; Li, T.; Klimanov, I.; Kuzmina, E.; Baez-Medina, H.; Solovyev, V.; Ovsyannikov, D.Y.; et al. Soluble HLA-I and HLA-II Molecules Are Potential Prognostic Markers of Progression of Systemic and Local Inflammation in Patients with COPD. Dis. Markers 2018, 2018, 3614341. [Google Scholar] [CrossRef] [PubMed]
- Ritz, D.; Gloger, A.; Weide, B.; Garbe, C.; Neri, D.; Fugmann, T. High-sensitivity HLA class I peptidome analysis enables a precise definition of peptide motifs and the identification of peptides from cell lines and patients’ sera. Proteomics 2016, 16, 1570–1580. [Google Scholar] [CrossRef] [PubMed]
- Poggi, A.; Zocchi, M.R. Mechanisms of tumor escape: Role of tumor microenvironment in inducing apoptosis of cytolytic effector cells. Arch. Immunol. Ther. Exp. 2006, 54, 323–333. [Google Scholar] [CrossRef]
- Puppo, F.; Contini, P.; Ghio, M.; Indiveri, F. Soluble HLA class I molecules/CD8 ligation trigger apoptosis of CD8+ cells by Fas/Fas-ligand interaction. Sci. World J. 2002, 2, 421–423. [Google Scholar] [CrossRef]
- Ly, L.V.; Bronkhorst, I.H.; van Beelen, E.; Vrolijk, J.; Taylor, A.W.; Versluis, M.; Luyten, G.P.; Jager, M.J. Inflammatory cytokines in eyes with uveal melanoma and relation with macrophage infiltration. Invest. Ophthalmol. Vis. Sci. 2010, 51, 5445–5451. [Google Scholar] [CrossRef]
- Fisson, S.; Ouakrim, H.; Touitou, V.; Baudet, S.; Ben Abdelwahed, R.; Donnou, S.; Miloudi, A.; Galand, C.; Bodaghi, B.; Lehoang, P.; et al. Cytokine profile in human eyes: Contribution of a new cytokine combination for differential diagnosis between intraocular lymphoma or uveitis. PLoS ONE 2013, 8, e52385. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.B. AJCC Cancer Staging Manual, 8th ed.; Springer: New York, NY, USA, 2017. [Google Scholar]
- Meuleman, T.; Drabbels, J.; van Lith, J.M.M.; Dekkers, O.M.; Rozemuller, E.; Cretu-Stancu, M.; Claas, F.H.J.; Bloemenkamp, K.W.M.; Eikmans, M. Lower frequency of the HLA-G UTR-4 haplotype in women with unexplained recurrent miscarriage. J. Reprod. Immunol. 2018, 126, 46–52. [Google Scholar] [CrossRef] [PubMed]
- van Essen, T.H.; van Pelt, S.I.; Versluis, M.; Bronkhorst, I.H.; van Duinen, S.G.; Marinkovic, M.; Kroes, W.G.; Ruivenkamp, C.A.; Shukla, S.; de Klein, A.; et al. Prognostic parameters in uveal melanoma and their association with BAP1 expression. Br. J. Ophthalmol. 2014, 98, 1738–1743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koopmans, A.E.; Verdijk, R.M.; Brouwer, R.W.; van den Bosch, T.P.; van den Berg, M.M.; Vaarwater, J.; Kockx, C.E.; Paridaens, D.; Naus, N.C.; Nellist, M.; et al. Clinical significance of immunohistochemistry for detection of BAP1 mutations in uveal melanoma. Mod. Pathol. 2014, 27, 1321–1330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rekers, N.V.; Bajema, I.M.; Mallat, M.J.; Zuidwijk, K.; Anholts, J.D.; Goemaere, N.; Haasnoot, G.W.; van Groningen, M.C.; van Kooten, C.; de Fijter, J.W.; et al. Quantitative polymerase chain reaction profiling of immunomarkers in rejecting kidney allografts for predicting response to steroid treatment. Transplantation 2012, 94, 596–602. [Google Scholar] [CrossRef]

| Clinical and Histopathologic Characteristics | Patients, n (%) a | ||
|---|---|---|---|
| sHLA Negative (n = 89) | sHLA Positive (n = 19) | p-Value * | |
| Gender | 0.09 b | ||
| Female | 33 (37) | 11 (58) | |
| Male | 56 (63) | 8 (42) | |
| Previous tumour treatment prior to enucleation | 0.69 d | ||
| No | 86 (97) | 18 (95) | |
| Yes | 3 (3) | 1 (5) | |
| Eye | 0.28 b | ||
| OD | 52 (58) | 7 (37) | |
| OS | 37 (42) | 12 (63) | |
| Age at enucleation | 0.46 e | ||
| in years, mean (±S.D.) | 59 (±14) | 63 (±16) | |
| Eye colour c (known in 58 cases) | 0.056 b | ||
| Light | 49 (88) | 10 (67) | |
| Dark | 7 (12) | 5 (33) | |
| Largest basal tumour diameter | 0.40 e | ||
| in mm, mean (±S.D.) (known in 107 cases) | 12.3 (±3.1) | 13.1 (±3.1) | |
| Tumour prominence | <0.001 e,* | ||
| in mm, mean (±S.D.) (known in 107 cases) | 7.0 (±2.9) | 9.8 (±2.2) | |
| Ciliary body involvement | <0.001 b,* | ||
| No | 64 (72) | 5 (26) | |
| Yes | 25 (28) | 14 (74) | |
| Mitotic count f (known in 101 cases) | 0.44 e | ||
| mean (±S.D.) | 4.7 (±3.3) | 6.4 (±7.1) | |
| Histopathologic cell type | 0.064 b | ||
| Spindle cell | 28 (32) | 2 (11) | |
| Epithelioid or mixed cell type | 61 (69) | 17 (89) | |
| Bruch’s membrane (known in 104 cases) | 0.076 d | ||
| Unclear | 10 (12) | 5 (26) | |
| Intact | 21 (25) | 1 (5) | |
| Broken | 53 (62) | 13 (68) | |
| AJCC Stage, 8th edition | <0.001 d,* | ||
| I | 11 (14) | 0 (0) | |
| IIA | 29 (36) | 0 (0) | |
| IIB | 23 (29) | 6 (40) | |
| IIIA, IIIB, IIIC | 17 (21) | 8 (53) | |
| IV | 0 (0) | 1 (7) | |
| Monosomy 3 status (known in 103 cases) | 0.034 b,* | ||
| D3 | 37 (44) | 3 (17) | |
| M3 | 48 (57) | 15 (83) | |
| 8q status (known in 95 cases) | 0.003 b,* | ||
| No gain of 8q | 35 (45) | 1 (6) | |
| Gain of 8q | 43 (55) | 16 (94) | |
| Duplication of chromosome 6p (known in 82 cases) | 0.98 b | ||
| No gain of 6p | 31 (46) | 7 (37) | |
| Gain of 6p | 36 (54) | 8 (42) | |
| Nuclear BAP1 staining (known in 97 cases) | 0.036 b,* | ||
| Normal | 29 (37) | 2 (11) | |
| Absent | 50 (63) | 16 (89) | |
| Metastases (known in 107 cases) | 0.029 b,* | ||
| Absent | 52 (59) | 6 (32) | |
| Present | 36 (41) | 13 (68) | |
| Vital status | 0.36 d | ||
| Dead due to UM metastases | 34 (38) | 11 (58) | |
| Average follow-up time, months | 50 | 27 | |
| Dead due to other cause | 19 (21) | 0 (0) | |
| Alive at last follow-up date | 36 (40) | 8 (42) | |
| sHLA | |||
|---|---|---|---|
| Fluidigm Marker | Negative (Median, 95% CI) | Positive (Median, 95% CI) | p-Value *,§ |
| HLA-A, n = 80 | 431 (218–834) | 1264 (172–2162) | 0.07 |
| HLA-B, n = 81 | 123,245 (81,117–266,604) | 205,282 (55,537–1,062,673) | 0.46 |
| β2M, n = 70 | 373,244 (226,274–566,287) | 416,625 (22,3013–1,391,012) | 0.60 |
| CD40, n = 82 | 670 (451–1454) | 516 (372–869) | 0.38 |
| CD8a, n = 69 | 34 (18–147) | 182 (15–1027) | 0.73 |
| CD4, n = 71 | 274 (163–347) | 188 (95–380) | 0.52 |
| CD3e, n = 65 | 116 (79–213) | 221 (43–1212) | 0.78 |
| CD163, n = 79 | 1023 (509–2000) | 839 (484–2404) | 0.52 |
| CD68, n = 81 | 4934 (2989–9072) | 5473 (2000–25,873) | 1.00 |
| sHLA | |||
|---|---|---|---|
| Variables | B (95% CI) | Beta (β) | p-Value |
| Univariate regression | |||
| Chromosome 3 status (n = 103) | 0.17 (0.01–0.31) | 0.21 | 0.034 * |
| Involvement of ciliary body (n = 108) | 2.87 (−0.43–−0.14) | −0.36 | <0.001 * |
| Tumour prominence (n = 107) | 0.045 (0.02–0.07) | 0.36 | <0.001 * |
| Multivariate regression | |||
| Model 1 | |||
| Chromosome 3 status | 0.097 (−0.53–0.25) | 0.13 | 0.20 |
| Involvement of ciliary body | −0.24 (−0.39–−0.86) | −0.30 | 0.002 * |
| Model 2 | |||
| Tumour prominence | 0.035 (0.01–0.06) | 0.27 | 0.003 * |
| Involvement of ciliary body | −0.233 (−0.38–−0.09) | −0.29 | 0.002 * |
| Model 3 | |||
| Chromosome 3 status | 0.44 (0.02–0.07) | 0.197 | 0.035 * |
| Tumour prominence | 0.15 (0.01–0.30) | 0.348 | <0.001 * |
| Model 4 | |||
| Chromosome 3 status | 0.10 (−0.46–0.25) | 0.13 | 0.17 |
| Tumour prominence | 0.04 (0.01–0.06) | 0.28 | 0.003 * |
| Involvement of ciliary body | −0.18 (−0.34–−0.03) | −0.23 | 0.021 * |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wierenga, A.P.A.; Gezgin, G.; van Beelen, E.; Eikmans, M.; Spruyt-Gerritse, M.; Brouwer, N.J.; Versluis, M.; Verdijk, R.M.; van Duinen, S.G.; Marinkovic, M.; et al. Soluble HLA in the Aqueous Humour of Uveal Melanoma Is Associated with Unfavourable Tumour Characteristics. Cancers 2019, 11, 1202. https://doi.org/10.3390/cancers11081202
Wierenga APA, Gezgin G, van Beelen E, Eikmans M, Spruyt-Gerritse M, Brouwer NJ, Versluis M, Verdijk RM, van Duinen SG, Marinkovic M, et al. Soluble HLA in the Aqueous Humour of Uveal Melanoma Is Associated with Unfavourable Tumour Characteristics. Cancers. 2019; 11(8):1202. https://doi.org/10.3390/cancers11081202
Chicago/Turabian StyleWierenga, Annemijn P. A., Gülçin Gezgin, Els van Beelen, Michael Eikmans, Marijke Spruyt-Gerritse, Niels J. Brouwer, Mieke Versluis, Robert M. Verdijk, Sjoerd G. van Duinen, Marina Marinkovic, and et al. 2019. "Soluble HLA in the Aqueous Humour of Uveal Melanoma Is Associated with Unfavourable Tumour Characteristics" Cancers 11, no. 8: 1202. https://doi.org/10.3390/cancers11081202
APA StyleWierenga, A. P. A., Gezgin, G., van Beelen, E., Eikmans, M., Spruyt-Gerritse, M., Brouwer, N. J., Versluis, M., Verdijk, R. M., van Duinen, S. G., Marinkovic, M., Luyten, G. P. M., & Jager, M. J. (2019). Soluble HLA in the Aqueous Humour of Uveal Melanoma Is Associated with Unfavourable Tumour Characteristics. Cancers, 11(8), 1202. https://doi.org/10.3390/cancers11081202