Effects of Beta-Blockers on Melanoma Microenvironment and Disease Survival in Human
Abstract
:1. Introduction
2. Results
2.1. Adrenergic Sources and Targets in Melanoma Tumors
2.2. Patient Characteristics
2.3. Exposure to Beta-Blockers and Histopathology of Melanoma
2.4. Survival Analyses
2.4.1. Progression-Free Survival
2.4.2. Melanoma Related Survival
2.4.3. Overall Survival
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Study Setting
4.3. Selection Strategy
4.4. Sample Preparation
4.5. Heat Induced Epitope Retrieval
4.6. Staining Procedure
4.7. Image Acquisition and Analyses
4.8. Quality Control for Image Quantification
4.9. Drugs
4.10. Statistics
4.10.1. Histopathological Data
4.10.2. Survival Analyses
4.11. Data Sharing
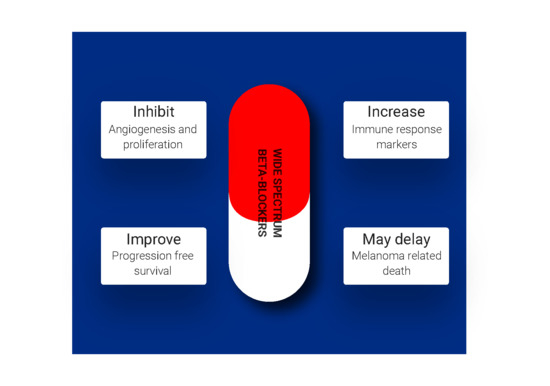
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Madden, K.S.; Sanders, V.M.; Felten, D.L. Catecholamine influences and sympathetic neural modulation of immune responsiveness. Annu. Rev. Pharmacol. Toxicol. 1995, 35, 417–448. [Google Scholar] [CrossRef]
- Yang, E.V.; Kim, S.; Donovan, E.L.; Chen, M.; Gross, A.C.; Webster Marketon, J.I.; Barsky, S.H.; Glaser, R. Norepinephrine upregulates VEGF, IL-8, and IL-6 expression in human melanoma tumor cell lines: Implications for stress-related enhancement of tumor progression. Brain. Behav. Immun. 2009, 23, 267–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wrobel, L.J.; Bod, L.; Lengagne, R.; Kato, M.; Prévost-Blondel, A.; Gal, F.-A.L.; Jean Wrobel, L.; Bod, L.; Lengagne, R.; Kato, M.; et al. Propranolol induces a favourable shift of anti-tumor immunity in a murine spontaneous model of melanoma. Oncotarget 2016, 7, 77825–77837. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schallreuter, K.U.; Wood, J.M.; Lemke, R.; LePoole, C.; Das, P.; Westerhof, W.; Pittelkow, M.R.; Thody, A.J. Production of catecholamines in the human epidermis. Biochem. Biophys. Res. Commun. 1992, 189, 72–78. [Google Scholar] [CrossRef]
- Granstein, R.D.; Luger, T.A. (Eds.) Neuroimmunology of the Skin; Springer: Berlin/Heidelberg, Germany, 2009; ISBN 978-3-540-35986-9. [Google Scholar]
- Bucsek, M.J.; Qiao, G.; MacDonald, C.R.; Giridharan, T.; Evans, L.; Niedzwecki, B.; Liu, H.; Kokolus, K.M.; Eng, J.W.-L.; Messmer, M.N.; et al. β-Adrenergic signaling in mice housed at standard temperatures suppresses an effector phenotype in CD8 + T cells and undermines checkpoint inhibitor therapy. Cancer Res. 2017, 77, 5639–5651. [Google Scholar] [CrossRef] [Green Version]
- Monte, M.D.; Casini, G.; Filippi, L.; Nicchia, G.P.; Svelto, M.; Bagnoli, P. Functional involvement of β3-adrenergic receptors in melanoma growth and vascularization. J. Mol. Med. 2013, 91, 1407–1419. [Google Scholar] [CrossRef]
- Calvani, M.; Pelon, F.; Comito, G.; Taddei, M.L.; Moretti, S.; Innocenti, S.; Nassini, R.; Gerlini, G.; Borgognoni, L.; Bambi, F.; et al. Norepinephrine promotes tumor microenvironment reactivity through β3-adrenoreceptors during melanoma progression. Oncotarget 2015, 6, 4615–4632. [Google Scholar] [CrossRef] [Green Version]
- Alexander, B.S.; Wood, M.D. Stereoselective blockade of central [3H]5-hydroxytryptamine binding to multiple sites (5-HT1A, 5-HT1B and 5-HT1C) by mianserin and propranolol. J. Pharm. Pharmacol. 1987, 39, 664–666. [Google Scholar] [CrossRef] [PubMed]
- Prisco, S.; Cagnotto, A.; Talone, D.; Blasi, A.D.; Mennini, T.; Esposito, E. Tertatolol, a new beta-blocker, is a serotonin (5-hydroxytryptamine1A) receptor antagonist in rat brain. J. Pharmacol. Exp. Ther. 1993, 265, 739–744. [Google Scholar] [PubMed]
- Tinajero, J.C.; Fabbri, A.; Dufau, M.L. Serotonergic inhibition of rat Leydig cell function by propranolol. Endocrinology 1993, 133, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Wrobel, L.J.; Le Gal, F.A. Inhibition of Human Melanoma Growth by a Non-Cardioselective β-Blocker. J. Investig. Dermatol. 2015, 135, 525–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moretti, S.; Massi, D.; Farini, V.; Baroni, G.; Parri, M.; Innocenti, S.; Cecchi, R.; Chiarugi, P. β-adrenoceptors are upregulated in human melanoma and their activation releases pro-tumorigenic cytokines and metalloproteases in melanoma cell lines. Lab. Investig. 2013, 93, 279–290. [Google Scholar] [CrossRef] [Green Version]
- De Giorgi, V.; Grazzini, M.; Benemei, S.; Marchionni, N.; Botteri, E.; Pennacchioli, E.; Geppetti, P.; Gandini, S. Propranolol for off-label treatment of patients with melanoma: Results from a cohort study. JAMA Oncol. 2018, 4, e172908. [Google Scholar] [CrossRef]
- Lemeshow, S.; Sørensen, H.T.; Phillips, G.; Yang, E.V.; Antonsen, S.; Riis, A.H.; Lesinski, G.B.; Jackson, R.; Glaser, R. β-Blockers and Survival among Danish Patients with Malignant Melanoma: A Population-Based Cohort Study. Cancer Epidemiol. Biomark. Prev. 2011, 20, 2273–2279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Giorgi, V.; Grazzini, M.; Gandini, S.; Benemei, S.; Lotti, T.; Marchionni, N.; Geppetti, P. Treatment with β-blockers and reduced disease progression in patients with thick melanoma. Arch. Intern. Med. 2011, 171, 779–781. [Google Scholar] [CrossRef] [PubMed]
- De Giorgi, V.; Gandini, S.; Grazzini, M.; Benemei, S.; Marchionni, N.; Geppetti, P. Effect of β-Blockers and other antihypertensive drugs on the risk of melanoma recurrence and death. Mayo Clin. Proc. 2013, 88, 1196–1203. [Google Scholar] [CrossRef] [PubMed]
- Reinisch, C.M.; Tschachler, E. The dimensions and characteristics of the subepidermal nerve plexus in human skin—Terminal Schwann cells constitute a substantial cell population within the superficial dermis. J. Dermatol. Sci. 2012, 65, 162–169. [Google Scholar] [CrossRef]
- Mäenpää, J.; Pelkonen, O. Cardiac safety of ophthalmic timolol. Expert Opin. Drug Saf. 2016, 15, 1549–1561. [Google Scholar] [CrossRef]
- Müller, L.; Jensen, B.P.; Bachmann, L.M.; Wong, D.; Wells, A.P. New technique to reduce systemic side effects of timolol eye drops: The tissue press method—Cross-over clinical trial. Clin. Exp. Ophthalmol. 2020, 48, 24–30. [Google Scholar] [CrossRef]
- Gérard, C.M.; Bruyns, C.; Delvaux, A.; Baudson, N.; Dargent, J.L.; Goldman, M.; Velu, T. Loss of tumorigenicity and increased immunogenicity induced by interleukin-10 gene transfer in B16 melanoma cells. Hum. Gene Ther. 1996, 7, 23–31. [Google Scholar] [CrossRef]
- Dluzniewski, P.J.; Wang, M.-H.; Zheng, S.L.; De Marzo, A.M.; Drake, C.G.; Fedor, H.L.; Partin, A.W.; Han, M.; Fallin, M.D.; Xu, J.; et al. Variation in IL10 and other genes involved in the immune response and in oxidation and prostate cancer recurrence. Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cospons. Am. Soc. Prev. Oncol. 2012, 21, 1774–1782. [Google Scholar] [CrossRef] [Green Version]
- Prey, S.; Leaute-Labreze, C.; Pain, C.; Moisan, F.; Vergnes, P.; Loot, M.; Taieb, A.; Cario-Andre, M. Mast cells as possible targets of propranolol therapy: An immunohistological study of beta-adrenergic receptors in infantile haemangiomas. Histopathology 2014, 65, 436–439. [Google Scholar] [CrossRef]
- Yuan, W.; Jin, Z.; Wei, J.; Liu, Z.; Xue, L.; Wang, X. Propranolol given orally for proliferating infantile haemangiomas: Analysis of efficacy and serological changes in vascular endothelial growth factor and endothelial nitric oxide synthase in 35 patients. Br. J. Oral Maxillofac. Surg. 2013, 51, 656–661. [Google Scholar] [CrossRef]
- Díaz-Flores, L.; Gutiérrez, R.; García, M.P.; Sáez, F.J.; Díaz-Flores, L.; Valladares, F.; Madrid, J.F. CD34+ stromal cells/fibroblasts/fibrocytes/telocytes as a tissue reserve and a principal source of mesenchymal cells. Location, morphology, function and role in pathology. Histol. Histopathol. 2014, 29, 831–870. [Google Scholar] [PubMed]
- Aponte-López, A.; Fuentes-Pananá, E.M.; Cortes-Muñoz, D.; Muñoz-Cruz, S. Mast cell, the neglected member of the tumor microenvironment: Role in breast cancer. J. Immunol. Res. 2018, 2018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melo, F.R.; Martin, S.S.; Sommerhoff, C.P.; Pejler, G. Exosome-mediated uptake of mast cell tryptase into the nucleus of melanoma cells: A novel axis for regulating tumor cell proliferation and gene expression. Cell Death Dis. 2019, 10, 1–16. [Google Scholar]
- Theoharides, T.C.; Conti, P. Mast cells: The JEKYLL and HYDE of tumor growth. Trends Immunol. 2004, 25, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Reed, J.A.; McNutt, N.S.; Bogdany, J.K.; Albino, A.P. Expression of the mast cell growth factor interleukin-3 in melanocytic lesions correlates with an increased number of mast cells in the perilesional stroma: Implications for melanoma progression. J. Cutan. Pathol. 1996, 23, 495–505. [Google Scholar] [CrossRef] [PubMed]






| Cell Type | DβH | NE | ADRB1 | ADRB2 | 5HT | 5HT1A | 5HT1B |
|---|---|---|---|---|---|---|---|
| Tumor cell | + | + | ND | + | ND | + | ND |
| Keratinocyte | + | ND | ND | + | ND | + | ND |
| Macrophage | + | + | + | ND | ND | ND | ND |
| Mast cell | ND* | ND | + | ND | ND | ND | ND |
| T-Cell | ND | ND | ND | + | ND | + | ND |
| blood vessels | ND | ND | ND | ND | ND | ND | + |
| Variables | No Beta-Blockers (n = 229) | Cardioselective Beta-Blockers (n = 42) | Wide Spectrum Beta-Blockers (n = 15) | p-Value |
|---|---|---|---|---|
| Gender, n (%) | 0.411 | |||
| Female | 96 (41.9) | 13 (31.0) | 6 (40.0) | |
| Male | 133 (58.1) | 29 (69.0) | 9 (60.0) | |
| Age in years at diagnosis, mean (±SD, median) | 59.4 (16.4, 62) | 71.7 (10.6, 71.5) | 69.3 (17.3, 70) | 0.0001 * |
| Mean Breslow thickness index (±SD, median) | 1.66 (2.33, 0.80) | 1.37 (1.82, 0.63) | 1.51 (1.38, 1.50) | 0.399 * |
| Type of melanoma, n (%) | 0.645 | |||
| SSM | 63 (27.5) | 10 (23.8) | 2 (13.3) | |
| NM | 140 (61.1) | 28 (66.7) | 10 (66.7) | |
| Other | 26 (11.4) | 4 (9.5) | 3 (20.0) | |
| Ulceration, n (%) | 26 (11.4) | 5 (11.9) | 4 (26.7) | 0.214 ** |
| Localization, n (%) | 0.053 ** | |||
| Trunk | 112 (48.9) | 15 (35.7) | 5 (33.3) | |
| Lower limb | 65 (28.4) | 9 (21.4) | 3 (20.0) | |
| Upper limb | 27 (11.8) | 7 (16.7) | 4 (26.7) | |
| Head & neck | 25 (10.9) | 11 (26.2) | 3 (20.0) | |
| Clark level, n (%) | 0.379 ** | |||
| II | 80 (34.9) | 17 (40.5) | 7 (46.7) | |
| III | 94 (41.1) | 15 (35.7) | 2 (13.3) | |
| IV | 38 (16.6) | 9 (21.4) | 5 (33.3) | |
| V | 14 (6.1) | 1 (2.4) | 1 (0.7) | |
| NA | 3 (1.3) | 0 (0) | 0 (0) | |
| AJCC staging, n (%) | 0.218 ** | |||
| IA | 137 (60.1) | 28 (66.7) | 7 (46.7) | |
| IB | 30 (13.2) | 3 (7.1) | 1 (6.7) | |
| IIA | 13 (5.7) | 5 (11.9) | 4 (26.7) | |
| IIB | 10 (4.4) | 1 (2.4) | 2 (13.3) | |
| IIC | 6 (2.6) | 1 (2.4) | 0 (0) | |
| IIIA | 12 (5.3) | 0 (0) | 0 (0) | |
| IIIB | 5 (2.2) | 2 (4.8) | 1 (6.7) | |
| IIIC | 10 (4.4) | 1 (2.4) | 0 (0) | |
| IIID | 3 (1.3) | 0 (0) | 0 (0) | |
| IV | 2 (0.9) | 1 (2.4) | 0 (0) |
| Variables | Overall | No Beta-Blockers | Cardio-Selective Beta-Blocker Users | Wide Spectrum Beta-Blocker Users | p-Value * | p-Value ** | p-Value ** |
|---|---|---|---|---|---|---|---|
| Intra tumor vessel density (n = 184) | 1.33 (±1.31, 1.04, 0.57–1.64) | 1.47 (±1.35, 1.17, 0.63–1.87) | 0.99 (±1.23, 0.68, 0.30–1.31) | 0.75 (±0.45, 0.63, 0.36–1.06) | 0.001 | 0.007 | 0.037 |
| KI67 (n = 174) | 14.3 (±10.3, 11.6, 6.6–20.0) | 14.9 (±10.3, 12.6, 7.6–20.8) | 14.0 (±10.6, 12.0, 7.0–19.0) | 8.46 (±8.5, 6.4, 4.5–8.5) | 0.028 | 0.947 | 0.021 |
| CD3 (n = 172) | 1306.4 (±1041.9, 1115.6, 478.2–1822.6) | 1204.1 (±981.7, 1047.8, 465.5–1717.0) | 1505.6 (±1251.0, 1278.7, 475.0–2102.8) | 1968.6 (±752.3, 1907.1, 1628.0–2332.0) | 0.016 | 0.524 | 0.015 |
| Granzyme B (n = 179) | 132.8 (±206.5, 61.4, 18.4–156.4) | 89.7 (±103.8, 52.3, 15.7–134.8) | 201.8 (±240.3, 104.4, 35.0–287.6) | 407.0 (±499.3, 220.9, 57.8–542.9) | 0.0006 | 0.043 | 0.003 |
| CD68 (n = 176) | 342.5 (±307.4, 261.3, 128.5–461.9) | 345.2 (±295.6, 275.8, 136.6–457.6) | 359.8 (±373.8, 208, 125.5–487.8) | 245.1 (±265.5, 154.7, 22.5–384.6) | 0.407 | - | - |
| MPO (n = 188) | 31.0 (±67.3, 9.9, 0.77–28.8) | 24.5 (±45.4, 9.6, 0–28.3) | 47.8 (±114.1, 10.0, 1.7–25.6) | 66.0 (±108.8, 17.3, 4.5–75.0) | 0.380 | - | - |
| CD34 + stromal fibroblasts (n = 175) | 4.56 (±3.49, 3.90, 1.92–5.82) | 5.00 (±3.54, 4.28, 2.39–6.63) | 3.59 (±3.25, 2.94, 1.31–4.59) | 2.36 (±2.09, 1.48, 0.87–3.46) | 0.001 | 0.036 | 0.009 |
| Inos (n = 163) | 381.2 (449.8, 256.9, 131.0–452.3) | 409.0 (±486.6, 268.6, 159.6–453.9) | 320.9 (±303.6, 215.8, 94.8–460.7) | 222.7 (±214.0, 111.2, 65.4–394.4) | 0.103 | - | - |
| IL10 (n = 147) | 195.0 (±207.3, 122.6, 39.7–296.0) | 184.5 (±191.9, 119.5, 48.2–235.5) | 184.6 (±268.7, 47.2, 26.2–296.0) | 339.1 (±183.6, 336.0, 201.0–435.0) | 0.0195 | 0.466 | 0.044 |
| TNFa (n = 148) | 191.1 (±251.8, 109.9, 42.5–225.8) | 163.4 (±225.2, 106.5, 41.6–181.3) | 223.4 (±232.0, 162.7, 65.5–256.1) | 416.7 (±416.5, 365.6, 23.4–692.8) | 0.086 | - | - |
| D240 (n = 194) | 0.23 (±0.30, 0.13, 0.05–0.29) | 0.25 (±0.32, 0.14, 0.05–0.33) | 0.17 (±0.22, 0.12, 0.02–0.23) | 0.13 (±0.12, 0.09, 0.06–0.14) | 0.220 | - | - |
| MHCII (n = 208) | 756.9, (±612.5, 648.1, 318.6–1012.3) | 752.8 (±627.4, 648.1, 290.2–1014.3) | 819.9 (±594.6, 703.2, 349.0–1072.7) | 640.9 (±492.5, 480.9, 360.4–912.8) | 0.593 | - | - |
| Mast cells (n = 185) | 179.6 (±129.4, 141.8, 96.0–238.9) | 162.6 (±107.1, 131.6, 89.1–208.9) | 269.6 (±188.3, 234.3, 133–402) | 147.6 (±92.3, 130.0, 88.0–205) | 0.004 | 0.003 | 0.985 |
| Conditions | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| Outcome Assessed | Hazard Ratio | 95%CI | p-Value | Hazard Ratio | 95%CI | p-Value |
| Progression free survival * | ||||||
| Use of beta-blockers | ||||||
| Never (n = 205) | 1.00 | - | 0.011 | 1.00 | - | 0.086 |
| Before melanoma diagnosis (n = 57) | 0.34 | 0.15–0.79 | 0.012 | 0.40 | 0.16–0.97 | 0.042 |
| After melanoma diagnosis (n = 24) | 0.38 | 0.14–1.07 | 0.067 | 0.59 | 0.21–1.65 | 0.317 |
| Breslow thickness index | 1.43 | 1.31–1.55 | <0.001 | 1.30 | 1.18–1.44 | <0.001 |
| Age in categories | ||||||
| <60 | 1.00 | - | 1.00 | - | 0.084 | |
| ≥60 | 0.84 | 0.52–1.35 | 0.467 | 0.65 | 0.40–1.06 | |
| Ulceration | 7.07 | 4.12–12.13 | <0.001 | 3.11 | 1.51–6.41 | 0.002 |
| Melanoma related survival | ||||||
| Use of beta-blockers | ||||||
| Never (n = 205) | 1.00 | - | 0.030 | 1.00 | - | 0.147 |
| Before melanoma diagnosis (n = 57) | 0.18 | 0.04–0.77 | 0.020 | 0.25 | 0.06–1.13 | 0.071 |
| After melanoma diagnosis (n = 24) | 0.41 | 0.12–1.41 | 0.159 | 0.58 | 0.18–1.92 | 0.372 |
| Breslow thickness index | 1.31 | 1.21–1.42 | <0.001 | 1.24 | 1.08–1.41 | 0.002 |
| Age in categories | ||||||
| <60 | 1.00 | - | 0.049 | 1.00 | - | 0.088 |
| ≥60 | 0.55 | 0.30–0.99 | 0.56 | 0.29–1.09 | ||
| Ulceration | 4.80 | 2.45–9.39 | <0.001 | 1.83 | 0.50–6.66 | 0.359 |
| Overall survival | ||||||
| Use of beta-blockers | ||||||
| Never (n = 205) | 1.00 | - | 0.056 | 1.00 | - | 0.094 |
| Before melanoma diagnosis (n = 57) | 1.21 | 0.72–2.03 | 0.468 | 0.93 | 0.54–1.60 | 0.782 |
| After melanoma diagnosis (n = 24) | 0.19 | 0.05–0.81 | 0.025 | 0.20 | 0.05–0.86 | 0.030 |
| Breslow thickness index | 1.25 | 1.18–1.33 | <0.001 | 1.23 | 1.13–1.33 | <0.001 |
| Age in years | 1.04 | 1.03–1.06 | <0.001 | 1.04 | 1.03–1.06 | <0.001 |
| Ulceration | 3.75 | 2.24–6.28 | <0.001 | 1.20 | 0.62–2.34 | 0.587 |
| Beta-Blocker Molecule, n (%) | |
|---|---|
| Cardioselective beta-blocker before melanoma diagnosis | |
| atenolol | 10 (23.8) |
| bisoprolol | 5 (11.9) |
| labetalol | 1 (2.4) |
| metoprolol | 24 (57.1) |
| nebivolol | 2 (4.8) |
| Wide spectrum beta-blocker before melanoma diagnosis | |
| carteolol a | 2 (13.3) |
| carvedilol | 1 (6.7) |
| propranolol | 4 (26.7) |
| sotalol | 1 (6.7) |
| timolol a | 7 (46.7) |
| Cardioselective beta-blocker after melanoma diagnosis | |
| atenolol | 4 (19) |
| bisoprolol | 3 (14.3) |
| cotenolol | 1 (4.8) |
| metoprolol | 12 (57.1) |
| nebivolol | 1 (4.8) |
| Wide spectrum beta-blocker after melanoma diagnosis | |
| propranolol | 1 (33.3) |
| carvedilol | 2 (66.7) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wrobel, L.J.; Gayet-Ageron, A.; Le Gal, F.-A. Effects of Beta-Blockers on Melanoma Microenvironment and Disease Survival in Human. Cancers 2020, 12, 1094. https://doi.org/10.3390/cancers12051094
Wrobel LJ, Gayet-Ageron A, Le Gal F-A. Effects of Beta-Blockers on Melanoma Microenvironment and Disease Survival in Human. Cancers. 2020; 12(5):1094. https://doi.org/10.3390/cancers12051094
Chicago/Turabian StyleWrobel, Ludovic Jean, Angèle Gayet-Ageron, and Frédérique-Anne Le Gal. 2020. "Effects of Beta-Blockers on Melanoma Microenvironment and Disease Survival in Human" Cancers 12, no. 5: 1094. https://doi.org/10.3390/cancers12051094
APA StyleWrobel, L. J., Gayet-Ageron, A., & Le Gal, F. -A. (2020). Effects of Beta-Blockers on Melanoma Microenvironment and Disease Survival in Human. Cancers, 12(5), 1094. https://doi.org/10.3390/cancers12051094