Night Work and Breast Cancer Risk in Nurses: Multifactorial Risk Analysis
Abstract
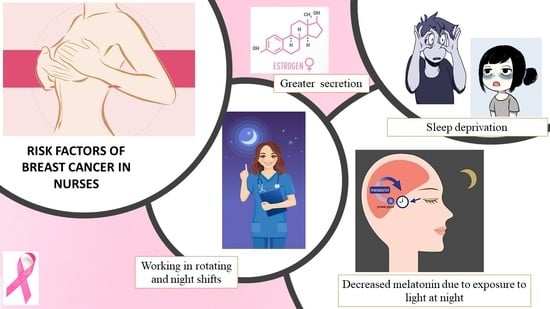
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Sample
2.2. Instrument
2.3. Variables
2.4. Procedure of Data Collection
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
3.1. Sociodemographic Data
3.2. Descriptive and Comparative Analysis between Healthy People and People Who Had or Ever Had Breast Cancer
3.3. Segmentation Tree Based on Risk Factors
3.4. Sex Segmentation Analysis
4. Discussion
4.1. Limitations
4.2. Implications for the Practice and Future Perspectives
- Improved shift work schedule, rotating periods, and breaks: work schedules should be adapted to allow balance between personal life and the adjustment of circadian rhythms before the rotating schedule goes to the next pattern. The shifts are recommended to be adjusted forwards (morning, afternoon, night) and it is also recommended to have a rest period of 24 h after each night shift, increasing the rest time as more consecutive nights have been worked. Ten hours, 12 h, or 24 h-shifts allow fewer consecutive shifts and longer rest periods, although it can cause fatigue due to the high number of working hours.
- Improved facilities: for example, providing adequate lighting, temperature, and ventilation. If possible, offering facilities that allow nurses to rest. The cafeteria or catering for workers should be provided with healthy products.
- Improving the relationship between workers and the company management would be important to increase job satisfaction and compliance with shifts, breaks, and the rotating schedule.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Red Española de Registros de Cáncer (REDECAN). Estimaciones de la Incidencia del Cáncer en España. 2020. Available online: https://redecan.org/redecan.org/es/Informe_incidencia_REDECAN_2020.pdf (accessed on 21 March 2021).
- Red Española de Registros de Cáncer (REDECAN). Estimaciones de la Incidencia del Cáncer en España. 2019. Available online: https://redecan.org/redecan.org/es/Estimaciones_Incidencia_Cancer_en_Espana_2019f2bb.pdf?file=837&area=210 (accessed on 21 March 2021).
- Observatorio de Informes de la Asociación Española Contra el Cáncer [Internet]. Informes Sobre Incidencia, Prevalencia y Mortalidad. Available online: http://observatorio.aecc.es/#datos-informes (accessed on 21 March 2021).
- Smigal, C.; Jemal, A.; Ward, E.; Cokkinides, V.; Smith, R.; Howe, H.L.; Thun, M. Trends in Breast Cancer by Race and Ethnicity: Update. CA: A Cancer J. Clin. 2006, 56, 168–183. [Google Scholar] [CrossRef] [Green Version]
- Verdecchia, A.; Francisci, S.; Brenner, H.; Gatta, G.; Micheli, A.; Mangone, L.; Kunkler, I.; EUROCARE-4 Working Group. Recent cancer survival in Europe: A 2000–02 period analysis of EUROCARE-4 data. Lancet Oncol. 2007, 8, 784–796. [Google Scholar] [CrossRef]
- Galceran, J.; Ameijide, A.; Carulla, M.; Mateos, A.; Quirós, J.R.; Rojas, D.; Alemán, A.; Torrella, A.; Chico, M.; REDECAN Working Group; et al. Cancer incidence in Spain. Clin. Transl. Oncol. 2017, 19, 799–825. [Google Scholar] [CrossRef]
- Sociedad Española de Oncología Médica (SEOM). Las Cifras del Cáncer en España. 2021. Available online: https://seom.org/prensa/el-cancer-en-cifras (accessed on 21 March 2021).
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Painting, Firefighting and Shiftwork; International Agency for Research on Cancer: Lyon, France, 2010; Volume 98. [Google Scholar]
- Stevens, R.G.; Hansen, J.; Costa, G.; Haus, E.; Kauppinen, T.; Aronson, K.J.; Castaño-Vinyals, G.; Davis, S.; Frings-Dresen, M.H.W.; Fritschi, L.; et al. Considerations of circadian impact for defining ’shift work’ in cancer studies: IARC Working Group Report. Occup. Environ. Med. 2011, 68, 154–162. [Google Scholar] [CrossRef]
- Pesch, B.; Harth, V.; Rabstein, S.; Baisch, C.; Schiffermann, M.; Pallapies, D.; Bonberg, N.; Heinze, E.; Spickenheuer, A.; Justenhoven, C.; et al. Night work and breast cancer—Results from the German GENICA study. Scand. J. Work. Environ. Health 2009, 36, 134–141. [Google Scholar] [CrossRef] [Green Version]
- National Toxicology Program. Draft Report on Carcinogens Monograph on Night Shift Work and Light at Night; U.S. Department of Health and Human Services: Washington, DC, USA, 2018. Available online: https://ntp.niehs.nih.gov/whatwestudy/assessments/cancer/ongoing/shiftwork/index.html (accessed on 21 March 2021).
- Touitou, Y.; Reinberg, A.; Touitou, D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption. Life Sci. 2017, 173, 94–106. [Google Scholar] [CrossRef]
- IARC Working Group on the Identification of Carcinogenic Hazards to Humans. Night Shift Work; International Agency for Research on Cancer: Lyon, France, 2020. [Google Scholar]
- Ward, E.M.; Germolec, D.; Kogevinas, M.; McCormick, D.; Vermeulen, R.; Anisimov, V.N.; Aronson, K.J.; Bhatti, P.; Cocco, P.; Costa, G.; et al. Carcinogenicity of night shift work. Lancet Oncol. 2019, 20, 1058–1059. [Google Scholar] [CrossRef]
- McElvenny, D.M.; Crawford, J.O.; Davis, A.; Dixon, K.; Alexander, C.; Cowie, H.; Cherrie, J.W. ; The Institution of Occupational Safety and Health Board (IOSH). A Review of the Impact of Shift Work on Occupational Cancer; IOSH: Wigston, UK, 2018; Available online: https://www.iosh.co.uk/shiftworkreview (accessed on 21 March 2021).
- Rosa, D.; Terzoni, S.; Dellafiore, F.; Destrebecq, A. Systematic review of shift work and nurses’ health. Occup. Med. 2019, 69, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Travis, R.C.; Balkwill, A.; Fensom, G.K.; Appleby, P.N.; Reeves, G.K.; Wang, X.-S.; Roddam, A.W.; Gathani, T.; Peto, R.; Green, J.; et al. Night Shift Work and Breast Cancer Incidence: Three Prospective Studies and Meta-analysis of Published Studies. J. Natl. Cancer Inst. 2016, 108, 169. [Google Scholar] [CrossRef]
- Cordina-Duverger, E.; Menegaux, F.; Popa, A.; Rabstein, S.; Harth, V.; Pesch, B.; Brüning, T.; Fritschi, L.; Glass, D.C.; Heyworth, J.S.; et al. Night shift work and breast cancer: A pooled analysis of population-based case–control studies with complete work history. Eur. J. Epidemiol. 2018, 33, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Fenton, S.; Rydz, E.; Peters, C.E.; Telfer, J. Carcinogenicity of Night Shift Work: Data Gaps and Research Challenges; CAREX: Vancouver, BC, Canada, 2020; Available online: https://www.carexcanada.ca/ (accessed on 21 March 2021).
- Fagundo-Rivera, J.; Gómez-Salgado, J.; García-Iglesias, J.; Gómez-Salgado, C.; Camacho-Martín, S.; Ruiz-Frutos, C. Relationship between Night Shifts and Risk of Breast Cancer among Nurses: A Systematic Review. Medicina 2020, 56, 680. [Google Scholar] [CrossRef]
- Wang, P.; Ren, F.-M.; Lin, Y.; Su, F.-X.; Jia, W.-H.; Su, X.-F.; Tang, L.-Y.; Ren, Z.-F. Night-shift work, sleep duration, daytime napping, and breast cancer risk. Sleep Med. 2015, 16, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Vega-Escaño, J.; Porcel-Gálvez, A.M.; Barrientos-Trigo, S.; Romero-Sánchez, J.M.; De Diego-Cordero, R. La turnicidad como factor determinante en la aparición de insomnio en población laboral: Revisión sistemática [Turnicity as a Determining Factor in the Occurrence of Insomnia in the Working Population: A Systematic Review]. Rev. Esp. Salud Pública. 2020, 94, e1–e12. Available online: https://medes.com/publication/152294 (accessed on 21 March 2021).
- Nagata, C.; Tamura, T.; Wada, K.; Konishi, K.; Goto, Y.; Nagao, Y.; Ishihara, K.; Yamamoto, S. Sleep duration, nightshift work, and the timing of meals and urinary levels of 8-isoprostane and 6-sulfatoxymelatonin in Japanese women. Chrono Int. 2017, 34, 1187–1196. [Google Scholar] [CrossRef]
- Dauchy, R.T.; Wren-Dail, M.A.; Dupepe, L.M.; Hill, S.M.; Xiang, S.; Anbalagan, M.; Belancio, V.P.; Dauchy, E.M.; Blask, D.E. Effect of Daytime Blue-enriched LED Light on the Nighttime Circadian Melatonin Inhibition of Hepatoma 7288CTC Warburg Effect and Progression. Comp. Med. 2018, 68, 269–279. [Google Scholar] [CrossRef]
- De Castro, T.B.; Bordin-Junior, N.A.; De Almeida, E.A.; Zuccari, D.A.P.D.C. Evaluation of melatonin and AFMK levels in women with breast cancer. Endocrine 2018, 62, 242–249. [Google Scholar] [CrossRef] [Green Version]
- Di Sibio, A.; Abriata, G.; Buffa, R.; Viniegra, M.; Forman, D.; Sierra, M.S. Etiology of Breast Cancer (C50) in Central and South America; International Agency for Research on Cancer: Lyon, France, 2016; Available online: http://www-dep.iarc.fr/CSU_resources.htm (accessed on 21 March 2021).
- Marques, J.H.; Mota, A.L.; Oliveira, J.G.; Lacerda, J.Z.; Stefani, J.P.; Ferreira, L.C.; Castro, T.B.; Aristizábal-Pachón, A.F.; Zuccari, D.A. Melatonin restrains angiogenic factors in triple-negative breast cancer by targeting miR-152-3p: In vivo and in vitro studies. Life Sci. 2018, 208, 131–138. [Google Scholar] [CrossRef] [Green Version]
- Bustamante-Montes, L.P.; Flores-Meza, B.; Hernández-Valero, M.A.; Cárdenas-López, A.; Dolores-Velázquez, R.; Borja-Bustamante, P.; Borja-Aburto, V.H. Night Shift Work and Risk of Breast Cancer in Women. Arch. Med Res. 2019, 50, 393–399. [Google Scholar] [CrossRef]
- Cos, S.; González, A.; Martínez-Campa, C.; Mediavilla, M.D.; Alonso-González, C.; Sánchez-Barceló, E.J. Estrogen-signaling pathway: A link between breast cancer and melatonin oncostatic actions. Cancer Detect. Prev. 2006, 30, 118–128. [Google Scholar] [CrossRef]
- Lie, J.-A.S.; Kjuus, H.; Zienolddiny, S.; Haugen, A.; Stevens, R.G.; Kjaerheim, K. Night Work and Breast Cancer Risk Among Norwegian Nurses: Assessment by Different Exposure Metrics. Am. J. Epidemiol. 2011, 173, 1272–1279. [Google Scholar] [CrossRef] [Green Version]
- Lie, J.-A.S.; Kjuus, H.; Zienolddiny, S.; Haugen, A.; Kjaerheim, K. Breast Cancer Among Nurses: Is the Intensity of Night Work Related to Hormone Receptor Status? Am. J. Epidemiol. 2013, 178, 110–117. [Google Scholar] [CrossRef] [Green Version]
- Hansen, J.; Stevens, R.G. Case–control study of shift-work and breast cancer risk in Danish nurses: Impact of shift systems. Eur. J. Cancer 2012, 48, 1722–1729. [Google Scholar] [CrossRef]
- Wegrzyn, L.R.; Tamimi, R.M.; Rosner, B.A.; Brown, S.B.; Stevens, R.G.; Eliassen, A.H.; Laden, F.; Willett, W.C.; Hankinson, S.E.; Schernhammer, E.S. Rotating Night-Shift Work and the Risk of Breast Cancer in the Nurses’ Health Studies. Am. J. Epidemiol. 2017, 186, 532–540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schernhammer, E.S.; Laden, F.; Speizer, F.E.; Willett, W.C.; Hunter, D.J.; Kawachi, I.; Colditz, G.A. Rotating night shifts and risk of breast cancer in women participating in the nurses’ health study. J. Natl. Cancer Inst. 2001, 93, 1563–1568. [Google Scholar] [CrossRef] [Green Version]
- Tamimi, R.M.; Baer, H.J.; Marotti, J.; Galan, M.; Galaburda, L.; Fu, Y.; Deitz, A.C.; Connolly, J.L.; Schnitt, S.J.; Colditz, G.A.; et al. Comparison of molecular phenotypes of ductal carcinoma in situand invasive breast cancer. Breast Cancer Res. 2008, 10, R67. [Google Scholar] [CrossRef] [Green Version]
- Kotsopoulos, J.; Chen, W.Y.; Gates, M.A.; Tworoger, S.S.; Hankinson, S.E.; Rosner, B.A. Risk factors for ductal and lobular breast cancer: Results from the nurses’ health study. Breast Cancer Res. 2010, 12, R106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marotti, J.D.; Collins, L.C.; Hu, R.; Tamimi, R.M. Estrogen receptor-β expression in invasive breast cancer in relation to molecular phenotype: Results from the Nurses’ Health Study. Mod. Pathol. 2010, 23, 197–204. [Google Scholar] [CrossRef] [Green Version]
- Asmat Inostrosa, M.P.; De La Torre Robles, J.M.; Casares Del Rio, M.V.; Espadas Lazo, C. Trabajo nocturno y cáncer de mama en personal sanitario. Rev. Asoc. Esp. Med. Trab. 2018, 27, 141. Available online: http://scielo.isciii.es/pdf/medtra/v27n3/1132-6255-medtra-27-03-141.pdf (accessed on 21 March 2021).
- Papantoniou, K.; Castaño-Vinyals, G.; Espinosa, A.; Aragonés, N.; Pérez-Gómez, B.; Ardanaz, E.; Altzibar, J.M.; Sanchez, V.M.; Gómez-Acebo, I.; Llorca, J.; et al. Breast cancer risk and night shift work in a case–control study in a Spanish population. Eur. J. Epidemiology 2016, 31, 867–878. [Google Scholar] [CrossRef] [Green Version]
- Peplonska, B.; Bukowska, A.; Lie, J.A.; Gromadzinska, J.; Zienolddiny, S. Night shift work and other determinants of estradiol, testosterone, and dehydroepiandrosterone sulfate among middle-aged nurses and midwives. Scand. J. Work. Environ. Health 2016, 42, 435–446. [Google Scholar] [CrossRef]
- Bracci, M.; Manzella, N.; Copertaro, A.; Staffolani, S.; Strafella, E.; Barbaresi, M.; Copertaro, B.; Rapisarda, V.; Valentino, M.; Santarelli, L. Rotating-shift nurses after a day off: Peripheral clock gene expression, urinary melatonin, and serum 17-β-estradiol levels. Scand. J. Work. Environ. Health 2014, 40, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Erdem, J.S.; Notø, H.Ø.; Skare, Ø.; Lie, J.S.; Petersen-Øverleir, M.; Reszka, E.; Pepłońska, B.; Zienolddiny, S. Mechanisms of breast cancer risk in shift workers: Association of telomere shortening with the duration and intensity of night work. Cancer Med. 2017, 6, 1988–1997. [Google Scholar] [CrossRef] [Green Version]
- Salamanca-Fernández, E.; Rodríguez-Barranco, M.; Guevara, M.; Ardanaz, E.; Lima, A.O.D.L.; Sánchez, M. Night-shift work and breast and prostate cancer risk: Updating the evidence from epidemiological studies. An. Sist. Sanit. Navar. 2018, 41, 211–226. [Google Scholar] [CrossRef] [Green Version]
- Jones, M.E.; Schoemaker, M.J.; McFadden, E.C.; Wright, L.B.; Johns, L.E.; Swerdlow, A.J. Night shift work and risk of breast cancer in women: The Generations Study cohort. Br. J. Cancer 2019, 121, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Peplonska, B.; Bukowska, A.; Sobala, W.; Reszka, E.; Gromadzinska, J.; Wasowicz, W.; Lie, J.A.; Kjuus, H.; Ursin, G. Rotating Night Shift Work and Mammographic Density. Cancer Epidemiology Biomarkers Prev. 2012, 21, 1028–1037. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiderpass, E.; Meo, M.; Vainio, H. Risk Factors for Breast Cancer, Including Occupational Exposures. Saf. Health Work. 2011, 2, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dickerman, B.; Liu, J. Does current scientific evidence support a link between light at night and breast cancer among female night-shift nurses? Review of evidence and implications for occupational and environmental health nurses. Work. Health Saf. 2012, 60, 273–281. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística (INE). Profesionales Sanitarios en España. Updated 28/05/2020. [Internet]. Available online: https://www.ine.es/prensa/epsc_2019.pdf (accessed on 21 March 2021).
- Nebot, M.; Manzanares, S.; López, M.J.; Ariza, C.; Galán, I.; Moncada, A.; Montes, A.; Pérez-Ríos, M.; Schiaffino, A.; Fernández, E. Estimación de la exposición al humo ambiental de tabaco: Revisión de cuestionarios utilizados en España [Estimation of environmental tobacco smoke exposure: Review of questionnaires used in Spain]. Gac. Sanit. 2011, 25, 322–328. [Google Scholar] [CrossRef] [Green Version]
- Fox, J. Using the R Commander: A Point-and-Click Interface for R; Chapman & Hall/CRC Press: Boca Raton, FL, USA, 2017. [Google Scholar]
- Malone, K.E.; Daling, J.R.; Doody, D.R.; Hsu, L.; Bernstein, L.; Coates, R.J.; Marchbanks, P.A.; Simon, M.S.; McDonald, J.A.; Norman, S.A.; et al. Prevalence and Predictors of BRCA1 and BRCA2 Mutations in a Population-Based Study of Breast Cancer in White and Black American Women Ages 35 to 64 Years. Cancer Res. 2006, 66, 8297–8308. [Google Scholar] [CrossRef] [Green Version]
- National Institute for Health and Care Excellence (NICE). Familial Breast Cancer: Classification and Care of People at Risk of Familial Breast Cancer and Management of Breast Cancer and Related Risks in People with a Family History of Breast Cancer. Cardiff (UK): National Collaborating Centre for Cancer. 2013. Last Updated: 20 November 2019. Available online: www.nice.org.uk/guidance/cg164. (accessed on 21 March 2021).
- Mavaddat, N.; Antoniou, A.C.; Easton, D.F.; Garcia-Closas, M. Genetic susceptibility to breast cancer. Mol. Oncol. 2010, 4, 174–191. [Google Scholar] [CrossRef]
- Sanguinetti, A.; Polistena, A.; Lucchini, R.; Monacelli, M.; Galasse, S.; Avenia, S.; Triola, R.; Bugiantella, W.; Cirocchi, R.; Rondelli, F.; et al. Male breast cancer, clinical presentation, diagnosis and treatment: Twenty years of experience in our Breast Unit. Int. J. Surg. Case Rep. 2016, 20, 8–11. [Google Scholar] [CrossRef] [Green Version]
- Sahin, C.; Ucpinar, B.A.; Mut, D.T.; Yilmaz, O.; Ucak, R.; Kaya, C.; Tanik, C. Male breast cancer with radiological and histopathological findings. Sisli Etfal Hastan Tip Bul. 2020, 54, 375–379. [Google Scholar] [CrossRef]
- Bender, P.F.M.; De Oliveira, L.L.; Costa, C.R.; De Aguiar, S.S.; Bergmann, A.; Thuler, L.C.S. Men and women show similar survival rates after breast cancer. J. Cancer Res. Clin. Oncol. 2016, 143, 563–571. [Google Scholar] [CrossRef]
- Thuler, L.C.S.; De Aguiar, S.S.; Rapozo, D.; Bello, M.A.; Bergmann, A. Characteristics and prognosis of male breast cancer in Brazil: A cohort study. Breast J. 2021, 27, 95–98. [Google Scholar] [CrossRef] [PubMed]
- Ottini, L.; Palli, D.; Rizzo, S.; Federico, M.; Bazan, V.; Russo, A. Male breast cancer. Crit. Rev. Oncol. Hematol. 2010, 73, 141–155. [Google Scholar] [CrossRef] [PubMed]
- Anderson, W.F.; Jatoi, I.; Tse, J.; Rosenberg, P.S. Male Breast Cancer: A Population-Based Comparison with Female Breast Cancer. J. Clin. Oncol. 2010, 28, 232–239. [Google Scholar] [CrossRef]
- Gao, Y.; Goldberg, J.E.; Young, T.K.; Babb, J.S.; Moy, L.; Heller, S.L. Breast Cancer Screening in High-Risk Men: A 12-year Longitudinal Observational Study of Male Breast Imaging Utilization and Outcomes. Radiology 2019, 293, 282–291. [Google Scholar] [CrossRef]
- Breastcancer.org. Breast Cancer Risk Factors in Men. [Internet]. Available online: https://www.breastcancer.org/es/sintomas/tipos/en_hombres/factores_de_riesgo (accessed on 21 March 2021).
- McPherson, K.; Steel, C.M.; Dixon, J.M. ABC of breast diseases: Breast cancer—Epidemiology, risk factors, and genetics. BMJ 2000, 321, 624–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vogel, V.G. Epidemiology, genetics, and risk evaluation of postmenopausal women at risk of breast cancer. Menopause 2008, 15, 782–789. [Google Scholar] [CrossRef]
- Gómez, E.M.; Cuetos, A.C.; Garrido, C.M.; Martín, C.C.; Velasco, F.A.; Sánchez, N.G.; Goñi, Á.Z. Cáncer de mama en mujeres muy jóvenes, nuestra experiencia. Clínica Investig. Ginecol. Obstet. 2016, 43, 17–23. [Google Scholar] [CrossRef]
- Berkey, C.S.; Tamimi, R.M.; Willett, W.C.; Rosner, B.; Hickey, M.; Toriola, A.T.; Frazier, A.L.; Colditz, G.A. Adolescent alcohol, nuts, and fiber: Combined effects on benign breast disease risk in young women. npj Breast Cancer 2020, 6, 1–5. [Google Scholar] [CrossRef]
- Keegan, T.H.M.; Press, D.J.; Tao, L.; DeRouen, M.C.; Kurian, A.W.; A Clarke, C.; Gomez, S.L. Impact of breast cancer subtypes on 3-year survival among adolescent and young adult women. Breast Cancer Res. 2013, 15, R95. [Google Scholar] [CrossRef] [Green Version]
- Karihtala, P.; Jääskeläinen, A.; Roininen, N.; Jukkola, A. Real-world, single-centre prospective data of age at breast cancer onset: Focus on survival and reproductive history. BMJ Open 2021, 11, e041706. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.; Loibl, S.; Pagani, O.; Graziottin, A.; Panizza, P.; Martincich, L.; Gentilini, O.; Peccatori, F.; Fourquet, A.; Delaloge, S.; et al. The European Society of Breast Cancer Specialists recommendations for the management of young women with breast cancer. Eur. J. Cancer 2012, 48, 3355–3377. [Google Scholar] [CrossRef]
- Jorgensen, J.T.; Karlsen, S.; Stayner, L.; Andersen, J.; Andersen, Z.J. Shift work and overall and cause-specific mortality in the Danish nurse cohort. Scand. J. Work. Environ. Health 2017, 43, 117–126. [Google Scholar] [CrossRef]
- Wickwire, E.M.; Geiger-Brown, J.; Scharf, S.M.; Drake, C.L. Shift Work and Shift Work Sleep Disorder: Clinical and Organizational Perspectives. Chest 2017, 151, 1156–1172. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-Y.; Song, P.; Choi, S.J.; Suh, S.; Kwon, S.O.; Joo, E.Y. The impact of the shift system on health and quality of life of sleep technicians. Sleep Med. 2020, 76, 72–79. [Google Scholar] [CrossRef]
- Di Muzio, M.; Reda, F.; Diella, G.; Di Simone, E.; Novelli, L.; D’Atri, A.; Giannini, A.; De Gennaro, L. Not only a Problem of Fatigue and Sleepiness: Changes in Psychomotor Performance in Italian Nurses across 8-h Rapidly Rotating Shifts. J. Clin. Med. 2019, 8, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costa, G. Shift Work and Health: Current Problems and Preventive Actions. Saf. Health Work. 2010, 1, 112–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, B.; Ma, S.H.; Shin, A.; Chang, M.-C.; Choi, J.-Y.; Kim, S.; Han, W.; Noh, D.-Y.; Ahn, S.-H.; Kang, D.; et al. Korean Risk Assessment Model for Breast Cancer Risk Prediction. PLoS ONE 2013, 8, e76736. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.-J.; Kim, K.; Kim, S.-Y.; Kim, J.-H.; Suh, C.; Son, B.-C.; Lee, C.-K.; Choi, J. Effects of shift work on abdominal obesity among 20–39-year-old female nurses: A 5-year retrospective longitudinal study. Ann. Occup. Environ. Med. 2016, 28, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gu, F.; Han, J.; Laden, F.; Pan, A.; Caporaso, N.E.; Stampfer, M.J.; Kawachi, I.; Rexrode, K.M.; Willett, W.C.; Hankinson, S.E.; et al. Total and Cause-Specific Mortality of U.S. Nurses Working Rotating Night Shifts. Am. J. Prev. Med. 2015, 48, 241–252. [Google Scholar] [CrossRef] [Green Version]
- Chan, D.S.M.; Abar, L.; Cariolou, M.; Nanu, N.; Greenwood, D.C.; Bandera, E.V.; McTiernan, A.; Norat, T. World Cancer Research Fund International: Continuous Update Project—Systematic literature review and meta-analysis of observational cohort studies on physical activity, sedentary behavior, adiposity, and weight change and breast cancer risk. Cancer Causes Control. 2019, 30, 1183–1200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekenga, C.C.; Parks, C.G.; Sandler, D.P. A prospective study of occupational physical activity and breast cancer risk. Cancer Causes Control. 2015, 26, 1779–1789. [Google Scholar] [CrossRef] [Green Version]
- Holtermann, A.; Marott, J.L.; Gyntelberg, F.; Søgaard, K.; Mortensen, O.S.; Prescott, E.; Schnohr, P. Self-reported occupational physical activity and cardiorespiratory fitness: Importance for cardiovascular disease and all-cause mortality. Scand. J. Work. Environ. Health 2016, 42, 291–298. [Google Scholar] [CrossRef] [Green Version]
- Lim, M.; Jeong, K.S.; Oh, S.-S.; Koh, S.-B.; Chang, S.-J.; Ahn, Y.-S. Effects of Occupational and Leisure-Time Physical Activities on Insomnia in Korean Firefighters. Int. J. Environ. Res. Public Health 2020, 17, 5397. [Google Scholar] [CrossRef] [PubMed]
- Savard, J.; Morin, C.M. Insomnia in the Context of Cancer: A Review of a Neglected Problem. J. Clin. Oncol. 2001, 19, 895–908. [Google Scholar] [CrossRef] [PubMed]
- Palesh, O.G.; Roscoe, J.A.; Mustian, K.M.; Roth, T.; Savard, J.; Ancoli-Israel, S.; Heckler, C.; Purnell, J.Q.; Janelsins, M.C.; Morrow, G.R. Prevalence, Demographics, and Psychological Associations of Sleep Disruption in Patients with Cancer: University of Rochester Cancer Center–Community Clinical Oncology Program. J. Clin. Oncol. 2009, 28, 292–298. [Google Scholar] [CrossRef]
- Savard, J.; Ivers, H.; Villa, J.; Caplette-Gingras, A.; Morin, C.M. Natural Course of Insomnia Comorbid with Cancer: An 18-Month Longitudinal Study. J. Clin. Oncol. 2011, 29, 3580–3586. [Google Scholar] [CrossRef]
- Moore, T.A.; Berger, A.M.; Dizona, P. Sleep aid use during and following breast cancer adjuvant chemotherapy. Psycho Oncol. 2011, 20, 321–325. [Google Scholar] [CrossRef]
- Lange, T.; Dimitrov, S.; Born, J. Effects of sleep and circadian rhythm on the human immune system. Ann. New York Acad. Sci. 2010, 1193, 48–59. [Google Scholar] [CrossRef] [PubMed]
- Blask, D.E. Melatonin, sleep disturbance and cancer risk. Sleep Med. Rev. 2009, 13, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Trudel-Fitzgerald, C.; Zhou, E.S.; Poole, E.M.; Zhang, X.; Michels, K.B.; Eliassen, A.H.; Chen, W.Y.; Holmes, M.D.; Tworoger, S.S.; Schernhammer, E.S. Sleep and survival among women with breast cancer: 30 years of follow-up within the Nurses’ Health Study. Br. J. Cancer 2017, 116, 1239–1246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boivin, D.; Boudreau, P. Impacts of shift work on sleep and circadian rhythms. Pathol. Biol. 2014, 62, 292–301. [Google Scholar] [CrossRef] [PubMed]
- González-González, A.; Mediavilla, M.D.; Sánchez-Barceló, E.J. Melatonin: A Molecule for Reducing Breast Cancer Risk. Molecules 2018, 23, 336. [Google Scholar] [CrossRef] [Green Version]
- Talib, W.; Odeh, L.; Basheti, I. Synergistic effect of thymoquinone and melatonin against breast cancer implanted in mice. J. Cancer Res. Ther. 2018, 14, S324–S330. [Google Scholar] [CrossRef]
- Lee, H.-E.; Lee, J.; Jang, T.-W.; Kim, I.-A.; Park, J.; Song, J. The relationship between night work and breast cancer. Ann. Occup. Environ. Med. 2018, 30, 11. [Google Scholar] [CrossRef]
- Dossus, L.; Boutron-Ruault, M.-C.; Kaaks, R.; Gram, I.T.; Vilier, A.; Fervers, B.; Manjer, J.; Tjonneland, A.; Olsen, A.; Overvad, K.; et al. Active and passive cigarette smoking and breast cancer risk: Results from the EPIC cohort. Int. J. Cancer 2014, 134, 1871–1888. [Google Scholar] [CrossRef] [Green Version]
- Luo, J.; Margolis, K.L.; Wactawski-Wende, J.; Horn, K.; Messina, C.; Stefanick, M.L.; Tindle, H.A.; Tong, E.; Rohan, T.E. Association of active and passive smoking with risk of breast cancer among postmenopausal women: A prospective cohort study. BMJ 2011, 342, d1016. [Google Scholar] [CrossRef] [Green Version]
- Colditz, G.A. Epidemiology and Prevention of Breast Cancer. Cancer Epidemiol. Biomark. Prev. 2005, 14, 768–772. [Google Scholar] [CrossRef] [Green Version]
- Menegaux, F.; Truong, T.; Anger, A.; Cordina-Duverger, E.; Lamkarkach, F.; Arveux, P.; Kerbrat, P.; Févotte, J.; Guénel, P. Night work and breast cancer: A population-based case-control study in France (the CECILE study). Int. J. Cancer 2012, 132, 924–931. [Google Scholar] [CrossRef]
- James, R.E.; Lukanova, A.; Dossus, L.; Becker, S.; Rinaldi, S.; Tjønneland, A.; Olsen, A.; Overvad, K.; Mesrine, S.; Engel, P.; et al. Postmenopausal Serum Sex Steroids and Risk of Hormone Receptor–Positive and -Negative Breast Cancer: A Nested Case–Control Study. Cancer Prev. Res. 2011, 4, 1626–1635. [Google Scholar] [CrossRef] [Green Version]
- Pollán, M.; Ascunce, N.; Ederra, M.; Murillo, A.; Erdozáin, N.; Alés-Martínez, J.E.; Pastor-Barriuso, R. Mammographic density and risk of breast cancer according to tumor characteristics and mode of detection: A Spanish population-based case-control study. Breast Cancer Res. 2013, 15, R9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López-Abente, G.; Aragonés, N.; Pérez-Gómez, B.; Pollán, M.; García-Pérez, J.; Ramis, R.; Fernández-Navarro, P. Time trends in municipal distribution patterns of cancer mortality in Spain. BMC Cancer 2014, 14, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schernhammer, E.S.; Kroenke, C.H.; Laden, F.; Hankinson, S.E. Night work and risk of breast cancer. Epidemiology 2006, 17, 108–111. [Google Scholar] [CrossRef]
- El-Benhawy, S.A.; El-Tahan, R.A.; Nakhla, S.F. Exposure to Radiation During Work Shifts and Working at Night Act as Occupational Stressors Alter Redox and Inflammatory Markers. Arch. Med. Res. 2021, 52, 76–83. [Google Scholar] [CrossRef] [PubMed]
- López-Guillén García, A.; Vicente Pardo, J.M.; Retorno al trabajo tras cáncer de mama [Return to Work after Breast Cancer]. Med. Segur. Trab. 2017, 63, 51. Available online: http://scielo.isciii.es/scielo.php?script=sci_abstract&pid=S0465-546X2017000100051 (accessed on 21 March 2021).
- Kossek, E.E.; Lee, K.-H. Work-Family Conflict and Work-Life Conflict. In Oxford Research Encyclopedia of Business and Management; Oxford University Press: New York, NY, USA, 2017; pp. 1–23. [Google Scholar] [CrossRef]
- Badana, M.A.N.S.; Andel, R. Aging in the Philippines. Gerontologist 2018, 58, 212–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Labrague, L.; Ballad, C.; Fronda, D. Predictors and outcomes of work–family conflict among nurses. Int. Nurs. Rev. 2020. [Google Scholar] [CrossRef]
- Masuda, A.D.; Sortheix, F.M.; Beham, B.; Naidoo, L.J. Cultural value orientations and work–family conflict: The mediating role of work and family demands. J. Vocat. Behav. 2019, 112, 294–310. [Google Scholar] [CrossRef]
- Pinto, K.A.; Menezes, G.M.; Griep, R.H.; Lima, K.T.; Almeida, M.C.; Aquino, E.M.L. Work-family conflict and time use: Psychometric assessment of an instrument in ELSA-Brazil. Rev. Saúde Pública 2016, 50, 39. [Google Scholar] [CrossRef] [PubMed]
- Svedberg, P.; Mather, L.; Bergström, G.; Lindfors, P.; Blom, V. Time pressure and sleep problems due to thoughts about work as risk factors for future sickness absence. Int. Arch. Occup. Environ. Health 2018, 91, 1051–1059. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Health Status | Number of Cases | Percentage | Age (Mean) | Age (SD) |
|---|---|---|---|---|
| Healthy | 502 | 51.97% | 41.29 | 10.66 |
| Cancer | 99 | 10.25% | 41.89 | 10.06 |
| Breast cancer | 56 | 5.80% | 41.41 | 10.63 |
| Male | 5 | 0.52% | 38.40 | 11.46 |
| Female | 51 | 5.28% | 41.71 | 10.50 |
| Other cancer | 43 | 4.45% | 42.51 | 9.23 |
| Other illness | 365 | 37.78% | 40.91 | 10.64 |
| Overall | 966 | 100.00% | 41.21 | 10.60 |
| N (%) | Breast Cancer (%) (N = 56) | Healthy (%) (N = 502) | χ2 | p | Odds Ratio (CI = 95%) | |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 58 (10.4) | 8.6 | 91.4 | 0.144 | 0.705 | 0.831 (0.318, 2.173) |
| Female | 500 (89.6) | 10.2 | 89.8 | |||
| Age | ||||||
| 41 years or younger | 281 (50.4) | 8.9 | 91.1 | 0.813 | 0.367 | 0.775 (0.445, 1.350) |
| Older than 41 | 277 (49.6) | 11.2 | 88.8 | |||
| Marital status | ||||||
| With partner | 317 (56.8) | 12.3 | 87.7 | 4.178 | 0.041 | 1.848 (1.018, 3.355) |
| Single | 241 (43.2) | 7.1 | 92.9 | |||
| Academic degree | ||||||
| Nursing degree | 303 (54.3) | 10.6 | 89.4 | 0.203 | 0.653 | 1.137 (0.651, 1.985) |
| Nursing speciality, Master or Doctorate | 255 (45.7) | 9.4 | 90.6 | |||
| Hormonal-based oral contraceptives * | ||||||
| Yes | 334 (66.3) | 11.7 | 88.3 | 0.594 | 0.441 | 1.272 (0.689, 2.350) |
| Never | 170 (33.7) | 9.4 | 90.6 | |||
| Mammography * | ||||||
| Yes | 211 (42.5) | 26.1 | 73.9 | ** | <0.001 | 0.739 (0.682, 0.801) |
| Never | 286 (57.5) | 0 | 100 | |||
| Familial breast cancer * | ||||||
| Yes | 72 (13.1) | 19.4 | 80.6 | 7.814 | 0.005 | 2.511 (1.293, 4.879) |
| No | 479 (86.9) | 8.8 | 91.2 | |||
| Regular exposure to electromagnetic fields | ||||||
| Ever | 480 (86.0) | 90.0 | 10.0 | 0.005 | 0.944 | 1.029 (0.467, 2.266) |
| Never | 78 (14.0) | 89.7 | 10.3 | |||
| Regular exposure to cytostatic medication | ||||||
| Ever | 392 (70.3) | 90.1 | 9.9 | 0.011 | 0.916 | 1.033 (0.566, 1.883) |
| Never | 166 (29.7) | 89.8 | 10.2 | |||
| BMI | ||||||
| Underweight | 10 (1.8) | 20.0 | 80.0 | 8.074 | 0.045 | - |
| Normal | 376 (67.4) | 7.7 | 92.3 | |||
| Overweight | 128 (22.9) | 13.3 | 86.7 | |||
| Obese | 44 (7.9) | 18.2 | 81.8 | |||
| Physical activity at work | ||||||
| Light | 124 (22.2) | 8.1 | 91.9 | 30.175 | <0.001 | - |
| Moderate | 313 (56.1) | 9.6 | 90.4 | |||
| Hard | 113 (20.3) | 8.8 | 91.2 | |||
| Very hard | 8 (1.4) | 75.0 | 25.0 | |||
| Physical activity last week (hours) | ||||||
| Two hours or less | 286 (51.25) | 9.4 | 90.6 | 0.230 | 0.631 | 0.874 (0.530, 1.518) |
| More than 2 h | 272 (28.75) | 10.7 | 89.3 | |||
| Children younger than 14 | ||||||
| Yes | 225 (40.3) | 10.7 | 89.3 | 0.166 | 0.684 | 1.123 (0.642, 1.963) |
| No | 333 (59.7) | 9.6 | 90.4 | |||
| Care for dependents at home | ||||||
| Yes | 58 (10.4) | 24.1 | 75.9 | 14.257 | <0.001 | 3.470 (1.759, 6.844) |
| No | 500 (89.6) | 8.4 | 91.6 | |||
| Regular sleep schedule or pattern | ||||||
| Yes | 241 (43.2) | 11.6 | 88.4 | 1.177 | 0.278 | 1.357 (0.781, 2.359) |
| No | 317 (56.8) | 8.8 | 91.2 | |||
| Sleep medication | ||||||
| Yes | 116 (20.8) | 28.4 | 71.6 | 54.988 | <0.001 | 7.243 (4.047, 12.964) |
| No | 442 (79.2) | 5.2 | 94.8 | |||
| Did you ever smoke? | ||||||
| Yes | 301 (53.9) | 10.0 | 90.0 | 0.003 | 0.953 | 0.984 (0.565, 1.711) |
| No | 257 (46.1) | 10.1 | 89.9 | |||
| Currently smoking cigarettes | ||||||
| Yes, everyday | 82 (14.7) | 8.5 | 91.5 | 0.347 | 0.841 | - |
| Yes, some days | 24 (4.3) | 8.3 | 91.7 | |||
| No, I do not smoke | 452 (81.0) | 10.4 | 89.6 | |||
| The workplace complies with the smoking ban | ||||||
| Totally | 124 (22.2) | 16.1 | 83.9 | 11.377 | 0.010 | - |
| Almost always | 239 (42.8) | 10.9 | 89.1 | |||
| Hardly ever | 141 (25.3) | 6.4 | 93.6 | |||
| Never | 54 (9.7) | 1.9 | 98.1 | |||
| Exposition to tobacco smoke at home | ||||||
| More than 5 h a day | 22 (3.9) | 31.8 | 68.2 | 15.967 | 0.001 | - |
| Between 1 and 5 h a day | 36 (6.5) | 0 | 100 | |||
| Less than 1 h a day | 42 (7.5) | 7.1 | 92.9 | |||
| Never or hardly ever | 458 (82.1) | 10.0 | 90.0 | |||
| Organization * | ||||||
| Public system | 476 (85.9) | 9.9 | 90.1 | 0.204 | 0.651 | 0.840 (0.394, 1.791) |
| Private system/Consortium | 78 (14.1) | 11.5 | 88.5 | |||
| Healthcare level | ||||||
| Primary care | 102 (18.3) | 13.7 | 86.3 | 3.950 | 0.139 | - |
| Hospital or Emergencies | 435 (77.9) | 9.7 | 90.3 | |||
| Other *** | 21 (3.8) | 0 | 100 | |||
| Years of experience in the current company | ||||||
| 10 years or less | 270 (48.4) | 3.0 | 97.0 | 28.985 | <0.001 | 0.153 (0.071,0.329) |
| More than 10 years | 288 (51.6) | 16.7 | 83.3 | |||
| Type of contract | ||||||
| Full-time | 485 (86.9) | 10.9 | 89.1 | 3.267 | 0.071 | 2.863 (0.871, 9.412) |
| Part-time | 73 (13.1) | 4.1 | 95.9 | |||
| Shift work at this moment | ||||||
| No | 114 (20.4) | 20.2 | 79.8 | 16.315 | <0.001 | 3.148 (1.765, 5.615) |
| Yes | 444 (79.6) | 7.4 | 92.6 | |||
| Rotating shift work at this moment | ||||||
| No | 104 (18.6) | 18.3 | 81.7 | 9.597 | 0.002 | 2.519 (1.382, 4.592) |
| Yes | 454 (81.4) | 8.1 | 91.9 | |||
| Total years worked * | ||||||
| 16 years or less | 280 (52.8) | 1.8 | 98.2 | 36.842 | <0.001 | 0.090 (0.035, 0.232) |
| More than 16 years | 250 (47.2) | 16.8 | 83.2 | |||
| Total years working regularly more than 3 nights per month | ||||||
| 10 years or less | 317 (56.8) | 4.7 | 95.3 | 22.870 | <0.001 | 0.242 (0.131, 0.449) |
| More than 10 years | 241 (43.2) | 17.0 | 83.0 | |||
| Night work at this moment | ||||||
| No | 180 (32.3) | 16.7 | 83.3 | 12.940 | <0.001 | 2.708 (1.548, 4.735) |
| Yes | 378 (67.7) | 6.9 | 93.1 | |||
| Total night shifts * | ||||||
| Up to 500 night shifts | 302 (56.2) | 5.3 | 94.7 | 12.187 | <0.001 | 0.342 (0.184, 0.639) |
| From 500 night shifts onwards | 235 (43.8) | 14.0 | 86.0 | |||
| Age of first night shift | ||||||
| 22 or younger | 289 (51.8) | 9.7 | 90.3 | 0.080 | 0.777 | 0.923 (0.532, 1.604) |
| Older than 22 | 269 (48.2) | 10.4 | 89.6 | |||
| Sick leaves * | ||||||
| 2 or less | 342 (62.2) | 3.8 | 96.2 | 36.977 | <0.001 | 0.161 (0.084, 0.309) |
| More than 2 | 208 (37.8) | 19.7 | 80.3 | |||
| Number of days on sick leave * | ||||||
| 40 days or less | 284 (51.6) | 1.1 | 98.9 | 47.121 | <0.001 | 0.048 (0.015, 0.158) |
| More than 40 days | 266 (48.4) | 18.0 | 82.0 | |||
| Sick leaves in the last year * | ||||||
| Without sick leave | 385 (69.5) | 4.4 | 95.6 | 40.782 | <0.001 | 0.165 (0.090, 0.303) |
| With sick leave | 169 (30.5) | 21.9 | 78.1 | |||
| Number of days on sick leave in the last year * | ||||||
| Never | 379 (68.5) | 4.5 | 95.5 | 36.134 | <0.001 | 0.180 (0.098, 0.331) |
| Some day | 174 (31.5) | 20.7 | 79.3 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Salgado, J.; Fagundo-Rivera, J.; Ortega-Moreno, M.; Allande-Cussó, R.; Ayuso-Murillo, D.; Ruiz-Frutos, C. Night Work and Breast Cancer Risk in Nurses: Multifactorial Risk Analysis. Cancers 2021, 13, 1470. https://doi.org/10.3390/cancers13061470
Gómez-Salgado J, Fagundo-Rivera J, Ortega-Moreno M, Allande-Cussó R, Ayuso-Murillo D, Ruiz-Frutos C. Night Work and Breast Cancer Risk in Nurses: Multifactorial Risk Analysis. Cancers. 2021; 13(6):1470. https://doi.org/10.3390/cancers13061470
Chicago/Turabian StyleGómez-Salgado, Juan, Javier Fagundo-Rivera, Mónica Ortega-Moreno, Regina Allande-Cussó, Diego Ayuso-Murillo, and Carlos Ruiz-Frutos. 2021. "Night Work and Breast Cancer Risk in Nurses: Multifactorial Risk Analysis" Cancers 13, no. 6: 1470. https://doi.org/10.3390/cancers13061470
APA StyleGómez-Salgado, J., Fagundo-Rivera, J., Ortega-Moreno, M., Allande-Cussó, R., Ayuso-Murillo, D., & Ruiz-Frutos, C. (2021). Night Work and Breast Cancer Risk in Nurses: Multifactorial Risk Analysis. Cancers, 13(6), 1470. https://doi.org/10.3390/cancers13061470